Abstract
Background
Studies have shown that steroids can improve kidney survival and decrease the risk of proteinuria in patients with Immunoglobulin A nephropathy, but the overall benefit of steroids in the treatment of Immunoglobulin A nephropathy remains controversial. The aim of this study was to evaluate the benefits and risks of steroids for renal survival in adults with Immunoglobulin A nephropathy.
Methodology and Principal Findings
We searched the Cochrane Renal Group Specialized Register, Cochrane Controlled Trial Registry, MEDLINE and EMBASE databases. All eligible studies were measuring at least one of the following outcomes: end-stage renal failure, doubling of serum creatinine and urinary protein excretion. Fifteen relevant trials (n = 1542) that met our inclusion criteria were identified. In a pooled analysis, steroid therapy was associated with statistically significant reduction of the risk in end-stage renal failure (RR: 0.46, 95% CI: 0.27 to 0.79), doubling of serum creatinine (RR = 0.34, 95%CI = 0.15 to 0.77) and reduced urinary protein excretion (MD = −0.47g/day, 95%CI = −0.64 to −0.31).
Conclusions/Significance
We identified that steroid therapy was associated with a decrease of proteinuria and with a statistically significant reduction of the risk in end-stage renal failure. Moreover, subgroup analysis also suggested that long-term steroid therapy had a higher efficiency than standard and short term therapy.
Introduction
Immunoglobulin A (IgA) nephropathy or Berger's disease is the most common form of primary glomerulonephritis worldwide [1]–[5]. It is one of the major factors leading to end stage renal failure. About 15–20% of patients with apparent onset IgA nephropathy will develop end stage renal failure within 10 years, and 30–40% within 20 years [6]–[8]. The disease is characterized by accumulation of polymeric IgA1-containing complexes in the mesangial areas [9], [10]. IgA nephropathy can occur at all ages, but most commonly in the second and third decades of life, with a male gender preference [11]. Episodic macroscopic hematuria has been reported as the most common clinical manifestation (40–50% of cases) of IgA nephropathy patients, especially in the second and third decades of life [12]. It has also been found that <5% cases were complicated by upper respiratory infection or acute kidney injury (AKI), the most often in the elderly [13], [14].
Only in recent years has the pathogenetic mechanism underlying IgA nephropathy been found, which can be divided into three essential steps: i) generation of abnormal IgA1 and formation of IgA1 complexes; ii) generation of mesangial injury mediated by interaction of IgA1 complexes with mesangial IgA receptors, and iii) progression of IgA-mediated mesangial injury towards renal failure [15], [16]. Moreover, IgA nephropathy is highly variable both clinically and pathologically [11], [16]. The clinical features ranged from asymptomatic hematuria to rapid progressive glomerulonephritis (RPGN) [14]. IgA nephropathy is most often associated with microscopic hematuria or recurrent macroscopic hematuria, and spontaneously resolving acute renal failure can also occur; this condition can sometimes lead to chronic kidney disease as well [13], [17]. Pathologically, a spectrum of glomerular lesions can be seen, and mesangial proliferation with prominent IgA deposition can be observed in almost all biopsies [10], [18].
The goal of treatment for IgA nephropathy is to prevent sequelae. At the beginning of 1980s, corticosteroid treatment was firstly proposed for paediatric patients with IgAN and nephritic syndrome, which was generally seen as predictive of progressive renal insufficiency [16]. However, recent Cochrane systematic review failed to show the benefit of such treatment for adults, which only demonstrated the benefits and risks of steroids in renal survival in children with IgA nephropathy [19]. Another important review provided an unclear conclusion because it included trials with low quality [20]. Several clinical trials have been completed recently [21], [22], which demonstrated both the benefits and risks of steroids in renal survival in adults with IgA nephropathy.
We performed a systematic review and meta-analysis including the most updated evidence in the effects of steroid therapy on end-stage renal failure, doubling of serum creatinine, urinary protein excretion, and possible side-effects in patients with IgA nephropathy.
Methods
Search Strategy
We systematically searched the English literature to identify all relevant, randomized, double-blind, placebo-controlled trials regardless of publication status (published, unpublished, in press, and in progress), and to examine the effects of steroids on IgA nephropathy. Relevant trials were identified with the following procedure:
Electronic Searches: We searched the electronic databases MEDLINE, EMBASE, Cochrane Renal Group Specialized Register and Cochrane Controlled Trial Registry for relevant trials to a time limit of Apr. 10, 2010 using “Steroids” and “IgA nephropathy” as the search terms.
Other sources: We contacted authors to obtain any possible additional published or unpublished data and we searched the proceedings of the annual meeting in the Cochrane Renal Group Specialized Register. In addition, we searched for ongoing RCTs in the metaRegister of controlled trials using the search terms “Steroids” and “IgA nephropathy” as the above statement.
Study Selection
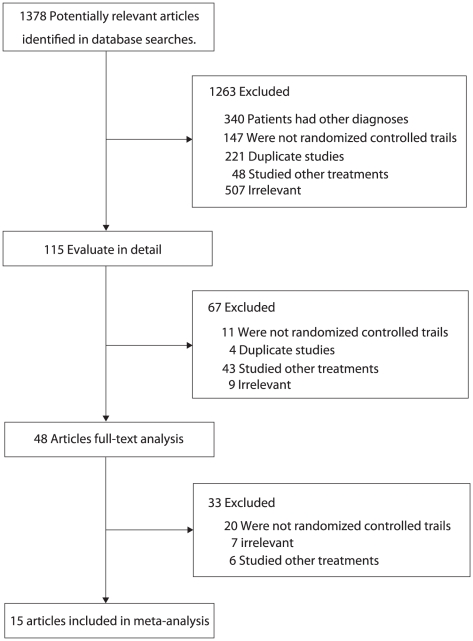
Two authors (Shi-Lei. Guo, Chun-Fang. Wu) screened the primary searching results to identify any relevant trials that required further retrieval (full text or abstract), and then they independently reviewed these studies, looking for trials that met the inclusion criteria (Figure 1). The inclusion criteria were broad so that it would be possible to include all evidence now existing, regardless of the study language, study quality, sample size and other factors. The included studies were randomized controlled trials or quasi-randomized controlled trials and any type of treatment with steroids (methylprednisolone or prednisolone) was compared to treatments without steroids.
Figure 1. Flow diagram showing the number of citations identified, retrieved and included in final analysis.
Data extraction
Data extraction was performed by two reviewers (Shi-Lei. Guo, Chun-Fang. Wu) independently using a standardized extraction form. If there was any disagreement between the two reviewers, it would be settled by discussion with a third reviewer (Yu-Hao. Zhou) until a consensus was reached.
Data were extracted from the included trials in terms of patients' characteristic, doses and modalities of treatment, methodological characteristics of the trials. The primary reported outcomes were summarized in tables. One author (Yu-Hao Zhou) entered the data into computer, and three other authors (Jia-Jie. Zang, Chun-Fang. Wu, and Jin-Fang. Xu) checked it.
Assessment of Methodological Quality
The quality of the trials was assessed according to the pre-fixed, including allocation concealment, blinding, Intention-to-treat analysis, and completeness of follow-up. Judgments regarding the presence of methodological biases were made according to Cochrane criteria guidelines [23]. Any disagreement among the three authors (Shi-Lei. Guo, Chun-Fang. Wu, and Jin-Fang. Xu) was settled by discussion with a fourth author (Yu-Hao. Zhou) until a consensus was reached.
Data Analysis
The effect of steroids on renal survival was evaluated in terms of incidence of end stage renal failure, doubling of serum creatinine and urinary protein excretion [24]–[26]. We used relative risk (RR) with 95% confidence intervals (CIs) for binary data and mean difference (MD) with 95% confidence intervals (CIs) for continuous data. We also did subgroup analysis to assess potential effect change for all results based on the type of control drug and duration of treatment. All estimates of effect were derived using a random-effects model with Mantel-Haenszel Statistics. Heterogeneity of treatment effects between studies was investigated visually by scatter plot and statistically by the heterogeneity statistic. When the
statistic. When the statistic was 0% to 40%, it indicates that heterogeneity is unimportant, 30% to 60% indicates moderate, 50% to 90% indicates substantial and 75% to 100% indicates considerable heterogeneity [27]. The P value is from the
statistic was 0% to 40%, it indicates that heterogeneity is unimportant, 30% to 60% indicates moderate, 50% to 90% indicates substantial and 75% to 100% indicates considerable heterogeneity [27]. The P value is from the  test. All the reported P values are two-sided and values of P<0.05 was regarded as statistically significant for all included studies. All analyses were calculated using STATA (version 10.0).
test. All the reported P values are two-sided and values of P<0.05 was regarded as statistically significant for all included studies. All analyses were calculated using STATA (version 10.0).
Results
We identified 1,378 articles from our initial electronic search, of which 1,263 were excluded during an initial review (title and abstract), we retrieved the full text for the remained 115 articles, and 15 clinical trials met the inclusion criteria (Figure 1): they contributed to the study of 1,542 patients with IgA nephropathy in this systematic review and meta-analysis. Table 1 summarized the characteristic of these studies and the important baseline information of the included patients. The follow-up for patients ranged from 3 to 281 months, and the number of patients included in every study ranged from 20 to 702. Of these studies, two trials [28], [31] compared steroids with anti-platelet drugs. Five trials [29], [32], [33], [35], [37] compared steroids with anti-inflammatory drugs and/or anti-thromboyte. Six trials [21], [22], [30], [34], [39], [40] compared steroids with supportive treatment. Placebo was compared with steroids in one trial [36] and only one trial [38] gave no treatment for the control group. In addition, three trials [34], [36], [38] investigated short-term steroid therapy, five trials [21], [22], [30], [32], [40] investigated standard-term steroid therapy and remaining seven trials [28], [29], [31], [33], [35], [37], [39] investigated long-term steroid therapy. Some of the included studies keep low-quality because many trials have design limitations. Table 2 shows the detailed quality of included individual trials.
Table 1. Characteristic of the included studies.
| Source | Population | No. of Patients | Interventions | Baseline renal function and/or proteinuria | Follow up (month) |
| Katafuchi R 2008 [28] | Been biopsied with primary IgA nephropathy | 702 | (1) Methylprednisolone 1 g/day 3 days plus Prednisolone 30 mg/day 3 days plus Prednisolone 30 mg/day 2 years(2) Prednisolone 60 mg/day 2 years(2) Prednisolone 60 mg/day 4 weeks and then tapered off within 1 year, Prednisolone 20 mg or 30 mg/day 4 weeks and then tapered off within 1 year, Prednisolone 20 mg or 30 mg/day 1 month and Prednisolone was tapered and maintained for at least 2 years(3) Anti-platelet agent or with no medication 1 month and Prednisolone was tapered and maintained for at least 2 years(3) Anti-platelet agent or with no medication |
Serum creatinine(0.98 0.58 mg/dl) 0.58 mg/dl) |
62 |
| Koike M 2008[29] | Light microscopic findings | 48 | (1) Prednisolone was 0.4 mg/kgBW/day (20–30 mg/day)  4 weeks, then reduced to 10–20 mg on alternate days 4 weeks, then reduced to 10–20 mg on alternate days 12 months and 5–10 mg on alternate days for a subsequent year(2) dipyridamole or zilazep hydrochloride 150 or 300 mg/day 12 months and 5–10 mg on alternate days for a subsequent year(2) dipyridamole or zilazep hydrochloride 150 or 300 mg/day |
Steroid group serum creatinine was 0.92 0.26 mg/dl and non-steroid group was 1.15 0.26 mg/dl and non-steroid group was 1.15 0.35 mg/dl 0.35 mg/dl |
24 |
| Pozzi C 2004[30] | Biopsy-proven Ig A nephropathy | 86 | (1) Methylprednisolone 1 g/day 3 days and again 2 and 4 months later, other day oral prednisolone 0.5 mg/kg 3 days and again 2 and 4 months later, other day oral prednisolone 0.5 mg/kg 6 months(2) Supportive treatment 6 months(2) Supportive treatment |
Urinary protein excretion levels of 1–3.5 g/d | 120 |
| Moriyama T 2004[31] | Been diagnosed based on light-microscopic findings | 60 | (1) Prednisolone 0.8 mg/kg/day 4 weeks, then reduced to 20–30 mg on alternate days 4 weeks, then reduced to 20–30 mg on alternate days 12 months and 20 mg on alternate days 12 months and 20 mg on alternate days 12 months(2) Anti-platelet agent 12 months(2) Anti-platelet agent |
Steroid group serum creatinine was 1.21 0.44 mg/dl and non-steroid group was 1.27 0.44 mg/dl and non-steroid group was 1.27 0.33 mg/dl 0.33 mg/dl |
54.6 |
| Katafuchi R 2003[32] | Biopsy-proven new Ig A nephropathy | 103 | (1) Prednisolone 20 mg/day 1 month, 15 mg/day 1 month, 15 mg/day 1 month, 10 mg/day 1 month, 10 mg/day 1 month, 7.5 mg/day 1 month, 7.5 mg/day 3 months and 5 mg/day 3 months and 5 mg/day 18 months(2) dipyridamole 150 or 300 mg/day 18 months(2) dipyridamole 150 or 300 mg/day |
Steroid group serum creatinine was 0.92 0.24 mg/dl and non-steroid group was 0.91 0.24 mg/dl and non-steroid group was 0.91 0.21 mg/dl 0.21 mg/dl |
64.5 |
| Shoji T 2000[33] | Biopsy-proven Ig A nephropathy | 21 | (1) Prednisolone 0.8 mg/kg/day, then reduced to 0.4 mg/kg/day  1 month and tapered to 10 mg 1 month and tapered to 10 mg 1 year(2) dipyridamole 300 mg/day 1 year(2) dipyridamole 300 mg/day 1 year 1 year |
Proteinuria<1.5 g/day of protein and serum creatinine<1.5 mg/dl | 12 |
| K.N.Lai 1986[34] | Presence of IgA deposits in the mesangium | 34 | (1) Prednisolone 40–60 mg/day 8 weeks, then tapered by half 8 weeks, then tapered by half 4 months(2) no corticosteroid therapy 4 months(2) no corticosteroid therapy |
Steroid group urinary protein was 6.5 2.8 gm/day and non-steroid group was 4.7 2.8 gm/day and non-steroid group was 4.7 1.4 gm/day 1.4 gm/day |
38 |
| Kobayashi Y 1996[35] | Fulfilled the three conditions defining the early stage of progressive Ig A nephropathy | 90 | (1) Prednisolone 40 mg/day 4 weeks, 30 mg/day 4 weeks, 30 mg/day 8 weeks, 25 mg/day 8 weeks, 25 mg/day 8 weeks, 20 mg/day 8 weeks, 20 mg/day 8 weeks, then 15 mg/day 8 weeks, then 15 mg/day 6 months and thereafter was further tapered(2) dipyridamole 300 mg/day 6 months and thereafter was further tapered(2) dipyridamole 300 mg/day |
Creatinine clearance>70 ml/min | 120 |
| Welch TR 1992[36] | Been proved Ig A nephropathy | 20 | (1) Prednisolone 2 mg/kg(<80 mg) 12 weeks(2) placebo 12 weeks(2) placebo |
Serum creatinine<140umol/l | 3 |
| Kobayashi Y 1988[37] | Ig A nephropathy with primary glomerular deseases | 96 | (1) Prednisolone 40 mg/day 4 weeks, 30 mg/day 4 weeks, 30 mg/day 8 weeks, 25 mg/day 8 weeks, 25 mg/day 8 weeks, 20 mg/day 8 weeks, 20 mg/day 8 weeks, then 15 mg/day 8 weeks, then 15 mg/day 6 months and thereafter further tapered on a gradual basis(2) Non-steroidal anti-inflammatory and/or anti-thrombocyte drugs 6 months and thereafter further tapered on a gradual basis(2) Non-steroidal anti-inflammatory and/or anti-thrombocyte drugs |
Proteinuria>1.0 g/day | 48 |
| Julian BA 1993[38] | Biopsy-proven Ig A nephropathy | 35 | (1) Alternate day prednisolone 60 mg 3 months(2) No treatment 3 months(2) No treatment |
Creatinine clearance>25 ml/min | 24 |
| Uzu T 2003[39] | Biopsy-proven Ig A nephropathy | 45 | (1) Methylprednisolone 1 g/day 3 day, then oral prednisolone 40 mg/day 3 day, then oral prednisolone 40 mg/day 4 weeks, 30 mg/day 4 weeks, 30 mg/day 4 weeks, 25 mg/day 4 weeks, 25 mg/day 4 weeks, 20 mg/day 4 weeks, 20 mg/day 4 weeks, 15 mg/day 4 weeks, 15 mg/day 2 months, and gradual reduction in 6 months(2) Supportive treatment 2 months, and gradual reduction in 6 months(2) Supportive treatment |
Serum creatinine<106umol/l | 36 |
| Manno C[21] | Biopsy-proven Ig A nephropathy | 97 | (1) Prednisolone 1.0 mg/kg/day 2 months, then 0.2 mg/kg/day 2 months, then 0.2 mg/kg/day  4 months(2) ramipril 4 months(2) ramipril |
Serum creatinine was 1.08 mg/dl | 96 |
| Lv J[22] | Biopsy-proven Ig A nephropathy | 63 | (1) oral prednisone 0.8 to 1.0 mg/kg/day 8 weeks, then the dose was tapered by 5 to 10 mg every 2 weeks(2) cilazapril 8 weeks, then the dose was tapered by 5 to 10 mg every 2 weeks(2) cilazapril |
Serum creatinine was 1.1 mg/dl | 48 |
| Locatelli F 2001[40] | Biopsy-proven Ig A nephropathy | 86 | (1) Methylprednisolone 1 g/day 3 day at the beginning of vmonths 1, 3, and 5, and again two and four months later, oral prednisolone 0.5 mg/kg 3 day at the beginning of vmonths 1, 3, and 5, and again two and four months later, oral prednisolone 0.5 mg/kg 6 months(2) Supportive treatment 6 months(2) Supportive treatment |
Plasma creatinine levels<1.5 ml/dL | 64 |
Table 2. Risk of Bias in Studies.
| Source | Intention-to-treat analysis | Allocation concealment | Blinding | Lost to follow up |
| Katafuchi R 2008 [28] | No | Unclear | Unclear | No lost to follow-up |
| Koike M 2008[29] | Yes | Unsealed envelops | Yes: patients and caregivers | No lost to follow-up |
| Pozzi C 2004[30] | Yes | Yes | Unclear | No lost to follow-up |
| Moriyama T 2004[31] | Yes | Unclear | No | No lost to follow-up |
| Katafuchi R 2003[32] | No | Yes | No | Lost to follow-up: 13 patients |
| Shoji T 2000[33] | No | Yes | No | Lost to follow-up:2 patients |
| K.N.Lai 1986[34] | No | Unclear | No | No lost to follow-up |
| Kobayashi Y 1996[35] | No | Inadequate | No | Lost to follow-up:44 patients |
| Welch TR 1992[36] | Unclear | Yes | Yes: patients and investigators | Lost to follow-up:3 patients |
| Kobayashi Y 1988[37] | No | Unclear | Unclear | No lost to follow-up |
| Julian BA 1993[38] | No | Yes | Unclear | Lost to follow-up:2 patients |
| Uzu T 2003[39] | No | No | Unclear | No lost to follow-up |
| Manno C[21] | Yes | Yes | No | Lost to follow-up: 6 patients |
| Lv J[22] | Yes | Yes | No | Lost to follow-up: 3 patients |
| Locatelli F 2001[40] | Yes | Unclear | Unclear | Lost to follow-up: 12 patients |
Effects of Interventions
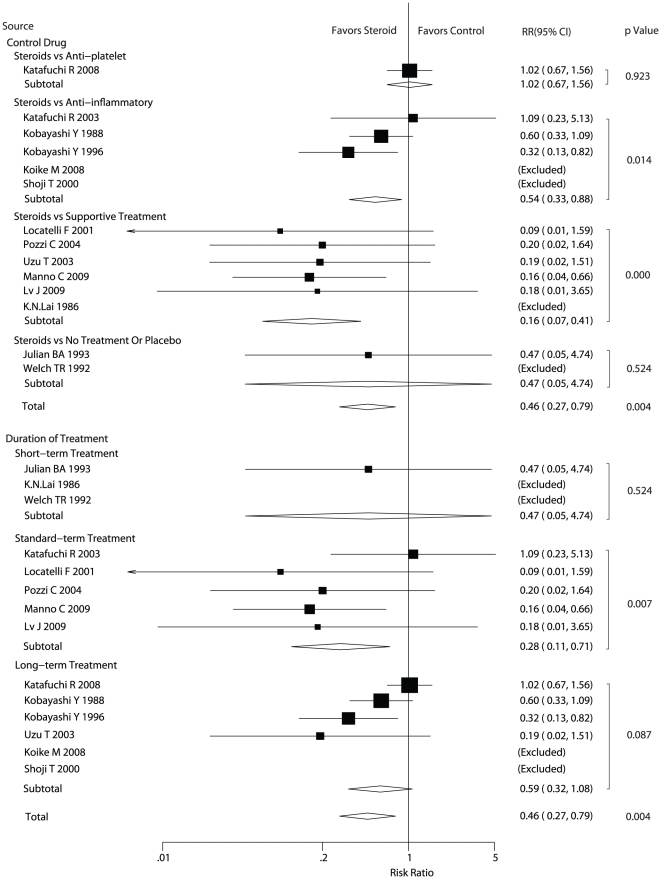
Data for the effect of steroids on end stage renal failure were available from fourteen trials. We also performed subgroup analyses based on the type of control drug or the duration of steroid therapy. In Figure 2, the pooled RR showed that the application of steroid therapy had a statistically significant relationship with reduced the risk of end stage renal failure (RR: 0.46, 95%CI: 0.27 to 0.79). Subgroup analysis based on the type of control drug showed that compared with anti-platelet for the treatment of patients in control group, steroids was not associated with a statistically significant reduction of the risk in end stage renal failure. Furthermore, the study of steroid therapy vs no treatment or placebo also provided no evidence that steroid therapy could reduced the risk of end-stage renal failure. In contrast, steroid therapy reduced the risk of end-stage renal failure compared with anti-inflammatory (RR = 0.54, 95%CI: 0.33 to 0.88) or supportive treatment (RR = 0.16, 95%CI: 0.07 to 0.41) with a statistical significance. Subgroup analysis based on the duration of treatment indicated that standard term therapy could lead to lower risk of end stage renal failure when compared with control group (RR = 0.28, 95%CI: 0.11 to 0.71), while this could not be observed for short and long term steroid therapy.
Figure 2. Effect of steroids on end-stage renal failure in patients with Ig A nephropathy.
CI, confidence intervals; RR, relative risk.
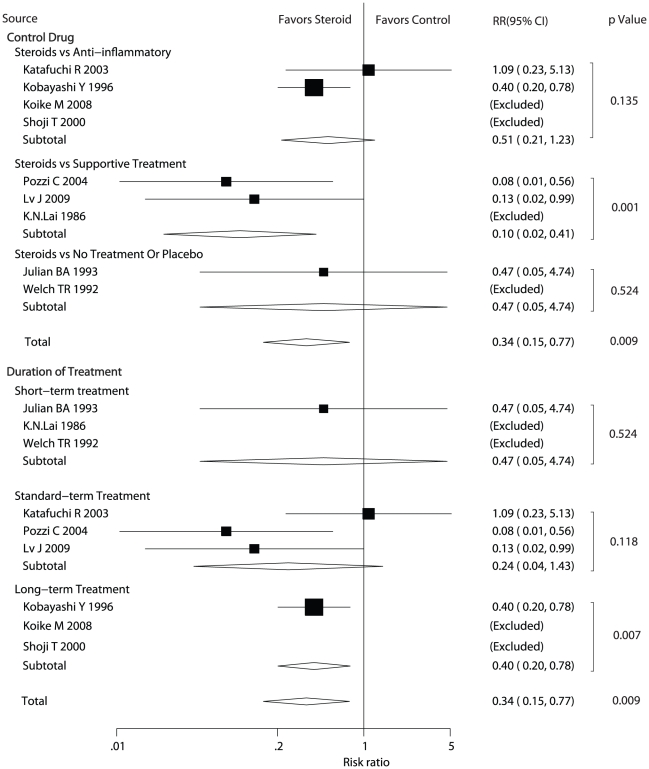
Data for the effect of steroids on doubling of serum creatinine were available from nine trials. We also performed subgroup analyses based on the type of control drug or the duration of steroid therapy. As shown in Figure 3, steroid therapy was associated with a statistically significant reduction of the risk in doubling of serum creatinine (RR = 0.34, 95% CI: 0.15 to 0.77). Subgroup analysis based on the type of control drug suggested that steroid therapy was not associated with lower risk of doubling of serum creatinine when patients in control group received anti-inflammatory treatment, placebo or no treatment. In contrast, steroid therapy statistically reduced the risk of doubling of serum creatinine compared with supportive treatment (RR = 0.10, 95%CI = 0.02 to 0.41). In addition, subgroup analysis based upon the duration of treatment showed that compared with control group, long term steroid therapy could lead to lower risk of doubling of serum creatinine (RR = 0.40, 95%CI = 0.20 to 0.78), while this could not be observed for short and standard term steroid therapy.
Figure 3. Effect of steroids on doubling of serum creatinine in patients with Ig A nephropathy.
CI, confidence intervals; RR, relative risk.
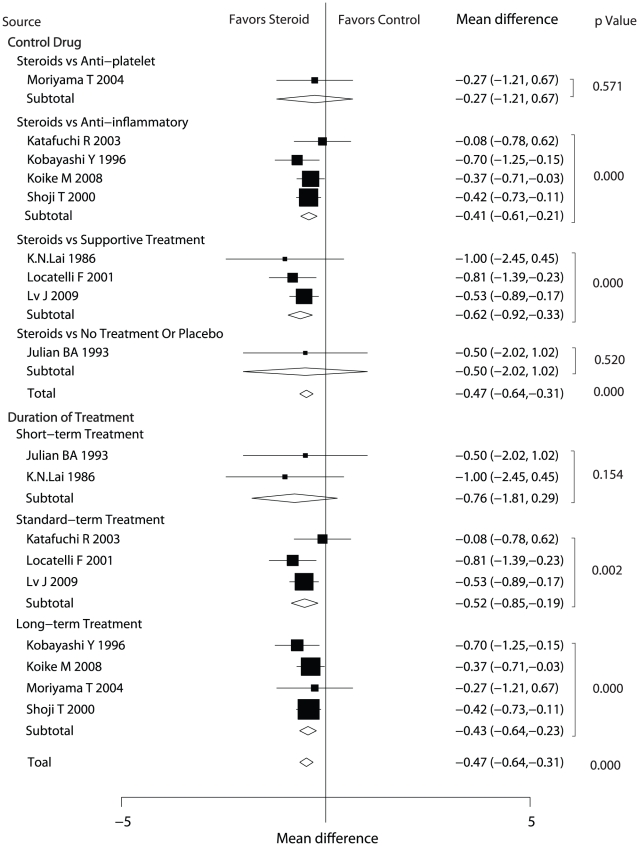
Data for the effect of steroids on urinary protein excretion were available from nine trials (Figure 4). Statistical analyses showed that steroid therapy reduced urinary protein excretion compared with control therapy (MD = −0.47 g/day, 95%CI = −0.64 to −0.31) Subgroup analysis based on the type of control drug suggested that steroid therapy was not associated with reduced urinary protein excretion when patients in control group received anti-platelet treatment, placebo or no treatment. In contrast, steroid therapy led to statistically significant reduced urinary protein excretion compared with anti-inflammatory (MD = −0.41 g/day, 95%CI = −0.61 to −0.21) and supportive treatment (MD = −0.62 g/day, 95%CI = −0.92 to −0.33). Subgroup analysis based on the duration of treatment indicated that there was an association between significantly decreased urinary protein excretion and steroid therapy in standard term (MD = −0.52 g/day, 95%CI = −0.85 to −0.19) and in long term (MD = −0.43 g/day, 95%CI = −0.64 to −0.23). But for short-term treatment, there was no evidence showing that steroid therapy could reduce the urinary protein excretion.
Figure 4. Effect of steroids on urinary protein excretion in patients with Ig A nephropathy.
CI, confidence intervals; WMD, weighted mean difference.
In addition, the analysis of adverse effect events was difficult, because a majority of these studies reported few adverse effects. It is unclear whether there were no events or they were not properly recorded, and even worse some trials did not report adverse events intentionally. Furthermore, it should be noticed that the reported adverse events of treatment or control group are specific or nonspecific, such as stomach bleeding and unusual-hypertension [40], [41].
Discussion
An increasing number of trials have evaluated the role of steroids in the treatment of IgA nephropathy and acquired various results, for which medical practitioners have few evidence-based treatment guidelines. In this large quantitative study, we performed a comprehensive literature search with no restrictions in publication status. More than 1542 patients were included to examine the effect of steroids on end-stage renal failure, doubling of serum creatinine and urinary protein excretion. The study suggested that compared with non-steroid therapy, steroid therapy was associated with clinically and statistically significant reduction of the risk in end stage renal failure (RR: 0.46, 95%CI: 0.27 to 0.79), doubling serum creatinine, (RR = 0.34, 95%CI = 0.15 to 0.77) and also urinary protein excretion at the end of treatment (MD = −0.47 g/day, 5%CI = −0.64 to −0.31).
Our results were consistent with the recommendations for the management of IgA nephropathy which were published in 1999 [13]. The recommendation indicated that IgA nephropathy patients should be treated with steroids to reduce proteinuria and stabilize renal function. However, the recommendation encountered criticism because it was based on a variety of sources, including non-randomized controlled trials data and with suboptimal methodological quality. Consequently, there was not enough information to provide strong evidence.
This meta-analysis showed that for patients with Ig A nephropathy, steroids could reduce the incidence of end stage renal failure, doubling serum creatinine and urinary protein excretion compared with patients receiving no steroidal treatment. Subgroup analysis showed that steroids vs anti-inflammatory could reduce the risk of end stage renal failure and the urinary protein excretion with a statistical significance. However, there was no evidence that steroid therapy protected against the doubling serum creatinine risk compared with anti-inflammatory therapy. The reason for this absence of difference could be that fewer events occurred and that the incidence of doubling serum creatinine was not reported in Kobayashi' study [37]. Furthermore, steroid therapy statistically reduced the risk of end-stage renal failure, doubling serum creatinine and also urinary protein excretion compared with supportive treatment. Subgroup analysis based upon the duration of treatment showed that compared with control group, long term steroid therapy was associated with a decrease of proteinuria and with a statistically significant reduction of the risk in end-stage renal failure, in addition, standard-term therapy was associated with a statistically significant reduction of the risk in end stage renal failure and urinary protein excretion. Finally, the P value for long-term therapy was very close to 0.05 for reducing the risk of end stage renal failure, which may be explained by the small amount of trials including results in this aspect. These findings corresponded with recent researches [40], [42], [43] that steroid therapy should be given for a long-term therapy.
To minimize the consequences of heterogeneity among the included studies, we performed a sequential exclusion of each trial from the pooled analysis. These exclusions did not affect the results of our meta-analysis.
Subgroup analysis is only done between-study hypothesis (not within-study hypothesis) in our review, because individual patient data and original data were not available. However, its validity was acceptable according to recently proposed criteria [44], [45], as we only conducted 2 subgroup analyses, which were based on the duration of treatment and on the type of control drug.
Recently, Cheng's review [46] illustrated that glucocoticoids significantly induced a protection of renal function and a reduction of proteinuria in patients with IgA nephropathy. This conclusion is in accordance with our own results. In addition, our subgroup analysis studied important factors which could affect the interpretation of our data. The results of this meta-analysis are promising because the outcomes consistently favor the use of steroids interventions. In all the interventions tested in the available trials, a long-term steroid therapy seems to be more beneficial.
The limitation of this study includes the inherent assumptions made for any meta-analysis, because the analysis uses pooled data either from published papers or provided by individual study authors, individual patient data and original data were not available, which prevented us doing more detailed relevant analysis and obtaining more comprehensive results. Furthermore, different follow-up times and therapy dose also could have affected our conclusions about the association between steroids and renal function. We also did not have sufficient data to get detailed effects of steroids on renal function. Therefore, we just gave a relative result by comparing steroid therapy with non-steroid therapy and provided a synthetic and comprehensive review.
For future research, promising interventions should be tested, including dosage, duration of treatment or combination with other influencing factors, such as cyclophosphamide, fish-oil, dipyridamole, antiplatelet drugs, etc, through which we might confirm the optimal time of treatment, the optimal dosage and the optimal therapy [47]. We suggest that ongoing trials would be improved by the following ways: i). Adverse events of clinical trials should be recorded and reported ii). Treatment duration and dosage should be taken into consideration before evaluating clinical outcomes.
Acknowledgments
The authors are grateful to Xin-Ji Zhang for valuable help with the literature search.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by the funding of the Ministry of Science and Technology of China (2009ZX09312-025, 2008ZX09312-007). The funder had no role in the study design, data collection, analysis, decision to publish or preparation of the manuscript.
References
- 1.Julian BA, Waldo FB, Rifai A, Mestecky J. IgA nephropathy, the most common glomerulonephritis worldwide. A neglected disease in the United States? Am J Med. 1988;84:129–32. doi: 10.1016/0002-9343(88)90019-8. [DOI] [PubMed] [Google Scholar]
- 2.Cheng KP, Fang GX, Wong MC, Ji YL, Chan KW, et al. A randomized prospective comparison of nadolol, captopril with or without ticlopidine on disease progression in Ig A nephropathy. Nephrology. 1998;4:19–26. [Google Scholar]
- 3.D' Amico G. The commonest glomerulonephritis in the world: Ig A nephropathy. Q J Med. 1987;64:709–727. [PubMed] [Google Scholar]
- 4.Tomiyoshi Y, Sakemi T, Ikeda Y, Ohtsuka Y, Nakamura M, et al. Cellular crescents and segmental glomerular necrosis in Ig A nephropathy are indicative of the beneficial effects of corticosteroid therapy. Intern Med. 2001;40:862–866. doi: 10.2169/internalmedicine.40.862. [DOI] [PubMed] [Google Scholar]
- 5.Levy M, Berger J. Worldwide perspective of IgA nephropathy. Am J Kidney Dis. 1988;12:340–347. doi: 10.1016/s0272-6386(88)80021-0. [DOI] [PubMed] [Google Scholar]
- 6.Schena FP. Immunoglobulin A nephropathy with mild renal lesion: a call in the forest for physicians and nephrologists. Am J Med. 2001;110:499–500. doi: 10.1016/s0002-9343(01)00684-2. [DOI] [PubMed] [Google Scholar]
- 7.Droz D. Natural history of primary glomerulonephritis with mesangial deposits of IgA. Contrib Nephrol. 1976;12:150–156. [Google Scholar]
- 8.D'Amico G, Colosanti G, Belg Barbiano di, Fellin G, Ragni A, et al. Long-term follow-up of IgA mesangial nephropathy: cliníco-histological study in 374 patients. Semin Nephrol. 1987;7:355–358. [PubMed] [Google Scholar]
- 9.Monteiro RC. New insights in the pathogenesis of Ig A nephropathy. Nefrologia. 2005;2:82–86. [PubMed] [Google Scholar]
- 10.Mestecky J, Tomana M, Crowley-Nowick PA, Moldoveanu Z, Julian BA, et al. Defective galactosilation and clearance of IgA1 molecules as a possible etiopathogenic factor in IgA nephropathy. Contrib Nephrol. 1993;104:172–82. doi: 10.1159/000422410. [DOI] [PubMed] [Google Scholar]
- 11.D'amico G. Treatment of IgA nephropathy: An overview. Nephrology. 1997;2:725–730. [Google Scholar]
- 12.Harmankaya O, Ozturk Y, Basturk T, Obek A, Kilicarslan I. Efficacy of immunosuppressive therapy in Ig A nephropathy presenting with isolated hematuria. Int Urol Nephrol. 2002;33:167–171. doi: 10.1023/a:1014424723466. [DOI] [PubMed] [Google Scholar]
- 13.Nolin L, Courteau M. Management of Ig A nephropathy: Evidence-based recommendations. Kidney Int. 1999;70:56–62. doi: 10.1046/j.1523-1755.1999.07008.x. [DOI] [PubMed] [Google Scholar]
- 14.Gutierrez E, Gonzalez E, Hernandez E, Morales E, Martinez MA, et al. Factors that determine an incomplete recovery of renal function in Macrohematuria-induced acute renal failure of Ig A nephropathy. Clin J Am Soc Nephrol. 2007;2:51–57. doi: 10.2215/CJN.02670706. [DOI] [PubMed] [Google Scholar]
- 15.Gallo GR, Katafuchi R, Neelakantappa K, Baldwin DS. Prognostic pathologic markers in IgA nephropathy. Am J Kidney Dis. 1988;12:363–5. doi: 10.1016/s0272-6386(88)80025-8. [DOI] [PubMed] [Google Scholar]
- 16.Laville M, Alamartine E. Treatment options for Ig A nephropathy in adults: a proposal for evidence-based strategy. Nephrol Dial Transplant. 2004;19:1947–1951. doi: 10.1093/ndt/gfh309. [DOI] [PubMed] [Google Scholar]
- 17.Neelakantappa K, Gallo GR, Baldwin DS. Proteinuria in IgA nephropathy. Kidney Int. 1988;33:716–21. doi: 10.1038/ki.1988.57. [DOI] [PubMed] [Google Scholar]
- 18.Barratt J, Feehally J. Treatment of Ig A nephropathy. Kidney Int. 2006;11:1934–1938. doi: 10.1038/sj.ki.5000419. [DOI] [PubMed] [Google Scholar]
- 19.Hodson EM, Willis NS, Craig JC. Corticosteroid therapy for nephrotic syndrome in children. Cochrane Db Syst Rev. 2006;1:1240–1296. doi: 10.1002/14651858.CD001533.pub4. [DOI] [PubMed] [Google Scholar]
- 20.Strippoli GFM, Manno C, Schena FP. An “evidence-based” survey of therapeutic options for Ig A nephropathy: assessment and criticism. Am. J Kidney Dis. 2003;41:1129–1139. doi: 10.1016/s0272-6386(03)00344-5. [DOI] [PubMed] [Google Scholar]
- 21.Manno C, Torres DD, Rossini M, Pesce F, Schena FP. Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric Ig A nephropathy. Nephrol Dial Transpl. 2009;12:3694–3701. doi: 10.1093/ndt/gfp356. [DOI] [PubMed] [Google Scholar]
- 22.Lv J, Zhang H, Chen Y, Li G, Jiang L, et al. Combination Therapy of Prednisone and ACE Inhibitor versus ACE-Inhibitor Therapy Alone in Patients With IgA Nephropathy: A Randomized Controlled Trial. Am J Kidney Dis. 2009;53:26–32. doi: 10.1053/j.ajkd.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 23.Higgins J, Altman DG. Assessing risk of bias in included studies. In: Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.1. Oxford, England: Cochrane Collaboration: chap 8; 2008. [Google Scholar]
- 24.Shimizu A, Takei T, Uchida K, Tsuchiya K, Nitta K. Predictors of poor outcomes in steroid therapy for immunoglobulin A nephropathy. Nephrology. 2009;14:521–526. doi: 10.1111/j.1440-1797.2009.01104.x. [DOI] [PubMed] [Google Scholar]
- 25.Waldo FB, Wyatt RJ, Kelly DR, Herrera GA, Benfield MR, et al. Treatment of Ig A nephropathy in children: efficacy of alternate-day oral prednisone. Pediatr Nephrol. 1993;5:529–532. doi: 10.1007/BF00852535. [DOI] [PubMed] [Google Scholar]
- 26.Ohashi T, Shimokawahara H. Effects of steroid therapy in Ig A nephropathy. Fukuoka lgaku zasshi. 1992;5:209–215. [PubMed] [Google Scholar]
- 27.Deeks JJ, Higgins JPT, Altman DG. Analyzing data and undertaking meta-analyses. In: Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.1. Oxford, UK: The Cochrane Collaboration: chap 9; 2008. [Google Scholar]
- 28.Katafuchi R, Ninomiya T, Mizumasa T, Ikeda K, Kumagai H, et al. The improvement of renal survival with steroid pulse therapy in IgA nephropathy. Nephrol Dial Transpl. 2008;23:3915–3920. doi: 10.1093/ndt/gfn394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koike M, Takei T, Uchida K, Honda K, Moriyama T, et al. Clinical assessment of low-dose steroid therapy for patients with IgA nephropathy: a prospective study in a single center. Clin Exp Nephrol. 2008;12:250–255. doi: 10.1007/s10157-008-0036-7. [DOI] [PubMed] [Google Scholar]
- 30.Pozzi C, Andrulli S, Del Vecchio L, Melis P, Fogazzi GB, et al. Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. J Am Soc Nephrol. 2004;15:157–163. doi: 10.1097/01.asn.0000103869.08096.4f. [DOI] [PubMed] [Google Scholar]
- 31.Moriyama T, Honda K, Nitta K, Yumura W, Nihei H. The effectiveness of steroid therapy for patients with advanced IgA nephropathy and impaired renal function. Clin Exp Nephrol. 2004;8:237–242. doi: 10.1007/s10157-004-0298-7. [DOI] [PubMed] [Google Scholar]
- 32.Katafuchi R, Ikeda K, Mizumasa T, Tanaka H, Ando T, et al. Controlled, prospective trial of steroid treatment in IgA nephropathy: a limitation of low-dose prednisolone therapy. Am J Kidney Dis. 2003;5:972–983. doi: 10.1016/s0272-6386(03)00194-x. [DOI] [PubMed] [Google Scholar]
- 33.Shoji T, Nakanishi I, Suzuki A, Hayashi T, Togawa M, et al. Early treatment with corticosteroids ameliorates proteinuria, proliferative lesions, and mesangial phenotypic modulation in adult diffuse proliferative IgA nephropathy. Am J Kidney Dis. 2000;2:194–201. doi: 10.1016/s0272-6386(00)70326-x. [DOI] [PubMed] [Google Scholar]
- 34.Lai KN, Lai FM, Ho CP, Chan KW. Corticosteroid therapy in IgA nephropathy with nephrotic sydrome: A long-term controlled trial. Clin Nephrol. 1986;4:174–180. [PubMed] [Google Scholar]
- 35.Kobayashi Y, Hiki Y, Kokubo T, Horri A, Tateno S. Steroid therapy during the early stage of progressive IgA nephropathy. A 10-year follow-up study. Nephrol. 1996;72:237–242. doi: 10.1159/000188848. [DOI] [PubMed] [Google Scholar]
- 36.Welch TR, Fryer C, Shely E, Witte DP, Quinlan M. Double-blind, controlled trial of short-term prednisone therapy in immunoglobulin A glomerulonephritis. J Pediatr. 1992;121:474–477. doi: 10.1016/s0022-3476(05)81808-6. [DOI] [PubMed] [Google Scholar]
- 37.Kobayashi Y, Hiki Y, Fujii K, Kurokawa A, Kamiyama M, et al. Effect of corticosteroids on renal function in progressive IgA nephropathy - Long-term follow-up study. Nippon Jinzo Gakkai Shi. 1988;9:73–80. [PubMed] [Google Scholar]
- 38.Julian BA, Barker C. Alternate-day prednisone therapy in IgA nephropathy: Preliminary analysis of a prospective, randomized, controlled trial. Contrib Nephrol. 1993;104:198–206. [PubMed] [Google Scholar]
- 39.Uzu T, Harada T, Ko M, Yamato M, Takahara K, et al. Effect of corticosteroid therapy on the progression of IgA nephropathy with moderate proteinuria. Clin Exp Nephrol. 2003;7:210–214. doi: 10.1007/s10157-003-0236-0. [DOI] [PubMed] [Google Scholar]
- 40.Locatelli F, Pozzi C, Del Vecchio L, Bolasco PG, Fogazzi GB, et al. Role of proteinuria reduction in the progression of Ig A nephropathy. Ren fail. 2001;23:495–505. doi: 10.1081/jdi-100104732. [DOI] [PubMed] [Google Scholar]
- 41.Komatsu H, Fujimoto S, Hara S, Sato Y, Yamada K, et al. Multivariate analysis of prognostic factors and effect of treatment in patients with Ig A nephropathy. Ren fail. 2005;1:45–52. [PubMed] [Google Scholar]
- 42.Pozzi C, Bolasco PG, Fogazzi GB, Andrulli S, Altieri P, et al. Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet. 1999;353:883–887. doi: 10.1016/s0140-6736(98)03563-6. [DOI] [PubMed] [Google Scholar]
- 43.Appel GB, Waldman M. The Ig A nephropathy treatment dilemma. Kidney Int. 2006;69:1939–1944. doi: 10.1038/sj.ki.5000434. [DOI] [PubMed] [Google Scholar]
- 44.Bender R, Bunce C, Clarke M, Simon G, Stefan L, et al. Attention should be given to multiplicity issues in systematic reviews. J Clin Epidemiol. 2008;61:857–865. doi: 10.1016/j.jclinepi.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 45.Guyatt GH, Wyer P, Ioannidis J. When to believe a subgroup analysis. In: Guyatt G, Rennie R, Meade M, Cook D, et al., editors. User's Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. New York, NY: McGraw-Hill; 2008. [Google Scholar]
- 46.Cheng J, Zhang X, Zhang W, He Q, Tao X, et al. Efficacy and Safety of Glucocorticoids Therapy for IgA Nephropathy: A Meta-Analysis of Randomized Controlled Trials. Am J Nephrol. 2009;30:315–322. doi: 10.1159/000226129. [DOI] [PubMed] [Google Scholar]
- 47.Knechtle SJ. Clinical trials: Where are we now? Immunol Rev. 2003;196:237–246. doi: 10.1046/j.1600-065x.2003.00086.x. [DOI] [PubMed] [Google Scholar]