Abstract
Younger women use both internal medicine and OBGYN clinics as primary sources of health care. However, the role of OBGYNs in cardiovascular disease (CVD) prevention is largely unexplored. The objective of this study is to examine rates of hypertension recognition in women under 50 who present with elevated blood pressures in family practice and internal medicine (Medicine) and OBGYN clinics, and to compare these rates across clinic type. The study’s population consisted of 34,627 non-pregnant women ages 18–49 with new-onset hypertension (defined as two consecutive visits with elevated blood pressures of SBP ≥140mmHg or DBP ≥90 mmHg with no prior hypertension history) from 2002–2006. Multivariate logistic regressions predicting the clinical recognition of hypertension (a recorded diagnosis of hypertension and/or an antihypertensive prescription by any provider within one year of the second elevated blood pressure) assessed the association between hypertension recognition and the clinic where the second elevated blood pressure was recorded. Analysis showed that hypertension was recognized in less than 33% of women with new-onset hypertension. Women whose second consecutive elevated blood pressure was recorded in OBGYN were less likely to be recognized as having hypertension within 12 months by any provider compared to women whose second consecutive elevated blood pressure was recorded in Medicine (OR=0.51;95% CI=(0.48, 0.54)). This study suggests that further attention be paid to identifying and treating CVD risk factors in women under 50 presenting in both Medicine and OBGYN, and that improved coordination across care settings has the potential to improve CVD prevention in young women.
Keywords: Hypertension, gender, CVD prevention, primary care, OBGYN
Introduction
Cardiovascular disease (CVD) is the leading cause of death, disability, and health care expenditure in the United States for women and men.1 The recognition and treatment of hypertension, a key CVD risk factor, is a critical component in preventing CVD-related mortality and morbidity.2–4 Hypertension is routinely managed in the primary care settings; 5–7 however, women access primary care differently than men. Obstetrics-gynecology (OBGYN) clinics serve as a main source of primary health care for many younger women. 8–14 Most ambulatory visits for women ages 15–44 in the U.S. take place in OBGYN clinics,12 and women under 35 are particularly likely to see their OBGYN as their primary care provider.15 However, there is very little information on extent to which hypertension screening and other CVD preventive care for young women is provided through OBGYN clinics.
Evidence on the level of primary care services provided by OBGYN clinics is mixed.11, 16–20 While women who use OBGYNs as their primary source of care may be more likely to receive preventive care services such as tobacco use screening and vaccinations 8 , other studies suggest that OBGYNs may provide a narrower range of primary care services than is provided in other primary care settings.21
Hypertension screening, recognition, and treatment are key components of primary care and effective strategies for CVD prevention, 22 yet the rates of diagnosis and treatment of hypertension in the OBGYN setting are unknown. The objectives of this study are to examine rates of hypertension recognition (defined as a recorded diagnosis of hypertension by any provider or a filled prescription for an antihypertensive medication) in women under the age of 50, and to compare these rates by type of clinic where high blood pressures indicating hypertension were initially recorded.
Methods
Study Population
This study was conducted within the Cardiovascular Research Network (CVRN), a consortium of research organizations affiliated with the HMO Research Network and sponsored by the National Heart Lung and Blood Institute (U19 HL91179-01). The study population consists of patients from the Cardiovascular Research Network (CVRN) Hypertension Registry, a multi-site data source comprised of over 500,000 patients with hypertension, from Kaiser Permanente Northern California and Kaiser Permanente Colorado. These two health plans serve 3.6 million members, roughly 725,000 of whom have either recognized or unrecognized hypertension. Further information on the CVRN Hypertension Registry definitions and data sources are available elsewhere.23–24
Since women under fifty are most likely to utilize OBGYN clinics for primary care 12, 15 , the study included women ages 18–49 with new-onset hypertension between 2002 and 2006 whose hypertension was manifest through two consecutive elevated blood pressures of systolic blood pressure (SBP) ≥140mmHg or diastolic blood pressure (DBP) ≥90 mmHg. 2, 22–24 Single blood pressure readings are taken by nursing staff (eg, medical assistants) after patients have been seated for 5 minutes in the examination room in both OBGYN and Medicine clinics. Aneroid sphygmomanometers (Welch-Allyn) are the preferred measurement method in Kaiser Permanente Colorado, whereas automated measurement devices (Mindray Medical) are recommended in Kaiser Permanente Northern California. However, there is some use of the other method in each region. Staff are certified in blood pressure measurement at the time of hiring and retrained annually. Equipment is monitored by nursing staff and recalibrated as needed by bioengineering services. Blood pressure readings from settings outside of OBGYN and Medicine clinics (approximately 3%) were excluded from analyses because urgent symptoms could affect blood pressure values and because of uncertainty that the above protocol was consistently followed in other settings.
For the small percentage of women with pre-existing diabetes or chronic kidney disease (<6%), lower cutpoints of SBP ≥ 130 mmHg and DBP ≥ 80 mmHg were used.22–24 To ensure that these cases were truly incident, patients with previous diagnoses of hypertension or evidence of antihypertensive medication use were excluded. Women whose elevated blood pressures were associated with pregnancy (i.e. were within 9 months prior or 2 months after a delivery date) were also excluded. To better distinguish incident from prevalent hypertension, study subjects were required to have at least 12 months continuous membership before the first elevated blood pressure. At least 12 months of continuous membership were required after the second consecutive elevated blood pressure to determine if recognition occurred.
Clinic of Elevated Blood Pressure Presentation
The clinic where the second consecutive elevated blood pressure occurred was identified through the electronic medical record and recorded in the CVRN hypertension registry. Patients were categorized based on whether this reading was recorded in a medicine (internal medicine or family medicine) clinic vs. an OBGYN clinic, since the presentation of this second consecutive elevated blood pressure is the point at which guidelines suggest that hypertension recognition should occur. 2, 22
Hypertension Recognition
Hypertension recognition was defined as a recorded diagnosis of hypertension or a filled prescription for an antihypertensive medication issued by any provider, regardless of specialty or subspecialty, and occurring on or after the date of the second consecutive elevated blood pressure.23–24 The study examined whether recognition occurred anytime within one year of this date. Using this definition, a successful referral to a medicine clinic for hypertension evaluation or treatment from an OBGYN would be considered to be appropriate recognition of the condition.
Statistical Analyses
Chi-square analyses were used to assess the association between hypertension recognition within 12 months of the second consecutive elevated blood pressure and the type of clinic where the second elevated blood pressure was recorded. The relationship between clinic type and hypertension recognition was then examined within key subgroups, including patient age categories (ages 18–29, 30–39, vs. 40–49) and increasing levels of SBP (both consecutive elevated blood pressures with SBP ≥150; the first SBP ≥150 and the second SBP ≥160; and both SBPs ≥160). We also examined recognition rates by clinic type within African-American women, due to their increased level of risk for CVD-related mortality and morbidity.2, 25–26
Multivariate logistic regression models were then used to adjust for patient age, the mean SBP of the two consecutive elevated blood pressures, body mass index (BMI),smoking status, and diagnoses of the following co-morbid conditions in the 12 months prior to the first elevated blood pressure: ischemic heart disease, stroke, peripheral vascular disease, congestive heart failure, depression, diabetes mellitus, and chronic kidney disease (all obtained through membership, inpatient, and ambulatory databases.) Socioeconomic status (SES), estimated by geocoding patients’ residence address to the 2000 U.S. Census data at the block group level, was also adjusted for in the analyses. Further information on these variables can be obtained elsewhere. 23 To ensure that results were not biased by the inclusion of the small subset of women who appeared to revert to normal blood pressure levels without treatment or recognition of hypertension, analyses were repeated after deleting the subgroup of women (n=1,882) who did not have elevated blood pressures in any of the five subsequent recorded blood pressure readings.
This study was approved by the Kaiser Permanente Northern California and Kaiser Permanente Colorado Institutional Review Boards.
Results
A total of 34,627 women were eligible for inclusion in the study. Women were 39.4 years old on average, and 42% were white (Table 1). Thirty-two percent of women had their second consecutive elevated blood pressure recorded in an OBGYN clinic. 56% of women had an SBP ≥ 150 mmHg in both of their recorded consecutive elevated blood pressures. Patient age varied by clinic presentation category, with more women ages 18–29 presenting their second elevated blood pressures in an OBGYN clinic. Patients were similar across clinic categories in race/ethnicity, mean SBP, comorbidity burden, BMI, smoking status, and socioeconomic status.
Table 1.
Patient Demographics and Clinical Characteristics
| Demographic / Clinical Characteristic |
TOTAL N(%) | Second Elevated Blood Pressure Detected In Medicine |
Second Elevated Blood Pressure Detected in OBGYN |
|---|---|---|---|
| n=34,627 | n=23,596 (68%) | n=11,031 (32%) | |
| Mean Age (SD) | 39.4 (7.9) | 40.0 (7.6) | 38.1 (8.3) |
| Ages 18–29 (%) | 4720 (14%) | 2742 (12%) | 1978 (18%) |
| Ages 30–39 (%) | 9662 (28%) | 6284 (27%) | 3378 (31%) |
| Ages 40–49 (%) | 20245 (58%) | 14570 (62%) | 5675 (51%) |
| Mean Systolic Blood Pressure (SBP) of Two Consecutive Elevated Blood Pressures (SD) |
145.7 (10.5) | 145.2 (11.0) | 146.9 (9.3) |
| Both Consecutive Elevated Blood Pressures w/ SBP >= 150 |
19,279 (56%) | 12,299 (52%) | 6,980 (63%) |
| Mean Annual visits to Medicine (SD) | 3.6 (4.5) | 4.1 (4.8) | 2.6 (3.3) |
| Mean Annual visits to Obgyn (SD) | 1.7 (3.4) | 1.1 (2.4) | 2.8 (4.8) |
| Race/Ethnicity | |||
| White | 42% | 42% | 44% |
| African American | 11% | 11% | 13% |
| Latino | 15% | 15% | 15% |
| Asian | 11% | 11% | 11% |
| Native American | 1% | 1% | 1% |
| Unknown/Other | 20% | 21% | 16% |
| Mean Income* | |||
| Missing | 3% | 3% | 3% |
| <30K | 7% | 7% | 7% |
| 30–<60K | 46% | 47% | 45% |
| 60+K | 44% | 43% | 45% |
| Education: % in Block with a BA* | |||
| Missing | 3% | 3% | 3% |
| < 30% | 5% | 5% | 5% |
| 30–<60% | 39% | 39% | 38% |
| 60+% | 53% | 52% | 54% |
| Comorbidities | |||
| Ischemic Heart Disease | 0.05% | 0.06% | 0.02% |
| Stroke | 0.09% | 0.12% | 0.04% |
| Peripheral Vascular Disease | 0.05% | 0.06% | 0.03% |
| Congestive Heart Failure | 0.03% | 0.04% | 0.00% |
| Depression | 13% | 14% | 10% |
| Diabetes | 5% | 5% | 3% |
| Chronic Kidney Disease | 0.73% | 0.83% | 0.52% |
| Current Smoker | 14% | 15% | 12% |
| Mean BMI (SD) | 31.6 (7.6) | 32.0 (7.6) | 30.8 (7.4) |
Note: All cross-OB/GYN variable differences significant at p<.0001;
from block-level geocoded data
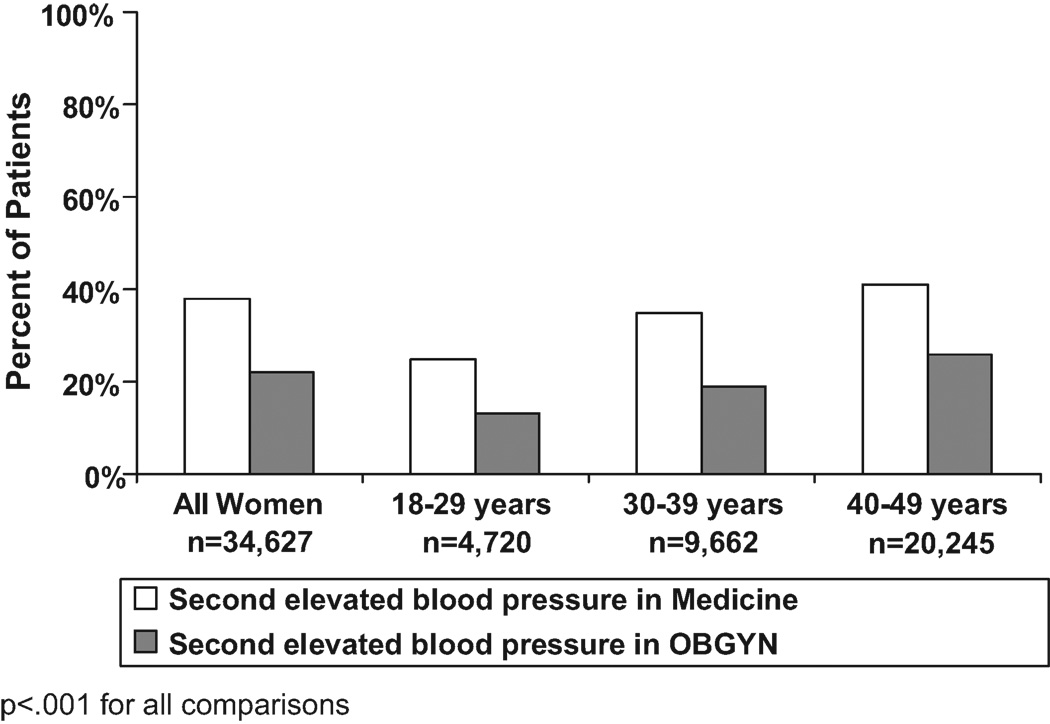
Women whose second consecutive elevated blood pressure occurred in an OBGYN clinic were significantly less likely to be recognized as hypertensive within a year by any provider (Figure 1). Less than one-quarter (22%) of women presenting in OBGYN with their second elevated blood pressure had their hypertension recognized within one year, compared with 38% of those presenting in Medicine (p<.0001). Among older women (ages 40–49), 25% of those presenting in OBGYN were recognized within a year compared with 41% in Medicine (p<.0001). Overall, women ages 18–29 had the lowest chance of having their hypertension recognized; less than 25% of women under 30 were recognized within a year regardless of the clinic where the elevated blood pressure occurred.
Figure 1.
Hypertension Recognized within 12 Months of Second Consecutive Elevated Blood Pressure, by Patient Age
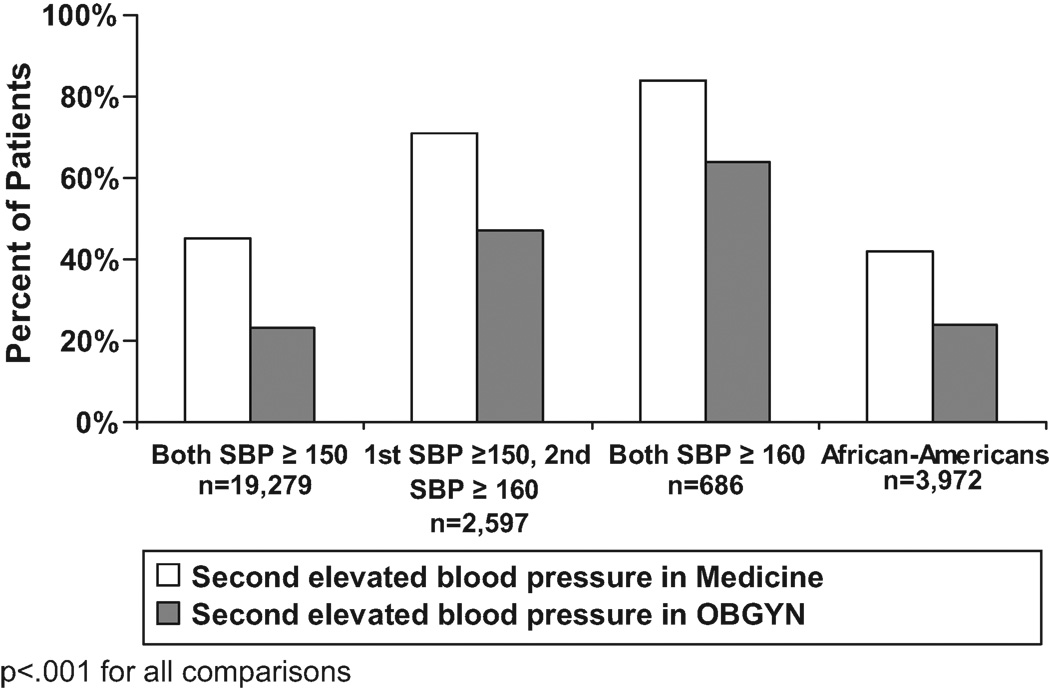
Figure 2 shows the rate of hypertension recognition by clinic type for women in higher risk groups based on SBP level and race/ethnicity. Women who presented with two SBPs ≥ 150 mm Hg and African American women were much less likely to be recognized as hypertensive within one year by any provider if their second consecutive elevated blood pressure occurred in OBGYN as opposed to Medicine. Significant differences in recognition rates between OBGYN and Medicine clinics persisted in the subgroups of women with one or more SBP > 160 mmHg.
Figure 2.
Hypertension Recognized within 12 Months of Second Consecutive Elevated Blood Pressure, by Systolic Blood Pressure Level
After adjusting for patient characteristics including age, SBP level, and race/ethnicity, women who presented their second consecutive elevated blood pressure in OBGYN were substantially less likely to be recognized as having hypertension within a year than those who received their second elevated blood pressure in a Medicine clinic (OR = .51; 95% CI = (.48, .54)); (Table 2).
Table 2.
Odds Ratios for Predicting Hypertension Recognition
| Predictor Variable | Hypertension Recognition within 12 Months of the Second Consecutive Elevated Blood Pressure:Odds Ratio (95% CI) |
|---|---|
| Second Elevated Blood Pressure Occurs in an OBGYN Clinic |
0.51 (0.48, 0.54) |
| Annual visits to Medicine | 1.10 (1.10, 1.11) |
| Annual visits to Obgyn | 0.97 (0.96, 0.98) |
| Race (White as referent) | |
| African-American | 1.36 (1.26, 1.47) |
| Native-American | 1.21 (0.95, 1.55) |
| Asian-American | 1.66 (1.53, 1.80) |
| Hispanic/Latino | 1.13 (1.05, 1.22) |
| Unknown/Other | 1.26 (1.18, 1.35) |
| Mean SBP of Two Consecutive Elevated Blood Pressures |
1.05 (1.05, 1.06) |
| Age (40–49 years as referent) | |
| 18–29 years | 0.51 (0.47, 0.55) |
| 30–39 years | 0.82 (0.77, 0.86) |
| Income (> $30K as referent) | |
| < $30,000 | 1.01 (0.91, 1.13) |
| Income Data Missing | 1.53 (1.00, 2.34) |
| Education (> 60% as referent) | |
| < 30% | 1.11 (0.99, 1.25) |
| 30–60% | 1.05 (1.00, 1.11) |
| Education Data Missing | 0.83 (0.55, 1.25) |
| Comorbidities | |
| Stroke | 1.05 (0.48, 2.31) |
| Ischemic Heart Disease | 5.96 (1.71, 20.8) |
| Congestive Heart Failure | 5.06 (0.58, 44.2) |
| Chronic Kidney Disease | 0.59 (0.42, 0.83) |
| Depression | 0.91 (0.85, 0.98) |
| Diabetes | 1.40 (1.24, 1.59) |
| Peripheral Vascular Disease | 1.63 (0.54, 4.98) |
| BMI (20–25 as referent) | |
| < 20 | 0.87 (0.75, 1.00) |
| 26–35 | 1.04 (0.94, 1.15) |
| 35–40 | 1.07 (0.95, 1.21) |
| > 40 | 1.05 (0.93, 1.19) |
| BMI Data Missing | 0.86 (0.79, 0.95) |
| Current Smoker | 0.90 (0.84, 0.96) |
Sensitivity analyses demonstrated that the differences in recognition rates by clinic type were similar in analyses examining the subgroup of women who presented with three consecutive elevated blood pressures, although recognition rates were somewhat higher in both settings (30% vs. 51% for Medicine and OBGYN clinics, respectively). A similar pattern of results was also seen when the analyses were repeated excluding the small subset of women who appeared to revert to normal blood pressure levels without treatment or recognition of hypertension (data not shown.)
Discussion
In this study of more than 30,000 women under age 50 in two large U.S. integrated healthcare delivery systems, we find that care in OBGYN clinics was associated with significantly lower levels of hypertension recognition compared to care in Medicine clinics. These lower rates of hypertension recognition for women whose high SBPs presented in OBGYN clinics were observed among older as well as younger women, in those with higher SBP elevations, and in African Americans, all groups at higher risk of adverse outcomes as a consequence of untreated hypertension. Nearly one-third of women in this sample had their second consecutive elevated blood pressure measured in OBGYN, mirroring the high rates of women using OBGYN clinics for primary care observed nationally 12, 15 . Taken together, these results suggest visits to the OBGYN clinic may be important, and currently missed, opportunities for CVD prevention.
There are persistent gender disparities in CVD risk factor levels, treatment, and outcomes. 27–32 These disparities may stem in part from a lack of recognition by both patients and clinicians of women’s risk for CVD, and of the importance of CVD prevention to women’s health.31 Primary care providers play a critical role in CVD prevention, and differences in how women access primary care may play a role in these disparities. OBGYN visits are a prime, and for some women perhaps the only, opportunity for CVD screening and prevention in younger women.33–34 This study’s findings suggest that improving hypertension recognition in OBGYN clinics may be an important strategy in reducing these disparities.35
This study found that recognition of hypertension within a year of a second consecutive elevated blood pressure reading was low among all patients in this cohort of women under the age of fifty, regardless of where the second elevated blood pressure occurred. Overall, only 32.9% of women had their hypertension recognized within a year, and less than 40% of women whose second elevated blood pressure occurred in a medicine clinic were recognized within a year. These percentages were only slightly higher among the significant number of women with two presenting SBPs ≥150. This finding is consistent with previous literature suggesting that younger age is associated with lower levels of hypertension diagnosis 36 and treatment.4 Since undiagnosed hypertension prior to age forty 21, 25 and length of time of exposure to high blood pressures 37 are known risk factors for CVD mortality, further attention to elevated blood pressures in women under 50 by providers in both medicine and OBGYN clinics may be an important approach to primary CVD prevention.
OBGYNS may not be comfortable initiating diagnosis and treatment for hypertension ,38–39 or prefer to focus on gynecologic care and refer issues of CVD prevention to a general internist or family physician. This may particularly be true in the setting of this study, where women are encouraged to have both a designated OBGYN for gynecologic care and a medicine provider for more general primary care. That women who present their second consecutive elevated blood pressures in OBGYN clinics had a significantly lower odds of hypertension recognition within a year by any provider indicates that care could be improved by either enhancing the frequency of referrals to general internists and family physicians, or by increasing the likelihood that OBGYNs will recognize and treat hypertension appropriately, or both. While individual physicians play a key role in CVD risk identification and prevention, ideally integrated health care systems should be able to detect incident hypertension regardless of the type of clinic in which it presents. Neither health care system in the study had system-level outreach programs targeted at the patients or their providers to address elevated blood pressures in young female patients without pre-existing CVD risk factors. System-level interventions such as point-of-care clinical decision support to identify hypertension and guide initial treatment, automated referrals, and active outreach to patients may improve recognizing and treating hypertension in women across all care sites. This study found that clinic type had a significant impact on hypertension recognition even within a large integrated delivery system with electronic medical records where referrals and outreach across clinics are more feasible than in many settings. This study’s findings of low levels of hypertension recognition and referral through OBGYN clinics suggests that addressing CVD risk factors in OBGYN may be a major opportunity to improve the cardiovascular health of women.
This study has a number of limitations that should be noted. This study defines hypertension recognition as the recording of a hypertension diagnosis or a dispensing of a hypertension medication. Lifestyle therapy, especially for younger adults, is an important approach to addressing incident hypertension, and it is possible that providers are treating incident hypertension with diet and lifestyle advice that we are unable to measure in the clinical data systems available to this study. Therefore providers treating incident hypertension with diet and lifestyle advice for a year without recording a diagnosis of hypertension would be incorrectly classified.
The data from this study is from two integrated delivery systems where medicine and OBGYN clinics are co-located at the same site. As OBGYNs can reasonably expect that their patients have other access to primary care, this may affect the rate of hypertension recognition in these OBGYN settings. While these results may not generalize to non-integrated delivery systems, they do suggest integration and close proximity alone may not be sufficient to provide appropriate preventive care. Similarly, the presence of electronic medical records in our study sites, which should facilitate access to prior blood pressure readings, limits the generalizability of these findings to settings without such information technologies. However, health care providers in this country are rapidly moving towards the use of EMRs to improve coordination of care; 40our results suggest that these technologies alone are also not sufficient to assure guideline-driven care.
While hypertension screening in primary care is a key component of CVD prevention, lipid testing and other CVD-related screenings are also traditionally provided through primary care. Further research should examine whether the type of clinic where women receive primary care plays a role in the receipt of these types of services as well.
Perspectives
Many young women with incident hypertension present in OBGYN clinics, and these women are substantially less likely to be diagnosed or treated for hypertension. These findings suggest that further attention to identifying and treating CVD risk factors be paid to young women presenting in OBGYN clinics, and that coordination of care across clinics may lead to improved care of this important CVD risk factor.
Acknowledgments
Sources of Funding: This study was funded by the National Heart Lung and Blood Institute (NHLBI) (U19 HL91179-01). The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the funding organizations. Dr. Schmittdiel’s work on this study was supported by the Office of Research in Women’s Health Building Interdisciplinary Careers in Women’s Health K12 Career Development Award (K12HD052163). Dr. Ho is supported by a VA HSR&D Career Development Award (05-026-1)* . Dr. Daugherty is supported by Award Number K08HL103776 from the National Heart, Lung and Blood Institute. The authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions: Drs. Schmittdiel and Bibbins-Domingo (KB) had the original idea for the study. The study was planned by Drs. Schmittdiel, Bibbins-Domingo, and Selby. Mr. Swain performed the statistical analysis. Dr. Schmittdiel drafted the article. All authors were involved in the interpretation of data and the revision of the manuscript for important intellectual content. All authors gave final approval of the manuscript submitted for publication. Dr. Schmittdiel is the guarantor for the study.
Conflicts of Interest: Dr. Ho serves as a consultant for Wellpoint, Inc. The authors have no other conflicts of interest to report.
References
- 1.Centers for Disease C, Prevention. Prevalence of heart disease--United States, 2005. MMWR.Morb Mortal Wkly Rep. 2007;56:113–118. [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materso BJ, Oparil S, Wright JT, Roccella EJ the National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, Franklin BA, Goldstein LB, Greenland P, Grundy SM, Hong Y, Miller NH, Lauer RM, Ockene IS, Sacco RL, Sallis JF, Jr, Smith SC, Jr, Stone NJ, Taubert KA. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106:388–391. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 4.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 5.McManus RJ, Mant J. Management of blood pressure in primary care. BMJ. 2009;338:b940. doi: 10.1136/bmj.b940. [DOI] [PubMed] [Google Scholar]
- 6.Andrade SE, Gurwitz JH, Field TS, Kelleher M, Majumdar SR, Reed G, Black R. Hypertension management: the care gap between clinical guidelines and clinical practice. Am J Manag Care. 2004;10:481–486. [PubMed] [Google Scholar]
- 7.O'Connor PJ, Quiter ES, Rush WA, Wiest M, Meland JT, Ryu S. Impact of hypertension guideline implementation on blood pressure control and drug use in primary care clinics. Jt Comm J Qual Improv. 1999;25:68–77. doi: 10.1016/s1070-3241(16)30428-x. [DOI] [PubMed] [Google Scholar]
- 8.Lewis BG, Halm EA, Marcus SM, Korenstein D, Federman AD. Preventive services use among women seen by gynecologists, general medical physicians, or both. Obstet Gynecol. 2008;111:945–952. doi: 10.1097/AOG.0b013e318169ce3e. [DOI] [PubMed] [Google Scholar]
- 9.Coleman VH, Laube DW, Hale RW, Williams SB, Power ML, Schulkin J. Obstetrician-gynecologists and primary care: training during obstetrics-gynecology residency and current practice patterns. Acad Med. 2007;82:602–607. doi: 10.1097/ACM.0b013e3180556885. [DOI] [PubMed] [Google Scholar]
- 10.Hurd WW, Barhan SM, Rogers RE. Obstetrician-gynecologist as primary care provider. Am J Manag Care. 2001;7:SP19–SP24. [PubMed] [Google Scholar]
- 11.Horton JA, Cruess DF, Pearse WH. Primary and preventive care services provided by obstetrician-gynecologists. Obstet Gynecol. 1993;82:723–726. [PubMed] [Google Scholar]
- 12.Leader S, Perales PJ. Provision of primary-preventive health care services by obstetrician-gynecologists. Obstet Gynecol. 1995;85:391–395. doi: 10.1016/0029-7844(94)00411-6. [DOI] [PubMed] [Google Scholar]
- 13.Higgins RV, Hall JB, Laurent S. Primary care by obstetricians and gynecologists: attitudes of the members of The South Atlantic Association of Obstetricians and Gynecologists. Am J Obstet Gynecol. 1997;177:311–317. doi: 10.1016/s0002-9378(97)70192-3. discussion 317–318. [DOI] [PubMed] [Google Scholar]
- 14.Lentz GM, Ayala L, Eckert LO. A comprehensive women's health care center: are gynecologists offering primary care? Am J Obstet Gynecol. 2006;194 doi: 10.1016/j.ajog.2006.03.010. 1660-1666-7. [DOI] [PubMed] [Google Scholar]
- 15.Henderson JT, Weisman CS. Women's patterns of provider use across the lifespan and satisfaction with primary care coordination and comprehensiveness. Medical care. 2005;43:826–833. doi: 10.1097/01.mlr.0000170422.73033.eb. [DOI] [PubMed] [Google Scholar]
- 16.American College of O, Gynecologists. [Accessed October 6, 2009];ACOG Encourages Ob-Gyns to Address the Health Risks of Obesity in Women. http://www.acog.org/from_home/publications/press_releases/nr09-30-05-1.cfm.
- 17.Power ML, Cogswell ME, Schulkin J. Obesity prevention and treatment practices of U.S. obstetrician-gynecologists. Obstet Gynecol. 2006;108:961–968. doi: 10.1097/01.AOG.0000233171.20484.db. [DOI] [PubMed] [Google Scholar]
- 18.Schrag SJ, Fiore AE, Gonik B, Malik T, Reef S, Singleton JA, Schuchat A, Schulkin J. Vaccination and perinatal infection prevention practices among obstetrician-gynecologists. Obstet Gynecol. 2003;101:704–710. doi: 10.1016/s0029-7844(03)00010-3. [DOI] [PubMed] [Google Scholar]
- 19.Gonik B, Jones T, Contreras D, Fasano N, Roberts C. The obstetrician-gynecologist's role in vaccine-preventable diseases and immunization. Obstet Gynecol. 2000;96:81–84. doi: 10.1016/s0029-7844(00)00860-7. [DOI] [PubMed] [Google Scholar]
- 20.Coco A. How often do physicians address other medical problems while providing prenatal care? Ann Fam Med. 2009;7:134–138. doi: 10.1370/afm.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scholle SH, Chang J, Harman J, McNeil M. Characteristics of patients seen and services provided in primary care visits in obstetrics/gynecology: data from NAMCS and NHAMCS. Am J Obstet Gynecol. 2004;190:1119–1127. doi: 10.1016/j.ajog.2003.09.059. [DOI] [PubMed] [Google Scholar]
- 22.Screening for high blood pressure: U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2007 Dec 4;147:783–786. doi: 10.7326/0003-4819-147-11-200712040-00009. [DOI] [PubMed] [Google Scholar]
- 23.Selby JV, Lee J, Swain BE, Tavel HM, Ho PM, Margolis KL, O’Connor PJ, Fine L, Schmittdiel JA, Magid DJ. Trends in time to confirmation and recognition of new-onset hypertension, 2002–2006. Hypertension. 2010;56:605–611. doi: 10.1161/HYPERTENSIONAHA.110.153528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ho PM, Zeng C, Tavel HM, Selby JV, O'Connor PJ, Margolis KL, Magid DJ. Trends in first line therapy for hypertension in the Cardiovascular Research Network (CVRN) Hypertension Registry, 2002–2007. Arch Intern Med. 2010;170:912–913. doi: 10.1001/archinternmed.2010.102. [DOI] [PubMed] [Google Scholar]
- 25.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Roger VL, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics--2010 Update. A Report From the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 27.Mosca L, Merz NB, Blumenthal RS, Cziraky MJ, Fabunmi RP, Sarawate C, Watson KE, Willey VJ, Stanek EJ. Opportunity for intervention to achieve American Heart Association guidelines for optimal lipid levels in high-risk women in a managed care setting. Circulation. 2005;111:488–493. doi: 10.1161/01.CIR.0000153859.66086.85. [DOI] [PubMed] [Google Scholar]
- 28.Holroyd-Leduc JM, Kapral MK, Austin PC, Tu JV. Sex differences and similarities in the management and outcome of stroke patients. Stroke. 2000;31:1833–1837. doi: 10.1161/01.str.31.8.1833. [DOI] [PubMed] [Google Scholar]
- 29.Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, Manhapra A, Mallik S, Krumholz HM. National Registry of Myocardial Infarction Investigators. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI, Canto J. Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med. 2009;169:1767–1774. doi: 10.1001/archinternmed.2009.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keyhani S, Scobie JV, Hebert PL, McLaughlin MA. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension. 2008;51:1149–1155. doi: 10.1161/HYPERTENSIONAHA.107.107342. [DOI] [PubMed] [Google Scholar]
- 32.Ferrara A, Mangione CM, Kim C, Marrero DG, Curb D, Stevens M, Selby JV. Translating Research Into Action for Diabetes Study Group. Sex disparities in control and treatment of modifiable cardiovascular disease risk factors among patients with diabetes: Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care. 2008 Jan;31(1):69–74. doi: 10.2337/dc07-1244. [DOI] [PubMed] [Google Scholar]
- 33.Grimes DA. Prevention of cardiovascular disease in women: role of the obstetrician-gynecologist. Am J Obstet Gynecol. 1988;158(6 Pt 2):1662–1668. doi: 10.1016/0002-9378(88)90207-4. [DOI] [PubMed] [Google Scholar]
- 34.Lewis V, Barnhart J, Houghton JL, Charney P. A brief office educational intervention improved referral rates for hypertension control in women. Int J Cardiol. 2008 doi: 10.1016/j.ijcard.2008.08.024. [DOI] [PubMed] [Google Scholar]
- 35.Barnhart J, Lewis V, Houghton JL, Charney P. Physician knowledge levels and barriers to coronary risk prevention in women: survey results from the Women and Heart Disease Physician Education Initiative. Women's health issues. 2007;17:93–100. doi: 10.1016/j.whi.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 36.Steckelings UM, Stoppelhaar M, Sharma AM, Wittchen HU, Krause P, Küpper B, Kirch W, Pittrow D, Ritz E, Göke B, Lehnert H, Tschöpe D, Höfler M, Pfister H, Unger T HYDRA Study Group. HYDRA: possible determinants of unsatisfactory hypertension control in German primary care patients. Blood Press. 2004;13:80–88. doi: 10.1080/08037050310030982. [DOI] [PubMed] [Google Scholar]
- 37.Pletcher MJ, Bibbins-Domingo K, Lewis CE, Wei GS, Sidney S, Carr JJ, Vittinghoff E, McCulloch CE, Hulley SB. Prehypertension during young adulthood and coronary calcium later in life. Ann Intern Med. 2008;149:91–99. doi: 10.7326/0003-4819-149-2-200807150-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parsey KS, Bastia LA, Couchman GM, Slack KD, Simel DL. The development of a primary care curriculum for obstetrics/gynecology residents. J Am Med Womens Assoc. 1998;53:137–139. [PubMed] [Google Scholar]
- 39.Stovall DW, Loveless MB, Walden NA, Karjane N, Cohen SA. Primary and preventive healthcare in obstetrics and gynecology: a study of practice patterns in the mid-atlantic region. J Womens Health (Larchmt) 2007;16:134–138. doi: 10.1089/jwh.2006.0066. [DOI] [PubMed] [Google Scholar]
- 40.Buntin MB, Jain SH, Blumenthal D. Health Information Technology: laying the infrastructure for national health reform. Health Aff (Millwood) 2010;29:1214–1219. doi: 10.1377/hlthaff.2010.0503. [DOI] [PubMed] [Google Scholar]