Abstract
Purpose
To explore the association between risk of malnutrition as well as current body mass index (BMI) and health-related quality of life (HRQoL) in elderly men and women from the general population.
Methods
In a cross-sectional population survey including 1,632 men and 1,654 women aged 65 to 87 years from the municipality of Tromsø, Norway, we assessed HRQoL by using the EuroQol (EQ-5D) instrument in three risk groups of malnutrition and in different categories of BMI. The Malnutrition Universal Screening Tool (‘MUST’) was used to evaluate the risk of malnutrition.
Results
We found a significant reduction in HRQoL with an increasing risk of malnutrition, and this was more pronounced in men than in women. The relationship between BMI and HRQoL was dome shaped, with the highest score values in the BMI category being 25–27.5 kg/m2.
Conclusions
HRQoL was significantly reduced in elderly men and women at risk of malnutrition. The highest HRQoL was seen in moderately overweight individuals.
Keywords: HRQoL, EQ-5D, Body mass index, Elderly, Malnutrition universal screening tool, Nutrition assessment
Introduction
Malnutrition and being underweight are persisting problems also in the affluent parts of the world and is more prevalent in the elderly than in other adult individuals [1]. In developed countries, malnutrition is largely related to diseases [2]. Throughout the previous decades, health-related quality of life (HRQoL) has received increased attention as a measure for comparing health statuses across different patient groups and for measuring health outcomes. While recent studies reveal strong evidence of increased morbidity [2, 3] and mortality [4, 5] in underweight elderly people, little attention has been given to the ways in which malnutrition affect HRQoL. Not only is the quantity of life, calculated in years, important for the increasing number of elderly individuals with longer life expectancies, but the quality of life is important as well.
The concept of HRQoL broadens a previous definition of health based on morbidity and mortality to include aspects such as subjective assessment of physical, emotional and social functioning [6]. Nutrition may affect both physical and psychological aspects important for HRQoL [2]. Several reports have found HRQoL to be reduced in obese individuals [7]. In a study of nursing home patients [8] and a smaller community-based study [9], quality of life was reduced in the elderly at risk of malnutrition. However, larger community-based studies evaluating HRQoL in the elderly at risk of malnutrition are lacking.
The purpose of the present study was to explore the association between risk of malnutrition, categories of body mass index and HRQoL in community-living elderly men and women using the EuroQol (EQ-5D) instrument [10].
Methods
Population for the study
The Tromsø Study is a health survey of the population of Tromsø, a medium-sized town in Norway. The 6th cross-sectional survey was conducted between October 2007 and December 2008. All independently living inhabitants aged 65 to 87 years (6,098) were invited, of which 4,017 (66%) participated by going to a study center for data collection. After exclusions (21 persons because height or weight had not been measured due to various disabilities, 412 persons because of missing weight loss information and additionally 298 persons due to lack of response to the EQ-5D health state descriptive system), 3,286 subjects (i.e., 54% of the eligible subjects) were included in the analyses of the EQ-5D-index. The second part of the EQ-5D exercise (the EQ VAS scale) had 1,306 respondents.
The regional board of research ethics approved the survey, and each participant gave written informed consent prior to inclusion in the study.
Nutritional screening tool and body mass index
At the study center, the participants, who were instructed to wear no shoes and light clothing, had their weight (kg) and height (cm) measured to the nearest decimal using a Jenix DS-102 stadiometer (Dong Sahn Jenix Co., Ltd., Seoul, Korea). Body mass index (BMI) was calculated as weight divided by the square of height (kg/m2). The participants were asked in a self-administrated questionnaire whether they had any involuntary weight loss during the last 6 months. If they had, they were asked how many kilograms (kg) had been lost. Weight loss was grouped as follows: below 5%, between 5 and 10% or above 10% of body weight prior to weight loss.
Based on the BMI and degree of weight loss, each subject was categorized into low, medium or high risk of malnutrition according to the malnutrition universal screening tool (‘MUST’) (Fig. 1). The ‘MUST’ tool is one of the nutritional screening instruments recommended by the European Society for Parenteral and Enteral nutrition [11], and it was originally developed by the British Society of Parenteral and Enteral nutrition (www.bapen.org.uk) [12]. It includes an acute disease component with no nutritional intake for >5 days, which normally necessitates hospitalization [12]. As participation in this study required the ability to independently visit a research center, the acute diseases component was set to zero. The weight loss question was slightly modified to state a time span of the “last 6 months”, but this encompasses the time span of “the past 3–6 months” in the original ‘MUST’ tool.
Fig. 1.
The malnutrition universal screening tool (‘MUST’) is composed of a BMI score, a weight loss score and an acute illness component. These are added, and based on the sum score, the risk of malnutrition can be assessed. The “Malnutrition Universal Screening Tool” is reproduced here with the kind permission of BAPEN (British Association for Parenteral and Enteral Nutrition). For further information on ‘MUST’ and management guidelines, see www.bapen.org.uk
Based on BMI alone, we further categorized the participants into six categories (<20.0, 20.0–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9 and ≥30 kg/m2), thereby including the WHO (World Health Organization) definitions of overweight (25.0–29.9 kg/m2) and obesity (≥30 kg/m2) [13].
Assessment of HRQoL
HRQoL was measured by the EQ-5D, which is a standardized non-disease specific instrument consisting of two parts: the EQ-5D descriptive system and the EQ visual analogue scale (EQ VAS) [10]. The EQ-5D has been utilized in a number of studies, and the instrument is validated in acutely ill, elderly individuals [14] and community-living elderly women receiving medication (clodronate) for osteoporosis [15], but not in large populations of community-living elderly men and women. In a systematic literature review of self-assessed health instruments [16], the EQ-5D was one of the recommended generic health instruments for use in older people.
EQ-5D describes health in generic terms using five specific dimensions, which are important for elderly individuals: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension is divided into three levels of severity (no problems, some problems or extreme problems). Due to only a few participants reporting problems at the most severe level (extreme problems), this category was included with the individuals reporting some problems (second level) in the analyses of the various EQ-5D dimensions (Table 2). The EQ-5D instrument is designed for self-completion and was included as part of a self-administrated questionnaire. A single summary EQ-5D index with a maximum score of 1 is obtained by applying a scoring algorithm that assigns weights to each of the possible combinations of health, as described by the three levels within each of the five dimensions. In the current study, we applied the most widely used scoring algorithm, referred to as the UK time-trade-off tariff [17]. Subjects missing values from any of the five dimensions were excluded from the analyses.
Table 2.
Proportionsa of the 3,286 elderly men and women reporting problems in the various EQ-5D dimensions, The Tromsø study
| EQ-5D dimensions | Sex | All subjects | Subjects by risk of malnutrition | |||
|---|---|---|---|---|---|---|
| Low | Medium | High | P-valueb | |||
| Any dimensions | Men | 52.9 (864) | 52.2 (804) | 53.6 (30) | 85.7 (30) | <0.001 |
| Women | 69.7 (1,153) | 69.0 (1,034) | 74.7 (74) | 78.9 (45) | 0.51 | |
| Mobility | Men | 14.6 (238) | 13.7 (211) | 19.6 (11) | 45.7 (16) | <0.001 |
| Women | 22.4 (370) | 21.9 (328) | 29.3 (29) | 22.8 (13) | 0.31 | |
| Self-care | Men | 3.3 (54) | 2.7 (42) | 7.1 (4) | 22.9 (8) | <0.001 |
| Women | 4.7 (77) | 4.5 (67) | 5.1 (5) | 8.8 (5) | 0.1 | |
| Usual activities | Men | 12.6 (205) | 11.6 (178) | 21.4 (12) | 42.9 (15) | <0.001 |
| Women | 23.2 (383) | 21.8 (326) | 35.4 (35) | 38.6 (22) | <0.001 | |
| Pain/discomfort | Men | 45.7 (746) | 45.1 (695) | 45.4 (26) | 71.4 (25) | 0.007 |
| Women | 63.9 (1,057) | 63.4 (950) | 70.7 (70) | 64.9 (37) | 0.34 | |
| Anxiety/depression | Men | 12.3 (201) | 11.9 (183) | 16.1 (9) | 25.7 (9) | 0.01 |
| Women | 23.3 (385) | 22.0 (329) | 37.4 (37) | 33.3 (19) | 0.001 | |
aProportions are given as % (number) reporting problems
b P-value for linear trend across increasing risk categories of malnutrition
In addition to this indirect health index assigned through a descriptive system, a direct method was used asking subjects to rate their health on a visual analogue scale (VAS) with a maximum score of 100. The endpoints were labeled as “worst imaginable health state” and “best imaginable health state.”
The number responding to the EQ VAS scale question (669 men and 637 women) was lower than the number responding to the EQ-5D health state descriptive system. When comparing responders to non-responders on the EQ VAS scale, both groups had a mean EQ-5D health index of 0.82. In the responders, the mean BMI and age were somewhat lower (0.4 kg/m2 and 0.5 years, respectively). Although minor, these differences were statistically significant (BMI P = 0.02 and age P = 0.005).
Other variables
Information on socio-demographics and smoking status (Table 1) was also obtained from self-administrated questionnaires.
Table 1.
Characteristics of the participating elderly men and women, The Tromsø study
| Men | Women | P-valueb | |
|---|---|---|---|
| Na | 1,654 | 1,632 | |
| Age, years. Mean (SD) | 71.4 (5.4) | 72.1 (5.6) | <0.001c |
| Single living (%) | 24.6 | 48.2 | <0.001d |
| Post-secondary school education (%) | 30.0 | 18.4 | <0.001d |
| Household income ≥300,000 NOKe (%) | 58.4 | 40.3 | <0.001d |
| Smoking (%) | |||
| Never | 24.1 | 47.1 | <0.001d |
| Previous | 60.3 | 38.0 | |
| Current | 15.6 | 14.9 | |
| BMI kg/m2. Mean (SD) | 27.0 (3.6) | 26.9 (4.6) | 0.58c |
| Risk of malnutrition (%) | |||
| Low | 94.4 | 90.6 | <0.001d |
| Medium | 3.4 | 6.0 | |
| High | 2.1 | 3.4 | |
| EQ-5D index—mean (95% CI) | 0.86 (0.85–0.87) | 0.79 (0.78–0.80) | <0.001c |
| EQ VAS scoref—mean (95% CI) | 75.4 (74.3–76.6) | 73.0 (71.6–74.4) | 0.008c |
aThere are minor differences in the number of evaluated subjects due to variations in missing values on the self-administrated questionnaire (concerning education, income and smoking)
b P-values for the difference between men and women were estimated using the two-sample t-testc, chi-square testd
eNOK 8 = € 1
f637 women and 669 men reported the EQ VAS score
Data analyses
We stratified the analyses when dealing with risk categories of malnutrition and HRQoL by gender (Tables 2, 3; Figs. 2, 3). However, for the relation between BMI and HRQoL, tests for interaction between BMI and sex were found to be non-significant both for the EQ-5D index (P = 0.57) and the EQ VAS score (P = 0.37). The combined results for men and women are presented (Figs. 4, 5). Analysis of covariance was used to obtain age-adjusted mean values with corresponding 95% confidence intervals for different risk categories of malnutrition and categories of BMI (Figs. 2, 3, 4, 5). Differences between groups were evaluated by the chi-square test or t-test when appropriate (Tables 1, 2). Binary logistic regression with adjustment for age was used to estimate the association between the risk category of malnutrition and the various EQ-5D dimensions (Table 3). The association between increasing risk of malnutrition and the EQ-5D- or EQ VAS score was assessed by linear regression in a multivariate model adjusting for age. We tested for a quadratic relation between BMI categories and HRQoL by also including the BMI categories squared in a multivariate linear regression model (Figs. 4, 5).
Table 3.
Adjusteda odds ratios (95% confidence interval) for associations between various EQ-5D dimensions and risk category of malnutrition in 3,286 elderly men and women, The Tromsø study
| EQ-5D dimension | Risk category of malnutrition | ||||
|---|---|---|---|---|---|
| Low | Medium | High | P-valueb | ||
| Mobility | Men | 1.00 | 1.43 (0.72–2.84) | 4.91 (2.46–9.81) | <0.001 |
| Women | 1.00 | 1.32 (0.83–2.10) | 0.77 (0.40–1.48) | 0.95 | |
| Self-care | Men | 1.00 | 2.52 (0.86–7.34) | 9.56 (4.05–22.57) | <0.001 |
| Women | 1.00 | 0.98 (0.38–2.52) | 1.26 (0.47–3.38) | 0.71 | |
| Usual activities | Men | 1.00 | 1.94 (0.99–3.78) | 5.29 (2.62–10.65) | <0.001 |
| Women | 1.00 | 1.78 (1.14–2.77) | 1.72 (0.97–3.05) | 0.005 | |
| Pain/discomfort | Men | 1.00 | 1.00 (0.58–1.73) | 2.80 (1.37–5.72) | 0.011 |
| Women | 1.00 | 1.35 (0.86–2.11) | 1.00 (0.57–1.74) | 0.50 | |
| Anxiety/depression | Men | 1.00 | 1.43 (0.69–2.96) | 2.58 (1.19–5.61) | 0.012 |
| Women | 1.00 | 2.03 (1.32–3.11) | 1.59 (0.90–2.81) | 0.003 | |
aAdjusted for age
b P-value for linear trend across increasing risk categories of malnutrition
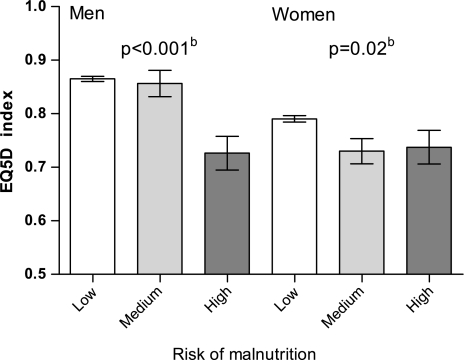
Fig. 2.
Meana EQ-5D index by risk of malnutrition in elderly men and women, The Tromsø Study. aAdjusted for age. b P-values for linear trend across the categories. Vertical lines indicate 95% CI
Fig. 3.
Mean EQ VAS scoresa by risk of malnutrition in elderly men and women, The Tromsø Study. aAdjusted for age. b P-values for linear trend across the categories. Vertical lines indicate 95% CI
Fig. 4.
Mean EQ-5D indexa by different categories of BMI in elderly men and women, The Tromsø study. aAdjusted for age and sex. Vertical lines indicate 95% CI
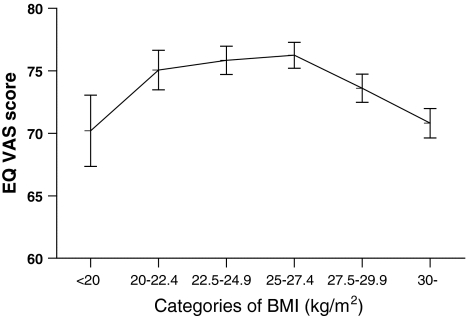
Fig. 5.
Mean EQ VAS scoresa by different categories of BMI in elderly men and women, The Tromsø study. aAdjusted for age and sex. Vertical lines indicate 95% CI
The importance of the differences in HRQoL scores between risk groups of malnutrition may be examined by calculating their effect size as the mean difference divided by the standard deviation (SD) of the control group [18]. We evaluated the detected differences against the criteria introduced by Cohen [19] using the SD of the low-risk category of malnutrition. Effect size values of 0.2–<0.5, 0.5–<0.8 and ≥0.8 were characterized as small, medium and large differences, respectively.
Two-sided P-values < 0.05 were considered to be statistically significant. The analyses were performed using SPSS statistical software version 17.0 (SPSS Inc., Chicago, Illinois, USA).
Results
The mean age (SD) was 71.7 (5.5) years, and there was approximately the same number of men (1,632) as women (1,654) included in the analyses (Table 1). Women tended to live alone, have lower education and have lower household income. More women (9.6%) than men (5.6%) were at risk of malnutrition (medium- and high-risk combined). HRQoL was lower in women than in men when assessed by the EQ-5D index and the EQ VAS score. For both men and women, the median and mean values of the EQ-5D index were almost identical, whereas the median EQ VAS score was somewhat higher than the mean in both men and women (numbers not shown).
Health dimensions
Table 2 shows the proportions of the participants reporting problems in any of the various EQ-5D dimensions of health. Overall, the majority of both women (70%) and men (53%) reported problems related to at least one of the health dimensions. One in four women reported difficulties in the dimensions of mobility, usual activities and anxiety/depression. The corresponding proportions for men were somewhat lower (12–15%). Pain and discomfort were reported by more than half of the women and by a somewhat lower proportion of the men.
With increasing risk of malnutrition, problems in all five health dimensions were reported more frequently (Table 2). However, the differences between the low- and high-risk categories were substantially larger in men than in women. A test for linear trend across increasing risk categories of malnutrition was statistically significant for two of the dimensions in women and for all five dimensions in men.
The strength of the associations between various risk categories of malnutrition and the different EQ-5D dimensions as outcome variables is further described in Table 3. In men, statistically significant associations were found for all of the five dimensions. For men in the high-risk category of malnutrition, the strongest association was found for self-care (odds ratio (OR) = 9.6). The corresponding OR estimates were 4.9 for mobility and 5.3 for usual activities. In women, the associations were strongest for two dimensions: usual activities (OR = 1.7) and anxiety/depression (OR = 2.0 for the medium-risk category).
Risk of malnutrition and HRQoL
The impact of increasing risk of malnutrition on the EQ-5D summary indices is shown in Fig. 2. The age-adjusted associations between increasing risk of malnutrition and the EQ-5D were significant for both men and women (P-value for men <0.001 and for women 0.02).
For the EQ VAS score (Fig. 3), a similar relationship was significant in men (P = 0.001), but not in women (P = 0.24).
When comparing the differences in mean score between the low- and high-risk categories of malnutrition, we found that the effect size for the EQ-5D score for men was 0.85 (large) and for women it was 0.26 (small). Corresponding values for the VAS scale were 0.97 (large) for men and 0.31 (small) for women. When comparing the low- and medium-risk categories of malnutrition, we found the effect size for the difference in EQ-5D score in women to be 0.30 (small), and the other estimated effect sizes were minor.
BMI and HRQoL
We found a dome-shaped relationship between BMI categories and both the EQ-5D index and the EQ VAS score, with the highest HRQoL in the BMI category of 25.0–27.5 kg/m2 (Figs. 4, 5). The P-values for a quadratic term of the BMI categories were <0.01 for both the EQ-5D index and the EQ-5D VAS score (adjusted for age and gender). Separate analyses for men and women revealed the same overall dome-shaped pattern.
Discussion
HRQoL is of increasing interest in epidemiology and health outcomes research. In this population-based study of elderly men and women, we found HRQoL to be significantly reduced in individuals at increased risk of malnutrition. All dimensions in the EQ-5D descriptive system were affected in men, while only two dimensions (usual activities and anxiety/depression) were affected in women. A dome-shaped relationship was seen between BMI and both the EQ-5D index and EQ VAS score.
Risk of malnutrition and HRQoL
To our knowledge, there are no similar, previous large-scale studies of the association between risk of malnutrition and HRQoL in elderly populations utilizing validated instruments. Due to the many different criteria and instruments in use for assessing both HRQoL and nutritional status, it is difficult to compare relevant studies. There are, however, reports from a smaller community-based study [9] and from more selected elderly populations [20–22] that have indicated that an association exists between the risk for malnutrition and reduced HRQoL. One study of hospitalized elderly individuals reports no clear association between malnutrition and HRQoL [23].
There are several possible explanations for the observed associations. Malnutrition and weight loss are important factors in the development of sarcopenia with loss of lean body mass and muscle function [24]. This may in turn be of special importance to EQ5D dimensions like self-care and usual activities, both significantly associated with the risk of malnutrition in the present study. Furthermore, malnutrition may affect the mental health of elderly individuals adversely, thereby reducing HRQoL [25]. Malnutrition may also be associated with diseases and conditions, which in turn decrease HRQoL.
BMI and HRQoL
The relation between BMI and HRQoL has been investigated in previous studies of elderly men and women, finding impaired HRQoL in both obese and underweight individuals [26–28], with the highest HRQoL in individuals of the BMI category 20–24.9 kg/m2. In the present study, we used narrower BMI categories. The differences in the HRQoL scores between the middle BMI categories were small; however, for the low-weight and obese individuals, we found a reduced HRQoL compared with the summit group consisting of the moderately overweight participants (BMI 25–27.5 kg/m2). In this respect, our results for HRQoL are in line with studies of mortality, indicating that moderately overweight, elderly men and women have the lowest mortality [29].
HRQoL in obese individuals may be impaired by associated comorbid conditions, especially pain [30]. Possible explanations for the reduced HRQoL among subjects with low BMI will largely correspond to the aspects discussed regarding individuals at increased risk of malnutrition.
The ‘MUST’ score of malnutrition is recommended for use in a community setting [11] and has acceptable test qualities in hospital populations when compared to more comprehensive instruments [31]. The EQ-5D is a standardized instrument developed to provide a non-disease specific measure of health status and is also suitable for use in studies of population health [10, 32]. The SF-36 questionnaire for HRQoL assessment is more comprehensive and has a larger evidence base [33]. However, in the extensive review of generic, self-assessed health instruments for use in older people by Haywood et al. [16], the EQ-5D was also found to have good reliability, validity and responsiveness. It has been found to have substantial agreement with the SF-36 [15].
One potential limitation of this study is the number of non-attending individuals and participants with missing values. All participants had to visit a research center, and consequently both individuals living in institutions and with physical limitations are underrepresented. Thus, the non-attending individuals were probably frailer, and it is unlikely that the observed associations were weaker in this group than in the participants. The cross-sectional design also limits conclusions about causality, although the most plausible direction originates with risk of malnutrition and moves towards HRQoL.
Gender differences
Women in the present study generally had a lower HRQoL than men, a finding reported in several studies of HRQoL in elderly individuals [34, 35]. This may be caused by a higher prevalence of disability and chronic conditions in women [36]. Other potential explanations for the observed sex difference include a lower socio-economic status, a greater tendency to report health problems or higher expectations of health and function in women when compared to men.
In the male participants, however, the impact of malnutrition on HRQoL was stronger than in women. Gender-specific analyses have not been performed in the previous studies addressing malnutrition and HRQoL. Research on body composition in older people has shown that during weight loss, men loose more lean mass than fat mass, whereas women loose more fat mass than lean mass [37]. It is possible that a relatively higher reduction in lean body mass can partly explain the stronger impact of malnutrition on HRQoL in men than in women.
Are the detected differences important? By using the Cohen criteria for effect sizes, the differences detected between the high- and low-risk categories in men can be regarded as large for both the EQ-5D index and the EQ VAS score. For women, the corresponding differences were low. Effect size estimates are based on the distribution of the data but have often been found to yield values that agree roughly with those estimated from more individually oriented methods [18].
Conclusion
HRQoL was significantly reduced in elderly people at increased risk of malnutrition, and this was more pronounced in men than in women. The highest HRQoL scores were found in moderately overweight individuals.
Acknowledgments
This work was supported by a grant from the center for research in the elderly, the Northern Regional Health Authority. The Tromsø 6 study was carried out by The University of Tromsø, Department of Community Medicine.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- HRQoL
Health-related quality of life
- BMI
Body mass index
- MUST
Malnutrition universal screening tool
- EQ-5D
EuroQol-5D
- EQ-5D index
Value attached to an EQ-5D state according to a particular set of weights
- EQ VAS
Standard vertical visual analogue scale
- CI
Confidence interval
- SD
Standard deviation
References
- 1.Pirlich M, Lochs H. Nutrition in the elderly. Best Practice & Research Clinical Gastroenterology. 2001;15(6):869–884. doi: 10.1053/bega.2001.0246. [DOI] [PubMed] [Google Scholar]
- 2.Stratton RJ, Green CJ, Elia M. Disease-related malnutrition: An evidence-based approach to treatment. Oxon: CABI Publishing; 2003. [Google Scholar]
- 3.Kvamme J-M, Wilsgaard T, Florholmen J, Jacobsen BK. Body mass index and disease burden in elderly men and women: The Tromsø study. European Journal of Epidemiology. 2010;25(3):183–193. doi: 10.1007/s10654-009-9422-z. [DOI] [PubMed] [Google Scholar]
- 4.Henderson S, Moore N, Lee E, Witham MD. Do the malnutrition universal screening tool (MUST) and Birmingham nutrition risk (BNR) score predict mortality in older hospitalised patients? BMC Geriatr. 2008;8:26. doi: 10.1186/1471-2318-8-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stratton RJ, King CL, Stroud MA, Jackson AA, Elia M. ‘Malnutrition universal screening tool’ predicts mortality and length of hospital stay in acutely ill elderly. British Journal of Nutrition. 2006;95(2):325–330. doi: 10.1079/BJN20051622. [DOI] [PubMed] [Google Scholar]
- 6.Drewnowski A, Evans WJ. Nutrition, physical activity, and quality of life in older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001;56(2):89–94. doi: 10.1093/gerona/56.suppl_2.89. [DOI] [PubMed] [Google Scholar]
- 7.Jia H, Lubetkin EI. The impact of obesity on health-related quality-of-life in the general adult US population. Journal of Public Health (Oxford, England) 2005;27(2):156–164. doi: 10.1093/pubmed/fdi025. [DOI] [PubMed] [Google Scholar]
- 8.Crogan NL, Pasvogel A. The influence of protein-calorie malnutrition on quality of life in nursing homes. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2003;58(2):159–164. doi: 10.1093/gerona/58.2.m159. [DOI] [PubMed] [Google Scholar]
- 9.Keller HH, Østbye T, Goy R. Nutritional risk predicts quality of life in elderly community-living Canadians. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2004;59(1):68–74. doi: 10.1093/gerona/59.1.m68. [DOI] [PubMed] [Google Scholar]
- 10.The Euro Qol Group EuroQol–a new facility for the measurement of health-related quality of life. The EuroQol group. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 11.Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clinical Nutrition. 2003;22(4):415–421. doi: 10.1016/S0261-5614(03)00098-0. [DOI] [PubMed] [Google Scholar]
- 12.Elia M. The “MUST” report. Nutritional screening of adults: a multidisciplinary responsibility. Worcs, UK: Malnutrition Advisory Group/The British Association for Parenteral and Enteral Nutrition; 2003. [Google Scholar]
- 13.WHO (2000). Consultation on obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization Technical Report Series, vol. 894. [PubMed]
- 14.Coast J, Peters TJ, Richards SH, Gunnell DJ. Use of the EuroQoL among elderly acute care patients. Quality of Life Research. 1998;7(1):1–10. doi: 10.1023/A:1008857203434. [DOI] [PubMed] [Google Scholar]
- 15.Brazier JE, Walters SJ, Nicholl JP, Kohler B. Using the SF-36 and EuroQol on an elderly population. Quality of Life Research. 1996;5(2):195–204. doi: 10.1007/BF00434741. [DOI] [PubMed] [Google Scholar]
- 16.Haywood K, Garratt A, Fitzpatrick R. Quality of life in older people: A structured review of generic self-assessed health instruments. Quality of Life Research. 2005;14(7):1651–1668. doi: 10.1007/s11136-005-1743-0. [DOI] [PubMed] [Google Scholar]
- 17.Dolan P. Modeling valuations for EuroQol health states. Medical Care. 1997;35(11):1095–1108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Fayers PM, Machin D. Clinical interpretation. In: Fayers PM, Machin D, editors. Quality of life, the assessment, analysis and interpretation of patient-reported outcomes. Chichester: Wiley; 2007. pp. 427–455. [Google Scholar]
- 19.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 20.Gombos T, Kertesz K, Csikos A, Söderhamn U, Söderhamn O, Prohaszka Z. Nutritional form for the elderly is a reliable and valid instrument for the determination of undernutrition risk, and it is associated with health-related quality of life. Nutrition Research. 2008;28(2):59–65. doi: 10.1016/j.nutres.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Vailas LI, Nitzke SA, Becker M, Gast J. Risk indicators for malnutrition are associated inversely with quality of life for participants in meal programs for older adults. Journal of the American Dietetic Association. 1998;98(5):548–553. doi: 10.1016/S0002-8223(98)00123-0. [DOI] [PubMed] [Google Scholar]
- 22.Eriksson BG, Dey DK, Hessler RM, Steen G, Steen B. Relationship between MNA and SF-36 in a free-living elderly population aged 70 to 75. The Journal of Nutrition, Health & Aging. 2005;9(4):212–220. [PubMed] [Google Scholar]
- 23.Hickson M, Frost G. An investigation into the relationships between quality of life, nutritional status and physical function. Clinical Nutrition. 2004;23(2):213–221. doi: 10.1016/S0261-5614(03)00127-4. [DOI] [PubMed] [Google Scholar]
- 24.Cruz-Jentoft AJ, Landi F, Topinkova E, Michel JP. Understanding sarcopenia as a geriatric syndrome. Current Opinion in Clinical Nutrition and Metabolic Care. 2010;13(1):1–7. doi: 10.1097/MCO.0b013e328333c1c1. [DOI] [PubMed] [Google Scholar]
- 25.Bhat RS, Chiu E, Jeste DV. Nutrition and geriatric psychiatry: A neglected field. Current Opinion in Psychiatry. 2005;18(6):609–614. doi: 10.1097/01.yco.0000186814.08826.db. [DOI] [PubMed] [Google Scholar]
- 26.Yan LL, Daviglus ML, Liu K, Pirzada A, Garside DB, Schiffer L, Dyer AR, Greenland P. BMI and health-related quality of life in adults 65 years and older. Obesity. 2004;12(1):69–76. doi: 10.1038/oby.2004.10. [DOI] [PubMed] [Google Scholar]
- 27.Soltoft F, Hammer M, Kragh N. The association of body mass index and health-related quality of life in the general population: Data from the 2003 health survey of England. Quality of Life Research. 2009;18(10):1293–1299. doi: 10.1007/s11136-009-9541-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Groessl EJ, Kaplan RM, Barrett-Connor E, Ganiats TG. Body mass index and quality of well-being in a community of older adults. American Journal of Preventive Medicine. 2004;26(2):126–129. doi: 10.1016/j.amepre.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 29.Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obesity Reviews. 2007;8(1):41–59. doi: 10.1111/j.1467-789X.2006.00248.x. [DOI] [PubMed] [Google Scholar]
- 30.Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obesity Reviews. 2001;2(3):173–182. doi: 10.1046/j.1467-789x.2001.00032.x. [DOI] [PubMed] [Google Scholar]
- 31.Kyle UG, Kossovsky MP, Karsegard VL, Pichard C. Comparison of tools for nutritional assessment and screening at hospital admission: A population study. Clinical Nutrition. 2006;25(3):409–417. doi: 10.1016/j.clnu.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 32.Krabbe, P., & Weijnen, T. (2003). Guidelines for analysing and reporting EQ-5D outcomes. In R. Brooks, R. Rabin, & F. de Charro (Ed.). (pp. 7–8). Dordrecht: Kluwer Academic Publishers.
- 33.Amarantos E, Martinez A, Dwyer J. Nutrition and quality of life in older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001;56(2):54–64. doi: 10.1093/gerona/56.suppl_2.54. [DOI] [PubMed] [Google Scholar]
- 34.Cline CM, Willenheimer RB, Erhardt LR, Wiklund I, Israelsson BY. Health-related quality of life in elderly patients with heart failure. Scandinavian Cardiovascular Journal. 1999;33(5):278–285. doi: 10.1080/14017439950141524. [DOI] [PubMed] [Google Scholar]
- 35.Linzer M, Spitzer R, Kroenke K, Williams JB, Hahn S, Brody D, deGruy F. Gender, quality of life, and mental disorders in primary care: Results from the PRIME-MD 1000 study. American Journal of Medicine. 1996;101(5):526–533. doi: 10.1016/S0002-9343(96)00275-6. [DOI] [PubMed] [Google Scholar]
- 36.Orfila F, Ferrer M, Lamarca R, Tebe C, Domingo-Salvany A, Alonso J. Gender differences in health-related quality of life among the elderly: The role of objective functional capacity and chronic conditions. Social Science and Medicine. 2006;63(9):2367–2380. doi: 10.1016/j.socscimed.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 37.Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Nevitt M, Harris TB. Weight change and the conservation of lean mass in old age: The health, aging and body composition study. The American Journal of Clinical Nutrition. 2005;82(4):872. doi: 10.1093/ajcn/82.4.872. [DOI] [PubMed] [Google Scholar]