Abstract
The late management of spontaneous esophageal perforation is the most challenging problem for the surgeon. In this paper, we present a case in whom a spontaneous esophageal perforation was successfully treated by T-tube drainage after unsuccessful conservative treatment. The patient, a 68-year-old male, was admitted to the hospital with sudden upper abdominal pain. After 2 days, esophageal perforation was diagnosed, and conservative management was begun. Thereafter, the subcutaneous emphysema disappeared, and the patient's temperature decreased. However, on day 13, the patient's temperature spiked above 38°C, and computed tomography showed a mediastinal abscess. An emergency left thoracotomy with laparotomy was performed. Since a 2-cm longitudinal perforation with severe inflammatory reactions was observed, the T-tube drainage method was performed. The patient was discharged without postoperative complications and has not experienced any gastrointestinal symptoms, such as gastroesophageal reflux or dysphagia. In conclusion, the T-tube drainage method appears to be a simple and effective method for the late management of esophageal perforation with severe inflammatory reaction.
Key Words: Esophageal perforation, Management, T-tube drainage
Introduction
Spontaneous esophageal perforation is a life-threatening condition with a high mortality rate. If treatment is begun within 24 h of onset, primary closure of the rupture is recommended and offers the best survival rate [1]. However, diagnosis and treatment are often delayed because the disease is extremely rare and is confused with many other disorders, resulting in a fatal outcome in some cases. The late management of esophageal perforation is a very challenging problem for a surgeon. The T-tube drainage method is technically very easy and safe and avoids the postoperative complications associated with primary suture or esophagectomy with primary or secondary reconstruction [2]. In this paper, we present a case in whom a spontaneous esophageal perforation was successfully treated by T-tube drainage after unsuccessful conservative treatment.
Case Report
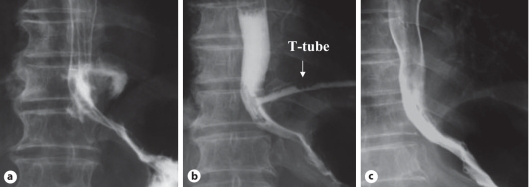
A 68-year-old man, a heavy drinker, was hospitalized for sudden upper abdominal pain. His abdomen was soft, and signs of peritoneal irritation were negative. Chest and abdominal X-rays showed no abnormality. After 2 days, he developed subcutaneous emphysema and a fever in excess of 38°C. Computed tomography (CT) showed mediastinal emphysema without pleural effusion. An esophagogram revealed extravasation of the contrast medium from the left lower esophagus to the mediastinal cavity (fig. 1a). Since his condition met the relevant criteria for selecting nonoperative treatment of esophageal perforation established by Shaffer et al. [3], conservative management was begun. Thereafter, the subcutaneous emphysema disappeared, and the patient's temperature decreased. However, on day 13, his temperature spiked above 38°C, and a CT showed a mediastinal abscess. An emergency left thoracotomy with laparotomy was performed. A 2-cm longitudinal perforation with inflammatory reactions and a periesophageal abscess were observed on the left side of the esophageal wall, about 5 cm proximal to the esophagogastric junction. After mediastinal irrigation, a latex rubber T-tube, generally used for operations for common bile duct stones, was inserted into the rupture, and the esophageal wall around the T-tube was closed by interrupted 3-0 sutures. The T-tube, which was brought out through the lateral chest wall, was connected to free the drainage. An intrathoracic drainage tube was also inserted, but a gastrostomy was not performed. During the postoperative period, saliva gushed through the T-tube when the patient coughed. On postoperative day 7, the intrathoracic drainage tube was removed. On postoperative day 24, no evidence of leakage into the thoracic cavity was observed by esophagogram, and the T-tube was obviated (fig. 1b). Thereafter, a thoracotomy tube was inserted 2 cm lateral to the esophagus through the fistula and withdrawn little by little each day. Human antihemolytic factor XIII (Fibrogammin P, Aventis Pharma Ltd., Tokyo, Japan) was intravenously administered for 5 days. Six days after removal of the T-tube, the esophagogram showed complete healing of the fistula (fig. 1c). The patient was discharged without postoperative complications.
Fig. 1.
a Esophagogram revealed extravasation of contrast medium (Gastrografin) from the left lower esophagus to the mediastinal cavity. b A contrast material (Gastrografin) swallow was performed on postoperative day 24. No evidence of leakage into the thoracic cavity was found. c Six days after removal of the T-tube, barium swallow showed complete healing of the esophago-pleura-cutaneous fistula.
Discussion
Spontaneous perforation of the esophagus was first identified by Boerhaave in 1724 and is well known as Boerhaave's syndrome. However, the condition is often confused with many other disorders, such as myocardial infarction, peptic ulcer, pancreatitis, dissecting aortic aneurysm, and pulmonary embolism, because the disease is extremely rare and the classic findings of vomiting, chest pain, and subcutaneous emphysema are often absent in early cases [2]. Delayed diagnosis produces an unfavorable outcome with a mortality rate of 20–40% [2].
The late management of esophageal perforation is a very challenging problem for a surgeon. The most important factors determining the choice of treatment are the clinical status of the patient, the vitality of the esophagus around the rupture, and the extent of contamination. The following treatments have been advocated: (1) primary suture and external drainage, (2) primary suture with reinforcement, (3) T-tube drainage through the perforation, and (4) esophagectomy with primary or secondary reconstruction [2]. It has been reported that the frequency of leakage for primary suture after delayed diagnosis is at least 50% [4]. An esophagectomy, which is performed to prevent esophageal leakage, is too invasive for patients in poor medical condition. In our case, we selected the T-tube drainage method because an inflammatory reaction on the edge of the perforation and a periesophageal abscess were observed and because the patient was a malnourished alcoholic. After surgery, we found that saliva gushed through the T-tube when the patient coughed. This finding strongly suggests that the rapid rise of intra-esophageal pressure may cause leakage of the suture line if a primary suture with or without reinforcement is performed. Therefore, decompression of the esophageal lumen is needed to prevent leakage of the suture line. The patient was discharged without postoperative complications or subsequent gastrointestinal symptoms. The T-tube drainage method appears to be a simple and effective method for the late management of esophageal perforation with severe inflammatory reaction.
However, the fistula after removal of the T-tube takes a long time to heal because the esophagus has no mesentery and no mesothelial cells to seal the laceration [2, 4]. Ojima et al. introduced a method using T-tube mediastinoabdominal drainage to overcome this difficult problem. The fistula usually dried up within 5 days [2]. Factor XIII has been recognized as an important wound-healing factor, and the administration of factor XIII enhances the granulation of surgical wounds in clinical and experimental studies [5]. In our case, human antihemolytic factor XIII was given intravenously, and complete healing of the esophago-pleura-cutaneous fistula was accomplished within 6 days of the removal of the T-tube. This finding seems to be equivalent to the results achieved on fistula healing using T-tube mediastinoabdominal drainage. The infusion of factor XIII may be beneficial for better fistula healing. However, such a conclusion cannot be made on the basis of a single report. Indeed, in view of the potential benefit of such a procedure, clinical trials should be conducted to gather more evidence.
References
- 1.Bladergroen MR, Lowe JE, Postlethwait RW. Diagnosis and recommended management of esophageal perforation and rupture. Ann Thorac Surg. 1986;42:235–239. doi: 10.1016/s0003-4975(10)62725-7. [DOI] [PubMed] [Google Scholar]
- 2.Ojima H, Kuwano H, Sasaki S, Fujisawa T, Ishibashi Y. Successful late management of spontaneous esophageal rupture using T-tube mediastinoabdominal drainage. Am J Surg. 2001;182:192–196. doi: 10.1016/s0002-9610(01)00670-5. [DOI] [PubMed] [Google Scholar]
- 3.Shaffer HA, Jr, Valenzuela G, Mittal RK. Esophageal perforation. A reassessment of the criteria for choosing medical or surgical therapy. Arch Intern Med. 1992;152:757–761. doi: 10.1001/archinte.152.4.757. [DOI] [PubMed] [Google Scholar]
- 4.Sakamoto Y, Tanaka N, Furuya T, et al. Surgical management of late esophageal perforation. Thorac Cardiovasc Surg. 1997;45:269–272. doi: 10.1055/s-2007-1013747. [DOI] [PubMed] [Google Scholar]
- 5.Saito H, Fukushima R, Kobori O, Kawano N, Muto T, Morioka Y. Marked and prolonged depression of factor XIII after esophageal resection. Surg Today. 1992;22:201–206. doi: 10.1007/BF00308823. [DOI] [PubMed] [Google Scholar]