Abstract
Objective
Based on social ecological theory, this study examined the joint relations among adolescents’ family, peer, and school contexts and depressive symptoms in youth with spina bifida using cumulative, protective, and specific effects models.
Method
Sixty families of adolescents with spina bifida and 65 comparison families reported on adolescent’s positive experiences within these contexts and on depressive symptoms when youth were 14–15 and 16–17 years old.
Results
Adolescents with spina bifida had fewer total positive contexts and less positive experience within peer and school contexts, as compared to typically developing adolescents. Greater total number of positive contexts and higher levels of positive experiences within family and school contexts were associated with fewer depressive symptoms for both groups; peer positive experiences were related to lower depressive symptoms for typically developing adolescents only.
Conclusion
Adolescents with spina bifida have fewer positive contexts, which may place them at risk for higher levels of depressive symptoms.
Keywords: Spina bifida, adolescence, depression, family functioning, school functioning, peers
The Impact of Family, Peer, and School Contexts on Depressive Symptoms in Adolescents with Spina Bifida
Research based on social ecological theory has consistently demonstrated that adolescent psychological functioning is shaped by the reciprocal influences of intrapersonal characteristics and contextual features inherent within social ecologies. (Bronfenbrenner, 1979, 2004; Brown, 2002). Because youth are actively involved in many contexts simultaneously, their development is shaped by a combination of their experiences across all of these contexts. Recently, comprehensive models (e.g., cumulative effects models; Evans, Kim, Ting, Tesher, & Shannis, 2007) have been used to more clearly delineate the complex manner in which factors across multiple contexts jointly affect adolescent psychosocial outcomes through their mutual relations (Morales & Guerra, 2006; Simmons & Blyth, 1987). However, studies examining joint effects of multiple social contexts have been rare within the child health psychology literature. Generally, studies in pediatric psychology have focused on independent effects of factors present within family, peer, or school contexts on child health outcomes, with little acknowledgement that adolescents’ psychosocial development is influenced by a combination of their experiences across these various social contexts (Brown, 2002).
The purpose of this study was to apply a social-ecological framework to the study of psychological functioning in a pediatric sample of adolescents with spina bifida. The first aim of this study was to determine the impact of spina bifida on youths’ functioning by comparing reports of their positive experiences within three contexts—family, peers, and school—to those of a matched sample of typically developing youth. Changes in reports of positive experiences within these contexts were also examined for both groups over early to middle adolescence. A second aim of this study was to examine the potential psychological benefits that adolescents with spina bifida derive from their positive experiences across family, peer, and school contexts. To do this, three effects models—cumulative, protective, and specific effects—were each evaluated for their utility in describing the mechanisms through which adolescents’ positive experiences within these social contexts combine to influence the development of depressive symptoms, both independently and through their joint effects.
Adolescents with spina bifida encounter unique challenges associated with their physical disability. This congenital neural tube defect, which affects approximately 18 of every 100,000 live births in the United States annually (CDC, 2008), is characterized by a lesion along the spinal column and distinct brain malformations (i.e., hydrocephalus and Chiari II malformation) that result in a number of motor, sensory, autonomic, and cognitive impairments such as paraplegia, bladder and bowel dysfunction, clubfoot and other orthopedic conditions, and neurocognitive deficits in the areas of visuospatial processing, attention, memory, and higher-order language abilities (Burmeister, Hannay, Fletcher, Boudousquie, & Dennis, 2005; Dennis et al., 2004; Sandler, 1997). During adolescence, functional limitations associated with these impairments affect the way in which youth with spina bifida interact with their environments within family, peer, and school contexts. For example, mobility limitations that require ambulation with a wheelchair or other assistive equipment, intermittent catheterization toileting regimen and other demanding medical management tasks, and difficulties with social skills and social performance (Holmbeck et al., 2003; Sandler, 1997), are just a few examples of spina bifida-related factors that require special support from others and necessitate additional resources from the various social contexts in which these adolescents are engaged. In this study, spina bifida was conceptualized as an intrapersonal factor that influences these adolescents’ experiences and interactions within family, peer, and school contexts.
This study’s focus on factors contributing to the onset of depressive symptoms in adolescents with spina bifida is an important area of inquiry for several reasons. First, because rates of depressive symptoms generally increase during middle adolescence (Garber, Keiley, & Martin, 2002; Steinberg & Morris, 2001) and youth with spina bifida are at greater risk of developing internalizing symptoms (i.e., depression and anxiety symptoms; Appleton et al., 1997; Cate, Kennedy, & Stevenson, 2002; Holmbeck et al., 2003; Lavigne & Faier-Routman, 1992), adolescents with spina bifida are particularly vulnerable to developing depression. Furthermore, given that youth who experience adolescent-onset of depressive symptoms are more likely to have recurrent episodes of depression throughout adulthood (Graber, 2004), and that depression negatively impacts capacity for self-care, employment, and other areas of functioning (Judd et al., 2000), research on factors contributing to depressive symptoms in youth with spina bifida has direct implications for preventing not only depression, but also associated functional impairments, in a group of youth that are most at risk for these problems.
A central focus of this study is the potential benefits that adolescents with spina bifida gain through their positive experiences within the multiple social contexts in which they are embedded. Empirical findings from previous studies on youth psychological functioning provide support for this focus on positive experiences; there is substantial evidence that positive experiences within family, peer, and school contexts promote adaptive outcomes in adolescents. Within the family context, parental acceptance and support have been found to be directly related to positive adolescent self-perceptions (Petersen, Leffert, Graham, Alwin, & Ding, 1997). Although parent-child relationships remain an important source of support for all youth, the positive experiences within the family environment may be an especially relevant resource for adolescents with spina bifida. These youth continue to rely on parents for assistance with daily medical care needs well into young adulthood, thus maintaining closer contact with parents and preserving social connections with them, as well. Typically developing adolescents, conversely, disengage from the family during middle adolescence in favor of spending increased time in the company of peers or involvement in activities outside the home (Holmbeck, 2002; Larson, Richards, Moneta, Holmbeck, & Duckett, 1996).
With respect to the peer context, studies examining connections between peer interactions and depressive symptoms have generally focused on the effects of negative peer experiences on psychological functioning (Graber, 2004) with little investigation into ways in which positive peer relations might bolster psychological health. However, there is consistent evidence that other adaptive psychosocial outcomes, such as pro-social behaviors, may be encouraged through positive peer affiliations (Mounts & Steinberg, 1995). Because youth with spina bifida have smaller social networks (Ellerton, Stewart, Ritchie, & Hirth, 1996) and fewer friends (Holmbeck et al., 2010), have less social acceptance from peers (Holmbeck et al., 2010), and experience greater social isolation as compared to typically developing youth (Borjeson & Lagergren, 1990), they may have less opportunity for positive peer experiences.
Finally, findings from previous studies indicate that the school context also has a significant impact on a variety of adolescent psychological outcomes, such as self-esteem (Shiu, 2001) and general social-emotional well-being (Eccles et al., 1993). Specifically, youth with spina bifida may have fewer positive school experiences because of their difficulties with academic achievement (due to neuropsychological deficits; Rose & Holmbeck, 2007; Wills, 1993), extended absences from school following repeated invasive medical interventions, and the obstacles they encounter in performing necessary medical self-care tasks (e.g., catheterization). In summary, findings from previous studies suggest that positive experiences within family, peer, and school contexts independently contribute to adaptive psychological outcomes in youth. However, due to factors related to their medical condition, adolescents with spina bifida may have less access to these resources within peer and school contexts, which may, in turn, negatively impact psychological outcomes.
The first aim of this study was to compare positive family, peer, and school experiences across time and across groups (spina bifida versus typically developing adolescents). The inclusion of a carefully matched comparison sample of typically developing adolescents in this study allowed for conclusions about the degree to which having a chronic physical disability such as spina bifida affects adolescents’ positive experiences within particular social contexts. Fewer positive experiences for adolescents with spina bifida would indicate that having this physical disability adversely affects adolescents’ functioning within these contexts. Comparisons of mean levels of positive experiences within social contexts over time also provide important information about how adolescents’ experiences within those contexts change as they grow older. Finally, examination of differential levels of positive experiences across the various social contexts provides information about functioning in different settings. Based on the reviewed literature, it was predicted that adolescents with spina bifida would have fewer total number of social contexts that could be designated as “positive”. Specifically, they were expected to have significantly fewer positive experiences in the peer and school contexts and more positive family experiences, as compared to typically developing youths. Furthermore, positive peer experiences were expected to increase, and positive family experiences were expected to decrease, for youth in the comparison group. However, no significant variations in positive family, peer, or school experiences were expected for adolescents with spina bifida over this time period.
The second aim of this study was to evaluate the relative utility of three effects models in describing associations among adolescents’ positive experiences across multiple contexts and their psychological outcomes. Within the child development literature, various effects models (e.g., cumulative risk models, risk-protection models; Morales & Guerra, 2006; Stouthamer-Loeber, Loeber, Wei, Farrington, & Wilkstrom, 2002) have been used successfully to test the complex relations among contextual stressors and intrapersonal domains in predicting negative psychosocial outcomes, such as youth delinquency. However, evaluations of multiple positive contextual influences in predicting positive youth adjustment outcomes are more rare (Schwartz, Pantin, Coatsworth, & Szapocznik, 2007), especially in the studies involving youth with chronic health conditions. In this study, cumulative, specific, and protective effects models were each examined cross-sectionally and longitudinally to determine whether positive contextual experiences had an immediate association with, or a longer-term effect on, psychological adjustment.
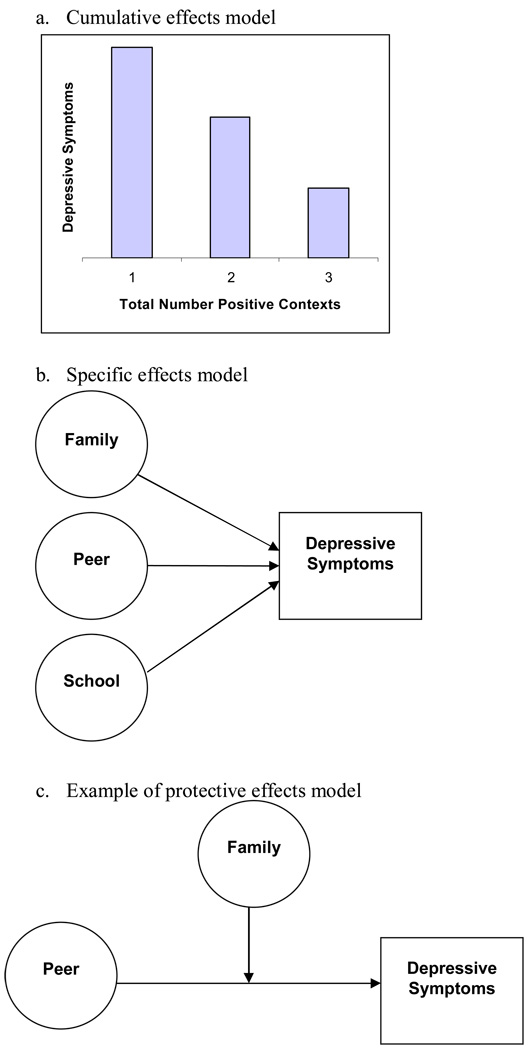
The first set of analyses, the cumulative effects tests (see Figure 1a), was used to determine whether adolescents demonstrate incrementally better psychological outcomes with greater total numbers of positive contexts. For both adolescents with spina bifida and for typically developing adolescents, positive experiences were expected to demonstrate a cumulative effect on depressive symptoms. Next, a specific effects model (see Figure 1b) was employed to assess the relative strength of the family, peer, and school contexts in predicting depressive symptoms for each of the samples. Whereas positive experiences within the family context were expected to be the strongest predictor of depressive symptoms for adolescents with spina bifida, the peer context was expected to have the strongest influence on psychological adjustment for typically developing adolescents. Finally, the protective effects model (see Figure 1c), evaluated interactions between contexts. This model was used to determine whether positive experiences within one context mitigated the effects of less positive experiences in another social context. For adolescents with spina bifida, positive family experiences were expected to protect against the negative effects of having less positive peer and school experiences. For adolescents in the comparison group, positive experiences within the peer and school contexts were expected to buffer the negative effects of less positive family experiences.
Figure 1.
Models of proposed cumulative, specific, and protective effects.
Method
Participants
Participants in this study were part of a larger, longitudinal study examining psychosocial adjustment of youth with spina bifida during the transition to adolescence, funded by the March of Dimes (e.g., Holmbeck et al., 2003). At the time of the first data collection (Time 1), 68 families of eight- and nine-year-olds with spina bifida (37 males, 31 females; M = 8.34 years) and a matched comparison sample of 68 typically developing eight- and nine-year-olds (M = 8.49 years) were interviewed in their homes. Participants in the typically developing group were matched with those in the spina bifida group on the following demographic variables: child age, child gender, child ethnicity, birth order, family structure (intact versus not intact), socioeconomic status, and age of parents (see Holmbeck et al., 2003, for further details on the demographics of each sample).
Data collection for the larger longitudinal study occurred every two years. The present study included data from the fourth and fifth waves of data collection (Time 4 and Time 5) when adolescents were 14–15 (M = 14.57; SD = 0.65) and 16–17 (M = 16.64; SD = 0.69) years of age, respectively. These time points were chosen because middle adolescence (ages 15–17 years) represents the time of the greatest growth in depressive symptoms within the general population of adolescents (Garber et al., 2002; Ge, Conger, & Felder, 2001; Hankin et al., 1998), making it an opportune time for examining potential contextual factors that contribute to this observed rise in depressive symptoms. At Time 4, 60 families of children with spina bifida participated (88% retention rate) and 65 families in the comparison sample participated (96%). Fifty-two families of adolescents with spina bifida (76%) and 61 families in the comparison group (90%) completed the Time 5 data collection. No differences in age, gender, race, SES, or child receptive language abilities were found between families who participated in study procedures at these time points versus those who did not.
Children with spina bifida were originally identified and recruited from four sources: a children’s hospital, a children’s hospital that cares exclusively for children with physical disabilities, a university-based medical center, and a statewide spina bifida association. The majority of youth with spina bifida had myelomeningocele (82%); 12% had lipomeningocele, and 6% had another type of spina bifida. The location of spinal lesion also varied, with 32% sacral, 54% had a lumbosacral or lumbar, and 13% thoracic. Most children with spina bifida had a shunt (71%), with an average of 2.50 (SD = 2.91) shunt surgeries at Time 1. Sixty-three percent of participants with spina bifida ambulated with braces, 18% used a wheelchair, and 19% walked unassisted. The final sample of 68 children did not differ significantly from children of families who declined to participate in terms of lesion level, χ2 (2, N = 116) = 0.62, p > .05, or type of spina bifida, χ2 (1, N = 119) = 1.63, p > .05.
Families in the comparison group were recruited by contacting schools in which participating children with spina bifida were enrolled (see Holmbeck et al., 2003 for a more detailed description of recruitment and matching procedures). Within the final sample of participating families, all adolescents and biological mothers took part in the study. Fifty-five (81%) biological fathers/step-fathers of children with spina bifida and 52 (76%) biological/step-fathers of typically developing children also participated. The majority of families were White (n = 113; 86.76%), but the sample was diverse with respect to socioeconomic status (M = 44.79; SD = 21.46), as measured by the Hollingshead Four Factor Index (1975) of socioeconomic status.
Procedure
Prior to data collection, human subjects’ approval was granted by Institutional Review Boards (IRBs) from the researchers’ home institution and at all cooperating hospitals from which participants were recruited. Data for each wave of the study were collected during three-hour visits to each family’s home. Data collection was conducted by trained graduate and undergraduate research assistants. Each session began with a brief overview of study goals and a review of confidentiality issues. Parents provided consent for themselves and their adolescents to participate and adolescents provided assent for their own participation. Parents also signed a release of information form for medical chart reviews and for the adolescent’s teacher to complete a set of questionnaires. Families then completed several questionnaire packets, a series of videotaped family interaction tasks, and audio-taped self-interviews. To aid comprehension of measures, research assistants were available to read questionnaires aloud to participants when needed and laminated cards illustrating Likert-scale item response options were used to facilitate accurate responses. Families were paid $100 for their participation at Time 4 and again at Time 5.
Measures
Data used for the current study were obtained through mother-, father-, adolescent-, and teacher-report on questionnaire measures. To decrease the impact of common method variance, mother-, father-, and teacher-report data were used for the independent variables (i.e., positive family, peer, and school experiences), and adolescent-report was used for the dependent variable (i.e., depressive symptoms).
Family context
A measure of parental acceptance and a measure of family cohesion were combined to form the Family Context (see Results for details on procedures for combining scales to form context composites). Mother- and father-reported parental acceptance was assessed with the eight “acceptance” items from the acceptance/rejection domain of the Child Report of Parental Behavior Inventory (CRPBI; Schuldermann & Schuldermann, 1970), which had been adapted for responses by parents. Items assessing a range of parenting behaviors were rated by respondents on a three-point scale ranging from, “not like”, “somewhat like”, or “a lot like” the parent. Across the two time points and reporters, α values ranged from .78 to .86. Family cohesion was assessed with mother- and father-report on the nine “cohesion” subscale items from the Family Environment Scale (FES; Moos & Moos, 1981). Responses were recorded on a four-point scale ranging from “strongly disagree” to “strongly agree”. Alpha values ranged from .79 to .82 across the two time points for mother- and father-report.
Peer context
Measures of social competence and social acceptance were combined to form the Peer Context. Social competence was measured with mother- and father-report on the Child Behavior Checklist (CBCL; Achenbach, 1991) social competence subscale. Items assessed adolescents’ participation in social groups and organizations, as well as number of close friends and frequency of contact with friends outside of school. Response format was on a three-point scale, with options “not true”, “somewhat or sometimes true”, and “very true or often true” and higher scores representing more favorable social competence. Scale alphas are not appropriate for this scale, due to the count format of the measure (Achenbach, 1991). Perceived adolescent social acceptance by peers was obtained from mother-, father-, and teacher-report on the three-item social acceptance subscale of Harter’s (1985) Rating Scale of Child’s Actual Behavior. Parent-report of this measure was adapted from the teacher version of the same name. For each item, respondents first choose which one of two response options is most like the adolescent, and then rate whether that response option is “really true” or “sort of true” for the adolescent. Across the two time points and three reporters, α values ranged from .73 to .94.
School context
Measures of scholastic competence and academic grades were combined to form the School Context. Mother-, father-, and teacher-report of adolescent scholastic competence were gathered through responses to items of the Rating Scale of Actual Behavior (Harter, 1985; described above), scholastic competence subscale. Across the two time points and three reporters, α values ranged from .75 to .89. Mothers reported adolescents’ grades from their most recent report card. Grade point averages were computed for four classes (i.e., science, social studies, English, and math) with higher scores indicating better grades.
Depressive symptoms
Adolescent depressive symptoms were assessed with adolescent-report on the Child Depression Inventory (CDI; Kovacs, 1992). This 27-item measure assesses five dimensions of depressive symptoms: Negative Mood, Interpersonal Difficulties, Negative Self-Esteem, Ineffectiveness, and Anhedonia. Respondents rate their degree of depressive symptomatology by choosing among three response options representing three levels of symptom severity (with higher scores indicating a greater degree of depressive symptoms). Internal consistencies were α = .82. and α = .87 at Time 4, and α = .92 and α = .86 at Time 5 for the spina bifida and comparison samples, respectively.
Results
Preliminary Statistical Considerations
Formation of context composites
To limit the number of analyses (thereby decreasing the chance of Type I error), data were combined for each measure for which multiple reports existed. All correlations between reporters for the same measure were above r ≥ .30 and were significant at the p ≤ .01 level (r’s ranged from .31 to .75). Therefore, measures were collapsed across mother, father, and teacher report, as available.
Formation of total number of positive contexts count variable
After combining variables across reporters, the two measures for each context were combined to form each of the Family, Peer, and School context composite indices. Following a z-score transformation, the internal consistency between the two measures contributing to each context was examined. All alpha coefficients were α ≥ .70, and the measures designated for each respective context were combined by computing the mean of the two scales, which had previously been converted into z-scores. This resulted in a single context composite variable for each of the family, peer, and school contexts.
For analyses testing the proposed specific and protective effects models, degree of positive experience within the family, peer, and school contexts were each measured on a continuous metric. To perform analyses examining the potential cumulative effects of positive experiences across multiple contexts, the context composite index scores (measured on a continuous scale) were transformed into dichotomous variables. Adolescents with scores above the total sample mean for a given composite context index were coded as “1” (i.e., indicating sufficient positive experiences to designate the context as overall “positive”), and those with scores below the mean for a given context composite index were coded as “0” (i.e., fewer positive experiences; does not reach level to be designated as “positive” overall). The total number of contexts in which adolescents received a score of “1” was then summed, yielding a total number of positive contexts score, which ranged from “0” to “3”.
Group Differences in Positive Experiences
Total number of positive contexts
As predicted, findings from two independent samples t-tests comparing group differences of total number of positive contexts at Times 4 and 5 supported the hypothesis that adolescents with spina bifida would have fewer positive contexts than typically developing adolescents (see Table 1). Adolescents with spina bifida had significantly fewer total number of positive contexts than did typically developing adolescents at Time 4 [t(131.77) = −3.79, p < .001)] and at Time 5 [t(134) = −3.60, p < .001]. On average, adolescents with spina bifida had 1.03 positive contexts (SD = .99) at Time 4, whereas typically developing adolescents had a mean of 1.72 positive contexts (SD = 1.13) at the same time point. At Time 5, two years later, adolescents with spina bifida averaged 1.01 positive contexts (SD = 1.03) and typically developing adolescents averaged 1.68 positive contexts (SD = 1.11). Effect sizes were d = .65 and d = .63 (both medium effects) at Times 4 and Time 5, respectively.
Table 1.
Independent Samples T-tests Comparing Total Number of Positive Contexts and Mean Levels of Positive Experiences within Family, Peer, and School Contexts Between Adolescents with Spina Bifida and Typically Developing Adolescents at Time 4 and Time 5
| Time 4 | Time 5 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Group | Mean | SD | t | d | Mean | SD | t | d |
| Total Number Positive Contexts |
SB | 1.03 | .99 | −3.79** | .65 | 1.01 | 1.03 | −3.60** | .63 |
| TD | 1.72 | 1.13 | 1.68 | 1.11 | |||||
| Family Context | SB | .01 | .72 | .15 | .02 | .06 | .85 | .63 | .12 |
| TD | −.01 | 1.02 | −.05 | .93 | |||||
| Peer Context | SB | −.34 | .83 | −4.47** | .81 | −.38 | .96 | −4.39** | .83 |
| TD | .33 | .82 | .33 | .73 | |||||
| School Context | SB | −.30 | .87 | −3.15** | .56 | −.34 | .87 | −3.48** | .67 |
| TD | .20 | .91 | .24 | .87 | |||||
p≤.05;
p≤.01;
SB = spina bifida group; TD = typically developing group
Note: Total Number of Positive Contexts and Family, Peer, and School Context variables are on different metric scales. Total Number Positive Contexts range from “0” to “3”; Family, Peer, and School Context are z-scores ranging from negative to positive.
Mean levels of family, peer, and school positive experiences
Six independent samples t-tests were conducted to examine group differences in positive experiences within the family, peer, and school contexts (see Table 1). There were no differences in mean levels of positive family experiences between adolescents with spina bifida and typically developing adolescents at Time 4, t(122) = .15, ns, or at Time 5, t(111) = .63, ns. However, as hypothesized, there were significant group differences in mean levels of positive peer and school experiences. At both time periods, adolescents with spina bifida had significantly less positive experiences in the peer context [Time 4: t(123) = −4.47, p < .001; Time 5: t(94.42) = −4.39, p < .001] and the school context [Time 4: t(123) = −3.15, p < .01; Time 5: t(110) = −3.48, p < .01]. Effect sizes for these four significant findings ranged from d = .56 (medium effect) to d = .83 (large effect)1.
Differences in Positive Experiences Over Time
No support was found for any of the hypothesized changes in total number of positive contexts, or changes in mean levels of positive experiences in specific contexts, from Time 4 to Time 5. Findings indicate that between the ages of 14–15 and 16–17, adolescents in both groups maintained similar levels of comfort within each of the contexts.
Positive Contexts and Depressive Symptoms
Overview of regression analyses
A series of hierarchical multiple regression analyses was conducted to determine whether adolescent family, peer, and school contexts were related concurrently or prospectively to adolescent report of depressive symptoms. To determine whether these effects were moderated by group status (spina bifida or comparison), this variable was included in the analyses as well (dummy coded: 0=spina bifida, 1=comparison). Prior to running the regression analyses, all continuous variables (family, peer, and school context composite variables) were centered by subtracting the sample mean from all individuals’ scores on the variable, producing a revised sample mean of zero (Aiken & West, 1991; Holmbeck, 1997). Separate sets of analyses were run to test each of the cumulative, specific, and protective effects models concurrently at Time 4 and Time 5 and longitudinally from Time 4 to Time 5.
Cumulative effects
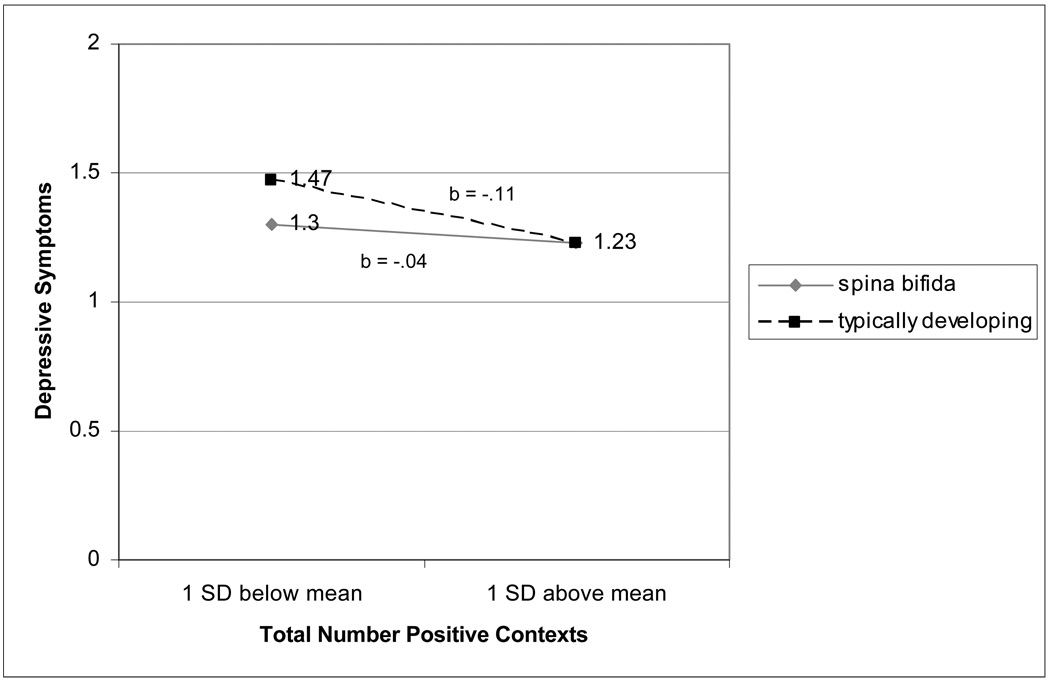
Separate cross-sectional regression analyses were conducted for each time point and longitudinal analyses were conducted to predict change in depressive symptoms from Time 4 to Time 5 with the number of positive contexts at Time 4 as the independent variable. Total number of positive contexts and group status variables were entered in the first step of the regression model and the group status x total number of positive contexts interaction term was entered at Step 2 (see Table 2). At Time 4, group status, β = .19; F(2, 121) = 8.98, p < .05, and adolescents’ total number of positive contexts, β = −.31; F(1, 122) = 13.18, p < .001, were associated with adolescent depressive symptoms. As predicted, greater positive experiences across the three contexts was associated with fewer depressive symptoms; however, comparison group status was unexpectedly related to higher levels of depressive symptoms. The relation between total number of positive contexts and depressive symptoms was moderated by group status, β = −.27; F(3, 120) = 7.50, p < .05, which was probed according to methods suggested by Aiken and West (1991) and Holmbeck (2002). The simple slope for the spina bifida group was nonsignificant β = −.16; F(3, 120) = 7.50, ns, indicating that level of depressive symptoms for adolescents with spina bifida was not associated with their total number of positive contexts at Time 4 (see Figure 2). However, within the comparison group, greater total number of positive contexts was associated with fewer depressive symptoms, β = −.52; F(3, 120) = 7.50, p < .001, as predicted.
Table 2.
Multiple Regression Effects for Group and Total Number of Positive Contexts on Adolescent Depressive Symptoms at Time 4 and Time 5
| Time 4 | Time 5 | |||||||
|---|---|---|---|---|---|---|---|---|
| Step | β | R2 | ΔR2 | F | β | R2 | ΔR2 | F |
| 1. Total Number | −.31 | .10 | .10 | 13.18** | −.44 | .19 | .19 | 25.21** |
| Positive Contexts | ||||||||
| Group | .19 | .13 | .03 | 8.98* | .20 | .23 | .04 | 15.63* |
| 2. Group × Total Number | −.27 | .16 | .03 | 7.50* | .06 | .23 | .00 | 10.40 |
| Positive Contexts | ||||||||
p≤.05;
p≤.01
Figure 2.
Regression lines for relation between total number of positive contexts and depressive symptoms as moderated by group status at Time 4.
At Time 5, group status, β = .19; F(2, 121) = 8.98, p < .05, and adolescents’ total number of positive contexts, β = −.31; F(1, 122) = 13.18, p < .001, were associated with adolescent depressive symptoms. Specifically, typically developing youth reported more depressive symptoms and for adolescents in both the spina bifida and comparison groups, having fewer positive contexts was associated with depressive symptoms.
For the longitudinal analysis examining the association between total number of positive contexts and change in adolescent depressive symptoms over time, adolescent depressive symptoms at the earlier time period (Time 4) was entered into the first step of the analysis, followed by group status and Time 4 total number of positive contexts at Step 2, then the group status x total number of positive contexts two-way interaction variable at Step 3. Total number of positive contexts at the earlier time point did not have a significant long-term effect on adolescents’ depressive symptoms two years later.
Specific effects
In regression analyses examining concurrent relations between levels of positive experiences within the family, peer, and school contexts and depressive symptoms at Time 4 and Time 5, group status was entered in the first step, each of the three positive context variables were entered in Step 2, and three interaction terms representing the moderating effect of group status on the association between positive contexts and depressive symptoms were entered at the third step (see Table 3). At each time point, positive experiences within the school [Time 4: β = −.42; F(1, 108) = 12.49, p < .01; Time 5: β = −.25; F(1, 108) = 7.04, p < .01] and family [Time 4: β = −.25; F(1, 108) = 11.61, p < .01; Time 5: β = −.33; F(1, 108) = 6.81, p < .01] contexts were associated with adolescent depressive symptoms at the respective time points, such that greater positive experiences was associated with fewer depressive symptoms.
Table 3.
Multiple regression effects of group status and Family, Peer, and School Contexts on Adolescent Depressive Symptoms at Time 4 and Time 5
| Time 4 | Time 5 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step | β | R2 | ΔR2 | F | Step | Β | R2 | ΔR2 | F |
| 1. Group | .07 | .01 | .01 | .65 | 1. Group | .80 | .01 | .01 | .69 |
| 2. School Context | −.42 | .17 | .17 | 12.49** | 2. Family Context | −.33 | .11 | .11 | 6.81** |
| Family Context | −.25 | .23 | .05 | 11.61** | School Context | −.25 | .17 | .05 | 7.04* |
| Peer Context | −.16 | .24 | .02 | 9.48 | |||||
| 3. Group × Peer Context | −.39 | .31 | .06 | 10.25** | |||||
p≤.05;
p≤.01
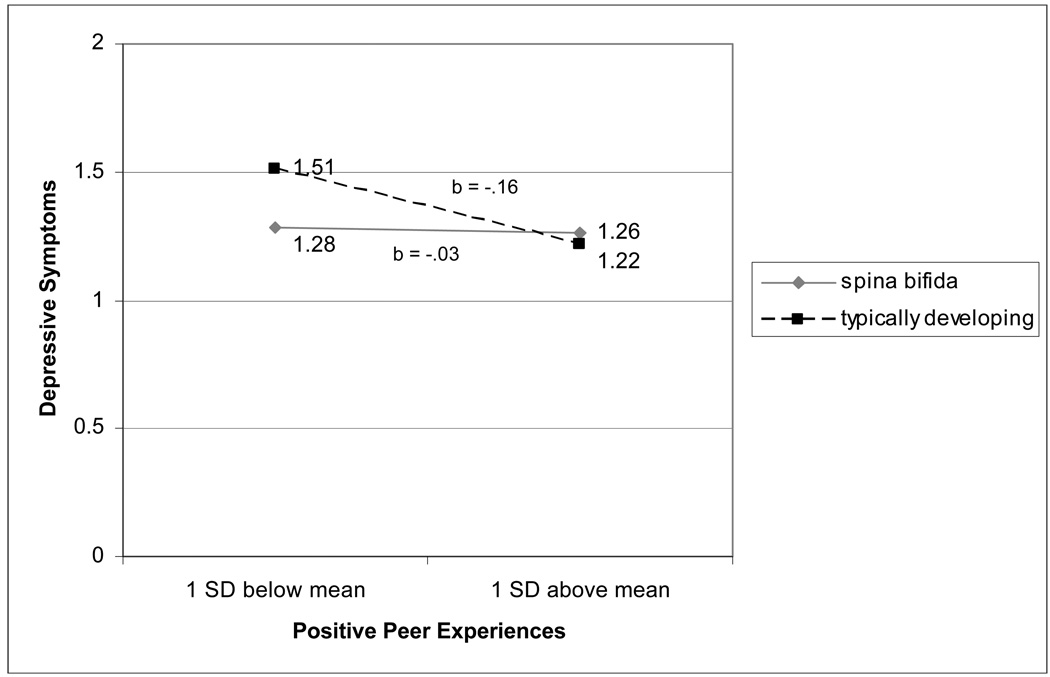
Although there were no main effects for peer positive experiences, a significant moderation effect was found at Time 4 for the relation between positive experiences in the peer context and adolescent depressive symptoms as moderated by group status, β = −.39; F(5, 117) = 10.25, p < .01. Post hoc probing indicated that, for adolescents in the comparison group, greater peer positive experiences was associated with fewer depressive symptoms, β = −.61; F(3, 120) = 8.49, p < .01 (see Table 3 and Figure 3), but was unrelated to depressive symptoms for adolescents with spina bifida. The longitudinal analysis examining associations between family, peer, and school positive experiences and change in depressive symptoms yielded no significant main or interactive effects for family, peer, or school contexts.
Figure 3.
Regression lines for relation between peer context and depressive symptoms as moderated by group status at Time 4.
Protective effects
Cross-sectional and longitudinal regression analyses examining the protective effects of the family, peer, and school contexts were conducted separately for the spina bifida and comparison groups with the interaction terms representing the moderating effect of positive experiences in one context on the association between positive experiences in another context and depressive symptoms entered in the final step. Only significant interaction effects are discussed in this section.
Across the six regression analyses, only the peer context x school context interaction in the analysis involving adolescents with spina bifida at Time 4 emerged as significant, β = .29; F(3, 55) = 3.28, p < .05. Interestingly, this significant interaction effect occurred in an analysis predicting depressive symptoms in adolescents with spina bifida, rather than analyses examining this relation within the comparison group, as had been predicted. The simple slope for the regression line representing low levels of positive experiences in the peer context was significant, β = −.62; F(3, 55) = 4.00, p < .01, and indicated that adolescents with spina bifida with less positive peer experiences reported fewer depressive symptoms at higher levels of school positive experiences. At higher levels of peer positive experiences, school positive experiences were not associated with depressive symptoms.
Discussion
Based on a social ecological framework, this study examined the associations among intrapersonal and contextual domains in predicting depressive symptom outcomes in adolescents with spina bifida. First, as predicted, findings indicate that adolescents with spina bifida have a smaller number of positive contexts as compared to typically developing youth of the same age, with less positive experiences in peer and school contexts, specifically. These findings are consistent with past research describing the struggles of adolescents with spina bifida in these two social contexts. Neurocognitive deficits associated with their condition (Fletcher et al., 1996) often interfere with the academic achievement of youth with spina bifida, and these problems with academics become more pronounced during the high school years when school work demands the use of more abstract language and organizational skills. Adolescents’ challenges with completing daily self-care tasks in the school setting likely also contribute to these reports of less positive school experiences (Katrancha, 2008). Likewise, the lower levels of positive peer experiences reported for adolescents with spina bifida in this study corresponds with findings from previous studies, which have consistently described social isolation (Blum, 1992), fewer number of friends (Holmbeck et al., 2010), and other social adjustment difficulties in these youth. Social skills deficits (Rose & Holmbeck, 2007), mobility limitations (Bier, Prince, Tremont, & Msalt, 2005; Buran, Sawin, Brei, Fastenau, 2004; Schoenmakers, Gulmans, Gooskens, Pruijs, & Helders, 2005), and other spina bifida-related physical disabilities have been suggested as potential factors that interfere with these youths’ peer interactions and inhibit them from participating in normal youth activities (e.g., organized clubs). Although not the focus of this study, future research should continue to investigate possible reasons for social functioning difficulties, as problems with peers have been identified as a major concern for many parents of adolescents with spina bifida (Blum, Resnick, Nelson, & St. Germaine, 1991; Holmbeck et al., 2003).
Reports of positive family experiences were similar for adolescents with spina bifida and typically developing youth at 14–15 and 16–17 years of age. These findings support the prediction that family continues to be a consistent source of support for both groups during this developmental period. Neither group reported changes in total number of positive contexts, or variations in positive experiences in any specific context, between the ages of 14–15 and 16–17 years of age, indicating that any re-organization or shifts within family, peer, and school contexts are subtle, and do not interfere with the positive experiences youth are able to obtain in these contexts.
A major hypothesis of this study was that positive experiences across multiple contexts promote better psychological adjustment in adolescents. This hypothesis was supported from findings utilizing several effects models, although some variability was observed. Regarding the cumulative effects model, having positive experiences across multiple contexts was not a significant determinant of depressive symptoms for youth with spina bifida at ages 14–15 years old; having a greater number of positive contexts was beneficial for typically developing youth at this age. At ages 16–17 years, greater total number of positive contexts was inversely associated with depressive symptoms for both groups of youth. Because more positive contexts had a promotive effect on psychological functioning for typically developing youth at both time points, but these same beneficial effects of multiple positive contexts were not observed for adolescents with spina bifida for several more years, one conclusion from these findings could be that, at the earlier age, adolescents with spina bifida are able to draw support from fewer contexts in order to preserve psychological functioning. However, as they grow older, they, like typically developing youth, benefit from having positive experiences in multiple contexts. This may represent a developmental lag for youth with spina bifida as compared to typically developing adolescents, perhaps indicating that the normative desire to look beyond the family for sources of support and acceptance occurs at a slightly older stage of adolescence for youth with spina bifida. Such developmental lags have been observed in previous investigations of other domains of psychosocial adjustment, as well. For example, a two-year delay in decision-making autonomy was observed in youth with spina bifida, as compared to their able-bodied counterparts (Devine, Wasserman, Gershenson, Holmbeck, & Essner, in press). Such findings suggest that youth with spina bifida follow a normative, but delayed, trajectory of development across a range of psychosocial domains.
Analyses testing the specific effects of positive experiences within the family, peer, and school contexts revealed that, as predicted, positive family and school experiences were inversely associated with depressive symptoms for adolescents with spina bifida and for typically developing youth. A greater degree of positive peer experiences was associated with fewer depressive symptoms of typically developing adolescents at age 14–15, but not at age 16–17. Positive experiences in the peer context had no effect on depressive symptoms of adolescents with spina bifida at either time point. Thus, although positive experiences with peers were found to minimize depressive symptoms for typically developing youth at the earlier time point, overall findings suggest that support, acceptance, and adaptive functioning in the family and school contexts more broadly affect psychological health of all youth throughout adolescence.
Findings generally failed to support the hypotheses for the protective effects model (with only one significant interaction effect). Although the sample size in this study was relatively large as compared to other pediatric studies of youth with spina bifida, it was not sufficient to detect small or medium effects (Aiken & West, 1991). Future studies that employ larger samples of adolescents with spina bifida would be better able to detect significant interaction effects.
This study features several methodological strengths, including a matched comparison sample of typically developing youth, separate reporters for dependent and independent variables as a control for common method variance, and a longitudinal design that allows for observation of changes across time. The emphasis on beneficial effects of positive experiences across multiple social contexts has been a neglected area of study both in the broader literature on youth psychosocial development (Schwartz et al., 2007), but especially in studies involving youth with chronic physical disabilities (Brown, 2002). A move toward this social-ecological approach has the potential to provide important information about ways in which having a physical disability affects adolescents’ experiences of positive interactions within the various social contexts in which they are embedded, and thus can reveal important areas for clinical intervention work aimed at improving social-emotional well-being of these youth.
This study also has several methodological limitations that could be improved upon in future research in this area. First, contextual domains used in this study to represent “positive experiences” were chosen based on their observed associations with adaptive psychosocial outcomes in previous studies. However, future work should continue to investigate other aspects of these contexts that consistently promote psychological health and could also be designated as “positive”. Additionally, participants in the current study were primarily White, which limits the generalizability of these findings to diverse populations of adolescents with spina bifida. Future research should include more diverse samples, with a greater representation of Hispanic families, due to the relatively high rate of spina bifida in this population (Lary & Edmonds, 1996). Finally, other contexts should be considered in future work. For example, the work setting might be an important context that could greatly impact psychological health for some adolescents. Reports in the pediatric psychology literature have suggested that the medical setting is another relevant context that may greatly affect the adjustment of these adolescents (Brown, 2002).
Dichotomization of continuous variables has several advantages as compared to the more common use of independent variables in raw score format. Relevant to the current study, dichotomization facilitates the creation of “promotive factor” indices that represent combinations of contextual factors as they occur in lived experience. This pattern-centered approach (e.g., Schulenberg, Wadsworth, O’Malley, Bachman, & Johnston, 1996), provides meaningful, clinically relevant information about the ways in which adolescent outcomes vary as a function of the various combinations of contextual factors present in their lives (Farrington & Loeber, 2000). Thus, whereas specific effects analyses describe simple, direct associations between single predictor and outcome factors, cumulative analyses following the pattern-centered approach describe the incremental benefits in psychological outcomes that youth derive from experiencing the predictor variable across a wider range of contexts.
However, there are also limitations of dichotomization. Specifically, in this study, when creating the “total number of positive contexts” categorical variable for hypotheses involving the assessment of cumulative positive experiences, cut-off scores used to designate adolescents as “having” versus “not having” generally positive experiences in a particular context were based on the overall sample mean score for each specific context, and were, therefore, sample specific. This method limits the generalizability of findings, as designations of positive experiences could vary widely depending on the sample characteristics, and might potentially alter the study findings. Dichotomization of continuous variables also results in a loss of variability and has been criticized for its potential to limit the strength of associations in analyses, although this disadvantage was not as relevant for this study, given that significant findings were obtained for analyses examining cumulative effects. Furthermore, it must be emphasized that participants with composite scores lower than the sample mean should not be mistakenly referred to as having “negative” experiences within the specific context. Rather, those participants would be considered to experience generally less positive experiences within the specific context.
Several important clinical implications can be drawn from the results of this study. First, given that positive experiences across a range of contexts were associated with psychological adjustment in adolescents with spina bifida, clinicians should be mindful of conducting comprehensive assessments of acceptance, support, and competency across a variety of contexts. Although research has indicated that adolescents with spina bifida continue to report satisfaction with family relationships during adolescence (Coakley, Holmbeck, Friedman, Greenley, & Thill, 2002), the findings of this study indicate that positive family experiences alone do not ensure adaptive psychological outcomes for these adolescents. Thus, caregivers and professionals should encourage adolescents with spina bifida to seek out opportunities for positive interactions in a variety of social contexts. Finally, although positive peer experiences were not associated with depressive symptoms in adolescents with spina bifida in this study, this finding should not be interpreted as evidence that these youth are unaffected by their comparatively lower levels of positive peer experiences. During the transition to young adulthood, the gap between the social functioning of adolescents with spina bifida and typically developing youth appears to widen (Barf et al., 2007), and interpersonal skills often become more relevant for the attainment of other young adult developmental achievements (such as the formation of romantic partnerships and mature, adult friendships). Thus, it is recommended that caregivers and clinicians continue to encourage normative peer relations that would result in positive peer experiences during late adolescence and emerging adulthood.
Acknowledgments
Completion of this manuscript was supported in part by research grants from the March of Dimes Birth Defects Foundation (12-FY01-0098) and the National Institute of Child Health and Human Development (RO1 HD048629). Portions of this research were presented at the meetings of the Society of Research on Adolescence, 2008. The authors wish to thank Ann Walsh Johnson, Joy Ito, Pat McGovern, Pat Braun, Caroline Anderson, David McLone, John Lubicky, the Spina Bifida Association of Illinois, the staff of the spina bifida clinics at Children’s Memorial Hospital, Shriners Hospitals for Children-Chicago, and Loyola University of Chicago Medical Center. We also thank numerous undergraduate and graduate research assistants for help with data collection and data entry. Most importantly, we gratefully acknowledge the contributions to this study by the parents, children, teachers, and health professionals who participated over many years.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/REP
All scale-level t-test comparisons, examined separately for each reporter, were identical to findings of context composite index analyses presented in Table 1, except for non-significant group differences between subscale means of Time 4 father-reported social acceptance, Time 5 father-reported social competence, and Times 4 & 5 mother-reported grade point average
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Appleton PL, Ellis NC, Minchom PE, Lawson V, Boll V, Jones P. Depressive symptoms and self-concept in young people with spina bifida. Journal of Pediatric Psychology. 1997;22(5):707–722. doi: 10.1093/jpepsy/22.5.707. [DOI] [PubMed] [Google Scholar]
- Barf HA, Post MWM, Verhoef M, Jennekens-Schinkel, Gooskens RHJM, Prevo AJH. Life satisfaction of young adults with spina bifida. Developmental Medicine & Child Neurology. 2007;49:458–463. doi: 10.1111/j.1469-8749.2007.00458.x. [DOI] [PubMed] [Google Scholar]
- Bier JB, Prince A, Tremont M, Msalt M. Medical, functional, and social determinants of health-related quality of life in individuals with myelomeningocele. Developmental Medicine and Child Neurology. 2005;47:609–612. [PubMed] [Google Scholar]
- Blum RW, Resnick MD, Nelson R, St Germaine A. Family and peer issues among adolescents with spina bifida and cerebral palsy. Pediatrics. 1991;88:280–285. [PubMed] [Google Scholar]
- Blum R. Chronic illness and disability in adolescence. Journal of Adolescent Health. 1992;13:364–368. doi: 10.1016/1054-139x(92)90029-b. [DOI] [PubMed] [Google Scholar]
- Borjeson MC, Lagergren J. Life conditions of adolescents with myelomeningocele. Developmental Medicine and Child Neurology. 1990;32:698–706. doi: 10.1111/j.1469-8749.1990.tb08430.x. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge: Harvard University Press; 1979. [Google Scholar]
- Bronfenbrenner U, editor. Making human beings human: Bioecological perspectives on human development. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- Brown RT. Society of pediatric psychology presidential address: Toward a social ecology of pediatric psychology. Journal of Pediatric Psychology. 2002;27(2):191–201. doi: 10.1093/jpepsy/27.2.191. [DOI] [PubMed] [Google Scholar]
- Buran CF, Sawin KJ, Brei TJ, Fastenau PS. Adolescents with myelomeningocele: Activities, beliefs, expectations, and perceptions. Developmental Medicine & Child Neurology. 2004;46:244–252. doi: 10.1017/s0012162204000404. [DOI] [PubMed] [Google Scholar]
- Burmeister R, Hannay HJ, Fletcher JM, Boudousquie A, Dennis M. Attention and executive functions in children with spina bifida meningomyelocele. Child Neuropsychology. 2005;11:265–284. doi: 10.1080/092970490911324. [DOI] [PubMed] [Google Scholar]
- Cate IM, Kennedy C, Stevenson J. Disability and quality of life in spina bifida and hydrocephalus. Developmental Medicine & Child Neurology. 2000;47:27–34. doi: 10.1017/s0012162201002146. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. QuickStats: Spina bifida and anencephaly rates—United States, 1991, 1995, 2000, and 2005. Morbidity and Mortality Weekly Report. 2008;57:15. [Google Scholar]
- Coakley RM, Holmbeck GN, Friedman D, Greenley RN, Thill AW. A longitudinal study of pubertal timing, parent-child conflict, and cohesion in families of young adolescents with spina bifida. Journal of Pediatric Psychology. 2002;27(5):461–473. doi: 10.1093/jpepsy/27.5.461. [DOI] [PubMed] [Google Scholar]
- Dennis M, Edelstein K, Hetherington R, Copeland K, Frederick J, Blaser SE, Kramer LA, Drake JM, Brandt M, Fletcher JM. Neurobiology of perceptual and motor timing in children with spina bifida in relation to cerebellar volume. Brain. 2004;127:1292–1301. doi: 10.1093/brain/awh154. [DOI] [PubMed] [Google Scholar]
- Devine K, Wasserman R, Gershenson L, Holmbeck G, Essner B. Mother-adolescent agreement regarding decision-making autonomy: A longitudinal comparison of families of adolescents with and without spina bifida. Journal of Pediatric Psychology. doi: 10.1093/jpepsy/jsq093. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles JS, Midgley C, Wigfield A, Buchanan CM, Reuman D, Flanagan C, Iver DM. Development during adolescence: The impact of stage-environment fit on adolescents' experiences in schools and families. American Psychologist. 1993;48:90–101. doi: 10.1037//0003-066x.48.2.90. [DOI] [PubMed] [Google Scholar]
- Ellerton M, Stewart MJ, Ritchie JA, Hirth AM. Social support in children with a chronic condition. Canadian Journal of Nursing Research. 1996;28:15–36. [PubMed] [Google Scholar]
- Evans GW, Kim P, Ting AH, Tesher HB, Shannis D. Cumulative Risk, maternal responsiveness, and allostatic load among young adolescents. Developmental Psychology. 2007;43(2):341–351. doi: 10.1037/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]
- Farrington DP, Loeber R. Some benefits of dichotomization in psychiatry and criminological research. Criminal Behaviour and Mental Health. 2000;10:100–122. [Google Scholar]
- Fletcher JM, Brookshire BL, Davidson KC, Francis DJ, Levin HS, Brandt ME, et al. Attentional skills and executive functions in children with early hydrocephalus. Developmental Neuropsychology. 1996;12:53–76. doi: 10.1037//0894-4105.12.4.578. [DOI] [PubMed] [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Ge X, Conger RD, Elder GH. Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Developmental Psychology. 2001;37:404–417. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- Graber JA. Internalizing problems during adolescence. In: Lerner RM, Steinberg L, editors. Handbook of Adolescent Psychology. 2nd ed. Hoboken, NJ: John Wiley & Sons, Inc; 2004. pp. 587–626. [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescenc e to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for Self-Perception Profile for Children: Revision of the Perceived Competence Scale for Children. Denver, CO: University of Denver; 1985. [Google Scholar]
- Hollingshead AA. Four factor index of social status. New Haven, CT: Yale University; 1975. Unpublished manuscript. [Google Scholar]
- Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. A developmental perspective on adolescent health and illness: An introduction to the special issues. Journal of Pediatric Psychology. 2002a;27:409–415. doi: 10.1093/jpepsy/27.5.409. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002b;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN, DeLucia C, Essner B, Kelly L, Zebracki K, Friedman D, Jandasek B. Trajectories of psychosocial adjustment in adolescents with spina bifida: A six-year four-wave longitudinal follow-up. Journal of Consulting and Clinical Psychology. 2010;78:511–525. doi: 10.1037/a0019599. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN, Westhoven VC, Shapera Phillips W, Bowers R, Gruse C, Nikolopoulos T, Davison K. A multimethod, multi-informant, and multidimensional perspective on psychosocial adjustment in preadolescents with SB. Journal of Consulting & Clinical Psychology. 2003;71:782–796. doi: 10.1037/0022-006x.71.4.782. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Zeller PJ, Paulus M, Leon AC, Maser JD, Endicott J, Coryell W, Kunovac JL, Mueller TI, Rice JP, Keller MB. Psychosocial disability during the long-term course of unipolar major depressive disorder. Archives of General Psychiatry. 2000;57:375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- Katrancha ED. Clean intermittent catherization in the school setting. Journal of School Nursing. 2008;24:197–204. doi: 10.1177/1059840508319865. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children's Depression Inventory--Manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Larson RW, Richards MH, Moneta G, Holmbeck G, Duckett E. Changes in adolescents’ daily interactions with their families from ages 10 to 18: Disengagement and transformation. Developmental Psychology. 1996;32:744–754. [Google Scholar]
- Lary JM, Edmonds LD. Prevalence of spina bifida at birth - United States, 1983–1990: A comparison of two surveillance systems. Morbidity and Mortality Weekly Report. 1996;45:15–26. [PubMed] [Google Scholar]
- Lavigne J, Faier-Routman J. Psychological adjustment to pediatric physical disorders: A meta-analytic review. Journal of Pediatric Psychology. 1992;12(2):133–157. doi: 10.1093/jpepsy/17.2.133. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press; 1981. [Google Scholar]
- Mounts NS, Steinberg L. An ecological analysis of peer influence on adolescent grade point average and drug use. Developmental Psychology. 1995;31:915–922. [Google Scholar]
- Morales JR, Guerra NG. Effects of multiple context and cumulative stress on urban children’s adjustment in elementary school. Child Development. 2006;77(4):907–923. doi: 10.1111/j.1467-8624.2006.00910.x. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Leffert N, Graham B, Alwin J, Ding S. Promoting mental health during the transition into adolescence. In: Schulenberg J, Maggs JL, Hurrelmann K, editors. Health Risks and Developmental Transitions During Adolescence. New York: Cambridge University Press; 1997. pp. 471–497. [Google Scholar]
- Rose B, Holmbeck GN. Attention and executive functions in adolescents with spina bifida. Journal of Pediatric Psychology. 2007;32(8):983–994. doi: 10.1093/jpepsy/jsm042. [DOI] [PubMed] [Google Scholar]
- Rutter M. Protective factors in children’s response to stress and disadvantage. In: Kent MW, Rolf JE, editors. Primary prevention of psychopathology. III. Social competence in children. Hanover, NH: University Press of New England; 1979. pp. 49–74. [Google Scholar]
- Sandler A. Living with Spina Bifida: A Guide for Families and Professionals. Chapel Hill, NC: The University of North Carolina Press; 1997. [Google Scholar]
- Schoenmakers MAGC, Gulmans VAM, Gooskens RHJM, Pruijs JEH, Helders PJM. Spinal fusion in children with spina bifida: Influence on ambulation level and functional abilities. European Spine Journal. 2005;14:415–422. doi: 10.1007/s00586-004-0768-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuldermann E, Schuldermann S. Replicability of the factor in children's report of parent behavior. Journal of Psychology. 1970;76:239–249. [Google Scholar]
- Schulenberg J, Wadsworth KN, O’Malley PM, Bachman JG, Johnston LD. Adolescent risk factors for binge drinking during the transition to young adulthood: Variable- and pattern-centered approaches to change. Developmental Psychology. 1996;32:659–674. [Google Scholar]
- Schwartz SJ, Pantin H, Coatsworth JD, Szapocznik J. Addressing the challenges and opportunities for today’s youth: Toward an integrative model and its implications for research and intervention. The Journal of Primary Prevention. 2007;28:117–144. doi: 10.1007/s10935-007-0084-x. [DOI] [PubMed] [Google Scholar]
- Shiu S. Issues in the education of students with chronic illness. International Journal of Disability, Development and Education. 2001;48:269–281. [Google Scholar]
- Simmons RG, Blyth DA. Moving into Adolescence: The Impact of Pubertal Change and School Context. Vol. 10. New York: Aldine De Gruyter; 1987. [Google Scholar]
- Steinberg L, Morris AS. Adolescent development. Annual Review of Psychology. 2001;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- Stouthamer-Loeber M, Loeber R, Wei E, Farrington DP, Wikstrom P-OH. Risk and promotive effects in the explanation of persistent serious delinquency in boys. Journal of Consulting and Clinical Psychology. 2002;70:111–123. doi: 10.1037//0022-006x.70.1.111. [DOI] [PubMed] [Google Scholar]
- Wills KE. Neuropsychological functioning in children with spina bifida and/or hydrocephalus. Journal of Clinical Psychology and Psychiatry. 1993;22:247–265. [Google Scholar]