Abstract
Background:
Peripheral giant cell granuloma is one of the reactive hyperplastic lesions of the oral cavity, which originates from the periosteum or periodontal membrane following local irritation or chronic trauma. The purpose of this study was to present the clinical characteristics of peripheral giant cell granuloma in a group of Iranian population.
Methods:
A series of 123 consecutive confirmed cases of peripheral giant cell granuloma after biopsy were evaluated. Age, sex, anatomic location, consistency, etiologic factor, pain and bleeding history, color, surface texture, and pedicle situation were recorded and were analyzed by chi-square test and values were considered to be significant if P < 0.05.
Results:
Age ranged from 6 to 75 years (mean 33 years). Women affected more than men (M/F 1:1.1). Peripheral giant cell granuloma was seen in the mandible more than in the maxilla and in the anterior region more than in the posterior region. In most cases, lesions were pink, pedunculated and had non-ulcerated surface. In less than half of the cases, there was no history of bleeding and also pain was rarely reported. Calculus was the most common etiologic factor.
Conclusion:
The results confirmed that the clinical features of peripheral giant cell granuloma in a group of Iranian population are almost similar to those reported by other investigators.
Keywords: Giant cell epulis, giant cell granuloma, trauma
Introduction
Chronic trauma can induce inflammation, produce granulation tissue with endothelial cells, chronic inflammatory cells and fibroblasts proliferation and manifests as an overgrowth called reactive hyperplasia.1 These tumor-like lesions are not neo-plastic, but they indicate a chronic process in which an exaggerated repair occurs (granulation tissue and formation of scars) following injury.2,3
Reactive hyperplastic lesions are categorized to several groups.1 Peripheral giant cell granuloma (PGCG) is one of the most frequent giant cell lesions of the jaws and originates from the connective tissue of the periosteum or the periodontal membrane.4 It is not a true neoplasm but rather a benign hyperplastic reactive lesion occurred4 in response to local irritation such as tooth extraction, poor dental restorations, ill-fitting dentures, plaque, calculus, food impaction and chronic trauma (Figure 1).5 Other names of this lesion are peripheral giant cell tumor, osteoclastoma, reparative giant cell granuloma, giant cell epulis and giant cell hyperplasia of the oral mucosa.4
Figure 1.

Initial appearance of peripheral giant cell granuloma
Histologically, PGCG is described as a non-encapsulated mass of tissue, containing numerous multinucleate osteoclast-like giant cells lying in a very cellular and vascular stroma (Figure 2).6
Figure 2.
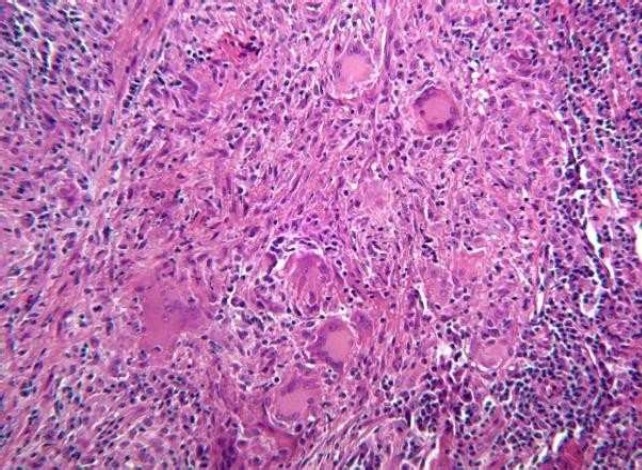
Histological appearance of peripheral giant cell granuloma. Fibrillar and reticular connective tissue stroma with abundant young connective tissue cells of fusiform shape, and multinucleated giant cells (H&E stain, magnification X400).
Clinically, PGCG manifests as a firm, soft, bright nodule or as a sessile or pedunculated mass and with occasionally ulcerated surface. The color, ranges from dark red to purple or blue.4 It is located in the interdental papilla, edentulous alveolar margin or at the marginal gingival level.4,5,7,8
They vary in size, though are rarely reported to exceed 2 cm in diameter.9 However, there have been reports of masses in excess of 5 cm, where factors such as deficient oral hygiene or xerostomia appear to play an important role in lesion growth.4 Incipient lesions may bleed and induce minor changes in gingival contour but large ones adversely affect normal oral function.4 Pain is not a common characteristic, unless they interfere with occlusion, in which case they may ulcerate and become infected.9 In some cases the underlying bone, suffers erosion and cup-shaped radiolucency occurs.1 The lesion can develop at any age. It is, however, more common in the fifth and sixth decades of life with a slight female predilection.5
Treatment comprises surgical resection, with extensive clearing of the base of the lesion to avoid relapse.5 The characteristics and clinical behavior of PGCG may vary in different populations and be difficult to predict, reflecting different environmental influences, lifestyles, and racial factors, assessment of which may help in the diagnosis and management. Information regarding gender, age, signs, and symptoms may be useful and lead to an early diagnosis and proper management, preventing further damage to hard and soft tissues of involved areas.
The purpose of this study was to describe the clinical features of 123 cases of PGCG at Tehran School of Dentistry, during a 4-year period
Materials and Methods
The objective of this case series study was determination of clinical characteristics of all cases of PGCG that were biopsied and examined histologically at Tehran School of Dentistry between April 2001 and April 2005.
After preparing a medical chart on patients’ age and sex and characteristics of lesion such as anatomic location, color, consistency, characteristics of lesion base (pedunculated or sessile), patients with oral lesions with a PGCG like lesion (PGCG was one of the differential diagnosis of their oral lesions) were examined and charts were filled out. Then, for certain diagnosis and treatment, patients were referred to department of Oral Surgery for biopsy. After diagnosis of PGCG, the microscopic slides were reviewed by a second pathologist to confirm the histological diagnosis of PGCG.
The data collected by examining patients including age, sex and characteristics of lesions such as anatomic location, color, consistency, characteristics of lesion base (pedunculated or sessile), characteristics of surface, etiologic factor and a history of bleeding or pain were analyzed by chisquare test and values were considered to be significant if P < 0.05.
Results
During the 4-year period, 123 cases of PGCG of oral cavity were biopsied and examined histologically at Tehran School of Dentistry.
Age:
The mean age of the patients was 33 years (age range 6-75 years).
Sex:
Out of 123 patients, 52.8% were females and 47.2% were males and the difference was not significant.
Anatomic location:
PGCG was seen in the mandible (64.6%) more than in the maxilla (35.3%) and in the anterior region ”canine to canine region” (57.7%) more than in the posterior region “first premolar to back” (42.35%). The most common sites in descending order were posterior of the mandible (35.2%), anterior of the mandible (29.5%), anterior of the maxilla (28.2%), posterior of the maxilla (7.1%).
Consistency and pedicle:
In 73.2% of cases, consistency was firm and in 61% of cases lesions were pedunculated.
Surface characteristics, bleeding, color of lesion and pain:
Ulcerated surface was seen in 45% of cases, probably because of trauma. In 60% of cases, the tendency to bleed was noted. The color of lesions in most cases was pink. Purple, pinkred, and red colors were less frequent. In 96% of cases, there was no history of pain and in remaining cases, dull and slight pain was reported.
Etiological factor:
In 40% of cases, no etiologic factor was found and in 31.8% of cases, calculus was the main etiologic factor. Other factors were inappropriate fillings, removable and fixed partial dentures and fracture in tooth structure.
Discussion
Peripheral giant cell granuloma is a benign hyperplastic lesion caused by local trauma or chronic trauma. It originates from the periodontal ligament or mucoperiosteum.4
Tehran is the most crowded city in Iran with a population of over 7 millions and School of Dentistry at Tehran University of Medical Sciences is the main referral center for patients with various oral cavity diseases.
In this study, the age of patients ranged from 6 to 75 years with the mean age of 33 years and with the highest incidence in the fourth decade of life, similar to other studies mentioned below. Shafer and Levy,10 Giansanti and Waldron11 and Reichart and Philipsen12 reported the average age of 30 years. Katsikeris et al believed the peak incidence to be between 4thand 5thdecades.8 Motamedi et al reported the average age of 31 years.5
PGCG affects females more than males,2,7,8,11 with a proportion of 1:1.5 or 1:2 according to Reichart and Philipsen12 or Giansanti and Waldron studies11 respectively. However Bhaskar et al,13 Salum et al,14 Zhang et al15 and also Murat et al16 reported a slight predilection for the male sex. But in some studies, PGCG had an equal prevalence in both genders.3,5 In our study, females were affected more than males, but the difference was not significant.
PGCG is more common in the lower jaw rather than the upper jaw.5,11,17 The reported proportion is 2.4:1 and in most cases, it occurs anterior to molar region.1,7,11,12 However, according to Pindburg18 the preferential location is the premolar and the molar zones. According to Motamedi et al, PGCG more frequently involves the mandible, commonly in the areas posterior to canines.5 In this study, lesions occurred more in the mandible and in the anterior region.
The consistency of lesions was dependent on the age of lesions because as time passes, maturation of lesions (increasing in collagen fibers) occurs and consistency shifts from soft to firm. In most studies, superiority in pedicle type was not mentioned.1,2,19 Regezi et al noted that PGCG was sessile,3 but in this study most lesions were pedunculated. Ulceration and bleeding can occur secondary to trauma.3 In this study more than one half of the cases had normal (non-ulcerated) surface. Pain was a rare finding in this study and it was not mentioned in similar studies either. Different etiologic factors were associated with PGCG, including complicated dental extractions, dental restorations in poor conditions, food impaction (dental apposition), plaque, calculus, etc.8,20,21 In this study, there was no etiologic factor in more than half of the cases, and calculus was the most causal factor.
On the other hand, Gunhan et al22 in their study on 26 PGCG cases suggested that these lesions could be influenced by sex hormones, and the giant cells were to be a potential target for estrogen (but not progesterone) action.4 In rare cases, giant cell granulomas are oral manifestations of hyperparathyroidism, when multiple lesions are identified and the patient suffers recurrences in spite of adequate treatment.4,10 The lesions typically associated with hyperparathyroidism appear centrally in bone and are referred to as brown tumors. In the lower jaw, these intrabony lesions can perforate the cortical layer, spreading towards the soft tissues and imitating a peripheral lesion.4 A parathyroid tumor or chronic renal failure primarily or secondarily can give rise to increased parathyroid hormone (PTH) production, which in turn favors the formation of giant cell lesions. Children with hypophosphatemic rickets (subclinical hyperparathyroidism) are also at an increased risk of developing such lesions. Histologically, brown tumors cannot be distinguished from giant cell granulomas.4
The treatment of PGCG comprises surgical resection with elimination of the entire base of the lesion and suppression of the etiologic factor. If resection is only superficial, the growth may recur. Most lesions respond satisfactorily to thorough surgical resection, with exposure of all the bone walls. When the periodontal membrane is affected, extraction of the adjacent teeth may prove necessary to insure full resection though this is initially contraindicated.4,23
In conclusion, the early and precise diagnosis of PGCG, allows conservative management with a less risk for teeth and adjacent bone.4
Acknowledgments
The authors thank Shabnam Shadman for her editorial comments and Dr. Kharazifard for statistical analysis.
References
- 1.Wood NK, Goaz PW. 5th ed. St.Louis: Mosby; 1997. Differential Diagnosis of Oral and Maxillofacial Lesions; pp. 141–2. [Google Scholar]
- 2.Carvalho YR, Loyola AM, Gomez RS, Araujo VC. Peripheral giant cell granuloma. An immunohisto-chemical and ultrastructural study. Oral Dis. 1995;1(1):20–5. doi: 10.1111/j.1601-0825.1995.tb00152.x. [DOI] [PubMed] [Google Scholar]
- 3.Regezi JA SJJR. 5th ed. St.Louis: WB. Saunders; 2007. Oral Pathology: Clinical Pathologic Correlations; pp. 112–3. [Google Scholar]
- 4.Chaparro-Avendano AV, Berini-Aytes L, Gay-Escoda C. Peripheral giant cell granuloma. A report of five cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2005;10(1):53–7. [PubMed] [Google Scholar]
- 5.Motamedi MH, Eshghyar N, Jafari SM, Lassemi E, Navi F, Abbas FM, et al. Peripheral and central giant cell granulomas of the jaws: a demographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(3):e39–e43. doi: 10.1016/j.tripleo.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 6.Flaitz CM. Peripheral giant cell granuloma: a potentially aggressive lesion in children. Pediatr Dent. 2000;22(3):232–3. [PubMed] [Google Scholar]
- 7.Shafer WG, Hine MK, Levy BM. 4th ed. Philadelphia: W.B. Saunders; 1983. Textbook of Oral Pathology; pp. 144–6. [Google Scholar]
- 8.Katsikeris N, Kakarantza-Angelopoulou E, Angelopoulos AP. Peripheral giant cell granuloma. Clinicopathologic study of 224 new cases and review of 956 reported cases. Int J Oral Maxillofac Surg. 1988;17(2):94–9. doi: 10.1016/s0901-5027(88)80158-9. [DOI] [PubMed] [Google Scholar]
- 9.Gandara-Rey JM, Pacheco Martins Carneiro JL, Gandara-Vila P, Blanco-Carrion A, Garcia-Garcia A, Madrinan-Grana P, et al. Peripheral giant-cell granuloma. Review of 13 cases. Med Oral. 2002;7(4):254–9. [PubMed] [Google Scholar]
- 10.Shafer WG, Hine MK, Levy BM, Tomich CE. 4th ed. Mexico city: Guanabara Koogan; 1987. Tratado de patologia bucal; pp. 143–5. [Google Scholar]
- 11.Giansanti JS, Waldron CA. Peripheral giant cell granuloma: review of 720 cases. J Oral Surg. 1969;27:787–91. [PubMed] [Google Scholar]
- 12.Reichart P, Philipsen H P. Peripheral giant cell granuloma: review of 720 cases. J Oral Surg. 2000:164. Atlas de Patologia Oral Barcelona: Masson; 2000 p 164. [PubMed] [Google Scholar]
- 13.Bhaskar SN, Cutright DE, Beasley JD, III, Perez B. Giant cell reparative granuloma (peripheral): report of 50 cases. J Oral Surg. 1971;29(2):110–5. [PubMed] [Google Scholar]
- 14.Salum FG, Yurgel LS, Cherubini K, De Figueiredo MA, Medeiros IC, Nicola FS. Pyogenic granuloma, peripheral giant cell granuloma and peripheral ossifying fibroma: retrospective analysis of 138 cases. Minerva Stomatol. 2008;57(5):227–32. [PubMed] [Google Scholar]
- 15.Zhang W, Chen Y, An Z, Geng N, Bao D. Reactive gingival lesions: a retrospective study of 2, 439 cases. Quintessence Int. 2007;38(2):103–10. [PubMed] [Google Scholar]
- 16.Muratakgül H, Güngrmü M, Harorli A. Peripheral giant cell granuloma. a clinical and radiological study. 2004;16(1):59–63. [Google Scholar]
- 17.Bodner L, Peist M, Gatot A, Fliss DM. Growth potential of peripheral giant cell granuloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83(5):548–51. doi: 10.1016/s1079-2104(97)90118-9. [DOI] [PubMed] [Google Scholar]
- 18.Pindborg JJ. 5th ed. London: Wiley-Blackwell; 1995. Atlas of Diseases of the Oral Mucosa; p. 186. [Google Scholar]
- 19.Greenberg MS, Glick M. 11th ed. Hamilton, Ontario: BC Decker Inc; 2008. Burket’s Oral Medicine; p. 134. [Google Scholar]
- 20.Angelopoulos AP. Pyogenic granuloma of the oral cavity: statistical analysis of its clinical features. J Oral Surg. 1971;29(12):840–7. [PubMed] [Google Scholar]
- 21.Shields JA. Peripheral giant-cell granuloma: a review. J Ir Dent Assoc. 1994;40(2):39–41. [PubMed] [Google Scholar]
- 22.Gunhan M, Gunhan O, Celasun B, Mutlu M, Bostanci H. Estrogen and progesterone receptors in the peripheral giant cell granulomas of the oral cavity. J Oral Sci. 1998;40(2):57–60. doi: 10.2334/josnusd.40.57. [DOI] [PubMed] [Google Scholar]
- 23.Warrington RD, Reese DJ, Allen G. The peripheral giant cell granuloma. Gen Dent. 1997;45(6):577–9. [PubMed] [Google Scholar]


