Abstract
Background
Patients with poor numeracy skills may have difficulty participating in shared-decision making, affecting their utilization of colorectal cancer (CRC) screening. We explored the relationship between numeracy, provider communication, and CRC screening.
Methods
Data was from the 2007 National Cancer Institute Health Information Trends Survey. Individuals age ≥50 years responded via mail or phone to items measuring numeracy, perceptions of provider communication quality, and CRC screening. After accounting for national sampling weights, multivariate logistic regression models examined the association between these factors.
Results
1436 subjects responded to an objective numeracy item via mail, and 3286 responded to a subjective numeracy item via mail or phone; 22.6% had low objective numeracy, and 39.4% low subjective numeracy. Low subjective numeracy was associated with a lower likelihood of perceiving high quality provider communication (OR 0.63-0.73), but for low objective numeracy, the opposite was observed (OR 1.51-1.64). Low objective or subjective numeracy was associated with less CRC screening. There was significant interaction between subjective numeracy, perceptions of provider communication and CRC screening.
Conclusion
Patient numeracy is associated with perceptions of provider communication quality. For individuals with low subjective numeracy, perceiving high quality communication offset the association between low numeracy and underutilization of CRC screening.
Introduction
Colorectal cancer (CRC) is a leading cause of preventable death in the United States (Jemal et al., 2008). Despite evidence that survival is highest at early stage of disease, CRC screening rates continue to be below recommended targets ((CDC), 2006). Risk factors for underutilization of CRC screening include a lack of health insurance, being a member of a racial/ethnic minority group, having less education and/or a low income (Cairns & Viswanath, 2006; Emmons et al., 2008; Meissner, Breen, Klabunde, & Vernon, 2006; Mobley et al., 2009). The identification of risk factors that could be targeted in health promotion interventions to improve the utilization of CRC screening remains a research and clinical priority.
Low health literacy has been identified as a potential risk-factor for CRC screening underutilization. While some studies have shown an association between low health literacy and less knowledge of CRC screening issues, (Miller, Brownlee, McCoy, & Pignone, 2007; Peterson, Dwyer, Mulvaney, Dietrich, & Rothman, 2007) none have shown an association between low literacy and lower screening rates (Guerra, Dominguez, & Shea, 2005; Miller et al., 2007; Peterson et al., 2007). Numeracy, defined as difficulty with the ability to use numbers in daily life, is an important and less studied component of overall literacy; low numeracy is common in the U.S. population (Kirsch, Jungeblut, Jenkins, & Kolstad, 1993; Lipkus, Samsa, & Rimer, 2001; Rothman, Montori, Cherrington, & Pignone, 2008; Williams et al., 1995). Several studies report an association between low numeracy and poor adherence to health behaviors in patients with chronic disease (Waldrop-Valverde et al., 2009; Cavanaugh et al., 2008; Estrada, Martin-Hryniewicz, Peek, Collins, & Byrd, 2004; Osborn, Cavanaugh, Wallston, White, & Rothman, 2009). Our previous work examining the association between numeracy and CRC screening using cross-sectional data from the 2007 Health Information National Trends Survey (HINTS) (Nelson et al., 2004) suggests low numeracy is also an independent risk factor for underutilization of CRC screening (Ciampa, Osborn, Peterson, & Rothman, 2010). In that study, respondents to the HINTS survey who were 50 years of age or older with low numeracy skills had a significantly lower odds of reporting up-to-date CRC screening compared to those with higher numeracy skills, independent of other sociodemographic characteristics. To our knowledge, factors contributing to this association have not been explored.
The relationship between numeracy and the decision to undergo CRC screening is likely multifaceted and complex. While studies have consistently shown one of the strongest predictors of CRC screening is a provider's recommendation (Brenes & Paskett, 2000; Cairns & Viswanath, 2006; Friedman, Webb, & Everett, 2004; Patel, Forjuoh, Avots-Avotins, & Patel, 2004; Taylor et al., 2003; Khankari et al., 2007), little is known about how providers communicate screening information to patients and how patients receive it (Lafata, Divine, Moon, & Williams, 2006). Numeracy skills may be critical in developing an accurate assessment of risk/benefit information that is needed for adequate shared decision making (Golbeck, Ahlers-Schmidt, Paschal, & Dismuke, 2005). Low numeracy skills have been associated with an inaccurate interpretation of general health risk information (Sheridan & Pignone, 2002; Sheridan, Pignone, & Lewis, 2003), as well as inaccurate perception of the risk of developing breast and colon cancer (Davids, Schapira, McAuliffe, & Nattinger, 2004; Donelle, Arocha, & Hoffman-Goetz, 2008). Low numeracy has also been associated with overestimating how much mammography reduces breast cancer risk (Schwartz, Woloshin, Black, & Welch, 1997). It is not yet clear from the literature how misperception of screening risks and benefits impact the screening behavior of those with low numeracy, how individuals with low numeracy perceive the quality of provider communication or how the complex interaction between numeracy and the communication of risk/benefit information might also impact health screening behavior.
Our study objective was to examine the relationship between numeracy and perceptions of provider communication. We predicted that individuals with low numeracy have important communication preferences and needs different from individuals with high numeracy, and perceptions of provider communication would moderate the association between numeracy and CRC screening utilization.
Methods
Data Source
The 2007 Health Information National Trends Survey (HINTS) is a nationally representative survey designed to explore the American public's cancer-related knowledge, attitudes and behavior. The conceptualization, design and implementation of the survey has been described previously (Nelson et al., 2004). HINTS 2007 used a dual-frame, mixed-mode (telephone and mail) collection strategy to maximize response rate. Trained interviewers conducted phone interviews using random digit dialing (RDD); additionally mail surveys were sent using addresses from a United States Postal Service list (USPS). The completed surveys were transformed via a composite estimator into a nationally representative sample. The overall response rate was 24.2% (n=4,092) for the telephone sample and 31.0% (n=3,582) for the mail sample. Each phone and mail respondent was assigned a sampling weight and 50 replicate weights; these weights were then combined to generate a composite weight with 50 replicates for computation of nationally representative data adjusted for non-response.
Study Population
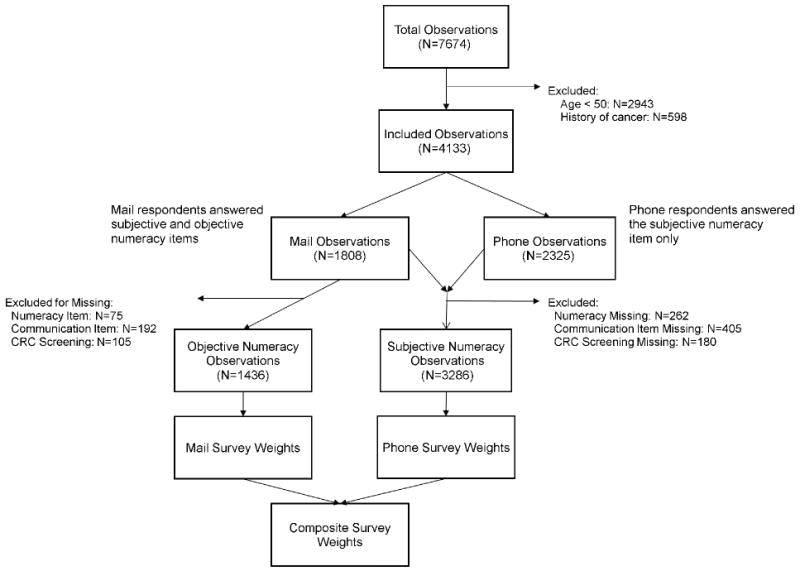
For the purposes of our analyses, we included telephone and mail respondents of the 2007 HINTS who were 50 years of age or older. Exclusion criteria was self-reported history of cancer other than non-melanoma skin cancer, and missing data for the numeracy, communication or CRC cancer screening survey items (Figure 1).
Figure 1. Eligibility criteria and sample sizes.
Measures
Demographic information included self-reported age, gender, race/ethnicity, annual income, education and health insurance status, and served as covariates in our analyses. Race, education, income, and insurance status were recorded as categorical variables.
Numeracy was measured with two items adapted from previously developed scales. The first item (Woloshin, Schwartz, & Welch, 2005) asked respondents to rate “In general, how easy or hard do you find it to understand medical statistics?” on a four-point Likert scale. This measure of subjective numeracy and was dichotomized a priori to “very easy/easy” or “hard/very hard” for the purpose of this analysis. All respondents to the HINTS survey were asked to answer this item (telephone and mail). Only mail respondents were also asked a second item (Lipkus et al., 2001), which asks respondents to answer the following question: “Which of the following numbers represents the biggest risk of getting a disease: 1 in 100, 1 in 1000 or 1 in 10?” This measure of objective numeracy was coded as correct or incorrect.
Perception of provider communication was measured with four discrete items that were original to HINTS 2007. They were: (1) “During the past 12 months, how often did doctors, nurses, or other health professionals give you the chance to ask all the health-related questions you had?” (health questions), (2) “How often did doctors, nurses, or other health professionals give the attention you needed to your feelings and emotions?” (attention to emotion), (3) “How often did they involve you in decisions about your health care as much as you wanted?” (involved in decisions), (4) “How often did they make sure you understood the things you needed to do to take care of your health?” (ensured understanding). Response options were on a 4-point Likert scale ranging from “never” to “always.” Scores were dichotomized a priori to “not always” vs. “always” for the purpose of analysis.
Ascertainment of CRC screening status (up-to-date or not) was by respondent self-report of a colonoscopy within the past 10 years, a sigmoidoscopy within 5 years, or a fecal-occult blood test within the past year, consistent with screening guidelines at the time of the study (“Screening for colorectal cancer: recommendation and rationale,” 2002). CRC-related tests were only counted as screening tests if they were reported to be part of a routine preventive exam. Tests done to diagnose problems were not counted as screening.
Data Analysis
Demographics were reported as unweighted sample sizes, and weighted means or proportions adjusted for composite national sample weights. Pearson's chi-square tests examined the association between race, education, income, and insurance status stratified by subjective and objective numeracy categories, and separately to examine differences in sociodemographic characteristics for mail versus phone sampling approaches. Independent samples t-tests examined mean age differences stratified by subjective and objective numeracy categories. Kendall-tau rank correlations examining the association between subjective numeracy and objective numeracy was poor (tau-b = 0.09, p < 0.001), and objective and subjective numeracy were therefore analyzed separately (Ciampa et al., 2010).
Univariate logistic regression models and multivariate logistic regression models adjusted for the aforementioned demographic factors examined the association between numeracy and each perception of provider communication item separately for both subjective and objective numeracy. A third multivariate model included an adjustment for sampling approach (mail vs phone) for analyses using subjective numeracy only. A separate multivariate logistic regression model was constructed to test for effect modification of each communication item on the association between numeracy and CRC screening utilization. Each model was stratified by communication item response and included an interaction term for numeracy and each communication item. Responses of “don't know” or “refused” were coded as missing. All analyses were conducted using STATA statistical software package (STATAcorp, Release 10. College Station, TX) using weighted data and replicate weights to perform a jackknife estimation of variance. Composite weights were used in all analyses involving subjective numeracy and mail sample weights were used in all analyses involving objective numeracy.
Results
Out of 7,674 respondents available for analysis, 4,133 met inclusion criteria (age 50 or older and no history of cancer). For subjective numeracy, data from 3,286 respondents were analyzed after 847 (20.5%) were excluded because of missing data. For objective numeracy, data from 1,436 respondents were analyzed after 372 (20.6%) were excluded because of missing data. Figure 1 summarizes eligibility criteria and sample sizes according to missing data.
The association between respondent demographics and subjective and objective numeracy categories are summarized in Table 1. The mean age was 63.3 years, 45.9% were male, and 78.3% were White. Almost half (48.2%) had a high-school education or less and 25.0% reported annual incomes of less than $20,000. The majority (92.6%) had health insurance.
Table 1. Demographics of Study Sample.
Unweighted Sample Size (N), Weighted Percentages, and 95% Confidence Intervals.
| Respondent Characteristic | Total Sample (N = 3286) | ||
|---|---|---|---|
| N | Weighted Mean or Percentage | 95% CI | |
| Mean Age | 63.3 | 62.8-63.7 | |
| Gender, % | |||
| Male | 1286 | 45.9 | 43.8-48.1 |
| Race/Ethnicity, % | |||
| White, Non-Hispanic | 2607 | 78.3 | 76.2-80.2 |
| Black, Non-Hispanic | 290 | 10.8 | 9.4-12.3 |
| Hispanic | 164 | 6.6 | 5.5-7.9 |
| Other† | 142 | 4.4 | 3.4-5.7 |
| Education, % | |||
| ≥ College grad | 1139 | 26.4 | 24.8-28.2 |
| Some college | 780 | 25.3 | 23.5-27.2 |
| ≤ HS grad | 1329 | 48.2 | 46.1-50.4 |
| Income, % | |||
| > $75K | 844 | 27.6 | 25.7-29.6 |
| $50K-$75K | 550 | 18.3 | 16.6-20.1 |
| $20K-$49K | 893 | 29.1 | 27.2-31.2 |
| < $20K | 791 | 25.0 | 23.1-26.9 |
| Insurance, % | |||
| Has Insurance | 3045 | 92.6 | 90.9-94.0 |
Other includes Asian American, Native American, Pacific Islander, Native Hawaiian and multiple races.
Overall 39.4% of the sample answered “hard” or “very hard” on the subjective numeracy item and were classified as having low subjective numeracy. Nearly one fourth (22.6%) of respondents answered the objective numeracy item incorrectly and were classified as having low objective numeracy. Low subjective and objective numeracy were significantly associated with older age, non-White race, less educational attainment, and lower annual income. Respondents from the mail sub-sample who answered the objective numeracy question were more likely to report higher incomes than those of the total, composite sample; otherwise there were no significant differences in demographic characteristics between respondents that answered the subjective vs. objective numeracy item. There was a trend towards mail sub-sample respondents having higher subjective numeracy than phone sub-sample respondents (p=0.07).
Each of the perception of provider communication item responses were skewed towards a response of “always” in the total sample: 60% respondents reported always having the opportunity to ask all the health related questions they had, 46% reported their provider always paid enough attention to their feelings and emotions, 54% said their provider always involved them in decisions as much as they would like and 63% reported their provider always checked to make sure they understood the things they needed to do to take care of their health.
Multivariate logistic regression models examining the relationship between numeracy and perception of provider communication items are summarized in Table 2. In unadjusted analysis, low subjective numeracy was significantly associated with lower rates of reporting “always” for each communication item (OR 0.64-0.78). In a separate, unadjusted analysis, low objective numeracy was significantly associated with higher rates or reporting “always” for each communication item (OR 1.47-1.79). These associations persisted in the adjusted analysis for both low subjective numeracy (OR 0.62-0.72) and low objective numeracy (OR 1.54-1.71).
Table 2. The Influence of Numeracy on the Perception of Patient-Provider Communication.
| Communication Item Response | Weighted % | OR, Adjusted† (95% CI) |
|---|---|---|
| Subjective Numeracy | ||
| Provider Always Allows Health Questions | 60.1 | |
| High Numeracy | 63.9 | Referent |
| Low Numeracy | 54.5 | 0.62 (0.50-0.77)* |
| Provider Always Pays Attention to Emotion | 46.3 | |
| High Numeracy | 48.6 | Referent |
| Low Numeracy | 42.7 | 0.72 (0.57-0.91)** |
| Provider Always Involves Patient in Decisions | 54.2 | |
| High Numeracy | 58.6 | Referent |
| Low Numeracy | 47.3 | 0.65 (0.54-0.78)* |
| Provider Always Ensures Understanding | 62.8 | |
| High Numeracy | 66.0 | Referent |
| Low Numeracy | 57.8 | 0.64 (0.49-0.82)* |
| Objective Numeracy | ||
| Provider Always Allows Health Questions | 59.5 | |
| High Numeracy | 57.5 | Referent |
| Low Numeracy | 66.6 | 1.69 (1.07-2.68)** |
| Provider Always Pays Attention to Emotion | 43.5 | |
| High Numeracy | 40.2 | Referent |
| Low Numeracy | 54.6 | 1.71 (1.22-2.40)** |
| Provider Always Involves Patient in Decisions | 49.6 | |
| High Numeracy | 46.9 | Referent |
| Low Numeracy | 58.9 | 1.70 (1.13-2.56)** |
| Provider Always Ensures Understanding | 56.2 | |
| High Numeracy | 54.0 | Referent |
| Low Numeracy | 64.5 | 1.54 (1.04-2.30)** |
Adjusted for Age, Gender, Race, Income, Education and Health Insurance
p < 0.001
p < 0.05
In the adjusted model, demographic characteristics were not significantly associated with the communication items. An additional adjustment for sampling approach did not impact the association between subjective numeracy and perceptions of provider communication (not shown).
In unadjusted analyses, responses of “always” for perception of provider communication items were associated with higher CRC screening utilization for each item: health questions (OR 1.30, p = 0.004), attention to emotion (OR 1.20, p = 0.04), involved with decisions (OR 1.30, p = 0.003) and ensured understanding (OR 1.33, p = 0.002). Younger age, female gender, and an annual income of below $35k were significantly associated with a lower odds of reporting an up-to-date CRC screening test.
There were statistically significant interactions among subjective numeracy (hard/very hard vs. easy/very easy) and the communication items related to the perception that patients had a chance to ask providers questions (health questions) and the perception that providers paid attention to patient's emotions (attention to emotion) on CRC screening utilization (Table 3). The interaction between the health questions and attention to emotion items and subjective numeracy was such that a response of “always” for those two items offset the previously observed association between low subjective numeracy and less reported CRC screening. There were no statistically significant interactions among subjective numeracy and the communication items related to the perception that patients were involved in medical decisions (involved decisions) or that providers ensured understanding of medical issues (ensured understanding) on CRC screening. There was also no significant interaction between objective numeracy and any of the communication items on CRC screening utilization.
Table 3. Effect of Perception of Patient-Provider Communication on the Association between Numeracy and CRC Screening (OR, Adjusted†, 95% CI and p-values for interaction between numeracy and communication).
| CRC Screening (Weighted % Reported) | Communication Item | |||||||
|---|---|---|---|---|---|---|---|---|
| Item 1 Responsea | Item 2 Responseb | Item 3 Responsec | Item 4 Responsed | |||||
| Always | Not Always | Always | Not Always | Always | Not Always | Always | Not Always | |
| CRC Screening Up-to-Date (51.3) | NA | NA | NA | NA | NA | NA | NA | NA |
| High Subjective Numeracy (53.4) | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Low Subjective Numeracy (47.8) | 1.01 (0.78-1.31) | 0.71 (0.53-0.95)* | 1.14 (0.85-1.51) | 0.67 (0.52-0.87)* | 1.0 (0.77-1.30) | 0.72 (0.54-0.95)* | 0.51 (0.31-0.83)* | 0.68 (0.38-1.19) |
| p-value, interaction | 0.03 | 0.01 | 0.13 | 0.28 | ||||
| CRC Screening Up-to-Date (55.6) | NA | NA | NA | NA | NA | NA | NA | NA |
| High Objective Numeracy (58.5) | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Low Objective Numeracy (45.7) | 0.52 (0.30-0.89)* | 0.68 (0.35-1.35) | 0.51 (0.24-1.10) | 0.66 (0.36-1.21) | 0.55 (0.30-0.99)* | 0.63 (0.35-1.16) | 0.51 (0.28-0.92)* | 0.65 (0.33-1.27) |
| p-value, interaction | 0.31 | 0.18 | 0.16 | 0.17 | ||||
Item 1: How often did doctors, nurses or other health professionals give you the chance to ask all the health-related questions you had?
Item 2: How often did doctors, nurses or other health professionals give the attention you needed to your feelings and emotions?
Item 3: How often did they involve you in decisions as much as you wanted?
Item 4: How often did they make sure you understood the things you needed to do to take care of your health?
Adjusted for Age, Gender, Race, Income, Education and Health Insurance
p< 0.05
Discussion
In this study of nationally representative data, low subjective numeracy was associated with perceiving low quality provider communication. Surprisingly this association was in the reverse direction for objective numeracy. Low subjective numeracy reduced the odds of a respondent reporting their communication needs were always met by their provider by 28-38%, while respondents with low objective numeracy had higher odds of reporting their communication needs were met. Additionally this study suggests that positive patient perceptions of some elements of provider communication quality may interact with subjective numeracy skills and offset the association observed between low subjective numeracy and less CRC screening.
There are several possible explanations for the disparate observations for subjective and objective numeracy. In this study, subjective and objective numeracy behaved as separate constructs, underscoring the discrepancy between confidence in numeracy skills and actual ability. The weak correlation between subjective and objective numeracy in this sample suggests individuals may have a distorted understanding of their own ability to understand and use numbers. This observation is supported by other's work that has shown that the correlation between subjective and objective numeracy is modest at best (Fagerlin, et al., 2007; Woloshin, Schwartz, & Welch, 2005). Individuals with low numeracy confidence may have different communication needs and/or make medical decisions in ways that differ from their peers with higher confidence. Individuals with higher objective numeracy may also have higher expectations that a health care provider engage them sufficiently to make their own care decisions and thus are more critical of the provider's communication skills. Lastly, these effects could be the results of limitations to the study design either from misclassification of numeracy, the highly subjective nature of the communication items, or through unmeasured confounders.
Many models of health behavior conceptualize the decision to pursue health screening as a personal analysis of perceived risks, benefits and barriers. Numeracy skills may be critical for understanding risk/benefit information which is needed for informed decision-making. Studies have shown that individuals with poor numeracy skills may misinterpret the risk/benefit ratio for cancer screening (Davids, et al., 2004; Donelle, et al., 2008; Schwartz, et al., 1997; Sheridan & Pignone, 2002; Sheridan, et al., 2003). Other work suggests individuals with low numeracy rely more on anecdotal information such as the experiences and advice of family and friends than on provider recommendations when making decisions (Fagerlin, Wang, & Ubel, 2005). The ability to follow through with screening itself depends on several numeracy dependent tasks (e.g. scheduling a follow-up appointment, taking the colonic preparation properly) and thus poses a challenge for individuals with low numeracy skills. We were unable to explore these issues in this study; future research is needed to address these important relationships.
There are other limitations to acknowledge. The cross-sectional design of the study does not allow us to make causal conclusions and leaves open the possibility that our observations are the result of unmeasured confounding variables. In particular, we did not have measures of respondent health literacy, depression or cognitive dysfunction that may each be associated with numeracy, subjective communication responses, and the ability to not only recall but also complete CRC screening. Even though the objective and subjective numeracy items were adapted from previously developed scales, they have not been validated as single item measures of numeracy. Measurement of perceptions of provider communication and CRC screening are subject to recall bias. The mixed-mode sample design of HINTS introduces the possibility of selection bias. The phone survey was in both English and Spanish whereas the mailed survey was in English only. The possibility of a social desirability effect in the phone sample or a mail respondent seeking help on the objective numeracy item are other potential sources of bias. However, adjusting for sampling approach in the regression models involving subjective numeracy did not alter our findings; the inability to similarly adjust for potential bias from sampling approach in the objective numeracy analyses is a limitation of the study.
As the model for clinical decision-making has shifted from a physician driven to a shared decision-making process, there is an increasing need for patients to take an active role in their own healthcare (Peters, Hibbard, Slovic, & Dieckmann, 2007). The success of the shared-decision model requires an activated, informed patient that is able to understand the information provided by their health provider and apply it in order to make a decision that reflects their own values (Charles, Gafni, & Whelan, 1997). The ability to understand risk and benefit information is vital to this process, especially in situations where there are multiple treatment options. Adequate numeracy skills are important to the process of making a shared decision. However not all patients have the same ability to participate fully in this process, and thus the success of this shared decision model also depends in part on the ability of the provider to communicate with the patient in a way that is consistent with the patient's capacity and preference to receive the information necessary to make a truly informed decision. By assisting patients of all numeracy skills make truly informed decisions, effective health communication may offset some of the observed disparities in CRC screening and serve as a target for future interventions designed to improve care for patients.
Acknowledgments
Dr. Ciampa is currently supported by the Veteran's Affairs Quality Scholars Fellowship Program. Dr. Osborn is currently supported by a Diversity Supplement Award (NIDDK P60 DK020593). Dr. Peterson is currently supported by an NCI Career Development Award (NCI 5K07 CA122827). Dr. Rothman is currently supported by an NIDDK Career Development Award (NIDDK 5K23 DK065294).
References
- (CDC) C. f. D. C. a. P. Increased use of colorectal cancer tests-United States, 2002 and 2004. MMWR Morb Mortal Wkly Rep. 2006;55(11):308–311. [PubMed] [Google Scholar]
- Brenes GA, Paskett ED. Predictors of stage of adoption for colorectal cancer screening. Prev Med. 2000;31(4):410–416. doi: 10.1006/pmed.2000.0729. [DOI] [PubMed] [Google Scholar]
- Cairns CP, Viswanath K. Communication and colorectal cancer screening among the uninsured: data from the Health Information National Trends Survey (United States) Cancer Causes Control. 2006;17(9):1115–1125. doi: 10.1007/s10552-006-0046-2. [DOI] [PubMed] [Google Scholar]
- Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- Ciampa PJ, Osborn CY, Peterson NB, Rothman RL. Association of Numeracy and Colorectal Cancer Screening Utilization. Paper presented at the Society of General Internal Medicine; Minneapolis, MN. 2010. [Google Scholar]
- Davids SL, Schapira MM, McAuliffe TL, Nattinger AB. Predictors of pessimistic breast cancer risk perceptions in a primary care population. J Gen Intern Med. 2004;19(4):310–315. doi: 10.1111/j.1525-1497.2004.20801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donelle L, Arocha JF, Hoffman-Goetz L. Health literacy and numeracy: key factors in cancer risk comprehension. Chronic Dis Can. 2008;29(1):1–8. [PubMed] [Google Scholar]
- Emmons K, Puleo E, McNeill LH, Bennett G, Chan S, Syngal S. Colorectal cancer screening awareness and intentions among low income, sociodemographically diverse adults under age 50. Cancer Causes Control. 2008;19(10):1031–1041. doi: 10.1007/s10552-008-9167-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada CA, Martin-Hryniewicz M, Peek BT, Collins C, Byrd JC. Literacy and numeracy skills and anticoagulation control. Am J Med Sci. 2004;328(2):88–93. doi: 10.1097/00000441-200408000-00004. [DOI] [PubMed] [Google Scholar]
- Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people's health care decisions: is a picture worth a thousand statistics? Med Decis Making. 2005;25(4):398–405. doi: 10.1177/0272989X05278931. [DOI] [PubMed] [Google Scholar]
- Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- Friedman LC, Webb JA, Everett TE. Psychosocial and medical predictors of colorectal cancer screening among low-income medical outpatients. J Cancer Educ. 2004;19(3):180–186. doi: 10.1207/s15430154jce1903_14. [DOI] [PubMed] [Google Scholar]
- Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. Am J Prev Med. 2005;29(4):375–376. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Guerra CE, Dominguez F, Shea JA. Literacy and knowledge, attitudes, and behavior about colorectal cancer screening. J Health Commun. 2005;10(7):651–663. doi: 10.1080/10810730500267720. [DOI] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- Khankari K, Eder M, Osborn CY, et al. Improving colorectal cancer screening among the medically underserved: a pilot study within a federally qualified health center. J Gen Intern Med. 2007;22:1410–1414. doi: 10.1007/s11606-007-0295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: a first look at the results of the National Adult Literacy Survey (NCES 93275) Washington, DC: US Department of Education; 1993. [Google Scholar]
- Lafata JE, Divine G, Moon C, Williams LK. Patient-physician colorectal cancer screening discussions and screening use. Am J Prev Med. 2006;31(3):202–209. doi: 10.1016/j.amepre.2006.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21(1):37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2006;15(2):389–394. doi: 10.1158/1055-9965.EPI-05-0678. [DOI] [PubMed] [Google Scholar]
- Miller DP, Jr, Brownlee CD, McCoy TP, Pignone MP. The effect of health literacy on knowledge and receipt of colorectal cancer screening: a survey study. BMC Fam Pract. 2007;8:16. doi: 10.1186/1471-2296-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobley L, Kuo TM, Urato M, Boos J, Lozano-Gracia N, Anselin L. Predictors of endoscopic colorectal cancer screening over time in 11 states. Cancer Causes Control. 21(3):445–461. doi: 10.1007/s10552-009-9476-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–460. doi: 10.1080/10810730490504233. discussion 481-444. [DOI] [PubMed] [Google Scholar]
- Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. 2009;32(9):1614–1619. doi: 10.2337/dc09-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P, Forjuoh SN, Avots-Avotins A, Patel T. Identifying opportunities for improved colorectal cancer screening in primary care. Prev Med. 2004;39(2):239–246. doi: 10.1016/j.ypmed.2004.03.026. [DOI] [PubMed] [Google Scholar]
- Peters E, Hibbard J, Slovic P, Dieckmann N. Numeracy skill and the communication, comprehension, and use of risk-benefit information. Health Aff (Millwood) 2007;26(3):741–748. doi: 10.1377/hlthaff.26.3.741. [DOI] [PubMed] [Google Scholar]
- Peterson NB, Dwyer KA, Mulvaney SA, Dietrich MS, Rothman RL. The influence of health literacy on colorectal cancer screening knowledge, beliefs and behavior. J Natl Med Assoc. 2007;99(10):1105–1112. [PMC free article] [PubMed] [Google Scholar]
- Rothman RL, Montori VM, Cherrington A, Pignone MP. Perspective: the role of numeracy in health care. J Health Commun. 2008;13(6):583–595. doi: 10.1080/10810730802281791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127(11):966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- Screening for colorectal cancer: recommendation and rationale. Ann Intern Med. 2002;137(2):129–131. doi: 10.7326/0003-4819-137-2-200207160-00014. [DOI] [PubMed] [Google Scholar]
- Sewitch MJ, Fournier C, Dawes M, Yaffe M, Snell L, Roper M, et al. Do physician recommendations for colorectal cancer screening differ by patient age? Can J Gastroenterol. 2007;21(7):435–438. doi: 10.1155/2007/938978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan SL, Pignone M. Numeracy and the medical student's ability to interpret data. Eff Clin Pract. 2002;5(1):35–40. [PubMed] [Google Scholar]
- Sheridan SL, Pignone MP, Lewis CL. A randomized comparison of patients' understanding of number needed to treat and other common risk reduction formats. J Gen Intern Med. 2003;18(11):884–892. doi: 10.1046/j.1525-1497.2003.21102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor V, Lessler D, Mertens K, Tu SP, Hart A, Chan N, et al. Colorectal cancer screening among African Americans: the importance of physician recommendation. J Natl Med Assoc. 2003;95(9):806–812. [PMC free article] [PubMed] [Google Scholar]
- Waldrop-Valverde D, Osborn CY, Rodriguez A, et al. Numeracy Skills Explain Racial Differences in HIV Medication Management. AIDS Behav. 2009 doi: 10.1007/s10461-009-9604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274(21):1677–1682. [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM, Welch HG. Patients and medical statistics. Interest, confidence, and ability. J Gen Intern Med. 2005;20(11):996–1000. doi: 10.1111/j.1525-1497.2005.00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye J, Xu Z, Aladesanmi O. Provider recommendation for colorectal cancer screening: examining the role of patients' socioeconomic status and health insurance. Cancer Epidemiol. 2009;33(3-4):207–211. doi: 10.1016/j.canep.2009.07.011. [DOI] [PubMed] [Google Scholar]


