Abstract
Liver involvement with acute myeloid leukemia (AML) is rarely reported. The majority of published cases suggest a cholestatic picture and obstructive jaundice at presentation. On the contrary, our patient presented with transaminitis without cholestasis. Elevated liver function tests persisted in our patient despite cholecystectomy; however, they normalized with chemotherapy administration, suggesting that AML was the causative effect of the hepatitis-like picture. Our review of the literature revealed that most reported cases of AML with liver involvement had short-lived remissions and an overall ominous prognosis. In our opinion, patients who have liver involvement with AML should be offered alternative investigational therapies with a low hepatic toxicity profile.
Key Words: Acute myeloid leukemia, Liver, Transaminitis
Case Report
A 66-year-old woman presented with a two-month history of progressive mid-thoracic back pain with anorexia and 10 pounds weight loss. Her exam was unrevealing. Laboratory work showed thrombocytopenia (63,000/μl), mild leukocytosis (12,400/μl), and mild transaminitis (AST and ALT were 49 and 73 U/L respectively). Hepatitis serology was negative. Review of the peripheral smear showed few circulating blasts. A bone marrow biopsy and aspirate confirmed acute myeloid leukemia (AML) with complex karyotype (deletions of chromosomes 1p, 11q and 19p along with t(8;11) translocation).
The patient developed worsening abdominal pain with rising AST and ALT. Abdominal magnetic resonance imaging (MRI) revealed an 11 mm T2 hyperintense lesion in the posterior dome of the liver with questionable stone in the neck of the gallbladder (fig. 1). Additional findings were suggestive of acute cholycystitis. While the patient underwent cholecystectomy, an intraoperative liver biopsy was performed showing hepatic infiltration with AML (fig. 2). Further studies confirmed that she had AML M0 based on the French-American-British (FAB) classification.
Fig. 1.
MRI abdomen with 11 mm nonspecific T2 hyperintense lesion in the posterior dome of the liver (arrow). Hepatosplenomegaly with smooth liver edges measuring 23 cm superior to inferior and the spleen 12.5 cm near the upper limit of normal. No changes suggestive of cirrhosis or fatty infiltration.
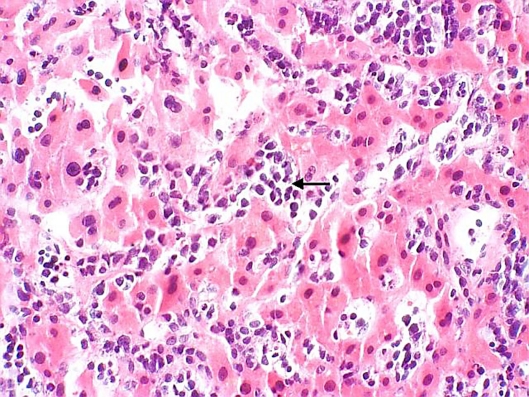
Fig. 2.
Leukemic myeloblasts infiltrating hepatic sinusoids (arrow).
The patient was treated with two induction therapy programs (classic 7 + 3 regimen then high-dose cytarabine) that finally rendered her in complete remission (CR). However, this was short-lived lasting only 8 weeks, at which point her AML recurred with hepatic infiltration. At the time of recurrence, she demonstrated worsening performance status (Eastern Cooperative Oncology Group: 3) and deconditioning with multiorgan failure justifying enrolling her in a palliative care and a hospice program. The patient died shortly thereafter.
Discussion
Liver involvement with AML is rarely reported. The majority of published cases suggest a cholestatic picture and obstructive jaundice at presentation [1, 2, 3]. On the contrary, our patient presented with transaminitis without cholestasis. Elevated liver function tests persisted in our patient despite cholecystectomy, however, they normalized with chemotherapy administration suggesting that AML was the causative effect of the hepatitis-like picture. While most reported cases suggested myelomonocytic leukemia with or without atypical eosinophils as the most commonly described AML with liver involvement [2], one other report identified a patient with AML M0 as having leukemic liver disease [3].
Reported cases are in line with our experience in this patient. Patients are usually treated with traditional AML-type programs that combine cytarabine with anthracyclines, however, remissions are short-lived and the overall prognosis is ominous. Only two case reports suggested favorable results. One case had inv (16) genomic aberration while the other had normal karyotype [1, 4]. All other reports confirm the short time from diagnosis until death.
Our case differs from other published reports in the literature in that our patient was older than most reported cases, presented with transaminitis as opposed to cholestasis, and had a subtype (AML M0) that is infrequently described in this setting. Unfortunately, our patient had the expected unfavorable outcome that others have described. In our opinion, patients who have liver involvement with AML should be offered alternative investigational therapies that have a low hepatic toxicity profile.
References
- 1.Goor Y, Goor O, Michalewitcz R, Cabili S. Acute myeloid leukemia presenting as obstructive jaundice. Jo Clin Gastroenterol. 2002;34:485–486. doi: 10.1097/00004836-200204000-00023. [DOI] [PubMed] [Google Scholar]
- 2.Rajesh G, Sadasivan S, Hiran KR, et al. Acute myeloid leukemia presenting as obstructive jaundice. Ind J Gastroenterol. 2006;25:93–94. [PubMed] [Google Scholar]
- 3.Matsueda K, Yamamoto H, Doi I. An autopsy case of granulitic sarcoma of the porta hepatis causing obstructive jaundice. J Gastroenterol. 1998;33:428–433. doi: 10.1007/s005350050108. [DOI] [PubMed] [Google Scholar]
- 4.Wandroo F, Murray J, Mutimer D, Hubscher S. Acute myeloid leukaemia presenting as cholestatic hepatitis. J Clin Pathol. 2004;57:544–545. doi: 10.1136/jcp.2003.013565. [DOI] [PMC free article] [PubMed] [Google Scholar]