Abstract
The genes encoding Slits and their Robo receptors are silenced in many types of cancer, including breast, suggesting a role for this signaling pathway in suppressing tumorigenesis. The molecular mechanism underlying these tumor-suppressive effects has not been delineated. Here, we show that loss of Slits, or their Robo1 receptor, in murine mammary gland or human breast carcinoma cells results in coordinate up-regulation of the Sdf1 and Cxcr4 signaling axis, specifically within mammary epithelium. This is accompanied by hyperplastic changes in cells and desmoplastic alterations in the surrounding stroma. A similar inverse correlation between Slit and Cxcr4 expression is identified in human breast tumor tissues. Furthermore, we show in a xenograft model that Slit overexpression down-regulates CXCR4 and dominantly suppresses tumor growth. These studies classify Slits as negative regulators of Sdf1 and Cxcr4 and identify a molecular signature in hyperplastic breast lesions that signifies inappropriate up-regulation of key prometastatic genes.
Introduction
The multistep model for breast carcinogenesis postulates that invasive carcinoma arises by way of intermediate hyperplastic lesions that progress in severity through stages of atypia to in situ and finally invasive carcinoma. It is generally recognized that there are clinically significant differences between various hyperplastic lesions, with some containing cellular and molecular changes that confer higher risk of progression to invasive disease. Pathologists identify clinically relevant differences later in disease progression, but early breast lesions are not well defined and further subclassification of their tumor potential by morphologic criteria is likely to be impossible. Consequently, assessing the potential risks associated with premalignant breast disease will rely on refining our understanding of the molecular signatures that confer increased risk of progression from epithelial hyperplasia to invasive carcinoma.
Up-regulation of CXCR4 is an example of one molecular change in breast cancer cells that is associated with poor prognosis (1, 2). Its role in directing metastasizing breast cancer cells to target sites is well established (3). Little is known, however, about the role of CXCR4 during breast cancer progression, although it is up-regulated early during cellular transformation (1, 4), along with SDF1 (5), which is produced by cancer-associated fibroblasts (CAF) and is in the local environment (6, 7). Recent studies have identified roles for this signaling pathway in primary breast tumors (8, 9), and in this context, one possibility is that signaling through the CXCR4/SDF1 axis drives proliferation, conferring selective advantage to cells as they transform into metastasizing carcinomas. Several mechanisms up-regulate CXCR4 during tumor metastasis (10–13), but there is little information about mechanisms regulating the SDF1/CXCR4 chemokine axis in organs at early stages of transformation.
SLITs (Slit1, Slit2, and Slit3) are a family of secreted proteins that mediate positional interactions between cells and their environment during development by signaling through ROBO receptors (Robo1, Robo2, Robo3, and Robo4; ref. 14). SLIT/ROBO signaling, however, is not restricted to development, and loss of these cues likely plays an important role during tumor progression. Slits and Robos are considered candidate tumor suppressor genes because their promoters are frequently hypermethylated in epithelial cancers (15–18). In ~50% of sampled human breast tumors, Slit2 or Slit3 gene expression is silenced (15, 19).
Cross-talk between SLIT/ROBO and CXCR4/SDF1 signaling has been observed in several systems, with the regulatory effect occurring downstream of the receptors and involving modulation of intracellular signaling intermediates. In leukocytes and human breast cancer cell lines, SLIT impedes SDF1-induced chemotaxis (20, 21). In breast cancer cells, this deterring effect occurs via SLIT-mediated inhibition of SDF1-induced activation of signaling pathways involved in motility (21). Similarly, in the nervous system, a reciprocal regulation of SLIT-mediated axonal repulsion by SDF1 is exerted through modulation of cyclic nucleotide signaling intermediates (22). These studies show an intriguing interrelationship between these signaling axes but do not address the consequences of losing the function of one of these signaling systems, such as occurs in breast during tumor progression when Slit expression is silenced.
Here, we investigate the consequences of losing SLIT/ROBO1 signaling in murine mammary gland, human breast cancer cells, and human tumors. We identify Sdf1 and Cxcr4 as critical targets of SLIT/ROBO1 regulation. Exploiting the ability to transplant knockout mammary epithelium into host mammary fat pads, we determine the compartment, epithelial or stromal, in which SLIT/ROBO1 signaling occurs, and how loss of signaling in one location leads to alterations across the epithelial/stromal boundary. Finally, we explore the tumor-suppressive capabilities of Slits using a xenograft model of human breast cancer.
Materials and Methods
Clinical samples
Frozen or formalin-fixed paraffin-embedded tissue specimens were collected at Johns Hopkins University (Baltimore, MD). All human tissue was collected using protocols approved by the Institutional Review Board. Informed consent was obtained from each individual who provided tissue linked with clinical data.
Animals
The study conformed to guidelines set by University of California at Santa Cruz animal care committee (Chancellor’s Animal Research Committee). Mouse Slit2, Slit3, and Robo1 nulls were generated and genotyped as described (23).
Transplant techniques
Mammary anlage was rescued from E16–20 embryos and transplanted into precleared fat pads of athymic nude mice (24). Tissue fragments from the resulting outgrowths were contralaterally transplanted to generate knockout and wild-type tissue controls (25).
Implantation of Elvax beads
Elvax, an ethylene vinyl copolymer capable of sustained slow release of bioactive molecules, was prepared as described (26), with pellets containing 225 ng SDF1 and 0.45 mg bovine serum albumin (BSA) for control. Pellets were contralaterally implanted into the fat pad of wild-type CD1 mice (n = 3), and tissue was harvested after 6 d.
Cell lines, DNA constructs, and antibodies
MCF7 and MDA-MB-231 cells were maintained in DMEM supplemented with 10% FCS. pGL-CXCR4(−375) contains CXCR4 between −357 and +51 relative to the transcription site followed by the luciferase gene (12). pCRII-SDF1 (for riboprobes) contains 538-nucleotide fragment of the mouse Sdf1 cDNA (27). Mouse image clone 3385804 (American Type Culture Collection). Small interfering RNA (siRNA) directed against Robo1 was from Santa Cruz Biotechnology. pSecTagB-hSlit3-C-myc was from Dr. Roy Bicknell (University of Birmingham, Birmingham, United Kingdom). The following antibodies were used: anti-CK14 (AF64, Covance), anti-SMA (1A4, Sigma), anti-Ki67 (Santa Cruz Biotechnology), anti-CXCR4 (Abcam), anti-SDF1 (Santa Cruz Biotechnology), anti-SLIT3 (Chemicon), anti-SLIT2 (Chemicon), anti-HA (Dr. Doug Kellog, University of California, Santa Cruz, CA), anti-Myc (9E10), anti-ROBO1 (Abcam), and anti-extracellular signal-regulated kinase (Santa Cruz Biotechnology).
Generation of stable cell lines
MDA-MB-231 cells were transfected with pSecTagB-Slit2-HA and pSecTagB-Slit3-Myc and selected in zeocin (Invitrogen). n = 3 lines were generated expressing SLIT2-HA and n = 2 lines expressing SLIT3-Myc.
Tumor generation
Stable cell lines (106 cells) were injected into precleared fat pads of nude mice. Tumor volume was calculated using the formula (length × width)2/2.
Immunohistochemistry
Tissue was fixed in 4% paraformaldehyde. Paraffin-embedded tissue was sectioned at 6 µm and serially mounted. Standard protocols were used and avidin-biotin complex method (Vector Labs) was used for amplification.
Scoring of immunohistochemistry
Immunostaining was scored according to percentage positive cells (P) and staining intensity (I). Score equals P + I. P scores 0 (none), 1 (<1%), 2 (1–10%), 3 (10–30%), 4 (30–60%), and 5 (>60%). I scores 0 (none), 1 (weak), 2 (intermediate), and 3 (strong).
siRNA transfection
MCF7 cells were transiently transfected using Robo1 siRNA (Santa Cruz Biotechnology) and Lipofectamine 2000 (Invitrogen) according to the manufacturers’ instructions. For three-dimensional culture, the “on-top” method was used (28). For luciferase assay, 48 h before harvest, cells were cotransfected with pGL-CXCR4(−375) (F-luciferase) and pRL-TK (R-luciferase). Cells were lysed using passive lysis buffer and assay was carried out in triplicate using the Dual-Luciferase Assay System (Promega) and Wallac Victor Luminometer (Perkin-Elmer Life Sciences) according to the manufacturers’ instructions. F-luciferase activity was normalized to R-luciferase activity (transfection efficiency).
Western blotting
Western blotting was performed using standard procedures (29). Band intensity was scanned using Typhoon 9410 imager and quantified using ImageQuant 5 software.
Quantitative real-time reverse transcription-PCR analysis
Real-time reverse transcription-PCR (RT-PCR) analysis was done as previously described (30). Data were first analyzed using the Sequence Detector Software SDS 2.0 (Applied Biosystems). Results were calculated and normalized relative to glyceraldehyde-3-phosphate dehydrogenase (GAPDH) control. All of the PCR assays were done in triplicate, and mean values are shown in figures.
In situ hybridization
In situ hybridization was carried out as described previously (23, 25).
Primary cell isolation
Primary mammary epithelial cells were prepared from mild collagenase and dispase digestion, as described (23). Cells were plated overnight and then trypsinized and placed onto Matrigel-coated coverslips.
Chemotaxis assay
Chemotaxis was examined as described before (29). Phase-contrast images were acquired at 0 and 60 min. The change in cell area in the directed quadrant was calculated using ImageJ.
Statistical analysis
We used factorial design ANOVA, unpaired t tests, or Mann-Whitney tests to analyze data as appropriate. Significant ANOVA values were subsequently subjected to post-test using the Tukey-Kramer comparison. We report P values for each statistical test; all P values were <0.05.
Results
Loss of Slit or Robo1 in mammary epithelium leads to the formation of hyperplastic, disorganized lesions
Given the expanding role of SLITs in epithelial biology, we hypothesized a tumor-suppressive function for Slits in breast. We previously showed that two Slit family members, Slit2 and Slit3, are expressed in murine mammary gland (23). The homozygous Slit2−/− mutation causes perinatal lethality. Therefore, to investigate the consequence of its loss in mature mammary gland, we generated Slit2−/−;Slit3−/− outgrowths by contralateral transplantation of knockout and wild-type anlage into cleared fat pads of immuno-compromised mice (24).
We examined mature Slit2−/−;Slit3−/− mammary outgrowths for morphology. Compared with the open lumens and organized bilayers of ducts in control outgrowths, Slit2−/−;Slit3−/− ducts displayed striking abnormalities (Fig. 1A). The phenotype was 100% penetrant, with ~ 30% of ducts having lesions extending between 0.3 and 5.0 mm. We categorized the lesions as mild and severe. Mild lesions contained cells in the luminal space (10.1% ± SE 1.9; n = 621 ducts; 5 outgrowths), and many of these cells were peeled away from the myoepithelial layer, similar to an adhesive defect previously described in Ntn1−/−;Slit2−/− glands (23). In severe lesions (17.8% ± SE 8.1; n = 621 ducts; 5 outgrowths), ductal lumens were occluded with a disorganized mass of cells (Fig. 1A). These excess cells suggested disrupted growth control due to either increased proliferation and/or decreased apoptosis. We labeled proliferating cells and observed a significant increase in the percentage of Ki67+ cells in Slit2−/−;Slit3−/−, compared with +/+, ducts (Fig. 1B). This increase is responsible for the excess cells because we evaluated apoptosis using activated caspase-3 staining and observed no difference (data not shown). Histopathologic analyses concurred with our observations that Slit2−/−;Slit3−/− tissue contains hyperplasias. Condensed and desmoplastic stroma surrounding the lesions were also noted in the diagnosis (Fig. 1A), as was a large influx of immune infiltrates in the knockout, compared with wild-type, tissue.
Figure 1.
Loss of Slit2 and Slit3 expression in mammary epithelium leads to the formation of hyperplastic disorganized lesions. A, lack of SLIT in the epithelium leads to lesion formation. Immunostaining with anti-CK14 on longitudinal sections and cross-sections through +/+ and Slit2−/−;Slit3−/− mammary outgrowths. Arrows, ductal myoepithelial cell layer; arrowheads, CK14-positive cells abnormally located in the lumen. Red bar, condensed desmoplastic stroma. L, lumen. B, lack of SLIT leads to hyperplasia. Representative lesion with dashed line indicating epithelial/stromal interface. Arrowheads, Ki67+ cells. Columns, mean percentage [n = 3 animals at 12 wk of age, 15 fields of view/animal (5×)]; bars, SD. ***, P < 0.0001, unpaired t test. C, lack of ROBO1 leads to a disorganized phenotype in three-dimensional culture. After transfection, MCF7 cells were grown in Matrigel. After 5 d, colonies were photographed (5×) and percentage of disorganized structures was counted. Representative images of colonies are shown. Scale bar, 10 µm. Columns, mean percentage; bars, SD. ***, P < 0.0001, ANOVA. RNAi, RNA interference. D, lack of ROBO1 increases the cell proliferation index. Columns, mean percentage of Ki67+ cells; bars, SD. **, P < 0.001, ANOVA.
ROBO1 is a SLIT receptor that could mediate the observed effects in the gland (23). Robo1−/− animals are viable so we evaluated the loss-of-function phenotype using intact glands. Ducts in Robo1−/− glands were hyperplastic and disorganized, displaying a phenotype that was indistinguishable from Slit2−/−;Slit3−/− ductal lesions (Supplementary Fig. S1). As was the case for Slit2−/−;Slit3−/− tissue, the penetrance of the phenotype was 100%, with ~30% of ducts displaying lesions that extended between 0.3 and 5.0 mm.
To investigate whether a similar phenotype occurred when SLIT/ROBO1 signaling was disrupted in human breast cells, we used the MCF7 line that retains several characteristics of differentiated mammary epithelium, including expression of Slit2, Slit3, and Robo1 (data not shown; ref. 31). Cells were treated with Robo1 siRNA to down-regulate SLIT/ROBO1 signaling (Supplementary Fig. S2) and then cultured in Matrigel. MCF7 cells formed smooth, nonpolarized colonies without central lumens. In contrast, the siRNA-treated colonies were large and disorganized, a phenotype that was rescued by reexpression of Robo1 (Fig. 1C). Immunostaining with Ki67 revealed a significantly higher fraction of proliferating cells in colonies treated with Robo1 siRNA compared with control (Fig. 1D). This was similar to the elevated proliferation observed in Slit2−/−; Slit3−/− outgrowths and Robo1−/− glands (Fig. 1B; Supplementary Fig. S2). Together, these data show that a consequence of Slit/Robo1 loss is elevated proliferation leading to hyperplastic lesions.
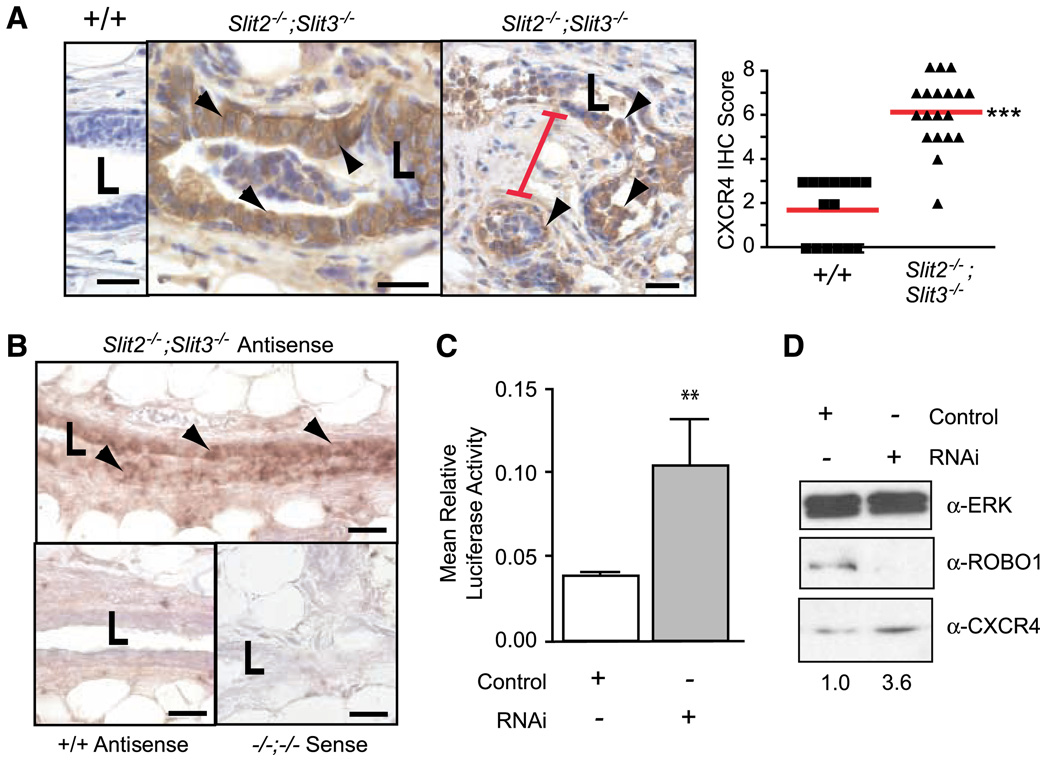
Loss of Slit up-regulates Cxcr4 expression
We sought candidates whose misexpression in the absence of SLIT/ROBO1 signaling is responsible for the observed hyperplastic phenotype. One candidate is CXCR4 because it is expressed early during breast tumorigenesis (1, 4), and blocking its expression or function inhibits breast tumor growth (8, 9). Western blots of whole gland lysates showed elevated CXCR4 expression in Slit2−/−;Slit3−/−, compared with +/+, tissue (Supplementary Fig. S3). Immunohistochemistry revealed CXCR4 expression in a large fraction of cells in Slit2−/−;Slit3−/− epithelium, with little or no expression in +/+ epithelium (Fig. 2A). We also observed condensed and desmoplastic stroma surrounding these CXCR4-positive lesions (Fig. 2A). Because CXCR4 is regulated by transcriptional and posttranscriptional mechanisms, we performed in situ hybridization studies and observed Cxcr4 in Slit knockout, but not wild-type, epithelium (Fig. 2B). A transcriptional mechanism also occurred in Robo1 siRNA-treated MCF7 cells because we observed increased Cxcr4 reporter gene activity and increased levels of CXCR4 in treated, compared with control, cells (Fig. 2C and D). Together, our results show that SLIT/ROBO1 signaling negatively regulates Cxcr4 expression, with loss of this regulation leading to elevated levels of CXCR4 in murine tissue and human breast cancer cells.
Figure 2.
Loss of Slit2 and Slit3 causes up-regulation of CXCR4 in mouse mammary gland and human MCF7 cells. A, in Slit2−/−;Slit3−/− outgrowths, CXCR4 protein expression is localized to epithelia, with desmoplastic stroma between lesions. Representative immunostaining with anti-CXCR4 on +/+ and Slit2−/−;Slit3−/− mammary outgrowths. Arrowheads, positive epithelial cells. Red bar, condensed desmoplastic stroma. Scale bar, 20 µm. CXCR4 immunostaining was scored according to positivity and staining intensity and plotted on a vertical scatter plot. Red bars, average score. Significantly more CXCR4 staining is seen in Slit2−/−;Slit3−/− outgrowths. ***, P < 0.0001, Mann-Whitney. B, Cxcr4 mRNA is specifically present in the epithelium of Slit2−/−;Slit3−/− outgrowths. In situ hybridization on +/+ and Slit2−/−;Slit3−/− outgrowths using antisense probes reveals Cxcr4 mRNA in Slit2−/−;Slit3−/−, but not +/+, cells. Arrowheads, positive epithelial cells. Sense probes show little or no background staining. Scale bar, 20 µm. L, lumen. C, loss of SLIT/ROBO signaling in MCF7 cells leads to up-regulation of Cxcr4 gene expression. Cells were treated with control or Robo1 siRNA and then cotransfected with pGL-CXCR4(−375), which contains the Cxcr4 promoter region coupled to the F-luciferase gene and pRL-TK (R-luciferase). Cells were lysed after 36 h and luciferase activity was measured in triplicate. Activities were normalized for transfection efficiency. Columns, mean relative luciferase activity; bars, SE. **, P = 0.0095, Mann-Whitney test. D, loss of SLIT/ROBO signaling in MCF7 cells leads to increased levels of CXCR4 protein. Representative immunoblots (n = 4). Numbers, CXCR4 band intensity.
If Slits silence Cxcr4 in normal breast, we hypothesize that loss of Slits in tumors will correspond with elevated Cxcr4. To investigate, we analyzed microarray data sets from human breast tumor samples available at Oncomine.org (32) and found an inverse correlation between Slit and Cxcr4 expression (Fig. 3A). We confirmed this by performing quantitative RT-PCR on a panel of human tumors; in 68% of tumors with elevated Cxcr4 expression, Slit2 or Slit3 levels were significantly reduced compared with their expression in normal tissue (Fig. 3B). We further verified these observations at the protein level using immunohistochemistry on samples of normal breast, ductal carcinoma in situ (DCIS), and infiltrating ductal carcinoma (IDC; Fig. 3C and D). Again, there were robust levels of SLIT2 and SLIT3 in normal tissue that significantly decreased with increasing tumor grade. In contrast, and as previously shown (1, 4), little or no CXCR4 was detectable in normal breast, but its expression significantly increased with higher tumor grade.
Figure 3.
Loss of Slit expression in human tumors correlates with up-regulation of Cxcr4. A, box plots of data from the Richardson microarray data set were drawn using the Oncomine Cancer Profiling Database (32). Slit2 (P = 2.6E–10) and Slit3 (P = 7.1E–9) expression is significantly reduced in tumors, whereas Cxcr4 (P = 1.8E–5) expression is elevated. Normal, n = 7; tumor, n = 40; P values from t test. B, expression levels, by quantitative PCR, of Slit2, Slit3, and Cxcr4 were obtained from a panel of tumors, with values normalized against internal control GAPDH. The data were then normalized to values obtained from normal breast (n = 6). A value of 1 equals expression level of the gene in average normal breast. Seventeen of 25 tumor samples (68%) showed elevated Cxcr4 expression compared with normal breast. In these tumors, this elevation corresponded with significantly reduced expression of Slit2 or Slit3. Columns, mean relative expression; bars, SE. Slit2 versus Cxcr4: **, P < 0.011; Slit3 versus Cxcr4: ***, P < 0.001, ANOVA. C, SLIT expression is decreased in tumors, whereas CXCR4 levels increase. Normal breast, DCIS, and IDC tissue sections were immunostained with anti-SLIT2, anti-SLIT3, and anti-CXCR4. Representative images are shown. Scale bar, 100 µm. D, immunostained sections were scored according to cell percentage positivity and staining intensity. Scores were plotted on a vertical scatter plot. Black bars, average score. Both SLIT2 (*, P = 0.01, ANOVA) and SLIT3 (***, P < 0.0001, ANOVA) exhibit decreased expression in DCIS and IDC compared with normal breast. In contrast, CXCR4 is expressed at very low levels in normal breast, but its expression increases in DCIS and IDC (**, P = 0.0005, ANOVA).
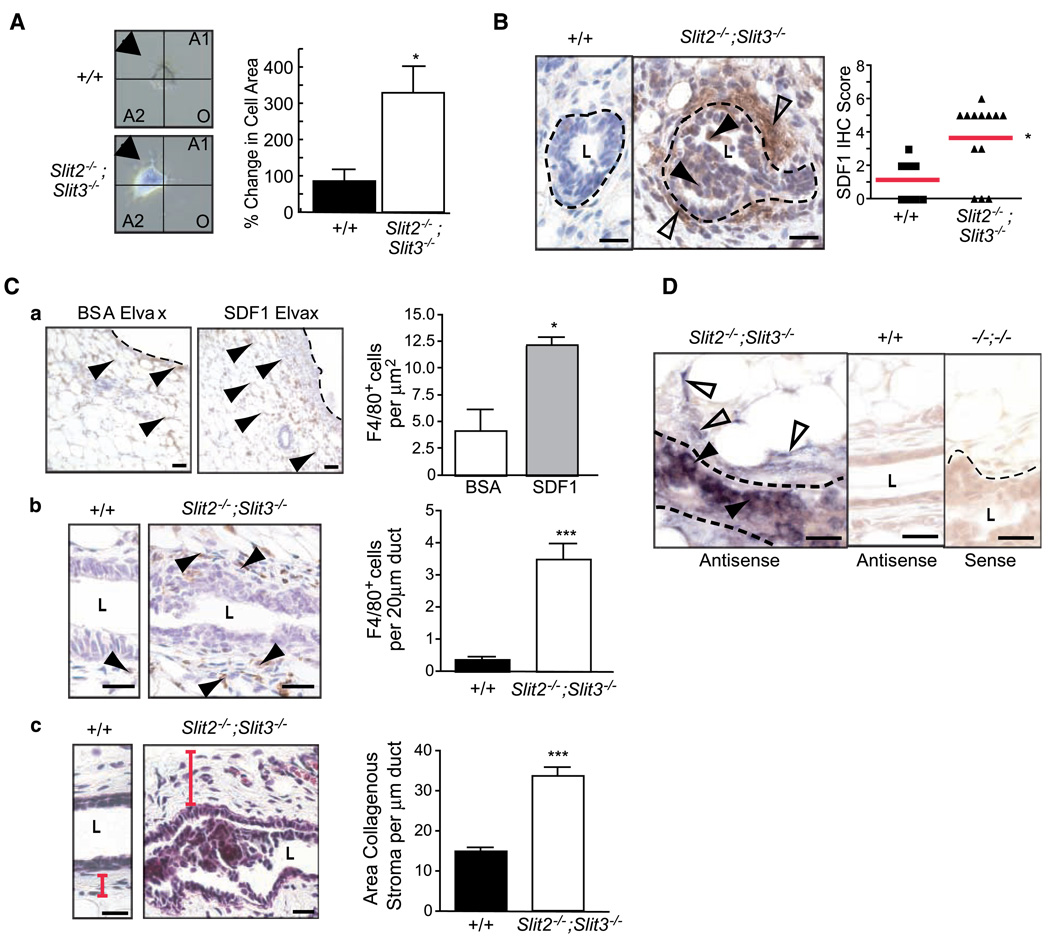
Loss of Slit expression results in coordinate up-regulation of SDF1
Although CXCR4 is up-regulated in the vast majority of sampled premalignant lesions, studies on human breast cancer cell lines have suggested that it is only active in metastatic cells (33). To evaluate CXCR4 activity in Slit2−/−;Slit3−/− cells, we performed chemotaxis assays. Slit2−/−;Slit3−/− cells did not exhibit robust migration as expected of primary cells harvested from premalignant tissue but instead responded to SDF1 by reorganizing their cell membrane and sending membranous projections toward a point source (Fig. 4A). Wild-type cells were unresponsive to SDF1. This result suggested that CXCR4 expressed on Slit2−/−;Slit3−/− cells is active and reacts to its ligand.
Figure 4.
Loss of Slit expression results in coordinate up-regulation of SDF1 and the formation of desmoplastic stroma. A, Slit2−/−;Slit3−/−, but not +/+, cells respond to a point source of SDF1. Primary epithelial cells were prepared from outgrowths and placed in stable liquid gradients of SDF1 (29). Phase-contrast images were acquired at 0 and 60 min. Using ImageJ, the change in cell area in the source quadrant (arrow) was calculated. Columns, mean percentage change (n = 7); bars, SE. *, P = 0.0018, Mann-Whitney. B, SDF1 protein is present in the stroma surrounding Slit2−/−;Slit3−/− outgrowths. Representative immunostaining with anti-SDF1 on +/+ and Slit2−/−;Slit3−/− mammary outgrowths. Dotted lines, epithelial/stromal interface. Open arrowheads, positive staining in stroma; arrowheads, epithelial cells expressing SDF1. Scale bar, 20 µm. SDF1 immunostaining was scored according to positivity and intensity. Scores were plotted on a vertical scatter plot. Red bars, average score. Significantly more SDF1 staining is seen in Slit2−/−;Slit3−/− outgrowths. *, P = 0.018, Mann-Whitney. C, SDF1 attracts macrophages. a, representative images of F4/80 staining in fat pads containing BSA versus SDF1 Elvax pellets. The number of F4/80+ cells surrounding pellets was counted and expressed as the number of F4/80+ cells per µm2. Columns, average; bars, SD. *, P = 0.0086, unpaired t test. Macrophages surround Slit2−/−;Slit3−/− ducts. b, representative images of F4/80 staining in +/+ versus Slit2−/−;Slit3−/− tissue. Duct length was measured and the number of F4/80+ cells was counted (ImageJ software). Columns, average; bars, SD. ***, P < 0.0001, unpaired t test (n = 3 animals, 10 fields of view/animal). Stroma surrounding Slit2−/−;Slit3−/− ducts is desmoplastic. c, representative images of Masson’s trichrome staining of +/+ versus Slit2−/−;Slit3−/− tissue. Red bar, width of stroma. Longitudinal images of ducts were taken and duct length and positively stained areas were measured (ImageJ software). Columns, average; bars, SD. ***, P < 0.0001, unpaired t test. Scale bar, 20 µm. D, Sdf1 mRNA is specifically present in subpopulations of elongated stromal cells (open arrowheads) and epithelial cells (closed arrowheads) in Slit2−/−;Slit3−/− outgrowths. In situ hybridization on +/+ and Slit2−/−;Slit3−/− outgrowths using antisense probes reveals Sdf1 mRNA in Slit2−/−;Slit3−/−, but not +/+, cells. Sense probes show no or little background staining. Scale bar, 20 µm.
This raised the question of whether SDF1 surrounded Slit2−/−;Slit3−/− lesions because recent studies have placed it in the tumor microenvironment (6, 7). We found abundant SDF1 expression in the epithelium and the surrounding stroma of knockout, but not wild-type, tissue (Fig. 4B). The presence of SDF1 is consistent with the histopathologic diagnosis that noted the infiltration of immune cells within desmoplastic stroma surrounding Slit2−/−;Slit3−/− lesions. Macrophages, which express CXCR4, represent a major component of immune infiltrates surrounding tumors and play a key role in promoting the angiogenic switch during malignant transition (34). To determine whether macrophages are attracted to SDF1, we implanted point sources of SDF1 or vehicle (BSA) into wild-type mammary glands (Fig. 4C, a). Significantly more macrophages (F4/80+) infiltrated into the tissue surrounding SDF1, compared with control, showing that SDF1 is a chemoattractant for macrophages and suggesting a role in recruiting these immune cells to tumors (Fig. 4C, a). Next, we performed F4/80 immunohistochemistry on Slit2−/−;Slit3−/− and control tissue and found a significant increase in macrophages surrounding knockout tissue (Fig. 4C, b). We also evaluated the stromal expression of collagen, a major constituent of desmoplastic stroma (Fig. 4C, c). Stroma surrounding Slit2−/−;Slit3−/− epithelium contained significantly more condensed, collagenous stroma, compared with +/+, consistent with the histopathologic analysis. To define the cellular source of SDF1, we performed in situ hybridization analyses and discovered Sdf1 in a fraction of epithelial cells and in a subset of elongated stromal cells that are likely to be fibroblasts based on their morphology (Fig. 4D). Thus, both CXCR4 and SDF1 are initially up-regulated in the epithelium, as has been recently observed in a xenograft model of DCIS (5). A local source of SDF1 may function to transform myoepithelial cells into CAFs or to recruit CAFs from circulating cells (35).
Epithelial regulation of CXCR4/SDF1 chemokine signaling axis
Together, the data show that loss of Slit expression leads to the coordinate up-regulation of Cxcr4 in epithelia and Sdf1 in both epithelia and stroma. This suggests that SLIT/ROBO1 signaling keeps SDF1/CXCR4 expression in check, but the regulatory networks may be complicated. Slit genes are expressed in the epithelia, but they encode a secreted cue that may act on any cell type expressing ROBO1 receptors. During mammary development, ROBO1 is expressed on myoepithelial cells (23), but as the gland matures, we observed a switch in its expression to include a subpopulation of luminal cells (Fig. 5A). ROBO1 was also expressed on stromal fibroblasts (Fig. 5A). Consequently, loss of Slit expression could regulate Sdf1 and Cxcr4 independently by disrupting ROBO1 signaling in both the stromal and epithelial compartments. Alternatively, loss of SLIT/ROBO1 signaling in just one compartment could up-regulate Sdf1 and Cxcr4 in both compartments.
Figure 5.
Coordinate up-regulation of CXCR4 and SDF1 is due to lack of SLIT/ROBO1 signaling within mammary epithelia. A, to examine Robo1 gene expression, we took advantage of the lacZ gene under the control of the endogenous Robo1 promoter in −/− tissue. a, longitudinal sections of Robo1−/− ducts stained for β-galactosidase activity. b, longitudinal section of +/+ duct immunostained with anti-ROBO1. Open arrows, positive stromal staining; arrowheads, positive epithelial cells. Scale bar, 20 µm. L, lumen. B, transplanted Robo1−/− mammary outgrowths show severe ductal defects similar to those observed in Slit2−/−;Slit3−/− outgrowths. Scale bar, 20 µm. C, CXCR4 protein is specifically expressed in the epithelium of Robo1−/− outgrowths. Representative immunostaining with anti-CXCR4 on +/+ stroma/+/+ epithelia and +/+ stroma/Robo1−/− epithelia. Arrows, positive cells. Scale bar, 20 µm. CXCR4 immunostaining was scored and plotted on a vertical scatter plot. Red bars, average score. Significantly more CXCR4 staining is seen in Robo1−/− outgrowths. ***, P < 0.0001, Mann-Whitney test. D, SDF1 is present in the stroma surrounding Robo1−/− epithelial outgrowths (a; open arrowheads) and in a subpopulation of epithelial cells (arrowheads). Representative immunostaining with anti-SDF1 on +/+ stroma/+/+ epithelia and +/+ stroma/Robo1−/− epithelia. SDF1 immunostaining was scored and plotted on a vertical scatter plot. Red bars, average score. Significantly more SDF1 staining is seen in Robo1−/− outgrowths. ***, P < 0.0001, Mann-Whitney test. Sdf1 mRNA is present in subpopulations of stromal fibroblasts (b; open arrowheads) and epithelial cells (arrowheads) in Robo1−/− outgrowths. In situ hybridization on +/+ stroma/+/+ epithelia and +/+ stroma/Robo1−/− epithelia outgrowths using antisense probes reveals Sdf1 mRNA in +/+ stroma/Robo1−/− epithelia but not +/+ stroma/+/+ epithelia cells. Sense probes show little or no background staining. Scale bar, 20 µm.
To investigate, we eliminated SLIT/ROBO1 signaling selectively in the epithelial compartment by transplanting Robo1−/− epithelium into wild-type stroma. In these chimeric glands, we observed disorganized, hyperplastic epithelial lesions (Fig. 5B), which were similar in phenotype, penetrance (100%), and expressivity (19.64% ± SE 9.77; n = 669 ducts; 6 outgrowths) to those seen in Slit2−/−;Slit3−/− transplants (Fig. 1A). We evaluated the chemokine axis and again found up-regulation of CXCR4 in Robo1−/− epithelium (Fig. 5C), and coordinate up-regulation of SDF1 in the surrounding +/+ stroma (Fig. 5D, a), which was desmoplastic and contained immune infiltrates similar to stroma surrounding Slit2−/−Slit3−/− tissue (data not shown). These data show that loss of SLIT/ROBO1 signaling in the epithelial compartment, alone, up-regulates SDF1 and CXCR4. This leads to phenotypic changes similar to those occurring in Slit2−/−;Slit3−/− transplants in which SLIT/ROBO1 signaling is disrupted in both compartments. To define the source of SDF1 in the transplanted tissue, we performed in situ hybridization studies and found Sdf1 mRNA in cell subpopulations in the epithelia and stroma (Fig. 5D, b), suggesting that loss of SLIT/ROBO1 signaling in breast epithelia at early stages of transformation both generates a local source of Sdf1 and up-regulates Cxcr4. We therefore conclude that loss of SLIT/ROBO1 signaling in the epithelia, alone, is sufficient to drive the observed morphologic and molecular changes, resulting in hyperplastic lesions, surrounded by desmoplastic stroma.
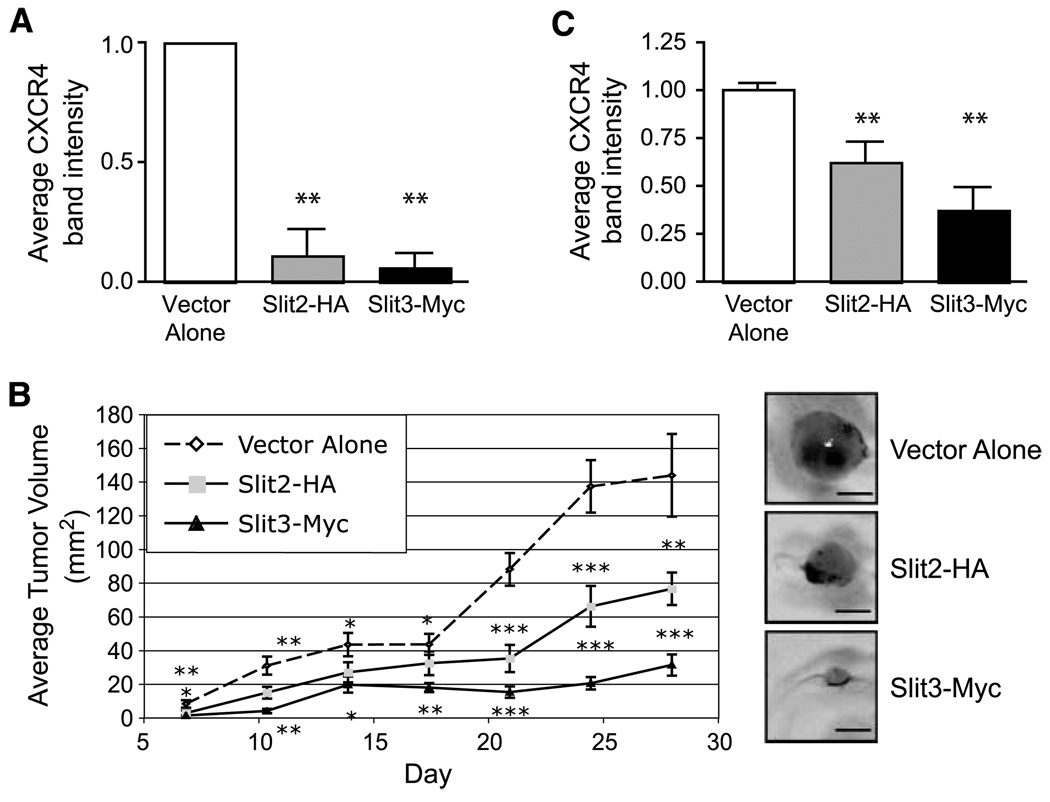
SLITs suppress CXCR4 expression and inhibit tumor growth
Given that SLITs exert this regulatory function by inhibiting the expression of Sdf1 and Cxcr4 within the mammary epithelium, we wondered whether overexpression of Slits in human breast carcinoma cells would suppress Cxcr4 expression and inhibit tumor growth. Previous studies have shown that the metastatic human cell line MDA-MB-231 expresses CXCR4, but not SDF1 (36), and that inhibiting CXCR4 expression or function in these cells blocks primary tumor growth (8, 9). Because MDA-MB-231 cells express ROBO1 and ROBO2 (21),4 signaling through these receptors could down-regulate CXCR4 expression and suppress tumor formation. To investigate, we transiently expressed Myc-Slit2 or Myc-Slit3 in MDA-MB-231 cells and documented decreased CXCR4 expression (Supplementary Fig. S4). Next, we generated stable cell lines expressing Slit2 (n = 3) or Slit3 (n = 2) and again found reduced CXCR4 levels (Fig. 6A). We also observed that Slit-expressing cells formed significantly fewer colonies, compared with control, when cultured in Matrigel (Supplementary Fig. S5). This suggested a general inhibition of cell growth, so we pursued the observation by establishing orthotopic xenograft tumors in immunocompromised hosts. We found that Slit-expressing cells formed significantly smaller tumors over time, with Slit3 producing the most dramatic effect (Fig. 6B). We confirmed sustained down-regulation of CXCR4 in Slit-expressing tumors after 28 days of in vivo incubation (Fig. 6C; Supplementary Fig. S6). Thus, expression of Slits in MDA-MB-231 cells both down-regulates CXCR4 and inhibits tumor growth. Together with the observation that targeting CXCR4 reduces tumor growth in numerous organs (37, 38), our results suggest that SLITs suppress tumor growth by inhibiting the proliferative consequences of elevated CXCR4 expression.
Figure 6.
Slit expression in MDA-MB-231 cells blocks tumor growth by reducing CXCR4 expression. A, Slit2-HA and Slit3-Myc stable cell lines express low levels of CXCR4 compared with vector alone control lines. Stable Slit2-HA (n = 3) and Slit3-myc (n = 2) cell lines were generated by clonal selection. Stable cell line extracts were probed with anti-CXCR4. Columns, mean CXCR4 band intensity (n = 2 for each line); bars, SE. **, P < 0.001, ANOVA. B, expression of Slit2 or Slit3 resulted in smaller tumor size. Tumors were generated using Slit and control stable cell lines. n = 12 mice for each line. Points, mean tumor volume at each day; bars, SE. ***, P < 0.0001; **, P < 0.001; *, P < 0.05, ANOVA. Representative images of orthotopic tumors are shown. Scale bar, 0.25 mm. C, tumors expressing Slit2 or Slit3 contain significantly less CXCR4 protein compared with control tumors. Columns, mean CXCR4 immunoblot band intensity from n = 3 tumors; bars, SE. **, P = 0.01, ANOVA.
Discussion
There is extensive literature on the molecular and genetic alterations that occur in invasive breast carcinoma and signify poor prognosis, but relatively little progress has been made in defining the genetic changes occurring in premalignant lesions. Here, we report that loss of Slit expression early during tumor progression up-regulates a key chemokine signaling axis and generates hyperplastic changes in the epithelium, along with desmoplastic changes in the stroma. Expression of CXCR4 was originally thought to occur late during tumor progression, generating cells that are ready to metastasize and home to organs expressing high levels of SDF1 (3). This restricted view of CXCR4 function, however, has been called into question because 93% of studied cases of atypical ductal carcinoma display high levels of CXCR4 (4), suggesting a role for CXCR4 in mediating earlier aspects of cellular transformation. Our data show that changes, loss and gain, in Slit expression function as a switch in the epithelium that up-regulate and down-regulate Cxcr4, leading to attendant changes in proliferation. We also show that loss of Slits results in the coordinate up-regulation of Sdf1 in both the epithelium and surrounding stroma and this is accompanied by changes in the local microenvironment consistent with transformation.
The importance of the tumor microenvironment is well established, but it is unclear how it is generated. Our studies show that loss of SLIT/ROBO1 signaling exclusively in the epithelia is sufficient to increase expression of both Cxcr4 and Sdf1 (Fig. 5). The establishment of an initial SDF1/CXCR4 signaling loop within the epithelium is supported by recent studies using human MCF10DCIS.com cells in a xenograft model (5). BothCXCR4 and SDF1 are expressed at low levels in early MCF10DCIS lesions. CXCR4 expression remains epithelial, but during intermediate stages of transformation, SDF1 is switched on in the activated stroma. Once the ductal carcinoma becomes invasive, SDF1 expression is extinguished in the epithelia and is exclusively expressed by CAFs in the activated stroma. The origin of these CAFs is currently unknown. Some may be transformed from normal fibroblasts by aberrant signals from cancerous epithelial cells, whereas others may be transformed after being recruited from circulating bone marrow–derived cells (35). In either case, the transformation of these cells seems to be a consequence of their interaction with the cancerous epithelium. Our data raise the possibility that up-regulation of epithelial SDF1, accompanying Slit loss, contributes to the recruitment and/or transformation of CAFs, and support the model that genetic changes in the tumor epithelium, alone, are sufficient to drive transformation of cells and the surrounding microenvironment (7).
Our data also provide in vivo evidence that the SDF1/CXCR4 axis is fully functional within the epithelium during preinvasive stages of breast transformation and that it promotes cell survival and proliferation. We show that loss of SLIT/ROBO1 signaling results in the development of hyperplastic lesions (Fig. 1) with the coordinate up-regulation of both CXCR4 and SDF1 in the mammary epithelium (Figs. 2, 4, and 5). This type of autocrine stimulation of cell growth by SDF1/CXCR4 has been documented in human breast cancer cells on overexpression of SDF1 (39) and was also observed in the MCF10DCIS.com cells, described above, in which intraepithelial SDF1/CXCR4 signaling gives way to signaling across the epithelial/stromal boundary as the tumor microenvironment becomes established (5). Numerous pathways have been implicated in the mitogenic activity of SDF1/CXCR4 and may be responsible for the hyperplastic lesions observed in Slit2−/−;Slit3−/− tissue (40). We are currently investigating the pathways that drive proliferation because targeting these pathways could provide therapies that arrest cellular proliferation in early stages of transformation.
The molecular mechanism through which cells acquire SDF1 and CXCR4 expression during the evolution of tumors is unclear. At later stages of cellular transformation, CXCR4 expression is up-regulated by several mechanisms (40). Our studies reveal a transcriptional mechanism during early stages of transformation that occurs within breast epithelia (Figs. 2, 4, and 5). We show that SLITs signal through their ROBO1 receptor to negatively regulate Cxcr4 and Sdf1. Negative transcriptional regulation of both Cxcr4 and Sdf1 has been shown in renal cells where hypoxia-inducible factors 1 and 2 (Hif1 and Hif2) are targeted for degradation by von Hippel-Lindau (VHL) proteins (11). It has been shown that loss of VHL leads to stabilization of Hifs and subsequent up-regulation of both Sdf1 and Cxcr4 due to the Hif response elements contained in their promoters (41). Hifs are frequently up-regulated during breast transformation (42) and can drive the inappropriate proliferation of cells even under conditions of normal oxygen (43). Thus, Hifs or VHL proteins may be targeted by SLIT/ROBO1 signaling, and we are currently investigating their expression profiles in Slit2−/−;Slit3−/− and Robo1−/− glands.
Numerous studies show epigenetic inactivation of Slits in multiple types of cancer (15, 16, 18, 19), and in breast, this loss of Slit also correlates with increasing tumor grade (44). Our histopathologic analyses of Slit2−/−;Slit3−/− and Robo1−/− mammary epithelium revealed hyperplastic lesions with no nuclear atypia (Fig. 1), a type of lesion that can be found in ~ 30% of women with benign proliferative breast disease (45). Epidemiologic studies show that identification of such lesions confers a 2-fold increase in relative risk of developing invasive breast cancer compared with women without proliferative disease. For patients diagnosed with lesions having the next stage of severity, hyperplasias with nuclear atypia, the relative risk of future invasive disease rises to ~ 5-fold and increases to 10-fold if there is also positive family history (45, 46). These numbers show that, although most patients will not develop invasive disease, a fraction will. With medical advances enabling detection of breast lesions at earlier stages, it will be crucial to develop methods that distinguish between nascent disease and normal biology because current methods relying on morphologic criteria are insufficient. Improved understanding of molecular signatures within breast lesions holds the promise of identifying those at high risk so they receive appropriate treatment while also identifying the majority who are not at risk so their medical concerns are dispelled (47). The findings presented in this report identify the loss of Slit expression as a marker of early lesions that have the potential to progress to invasive disease due to up-regulation of metastasis markers SDF1/CXCR4. We propose that these molecular alterations define a specific subclass of breast lesions whose early detection could lead to treatment strategies that prevent development of invasive disease.
Supplementary Material
Acknowledgments
Grant support: American Cancer Society grant RSG0218001MGO, California Breast Cancer Research Program grant 10PB-0188, and National Cancer Institute grant R01CA128902 (L. Hinck) and Congressionally Directed Medical Research Program grant BC043200 and National Cancer Institute grant U01 CA105490 (R.D. Cardiff).
Santa Cruz Biotechnology generously provided antibodies and siRNA reagents. Other generous gifts were the following: anti-Dutt1 (Dr. Rabbitts, University College, London, United Kingdom), anti-HA (Dr. Doug Kellogg), MCF7 and MDA-MB-231 cell lines (Dr. Bissell, Lawrence Labs, Berkeley, CA), pGL-CXCR4(−375) (Dr. Avraham, Harvard Medical School, Boston, MA), pCRII-SDF1 (Dr. Goffinet, University of Louvain Medical School, Brussels, Belgium), pRL-TK (Dr. Haussler, University of California, Santa Cruz, CA), pSecTagB-hSlit3-C-myc (Dr. Roy Bicknell), Slit3−/− mice (Dr. Ornitz, Washington University, St. Louis, MO), and Slit2−/− mice and Robo1−/− (Dr. Tessier-Lavigne, Genentech, Inc., South San Francisco, CA).
Footnotes
Note: Supplementary data for this article are available at Cancer Research Online (http://cancerres.aacrjournals.org/).
R. Marlow, unpublished data.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Salvucci O, Bouchard A, Baccarelli A, et al. The role of CXCR4 receptor expression in breast cancer: a large tissue microarray study. Breast Cancer Res Treat. 2006;97:275–283. doi: 10.1007/s10549-005-9121-8. [DOI] [PubMed] [Google Scholar]
- 2.Holm NT, Byrnes K, Li BD, et al. Elevated levels of chemokine receptor CXCR4 in HER-2 negative breast cancer specimens predict recurrence. J Surg Res. 2007;141:53–59. doi: 10.1016/j.jss.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 3.Muller A, Homey B, Soto H, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- 4.Schmid BC, Rudas M, Rezniczek GA, Leodolter S, Zeillinger R. CXCR4 is expressed in ductal carcinoma in situ of the breast and in atypical ductal hyperplasia. Breast Cancer Res Treat. 2004;84:247–250. doi: 10.1023/B:BREA.0000019962.18922.87. [DOI] [PubMed] [Google Scholar]
- 5.Tait LR, Pauley RJ, Santner SJ, et al. Dynamic stromal-epithelial interactions during progression of MCF10DCIS.com xenografts. Int J Cancer. 2007;120:2127–2134. doi: 10.1002/ijc.22572. [DOI] [PubMed] [Google Scholar]
- 6.Orimo A, Gupta PB, Sgroi DC, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121:335–348. doi: 10.1016/j.cell.2005.02.034. [DOI] [PubMed] [Google Scholar]
- 7.Allinen M, Beroukhim R, Cai L, et al. Molecular characterization of the tumor microenvironment in breast cancer. Cancer Cell. 2004;6:17–32. doi: 10.1016/j.ccr.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Lapteva N, Yang AG, Sanders DE, Strube RW, Chen SY. CXCR4 knockdown by small interfering RNA abrogates breast tumor growth in vivo. Cancer Gene Ther. 2005;12:84–89. doi: 10.1038/sj.cgt.7700770. [DOI] [PubMed] [Google Scholar]
- 9.Smith MC, Luker KE, Garbow JR, et al. CXCR4 regulates growth of both primary and metastatic breast cancer. Cancer Res. 2004;64:8604–8612. doi: 10.1158/0008-5472.CAN-04-1844. [DOI] [PubMed] [Google Scholar]
- 10.Helbig G, Christopherson KW, Bhat-Nakshatri P, et al. NF-κB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4. J Biol Chem. 2003;278:21631–21638. doi: 10.1074/jbc.M300609200. [DOI] [PubMed] [Google Scholar]
- 11.Staller P, Sulitkova J, Lisztwan J, Moch H, Oakeley EJ, Krek W. Chemokine receptor CXCR4 downregulated by von Hippel-Lindau tumour suppressor pVHL. Nature. 2003;425:307–311. doi: 10.1038/nature01874. [DOI] [PubMed] [Google Scholar]
- 12.Lee BC, Lee TH, Zagozdzon R, Avraham S, Usheva A, Avraham HK. Carboxyl-terminal Src kinase homologous kinase negatively regulates the chemokine receptor CXCR4 through YY1 and impairs CXCR4/CXCL12 (SDF-1α)-mediated breast cancer cell migration. Cancer Res. 2005;65:2840–2845. doi: 10.1158/0008-5472.CAN-04-3309. [DOI] [PubMed] [Google Scholar]
- 13.Li YM, Pan Y, Wei Y, et al. Upregulation of CXCR4 is essential for HER2-mediated tumor metastasis. Cancer Cell. 2004;6:459–469. doi: 10.1016/j.ccr.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 14.Hinck L. The versatile roles of “axon guidance” cues in tissue morphogenesis. Dev Cell. 2004;7:783–793. doi: 10.1016/j.devcel.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Dallol A, Dickinson RE, Latif F. Epigenetic disruption of the SLIT-ROBO interactions in human cancer. In: Ablin RJ, Jiang WG, Esteller M, editors. DNA methylation, epigenetic and metastasis. New York: Springer Netherlands; 2005. pp. 191–214. [Google Scholar]
- 16.Narayan G, Goparaju C, Arias-Pulido H, et al. Promoter hypermethylation-mediated inactivation of multiple Slit-Robo pathway genes in cervical cancer progression. Mol Cancer. 2006;5:16. doi: 10.1186/1476-4598-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmid BC, Rezniczek GA, Fabjani G, Yoneda T, Leodolter S, Zeillinger R. The neuronal guidance cue Slit2 induces targeted migration and may play a role in brain metastasis of breast cancer cells. Breast Cancer Res Treat. 2007;106:333–342. doi: 10.1007/s10549-007-9504-0. [DOI] [PubMed] [Google Scholar]
- 18.Latil A, Chene L, Cochant-Priollet B, et al. Quantification of expression of netrins, slits and their receptors in human prostate tumors. Int J Cancer. 2003;103:306–315. doi: 10.1002/ijc.10821. [DOI] [PubMed] [Google Scholar]
- 19.Sharma G, Mirza S, Prasad CP, Srivastava A, Gupta SD, Ralhan R. Promoter hypermethylation of p16INK4A, p14ARF, CyclinD2 and Slit2 in serum and tumor DNA from breast cancer patients. Life Sci. 2007;80:1873–1881. doi: 10.1016/j.lfs.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 20.Wu JY, Feng L, Park HT, et al. The neuronal repellent Slit inhibits leukocyte chemotaxis induced by chemotactic factors. Nature. 2001;410:948–952. doi: 10.1038/35073616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prasad A, Fernandis AZ, Rao Y, Ganju RK. Slit protein-mediated inhibition of CXCR4-induced chemotactic and chemoinvasive signaling pathways in breast cancer cells. J Biol Chem. 2004;279:9115–9124. doi: 10.1074/jbc.M308083200. [DOI] [PubMed] [Google Scholar]
- 22.Chalasani SH, Sabelko KA, Sunshine MJ, Littman DR, Raper JA. A chemokine, SDF-1, reduces the effectiveness of multiple axonal repellents and is required for normal axon path finding. J Neurosci. 2003;23:1360–1371. doi: 10.1523/JNEUROSCI.23-04-01360.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strickland P, Shin GC, Plump A, Tessier-Lavigne M, Hinck L. Slit2 and netrin 1 act synergistically as adhesive cues to generate tubular bi-layers during ductal morphogenesis. Development. 2006;133:823–832. doi: 10.1242/dev.02261. [DOI] [PubMed] [Google Scholar]
- 24.Robinson GW, Accili D, Hennighausen L. Rescue of mammary epithelium of early lethal phenotypes by embryonic mammary gland transplantation as exemplified with insulin receptor null mice. New York: Kluwer Academic/Plenum Press; 2000. pp. 307–316. [Google Scholar]
- 25.Srinivasan K, Strickland P, Valdes A, Shin GC, Hinck L. Netrin-1/neogenin interaction stabilizes multipotent progenitor cap cells during mammary gland morphogenesis. Dev Cell. 2003;4:371–382. doi: 10.1016/s1534-5807(03)00054-6. [DOI] [PubMed] [Google Scholar]
- 26.Silberstein GB, Daniel CW. Investigation of mouse mammary ductal growth regulation using slow-release plastic implants. J Dairy Sci. 1987;70:1981–1990. doi: 10.3168/jds.S0022-0302(87)80240-0. [DOI] [PubMed] [Google Scholar]
- 27.Tissir F, Wang CE, Goffinet AM. Expression of the chemokine receptor Cxcr4 mRNA during mouse brain development. Brain Res Dev Brain Res. 2004;149:63–71. doi: 10.1016/j.devbrainres.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 28.Lee GY, Kenny PA, Lee EH, Bissell MJ. Three-dimensional culture models of normal and malignant breast epithelial cells. Nat Methods. 2007;4:359–365. doi: 10.1038/nmeth1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bartoe JL, McKenna WL, Quan TK, et al. Protein interacting with C-kinase 1/protein kinase Cα-mediated endocytosis converts netrin-1-mediated repulsion to attraction. J Neurosci. 2006;26:3192–3205. doi: 10.1523/JNEUROSCI.3469-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu X, Chen H, Parker B, et al. HOXB7, a homeodomain protein, is overexpressed in breast cancer and confers epithelial-mesenchymal transition. Cancer Res. 2006;66:9527–9534. doi: 10.1158/0008-5472.CAN-05-4470. [DOI] [PubMed] [Google Scholar]
- 31.Dallol A, Da Silva NF, Viacava P, et al. SLIT2, a human homologue of the Drosophila Slit2 gene, has tumor suppressor activity and is frequently inactivated in lung and breast cancers. Cancer Res. 2002;62:5874–5880. [PubMed] [Google Scholar]
- 32.Richardson AL, Wang ZC, De Nicolo A, et al. X chromosomal abnormalities in basal-like human breast cancer. Cancer Cell. 2006;9:121–132. doi: 10.1016/j.ccr.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 33.Holland JD, Kochetkova M, Akekawatchai C, Dottore M, Lopez A, McColl SR. Differential functional activation of chemokine receptor CXCR4 is mediated by G proteins in breast cancer cells. Cancer Res. 2006;66:4117–4124. doi: 10.1158/0008-5472.CAN-05-1631. [DOI] [PubMed] [Google Scholar]
- 34.Lin EY, Li JF, Gnatovskiy L, et al. Macrophages regulate the angiogenic switch in a mouse model of breast cancer. Cancer Res. 2006;66:11238–11246. doi: 10.1158/0008-5472.CAN-06-1278. [DOI] [PubMed] [Google Scholar]
- 35.Orimo A, Weinberg RA. Stromal fibroblasts in cancer: a novel tumor-promoting cell type. Cell Cycle. 2006;5:1597–1601. doi: 10.4161/cc.5.15.3112. [DOI] [PubMed] [Google Scholar]
- 36.Kang H, Watkins G, Parr C, Douglas-Jones A, Mansel RE, Jiang WG. Stromal cell derived factor-1: its influence on invasiveness and migration of breast cancer cells in vitro, and its association with prognosis and survival in human breast cancer. Breast Cancer Res. 2005;7:R402–R410. doi: 10.1186/bcr1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubin JB, Kung AL, Klein RS, et al. A small-molecule antagonist of CXCR4 inhibits intracranial growth of primary brain tumors. Proc Natl Acad Sci U S A. 2003;100:13513–13518. doi: 10.1073/pnas.2235846100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Falco V, Guarino V, Avilla E, et al. Biological role and potential therapeutic targeting of the chemokine receptor CXCR4 in undifferentiated thyroid cancer. Cancer Res. 2007;67:11821–11829. doi: 10.1158/0008-5472.CAN-07-0899. [DOI] [PubMed] [Google Scholar]
- 39.Kang H, Mansel RE, Jiang WG. Genetic manipulation of stromal cell-derived factor-1 attests the pivotal role of the autocrine SDF-1-CXCR4 pathway in the aggressiveness of breast cancer cells. Int J Oncol. 2005;26:1429–1434. [PubMed] [Google Scholar]
- 40.Luker KE, Luker GD. Functions of CXCL12 and CXCR4 in breast cancer. Cancer Lett. 2006;238:30–41. doi: 10.1016/j.canlet.2005.06.021. [DOI] [PubMed] [Google Scholar]
- 41.Zagzag D, Krishnamachary B, Yee H, et al. Stromal cell-derived factor-1α and CXCR4 expression in hemangioblastoma and clear cell-renal cell carcinoma: von Hippel-Lindau loss-of-function induces expression of a ligand and its receptor. Cancer Res. 2005;65:6178–6188. doi: 10.1158/0008-5472.CAN-04-4406. [DOI] [PubMed] [Google Scholar]
- 42.Zhong H, De Marzo AM, Laughner E, et al. Overexpression of hypoxia-inducible factor 1α in common human cancers and their metastases. Cancer Res. 1999;59:5830–5835. [PubMed] [Google Scholar]
- 43.Dang DT, Chen F, Gardner LB, et al. Hypoxia-inducible factor-1α promotes nonhypoxia-mediated proliferation in colon cancer cells and xenografts. Cancer Res. 2006;66:1684–1936. doi: 10.1158/0008-5472.CAN-05-2887. [DOI] [PubMed] [Google Scholar]
- 44.Miller LD, Smeds J, George J, et al. An expression signature for p53 status in human breast cancer predicts mutation status, transcriptional effects, and patient survival. Proc Natl Acad Sci U S A. 2005;102:13550–13555. doi: 10.1073/pnas.0506230102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229–237. doi: 10.1056/NEJMoa044383. [DOI] [PubMed] [Google Scholar]
- 46.Fitzgibbons PL, Henson DE, Hutter RV. Benign breast changes and the risk for subsequent breast cancer: an update of the 1985 consensus statement. Cancer Committee of the College of American Pathologists. Arch Pathol Lab Med. 1998;122:1053–1055. [PubMed] [Google Scholar]
- 47.Jeffrey SS, Pollack JR. The diagnosis and management of pre-invasive breast disease: promise of new technologies in understanding pre-invasive breast lesions. Breast Cancer Res. 2003;5:320–328. doi: 10.1186/bcr655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.