Abstract
Heart failure is a leading cause of death in the United States, with around 5 million Americans currently suffering from congestive heart failure. The WANDA B. wireless health technology leverages sensor technology and wireless communication to monitor heart failure patient activity and to provide tailored guidance. Patients who have cardiovascular system disorders can measure their weight, blood pressure, activity levels, and other vital signs in a real-time automated fashion. The system was developed in conjunction with the UCLA Nursing School and the UCLA Wireless Health Institute for use on actual patients. It is currently in use with real patients in a clinical trial.
Keywords: Health monitoring, heart failure, real-time feedback, telemedicine, wireless health
I. Introduction
Congestive heart failure is a chronic condition that is a leading cause of hospitalization in the United States and a major part of the rising health care costs in the nation [1]. There are about 500,000 new cases of heart failure diagnosed each year in the US, and ten times that number of Americans currently suffer from heart failure. HF is characterized by decreased cardiac function caused by damage to the heart as a result of a heart attack, chronic hypertension, or exposure to toxins. The heart's inability to effectively pump blood results in fluid accumulation that manifests in the symptomatology of heart failure; namely shortness of breath, lower extremity swelling, chest pain, and limitations on exercise tolerance.
The most effective means of monitoring a patient's fluid status is to check his/her weight on a daily basis. An increase in weight indicates the retention of excess fluid, which requires increasing the dosage of diuretic medication to remove the excess fluid build-up. Close monitoring of patient weight has been shown to decrease the need for hospitalization, thus improving patient quality of life and decreasing the burden of this disease on the healthcare system. It is a simple but effective way for a patient to monitor his/her fluid balance and to take an active role in the management of the disease. However, the daily and precise monitoring of weight fluctuations has proven to be difficult for a large number of patients living with congestive heart failure. In addition, tracking other vital signs such as diastolic and systolic heart rate readings, daily calorie expenditure, and symptoms is also helpful. HF is often caused by systolic dysfunction where the heart muscle cannot pump or eject the blood out of the heart very well, or by diastolic dysfunction where the atrium does not fill up. As this pumping procedure stops, blood may back up in other areas of the body, producing congestion, e.g. in the lungs, the liver, the gastrointestinal tract or the arms and legs. This leads to a lack of oxygen and nutrition to other organs, which damages them and reduces their ability to work properly. Common symptoms of HF include shortness of breath with activity, or, after lying down for a while, coughing, swelling of feet and ankles, swelling of the abdomen, weight gain, irregular or rapid pulse, the sensation of feeling the heartbeat, difficulty sleeping, fatigue, weakness, faintness, loss of appetite, indigestion, etc. Many experts and researchers in cardiac medicine suggest monitoring those symptoms and tracking diastolic/systolic blood pressure and heart rate in order to prevent emergencies. Since those are also highly related to exercise, encouraging and monitoring patients' daily exercise are also essential [2]. However, without strong motivation to monitor one's vital signs and exercise regularly, and without user-friendly technology, it can be difficult to record and track patients' health information on a daily basis.
With an increasingly mobile society and the worldwide deployment of mobile and wireless networks, the wireless infrastructure can support many current and emerging healthcare applications. This technology employs the wireless technologies of GSM, satellite, radio, Bluetooth, Zigbee, and wireless LAN for communication. In addition, with recent advances in accelerometer, pressure, and gyroscope sensors among others, evaluating and monitoring daily physical activities and health conditions becomes can be accomplished more efficiently and more effectively. It aids bringing healthcare almost anytime and anywhere to anyone by removing constraints related to location and time and by improving quality. This wireless health concept includes pervasive health monitoring, intelligent emergency management systems, pervasive healthcare data access, and ubiquitous mobile telemedicine using smartphones. With wireless health applications and systems, patients can receive real-time feedback without visiting doctors or caregivers.
Wireless health technology can help patients who suffer from HF conditions by monitoring them and providing guidance and feedback using special computing facilities and algorithms. Patients who have cardiovascular system disorders can measure their weight, blood pressure, physical activity levels and other vital signs by using wireless health applications whenever and wherever they want. Also, the system will give a real-time computer-based analysis without visiting specialists. This helps prevent emergency situations and alert caregivers in order to help patients.
In this paper, we use Bluetooth-based weight scales, blood pressure monitors, WHI [12] Personal Activity Monitors (PAMs), touch-screen tablet PCs, cell phones, iPhones and an SMS message server system in order to monitor heart failure patients.
II. Related Work
Baker [3] discusses five prototypes of infant monitoring, alerting the deaf, blood pressure monitoring and tracking, and monitoring fire-fighter vital signs. The five prototypes use two sensor network mote technologies. One is the Tmote Sky, the latest derivative of the Berkeley Telos motes from Moteiv. The other one is the Corpand SHIMMER, Intel's Digital Health Group's platform for Sensing Health. In their Heart@Home blood pressure monitoring project, a SHIMMER mote is located on the wrist cuff connected to the electronic pressure sensor, and broadcasts these readings along with a time-stamp over the radio. Its PC-based software application provides a graph of the user's blood pressure and pulse rate over time.
Accelerometers are useful as they record intensity, frequency, and duration of activity as well as the total volume of activity accumulated. Movement is assessed directly with minimal hindrance to the user, making accelerometers ideal for users. Sherrill [4] develops a wearable sensor network which helps remotely monitor the activity of chronic obstructive pulmonary disease (COPD) patients. This system manipulates 2-axis or 3-axis accelerometers which are attached to the arms and legs. This system helps to monitor one's activity in the home or community, not in a constrained lab environment.
There are many advantages of using standardized health surveys across the patient population. They allow one to compare health profiles for groups in diagnosis, disease severity, and treatment regimens, and to monitor transitions in health status over time. The standardized health survey system also allows one to evaluate the relative benefits of different treatments, and to compare health outcomes across different health care systems. Widely used health status measurements must yield high quality data across diverse populations. McHorney [5] shows considerable evidence of the appropriateness of using the SF-36 survey system across different medical groups. This study shows high data completeness, and internal-consistency reliability.
Approximately 95 percent of all mobile phones in the U.S. today are capable of sending and receiving SMS (short message service) text messages. As of 2007, more than 100 million of the 250 million mobile phone subscribers in U.S. have used text messaging, and more than 41 million people send text messages every day. Mobile phones may provide an opportunity to improve behaviors like self-monitoring, in particular through the use of SMS text messages. For example, Obermayer [6] shows that sending text messages to mobile phones increases the effectiveness of a smoking cessation intervention among college students. Another study among young adults in New Zealand revealed that participants who received text messages were more likely to quit smoking in 6 weeks than those who used controls [7]. In a program conducted among youth with type 1 diabetes by Franklin [8], daily text messages were helpful for disease self-management, increased self-efficacy, and treatment adherence and achieved high satisfaction among participants.
Since there is no combined work that uses a home-based wireless health and activity status monitoring system, a touchscreen tablet PC-based standardized questionnaire system, and an SMS health-monitoring and usability questionnaire system, we designed a unified system especially designed for heart failure patients.
III. System Design
The overall system architecture is presented in Fig 3.1. In order to collect patients' information, the developed system uses a survey system. Answers to the survey questionnaires are delivered to the WANDA B. web-database through a 3G wireless connection. In addition, WANDA B. collects weight, blood pressure, activity, and daily SMS surveys. Whenever a patient measures one's weight and blood pressure, values are transmitted to the web-server via Bluetooth and a phone line connection. Answers to daily SMS questionnaires and calorie expenditure data values are also stored in the database. This data is accessible through the WANDA B. web application and through an iPhone application allowing one to monitor patients in real-time.
Fig 3.
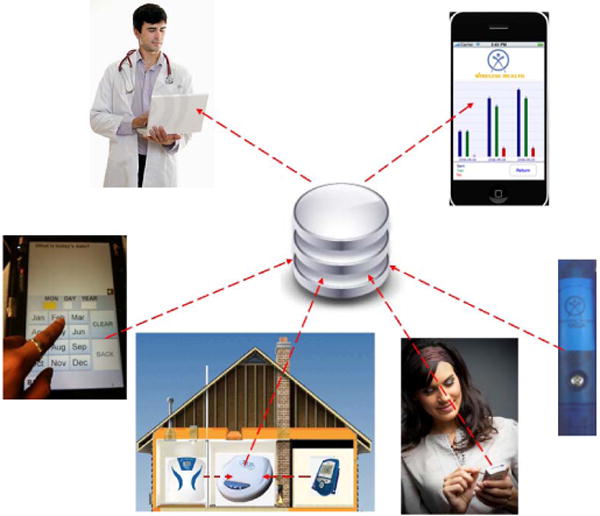

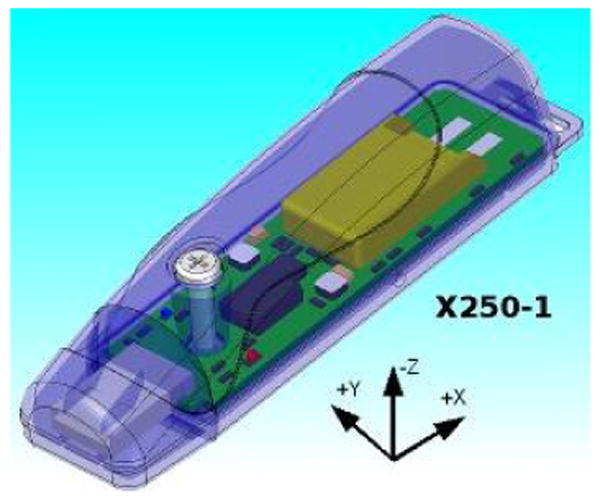
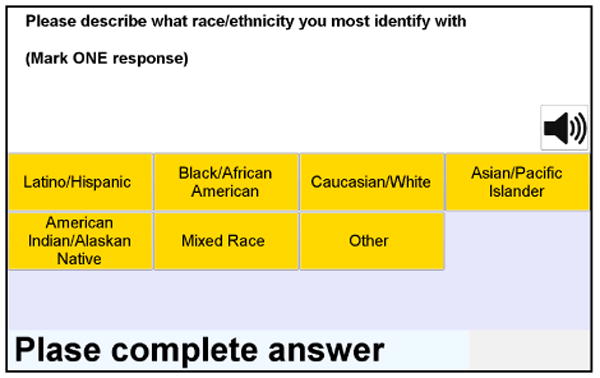
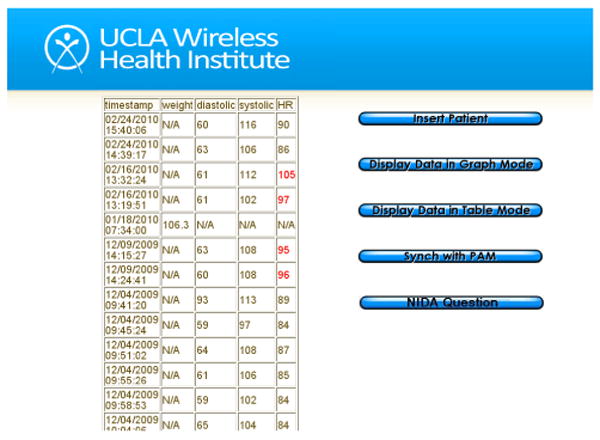
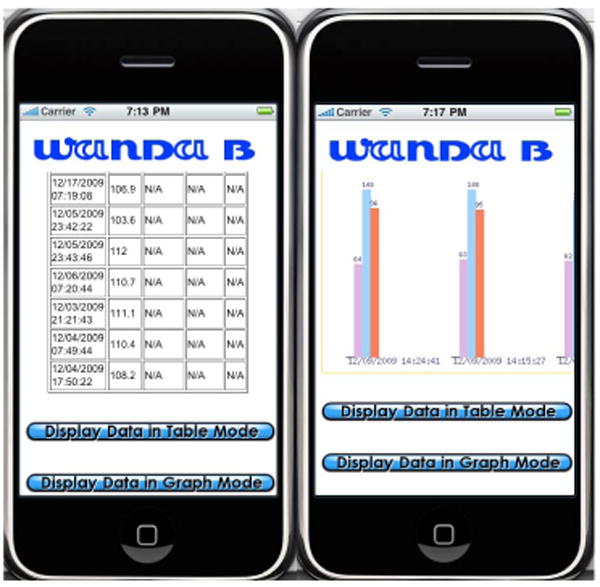
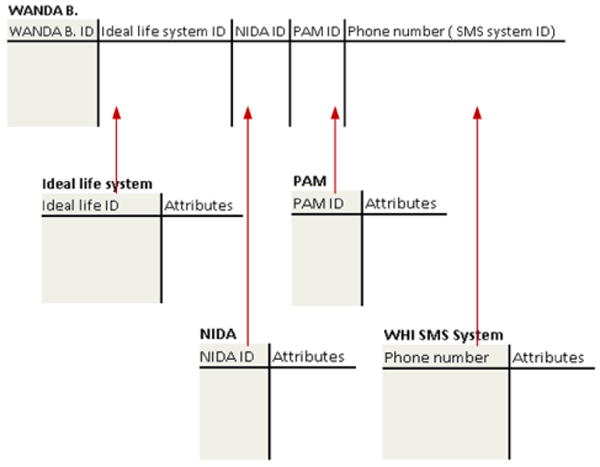
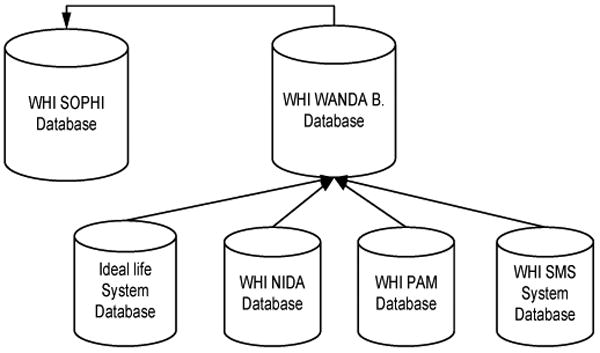
Fig 3.1. The WANDA B. system
Fig 3.2. Ideal Life Body Manager™, BP Manager™, and POD™
Fig 3.3. WHI PAM (Personal Activity Monitor)
Fig 3.4. WHI NIDA survey system
Fig 3.5. WANDA B. web application
Fig 3.6. WANDA B. iPhone application
Fig 3.7. Database structure in WANDA B. and a shared ID table
Fig 3.8. Database synchronization and recovery
A. The Weight and Blood Pressure Monitoring System
The Ideal Life system [10] includes the Body Manager™ body weight scale the BP Manager™ blood pressure monitor device that quickly and accurately measures diastolic blood pressure, systolic blood pressure and heart rate. The Body Manager™ and BP Manager™ systems collect weight and blood pressure data and send it to the Ideal Life Pod ™. Since the system supports Bluetooth, systems can communicate in the range of 300-400 feet. When the Ideal Life Pod™ receives data, it transmits data to the database system. Since WANDA B. is designed for patients who are not accustomed to using computers, the only requirement is that one connects an Ideal Life Pod™ system to a standard phone line. Then the main database server and Pod™ communicate via long-distance phone service plan.
B. The Activity Monitoring System
The WHI Personal Activity Monitor, or PAM, shown in Fig 3.3, is a small, light-weight, triaxial accelerometer-based activity recorder. The WHI PAM's small form factor allows it be easily carried in a patient's pocket, for example. The sample rate as well as the minimum acceleration threshold can be adjusted to ensure that data resolution requirements are met while optimizing for longer battery life. Time-series acceleration data is stored using an on-board flash memory card. Data transfer is achieved via USB on an internet-enabled PC, but future designs will support wireless communication. Using a patient's age, gender, height, and weight, the WHI PAM system calculates daily caloric expenditure based on the metabolic equivalents (METs) associated with approximations of the patient's activity levels throughout the day.
Based on activity information detected by the PAM device, it calculates the METs value (Table 3.1). Calories burned by each activity, then, are calculated by the following equation ([9])
Table 3.1. Activity levels and METs values.
| Physical Activity | MET |
|---|---|
| Light Intensity Activities | < 3 |
| Sleeping | 0.9 |
| writing, desk work, typing | 1.8 |
| walking, less than 2.0 mph (3.2 km/h), level ground, strolling | 2 |
| Moderate Intensity Activities | 3 to 6 |
| bicycling, stationary, 50 watts, very light effort | 3 |
| sexual activity (position dependent) | 3.3 |
| calisthenics, home exercise, light or moderate effort, general | 3.5 |
| bicycling, <10 mph (16 km/h), leisure, to work or for pleasure | 4 |
| bicycling, stationary, 100 watts, light effort | 5.5 |
| Vigorous Intensity Activities | > 6 |
| jogging, general | 7 |
| calisthenics, heavy, vigorous effort | 8 |
| running jogging, in place | 8 |
Calories = ((METs * 3.5 * weight (kg))/200) * duration (min)
C. The Survey System
NIDA is a touch-screen-based survey system that is operated on desktops, laptops and tablet PCs. NIDA uses an open XML-based format for questions and results, and supports text-to-voice functionality. For various users it provides several language options such as English, Spanish, etc. Therefore, depending on the user's preference, users can choose a language and choose to communicate by either text or voice. It stores and retrieves data from the remote site using the 3G wireless network. If there is no 3G network connection, NIDA stores data in a local database and waits until the device is in a 3G network area to upload data to the web database. Since it is computer-based, questionnaires are more standardized, and answers can be highly completed, as McHorney ([5]) emphasizes and implements. Additionally, since users don't need to be with interviewers, NIDA improves efficiency and reduces costs. Using light-weight tablet PCs, patients are more likely to answer frankly and freely than in the presence of interviewers. This unit is used at the beginning of the WANDA B. study in order to gather basic user information. Also, this system is used periodically to track the user's health status.
D. The Daily SMS Questionnaire System
Based on a schedule set by doctors, WANDA B.'s daily SMS survey system sends the SMS questionnaire in Table 3.2 in order to check any heart failure symptoms. The corresponding user responses (0: Not at all, 1: A little, 2: A great deal, 3: Extremely) are collected and recorded by the WHI SMS database. This SMS system sends a text message to the users to which they can reply in the same way as they do with their friends.
Table 3.2. WANDA B's daily SMS questions.
| Questionnaire Items |
|---|
| I could feel my heart beat faster |
| I could not breathe when I laid down |
| I felt pain in my chest |
| I had an upset stomach |
| I had a cough |
| I was tired |
| I could not catch my breath |
| My feet were swollen |
| I woke up at night because I could not breathe |
| My shoes were tighter than usual |
| I gained 3 or more pounds in the past week |
| I could not do my usual daily activities because I was short of breath |
WANDA B. also sends 25 usability questions via text message every month to obtain input from patients' on the system's usability (e.g. ease of use, usefulness). This information will be used to evaluate the system's feasibility from the patients' perspective.
E. The WANDA B. Web and iPhone Application
WANDA B. provides two different monitoring applications for healthcare providers. One is a web application ([13]), and the other is an iPhone application. Both the web application and the iPhone application have functions to check patients' weight, blood pressure, heart rate, and calorie consumption. Data can be viewed as graphs or tables. Also, the web application shows a statistical result of SMS answers. The graph mode shows the amount of calories burned in hourly-based format and other values in daily-based format (Fig 3.5).
The access to the web application requires user verification in order to prohibit random access by unauthorized users. The initial page asks for the user's ID and password which is only provided to approved users in a private meeting. Also, via the WANDA B. webpage, healthcare providers can add more patients and synchronize devices if needed.
An iPhone's 3.5 inch multi-touch display with 480-by-320-pixel resolution lets users navigate by touching the screen. The iPhone 3G uses a technology protocol called HSDPA (High-Speed Downlink Packet Access) to download data quickly over UMTS (Universal Mobile Telecommunications System) networks. In addition, its weight is only 135g, so it's easy to carry. Therefore, the WANDA B. iPhone application helps users access the same content in WANDA B. web database. Using a WANDA B. application on an iPhone enables caregivers to monitor patient status whenever and wherever they want. In the table mode, healthcare providers can check patient's daily answers to questionnaires, weight, blood pressure, heart rate, and calorie expenditure values. The table mode also provides statistical vales. The graph mode displays each value as a color bar (Fig 3.6).
F. The SMS Reminder and Alert System
For more accurate patient monitoring and analysis, WANDA B. was programmed to send text reminders to patients who fail to transmit their daily weights and health status data. Weight, blood pressure, and heart rate data that are transmitted daily are reviewed immediately after data transmission. If values are out of the threshold range (Table 3.3), it alerts healthcare providers to take action. In addition, if patient responses to any of the questions on Table3.2 are “3-a great deal” or “4-extremely”, the system will also send an alert message to the healthcare provider. Alert messages are sent via SMS, e-mail, and by phone.
Table 3.3. Acceptable range of each measured value.
| Values | Range |
|---|---|
| Systolic | > 90 |
| Diastolic | > 50 |
| Heart rate | < 90 or > 40 |
| Weight | < +2 (lb./day) |
G. System Integration and Backup
The need to combine records from different systems or healthcare organizations exists for many reasons, including patients moving or changing health care providers. To make all patients' medical records accessible to care providers, Bell [15] makes electronic medical records linked together using a massively distributed Master Patient Index (MPI). A MPI is a facility that correlates and references patient identifiers and performs matches. WANDA B. is also an integrated architecture of different systems such as Ideal Life system units, WHI NIDA, WHI PAM devices, and the WHI SMS system. Each system has its own database, patient ID, and item ID to distinguish each input measured by patients. In order to integrate data in distributed systems, a shared ID table is used in the WANDA B. system. To join keys used in Ideal Life systems, NIDA, and the PAM and SMS systems, the WANDA B. ID is used. Other input in different system databases are referenced via the WANDA B. ID table and original database tables (Fig 3.7) which enables the linkage of information located in several systems to a specific patient.
As data in the WANDA B. system is critical and personal, the lost of data is fatal. If there is missing data, the system cannot evaluate the patient's status accurately and give proper directions to the user. In order to preserve data, WANDA B. calls the WHI SOPHI database [11] every midnight and stores information accumulated during the day (Fig 3.8). WHI SOPHI is a database integration project, and it stores and displays web pages, files, and data from all projects at the UCLA WHI. Data backups are useful for restoring state following a disaster and restoring small numbers of files after they have been accidentally deleted or corrupted. Liu [16] also designed a federation of PACS that can be created, allowing a failed PACS archive to recover its image data from others in the federation in a seamless fashion.
IV. Test Bed
The use and testing of WANDA B. has approved by the UCLA Institutional Review Board (IRB), which approves, monitors, and reviews biomedical and behavioral research involving humans with the aim to protect the rights and welfare of the research subjects. Pilot data on Table 4.1 is being collected to test the system, since November, 31, 2009. Data from this pilot study will provide the information needed to develop a protocol for using the system in major clinical trials across different patient populations.
Table 4.1. Information about objects of the experiment.
| ID | Gender | Age | Height |
|---|---|---|---|
| 1 | Female | 21 | 5′2 |
| 2 | Female | 26 | 5′4 |
| 3 | Male | 46 | 5′7 |
| 4 | Male | 76 | 5′11 |
| 5 | Female | 55 | 5′1 |
| 6 | Female | 58 | 5′7 |
V. Conclusion
Heart failure is a leading cause of death in USA, and there are about 5,000,000 Americans currently suffering from heart failure. Wireless health technology that uses sensors and wireless communication methods can help those heart failure patients by monitoring them and providing guidance and feedback. Patients who have cardiovascular system disorders can measure their weight, blood pressure, activity and other vital signs by using wireless health applications whenever and wherever they need to. Also, the system will give a real-time and computer-based analysis without visiting specialists. This helps prevent emergency situations and alert caregivers in order to help patients.
In this paper, we presented the Weight and Activity with Blood Pressure Monitoring System (WANDA B.). WANDA B. uses a Bluetooth weight scale, a blood pressure monitor, WHI PAM (Personal Activity Monitor), NIDA, and WHI's SMS system. In order to use Ideal Life weight scales and blood pressure monitors, the user is only required to connect an Ideal Life Pod™ system to a standard phone line. Then, the main database server and a system communication unit send and receive data via long-distance phone service plan. The WHI PAM (Personal Activity Monitor) is a 3-axis accelerometer-based activity analyzer that calculates METs and calories burned during a day. NIDA is a touch-screen-based survey system that is operated on desktops, laptops and tablet PCs. Since users don't need to be with interviewers, NIDA improves efficiency and reduces costs. Also, using light-weight tablet PCs, patients are more likely to answer frankly and freely without interview bias. This unit is used at the beginning of the WANDA B. study in order to gather basic user information. Based on a schedule set by doctors, WANDA B.'s daily SMS survey system sends the SMS messages in Table 3.2 in order to check for heart failure symptoms. The SMS system sends a text message to the users to which they can reply in the same way as they do with their friends.
WANDA B. is an integrated architecture of different systems such as Ideal Life system units, WHI NIDA, WHI PAM, and WHI SMS system. Each system has its own database, patient ID, and item ID to distinguish each input measured in patients. In order to integrate data in a distributed system, a shared ID table is used in the WANDA B. system. As data in the WANDA B. system is critical and personal, the lost of data is fatal. In order to preserve data, WANDA B. calls the WHI SOPHI database every midnight and backs up information accumulated during the day.
WANDA B. provides a web application and an iPhone application for monitoring patients in real time. Also, if any value is out of the acceptable range, the system alerts caregivers to prevent any dangerous situations. Since heart rate, diastolic blood pressure, systolic blood pressure, and weight values are especially critical in heart failure, the system continuously monitors these values.
Fig 1.1. Devices used in WANDA B.

Acknowledgments
This publication was partially supported by Grant Number T15 LM07356 from the NIH/National Library of Medicine Medical Informatics Training Program
The authors would like to acknowledge the funding source: National Institute of Health-National Heart, Lung, and Blood Institute Grant 1R01HL093466-01. Dr. Evangelista also received support from the University of California, School of Nursing Intramural Research Grant and the University of California, Los Angeles, Resource Centers for Minority Aging Research/Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30-AG02-1684. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health. We would like to thank Professor William Kaiser and Professor Alex Bui for their helpful advice.
References
- 1.http://www.cvphysiology.com/Heart%20Failure/HF002.htm
- 2.http://www.nlm.nih.gov/medlineplus/ency/article/000158.htm
- 3.Baker CR. Wireless sensor networks for home health care. 21st International Conference on Advanced Information Networking and Applications Workshops (AINAW'07).2007. [Google Scholar]
- 4.Sherrill DM. Accelerometer-based measurement of exercise and mobility for pulmonary rehabilitation. IEEE 30th Annual Northeast Bioengineering Conference 2004.2004. [Google Scholar]
- 5.McHorney CA. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical care. 1994;32(1):40. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Obermayer JL. College smoking-cessation using cell phone text messaging. J Am Coll Health. 2004;53(2):71–78. doi: 10.3200/JACH.53.2.71-78. [DOI] [PubMed] [Google Scholar]
- 7.Rodgers A, C Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14(4):255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franklin VL. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 9.Jones NL. Clinical exercise testing. 2nd. Philadelphia: W. B. Saunders; 1982. [Google Scholar]
- 10.http://www.ideallifeonline.com/public/
- 11.http://cs.ucla.edu/∼ani/SOPHI/
- 12.http://www.wirelesshealth.ucla.edu/
- 13.http://www.wanda.net
- 14.Banerjee A. Challenges of Implementing Cyber-Physical Security Solutions in Body Area Networks. International Conference on Body Area Networks (BodyNets'09).2009. [Google Scholar]
- 15.Bell GB. Matching records in a national medical patient index. Comm ACM. 2001;44(9):83–88. [Google Scholar]
- 16.Liu BJ. Utilizing data grid architecture for the backup and recovery of clinical image data. Computerized medical imaging and graphics. 2005;29(2-3):95. doi: 10.1016/j.compmedimag.2004.09.004. [DOI] [PubMed] [Google Scholar]


