Abstract
This study investigates the potential heterogeneity of ecstasy or MDMA (3,4-methylenedioxy-N-methylamphetamine) users. Data came from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Latent class analysis (LCA) and multinomial logistic regression procedures were used to identify subtypes of ecstasy users. Approximately 1.6% (n=562) of adult participants (N=43,093) reported lifetime ecstasy use. LCA identified three subtypes of ecstasy users. Class 1 exhibited pervasive use of most drug classes (ecstasy–polydrug users, 37%). Class 2 reported a high rate of use of marijuana and cocaine and a moderate use of amphetamines (ecstasy–marijuana–stimulant users, 29%). Class 3 was characterized by a high rate of use of marijuana and a low use of primarily prescription-type drugs (ecstasy– marijuana users, 34%). Subtypes were distinguished by family income, history of substance abuse treatment, and familial substance abuse. Class 1 exhibited the highest prevalence of disorders related to the use of marijuana (77%), tobacco (66%), amphetamines (36%), opioids (35%), sedatives (31%), and tranquilizers (30%). The recent resurgence in ecstasy use among adults underscores the need to monitor trends in its use.
INTRODUCTION
The use of ecstasy or MDMA (3,4–methylenedioxymethamphetamine) constitutes an important public health concern.1 Recreational ecstasy use is associated with a long list of adverse effects, such as impaired driving, aggression, liver and heart damage, memory and other cognitive deficits, impaired immune competence, psychiatric distress and disorders, hormonal changes, and mortality.1,2 Ecstasy is also one of the most compromising and controversial illicit drugs due to its potential for serotonergic neurotoxicity and behavioral disturbances.1–4 Polysubstance use is often cited as a confounder in research on ecstasy’s neurotoxic effects, which not only creates challenges in attributing adverse consequences in drug users to any given drug, but also enhances the likelihood of neurotoxic and other adverse effects in ecstasy users.5–7 In this study, we capitalize on data from a nationally representative study of psychiatric comorbidity to understand the heterogeneity of ecstasy users in regards to substance use and psychiatric disorders. An understanding of the nature of these different subtypes is critical to etiological and prevention research.
Ecstasy comprises properties of both stimulants and hallucinogens and is classified as a hallucinogen.8 It is commonly known as one of several “club drugs” (eg, MDMA, methamphetamine, and d–lysergic acid diethylamide or LSD) that are used to maintain the high energy levels required for extended periods of dancing or to generate an altered state of consciousness.9 In the United States, ecstasy use reportedly increased significantly during the 1990s and early 2000s.9,10 When this trend was first noticed, the drug appeared to be used predominantly by whites and party or club participants, but it spread later to nonwhite groups (eg, Hispanics and blacks) and non-club settings.9,10 National treatment-related data have also revealed a significant increase in ecstasy/MDMA-related mortality and admissions to emergency departments from 1994 and 2001.11,12 Since 2002, national surveys of American students and the general population have shown a decline in ecstasy use.13,14 However, recent results from both Monitoring the Future Surveys13,15 and the National Survey on Drug Use and Health14 suggest that ecstasy use increased from 2006–2007 and remained stable in 2008. Nationally, the estimated number of new past-year ecstasy users decreased from 1.2 million in 2002 to 642,000 in 2003 and then rose to 860,000 in 2006, which was similar to the estimate in 2007.14 The vast majority (61–70%) of new ecstasy users in the United States are adults.14
Several studies have found that many ecstasy users also use alcohol, marijuana, and other stimulants such as cocaine and amphetamines.7,16–19 It has been suggested that stimulants are consumed to enhance ecstasy’s effects, while marijuana is often used to alleviate the discomfort and adverse mood states associated with the period following ecstasy use.17,20 Polydrug use, however, is likely to have particularly adverse neuropsychobiological effects.4,7 For example, because stimulants are also neurotoxic upon serotonergic and dopamine neurons, they may interact with ecstasy to enhance its adverse effects on users.5,7 Ecstasy’s reported associations with polysubstance use, as well as its negative effects, have important implications for prevention and intervention. As of now, there is limited information available concerning what particular subgroups may be at high risk for exhibiting substance use disorders (SUDs) and that should thus receive tailored or intense interventions. Little is also known about the extent to which ecstasy users are characterized by a severe pattern of psychiatric disorders, and whether early case finding and intervention within this population is warranted. Given the recent increase in ecstasy use among adults,14 we need to characterize better various types of users who constitute this population in order to identify vulnerable subgroups for tailored interventions.
Latent class analysis (LCA) is a particularly suitable method for investigating whether distinct subtypes or classes of drug users exist within a diverse sample of study participants.21,22 LCA’s unique strength lies in its capability to specify “unobserved” or “latent” subgroups of individuals. It has already been used to enhance the field’s understanding of variability in polysubstance use patterns.16 In LCA, observed variables are viewed as imperfect indicators of an underlying and unobserved construct, and a finite number of mutually exclusive classes are empirically derived from the analysis of co-occurring patterns of dichotomous variables. LCA thus can help elucidate whether there are discrete sets of ecstasy users by classifying them empirically into a few subgroups according to their reported use patterns of a variety of drugs. In this study, we apply LCA to investigate the existence of subtypes of ecstasy users. Study data are drawn from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), which is the largest national study of psychiatric comorbidity among American adults.23 NESARC also includes the most comprehensive assessment of psychiatric disorders presently available. Data concerning participants’ history of substance abuse treatment and familial substance abuse—a potentially robust indicator of severe substance abuse24,25—also help to determine their differential associations with various subtypes.
Recently, Keyes et al.26 examined the association of ecstasy use with mental and alcohol use disorders among young adults aged 18–29 years in the 2001–2002 NESARC. They found that both past-year and former ecstasy users as compared to non-drug users had increased odds of exhibiting alcohol use disorders, panic disorder, dysthymia, and antisocial personality disorder in their lifetime. Additionally, a history of bipolar and social phobia was associated with former ecstasy use, while a history of specific phobia was associated with past-year ecstasy use. Similarly, non-ecstasy drug users had greater odds of exhibiting all these lifetime disorders than non-drug users. Direct comparisons in psychiatric disorders between ecstasy users and non-drug users, however, are not reported by Keyes et al.26 Specific drug use disorders and nicotine dependence also are not examined by Keyes et al.26 In this paper, we extend from prior research26 by examining each of all SUDs among adult ecstasy users aged 18 and older and by applying LCA to enhance our investigation of subtypes of ecstasy users and their distinct profiles in demographics, history of substance abuse treatment and familiar substance abuse, specific SUD, and metal disorders. For ease of interpretations, we also examine prevalence rates and corresponding 95% confidence intervals of all disorders for non-ecstasy drug users. Two main questions are examined: 1) Are there subtypes of ecstasy users that are distinguished by their patterns of drug use? 2) If so, are various subtypes of ecstasy users associated with distinct socioeconomic characteristics, patterns of substance use and related disorders, history of substance abuse treatment and familial substance abuse, and mental disorders?
METHODS
Study Sample
The NESARC was designed and funded by the National Institute on Alcohol Abuse and Alcoholism, with supplemental support from the National Institute on Drug Abuse. It provides prevalence rates for both the Diagnostic and Statistical Manual of Mental Disorders, Fourth Revision (DSM-IV) Axis I (substance use, mood, and anxiety disorders) and Axis II (personality) disorders, and is the first national study to assess DSM-IV personality disorders.23 The target population was the civilian non-institutionalized population aged 18 years or older who resided in the United States or the District of Columbia, including Alaska and Hawaii. Eligible participants consisted of persons living in households, military personnel living off base, and residents of group quarters (ie, boarding houses, rooming houses, non-transient hotels and motels, shelters, facilities for housing workers, college quarters, and group homes). Study participants were selected using a multistage cluster sampling design. Professional lay interviewers from the Bureau of the Census administered the face-to-face personal interviews using computer assisted personal interviewing for the survey. Rights to confidentiality of NESARC participants were carefully protected. All NESARC participants provided written informed consent and were assured that their participation was voluntary. To increase the accuracy of national estimates of psychiatric disorders for various demographic subgroups, Hispanics (N = 8,308), non–Hispanic blacks (N = 8,245), and participants aged 18–24 years (N = 5,199) were oversampled. Of the 43,093 participants, 18,518 were male and 24,575 were female. The household and individual response rates were 89% and 93%, respectively. The overall survey response rate was 82%. Details of the survey designs are reported elsewhere.23
Study Variables
Demographic and socioeconomic variables examined included age, gender, race/ethnicity, educational level, current marital status, and total annual family income.19,27
In the drug use module, participants were given a flashcard and then indicated whether they had ever used each of nine drug classes listed on the card: marijuana, inhalants/solvents, cocaine/crack, hallucinogens/ecstasy, heroin, sedatives, amphetamines, tranquilizers, and opioids/analgesics. Drug use included the use of marijuana, inhalants/solvents, cocaine/crack, hallucinogens/ecstasy, heroin, and the nonmedical use of sedatives, amphetamines, tranquilizers, and opioids/analgesics. For hallucinogen use, participants first indicated whether they had ever used a hallucinogen (ie, ecstasy/MDMA, LSD, mescaline, psilocybin, phencyclidine or PCP, angel dust, or peyote). Those who reported any lifetime hallucinogen use were asked to report their use of ecstasy/MDMA. Participants who responded affirmative to the latter question were considered lifetime ecstasy users.26 Lifetime drug users who had never used ecstasy were referred as non-ecstasy drug users. Lifetime use of alcohol, tobacco, and each specific drug class was dichotomized.
Psychiatric disorders were assessed with the Alcohol Use Disorders and Associated Disabilities Interview Schedule–DSM-IV, an instrument of demonstrated reliability and validity.28 Participants were assessed on problems and disorders related to mood (major depression, dysthymia, mania, and hypomania), anxiety (panic disorder, agoraphobia, social phobia, specific phobia, and generalized anxiety disorder), personality (avoidant, dependent, obsessive-compulsive, paranoid, schizoid, histrionic, and antisocial), and substance use (tobacco/nicotine, alcohol, inhalants, marijuana, cocaine, hallucinogens, sedatives, amphetamines, tranquilizers, and opioids/analgesics).
Participants’ personal histories of substance abuse treatment were defined as having ever received any treatment or services for problems related to alcohol or drug use at any location (eg, an inpatient ward, outpatient clinic, emergency room, addiction treatment program, mental health treatment program, self-help group, jail, or church).29,30 A family history of substance abuse included any self-reported positive family history of alcohol or drug use problems among any of the respondent’s biological family members (ie, natural parents, sons, daughters, grandparents, full brothers, and full sisters).
Data Analysis
Data were drawn from the public-use data file of the 2001–2002 NESARC. Because NESARC used a complex multistage survey design, data were weighted and analyzed with SUDAAN.31 Demographic distributions and the prevalence of ecstasy use among all participants (N = 43,093) were examined. Within the subsample of lifetime ecstasy users (n = 562), the prevalence of hallucinogen use disorders and other drug use were calculated. LCA using Mplus32 was then applied to seven dichotomous drug use variables (any lifetime use of inhalants, cocaine, heroin, sedatives, amphetamines, tranquilizers, and opioids/analgesics, respectively) to empirically determine subtypes of ecstasy users. Because almost all ecstasy users (98%) reported consuming marijuana, this drug was excluded from the LCA. We evaluated the fit of models between two and six latent classes. Bayesian Information Criterion (BIC), entropy, and parsimony were all considered in selecting the final model.33,34 In general, lower BIC values indicate a better model. Entropy ranges from 0 to 1, with higher values indicating a clearer delineation of classes.
Multinomial logistic regression procedures31 were then conducted to determine whether LCA-defined subtypes differed in regards to participants’ socioeconomic characteristics, as well as variables related to their use of substance abuse treatment, familial substance abuse, and hallucinogen use. Finally, prevalence rates of specific psychiatric disorders by LCA-defined subtype were determined. For reference purposes, we also report rates of specific psychiatric disorders among drug users who had never used ecstasy. All results presented are weighted estimates except for sample sizes.
RESULTS
Prevalence of Ecstasy Use
Approximately 1.6% (n = 562) of study participants reported lifetime use of ecstasy, representing an estimated 3.2 million adults aged 18 years or older. A comparatively high prevalence of ecstasy use was found among young adults aged 18–29 years (4.8%), men (2.1%), whites (1.8%), American Indians/Alaska natives (2.4%), those who had never married (4.3%), and those who reported a family history of substance abuse (2.2%) or a personal history of using substance abuse treatment services (8.1%) (χ2 p < 0.01 for each comparison).
Ecstasy Users versus Non-Ecstasy Users
Regardless of ecstasy use, drug users were likely to be white and to have attended college than non-drug users (Table 1). Ecstasy users were more likely to be younger, single, and male than non-ecstasy drug users and non-drug users, but they were more likely than non-ecstasy drug users to be in the lowest family income group (<$35,000).
TABLE 1.
Selected demographic characteristics of ecstasy users, non-ecstasy drug users, and non-drug users in the 2001–2002 national epidemiologic survey on alcohol and related conditions (N = 43,093)
| Selected demographics, Weighted column % (95% CI) |
Ecstasy users | Non-ecstasy drug users | Non-drug users | χ2(df) P-values |
|---|---|---|---|---|
| Unweighted sample size | n = 562 | n = 8,578 | n = 33,953 | |
| Age group | ||||
| 18–29 years | 68.2 (63.0–72.9) | 24.9 (23.7–26.3) | 20.0 (19.2–20.8) | |
| 30–44 years | 25.3 (21.1–30.0) | 42.6 (41.2–44.0) | 27.8 (27.2–28.6) | 190.52 (4) |
| 45 years or older | 6.5 (4.8–8.9) | 32.5 (31.2–33.8) | 52.2 (51.0–53.4) | P < .001 |
| Gender | ||||
| Male | 63.4 (59.1–67.6) | 56.17 (54.9–57.5) | 45.3 (44.7–46.0) | 98.41 (2) |
| Female | 36.6 (32.4–40.9) | 43.8 (42.5–45.2) | 54.7 (54.0–55.4) | P < .001 |
| Race/ethnicity | ||||
| Black | 2.5 (1.5–4.1) | 10.2 (8.7–11.5) | 11.5 (10.3–12.9) | |
| Hispanic | 9.2 (6.7–12.4) | 8.0 (6.4–10.0) | 12.6 (10.1–15.5) | |
| Other | 8.0 (5.7–11.1) | 5.3 (4.5–6.2) | 6.8 (5.7–8.1) | 78.65 (8) |
| White | 80.4 (75.8–84.3) | 76.7 (74.0–79.2) | 69.1 (65.6–72.4) | P < .001 |
| Educational level | ||||
| < High school | 11.8 (8.8–15.7) | 11.1 (10.1–12.2) | 17.0 (15.9–18.1) | |
| High school | 24.6 (20.0–30.0) | 26.1 (24.5–27.8) | 30.3 (29.2–31.4) | 71.00 (4) |
| ≥College | 63.6 (58.2–68.7) | 62.8 (60.8–64.7) | 52.7 (51.5–53.9) | P < .001 |
| Total family income | ||||
| 0–$34,999 | 47.4 (42.2–45.1) | 38.0 (36.1–40.0) | 45.3 (43.9–46.6) | |
| $35,000–$69,999 | 29.2 (24.7–34.2) | 32.5 (31.2–33.8) | 32.1 (31.4–32.8) | 47.52 (4) |
| $75,000+ | 23.4 (19.0–28.5) | 29.5 (27.4–31.7) | 22.7 (21.4–24.0) | P < .001 |
| Marital status | ||||
| Wid./sep./divorced | 9.2 (6.6–12.6) | 16.0 (15.1–16.9) | 18.0 (17.5–18.5) | |
| Never married | 57.4 (52.5–62.3) | 24.4 (23.0–25.8) | 19.2 (18.3–20.2) | 85.74 (4) |
| Married | 33.4 (28.9–38.1) | 59.6 (58.0–61.2) | 62.7 (61.8–63.7) | P < .001 |
CI: confidence intervals
Prevalence of Hallucinogen Use Disorders
Among all participants, 1.7% met criteria for a lifetime DSM-IV hallucinogen use disorder (1.5%, abuse; 0.2% dependence). Among the subsample of ecstasy users, 31% met criteria for hallucinogen abuse, and an additional 6% met criteria for lifetime hallucinogen dependence.
Drug Use among Ecstasy Users
Marijuana (98%) and cocaine (61%) were the most common drugs used by ecstasy users, followed by opioids/analgesics (45%), amphetamines (41%), tranquilizers (39%), sedatives (39%), and inhalants (25%). About 5% of ecstasy users reported lifetime heroin use.
Latent Class Analysis
Results of LCA suggested a three-class model as the best fit based on the consideration of parsimony, clearer delineation of classes, and statistical power (ie, adequate sample size in each class). This model yielded the highest entropy value (0.90) and a relatively low BIC value (4078).
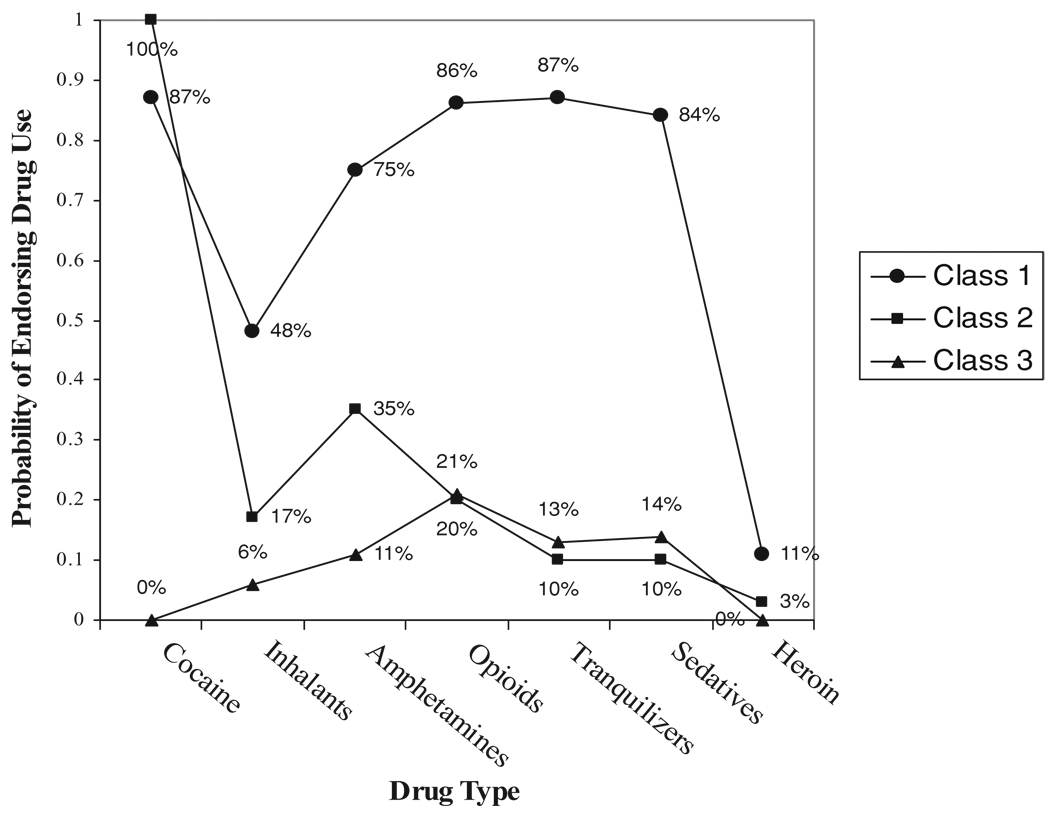
The three classes were distinguished by the extent of participants’ lifetime drug use (Figure 1). Class 1 (ecstasy–polydrug users) specified a large group (37%) of ecstasy users who manifested a high probability of using many types of drugs. Class 2 (ecstasy–marijuana–stimulant users, 29%) were users of marijuana and cocaine, and they also exhibited a moderate probability of using amphetamines. Class 3 (ecstasy–marijuana users, 34%) mainly used marijuana as their other psychoactive drug.
FIGURE 1.
Latent class analysis of subtypes of ecstasy/MDMA users in the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (N = 562). Class 1: Ecstasy–polydrug users. Class 2: Ecstasy–marijuana–stimulant users. Class 3: Ecstasy–marijuana users
Multinomial Logistics Regression Analysis of LCA-Defined Ecstasy Subtypes
Relative to the ecstasy–marijuana subtype (Table 2), older age (≥45 years), a low level of family income (<$35,000), onset of hallucinogen use before age 18 years, and a personal history of substance abuse treatment were associated with greater odds of being in the ecstasy–polydrug subtype. Compared with the ecstasy–marijuana–stimulant subtype, a low level of family income (<$35,000), a family history of substance abuse, and a personal history of substance abuse treatment also were associated with greater odds of being in the ecstasy–polydrug subtype. Finally, compared with ecstasy–marijuana users, a personal history of substance abuse treatment was associated greater odds of being classified as ecstasy–marijuana–stimulant users.
TABLE 2.
Adjusted odds ratios (AOR) and 95% confidence intervals (CIs) of LCA-defined subtypes of lifetime ecstasy users: 2001–2002 national epidemiologic survey on alcohol and related conditions (N = 562)
| Characteristics of ecstasy users* |
C1 vs. C3 ecstasy–polydrug users vs. ecstasy–marijuana users |
C2 vs. C3 ecstasy– marijuana–stimulant users vs. ecstasy–marijuana users |
C1 vs. C2 ecstasy–polydrug users vs. ecstasy–marijuana– stimulant users |
|---|---|---|---|
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Age group | |||
| 18–29 years | 0.17 (0.04–0.78)† | 0.33 (0.08–1.48) | 0.50 (0.19–1.32) |
| 30–44 years | 0.44 (0.10–2.01) | 0.85 (0.20–3.68) | 0.52 (0.20–1.40) |
| 45 years or older | 1.00 | 1.00 | 1.00 |
| Gender | |||
| Male | 1.25 (0.70–2.23) | 0.92 (0.51–1.65) | 1.36 (0.78–2.35) |
| Female | 1.00 | 1.00 | 1.00 |
| Race/ethnicity | |||
| Black | 0.63 (0.16–2.56) | 1.29 (0.44–3.71) | 0.49 (0.12–2.06) |
| Hispanic | 1.55 (0.62–3.87) | 1.48 (0.67–3.23) | 1.05 (0.52–2.11) |
| Other | 0.71 (0.26–1.95) | 0.77 (0.27–2.21) | 0.92 (0.27–3.20) |
| White | 1.00 | 1.00 | 1.00 |
| Educational level | |||
| <High school | 0.99 (0.34–2.90) | 0.67 (0.22–2.03) | 1.49 (0.52–4.30) |
| High school | 1.00 (0.48–2.09) | 0.85 (0.42–1.73) | 1.18 (0.58–2.40) |
| ≥College | 1.00 | 1.00 | 1.00 |
| Total family income | |||
| 0–$34,999 | 2.44 (1.08–5.48)† | 1.08 (0.53–2.20) | 2.25 (1.10–4.62)† |
| $35,000–$69,999 | 1.24 (0.52–2.97) | 1.00 (0.46–2.16) | 1.24 (0.56–2.76) |
| $75,000+ | 1.00 | 1.00 | 1.00 |
| Marital status | |||
| Wid./sep./divorced | 0.87 (0.25–3.08) | 0.53 (0.18–1.59) | 1.64 (0.62–4.32) |
| Never married | 0.80 (0.38–1.67) | 0.49 (0.24–1.01) | 1.62 (0.83–3.16) |
| Married | 1.00 | 1.00 | 1.00 |
| Age of first hallucinogen use | |||
| 17 years or younger | 2.65 (1.36–5.18)† | 1.74 (0.84–3.62) | 1.52 (0.88–2.64) |
| 18 years or older | 1.00 | 1.00 | 1.00 |
| Family history of alcohol or drug abuse | |||
| Yes | 1.49 (0.71–3.13) | 0.63 (0.30–1.30) | 2.38 (1.22–4.64)† |
| No | 1.00 | 1.00 | 1.00 |
| Personal history of using substance abuse treatment services | |||
| Yes | 4.65 (2.15–10.09)† | 2.58 (1.21–5.47)† | 1.80 (1.02–3.19)† |
| No | 1.00 | 1.00 | 1.00 |
| Lifetime hallucinogen use disorder | |||
| Abuse without dependence | 1.23 (0.69–2.19) | 1.09 (0.54–2.21) | 1.13 (0.62–2.05) |
| Dependence | 1.65 (0.35–7.79) | 1.01 (0.16–6.20) | 1.64 (0.47–5.73) |
| No | 1.00 | 1.00 | 1.00 |
The multinomial logistic model included all variables listed in the first column.
p < 0.05.
SUDs by LCA-Defined Ecstasy Subtypes
Ecstasy–polydrug users (Table 3) had the highest prevalence of SUD related to the use of marijuana (77%), tobacco (66%), amphetamines (36%), opioids/analgesics (35%), sedatives (31%), and tranquilizers (30%). Compared with ecstasy–marijuana users, they manifested a higher prevalence of SUD related to the use of alcohol (89% vs. 72%), cocaine (50% vs. 0%), inhalants (11% vs. 0%), and heroin (8% vs. 0%). A comparison with non-ecstasy drug users clearly showed that ecstasy–polydrug users had significantly higher rates of all SUDs, whereas ecstasy–marijuana–stimulant users had higher rates of disorders related to the use of alcohol, marijuana, cocaine, amphetamines, and heroin. Further, ecstasy–marijuana users had a higher rate of marijuana use disorders as compared to non-ecstasy drug users. Overall, ecstasy–polydrug users had a highest mean number of SUDs (5.0 [95% CI: 6.6–5.4]), followed by ecstasy–marijuana–stimulant users (3.2 [95% CI: 2.9–3.5]), and then by ecstasy–marijuana users (2.2 [95% CI: 2.0–2.5]) and non-ecstasy drug users (2.1 [95% CI: 2.0–2.1]).
TABLE 3.
Substance use disorders among ecstasy users and non-ecstasy drug users in NESARC (N = 9140)
| Lifetime prevalence: Column % (95% CI) |
C1: ecstasy–polydrug users |
C2: ecstasy–marijuana– stimulant users |
C3: ecstasy– marijuana users |
Non-ecstasy drug users |
χ2(df =3) P value |
|---|---|---|---|---|---|
| Sample size, N | 217 | 178 | 167 | 8578 | |
| Hallucinogen abuse | 36.2 (29.2–43.9) | 30.6 (22.0–40.8) | 25.7 (18.3–34.9) | ……. | NS |
| Hallucinogen dependence | 9.6 (5.5–16.1) | 4.0 (1.4–10.4) | 4.7 (1.3–15.5) | ……. | NS |
| Hallucinogen use disorders | 45.8 (38.6–53.3) | 34.6 (24.9–45.7) | 30.4 (21.9–40.5) | ……. | NS |
| Nicotine dependence | 66.4 (58.2–73.8) | 41.6 (33.3–50.4) | 42.9 (33.7–52.6) | 37.0 (35.2–39.0) | <0.001 |
| Alcohol use disorders | 89.1 (83.7–92.9) | 78.9 (70.0–85.6) | 72.2 (62.4–80.3) | 64.6 (62.7–66.4) | <0.001 |
| Any drug use disorders* | 92.1 (87.3–95.2) | 69.7 (60.0–77.9) | 58.2 (48.7–67.2) | 43.1 (41.5–44.7) | <0.001 |
| Marijuana use disorders | 77.4 (70.4–83.2) | 57.1 (48.4–65.4) | 48.5 (38.8–58.2) | 35.3 (33.8–36.8) | <0.001 |
| Cocaine use disorders | 50.1 (41.3–58.9) | 45.4 (35.6–55.4) | 0.0 | 10.9 (10.1–11.8) | <0.001 |
| Inhalant use disorders | 10.9 (6.9–16.8) | 2.9 (1.1–7.5) | 0.0 | 1.2 (1.0–1.6) | <0.001 |
| Opioid use disorders | 35.2 (27.2–44.1) | 5.7 (2.9–11.1) | 5.9 (2.2–14.9) | 5.5 (4.7–6.4) | <0.001 |
| Amphetamine/stimulant use disorders | 36.1 (29.0–43.8) | 14.7 (9.6–21.8) | 4.0 (1.0–14.4) | 8.0 (7.1–9.1) | <0.001 |
| Tranquilizer use disorders | 30.1 (22.8–38.5) | 1.0 (0.2–4.1) | 1.1 (0.2–5.0) | 3.8 (3.3–4.3) | <0.001 |
| Sedative use disorders | 30.5 (22.6–39.8) | 1.2 (0.2–5.5) | 1.6 (0.5–5.5) | 4.2 (3.7–4.7) | <0.001 |
| Heroin use disorders | 8.1 (4.7–13.5) | 3.6 (1.4–9.1) | 0.0 | 0.7 (0.2–0.9) | <0.001 |
| Total number of substance use disorders, mean (95% CI)† | 5.0 (6.6–5.4) | 3.2 (2.9–3.5) | 2.2 (2.0–2.5) | 2.1 (2.0–2.1) | <0.001‡ |
Any disorder from the use of nine drug classes: hallucinogens, marijuana, cocaine, inhalants, heroin, opioids/pain killers, amphetamines, sedatives, and tranquilizers.
Total number of disorders from the use of 11 substance classes (nicotine, alcohol, hallucinogens, marijuana, cocaine, inhalants, heroin, opioids/pain killers, amphetamines, sedatives, and tranquilizers).
CI: confidence interval. NS: p > 0.01.
F-test.
Mental Disorders by LCA-Defined Ecstasy Subtypes
Ecstasy–polydrug users (Table 4) exhibited a higher prevalence of dysthymia (12% vs. 2%) and antisocial personality disorder (31% vs. 10%) than did ecstasy–marijuana users. Ecstasy–marijuana–stimulant users had a higher prevalence of dysthymia than did ecstasy–marijuana users (13% vs. 2%). Comparisons with non-ecstasy drug users showed that ecstasy–polydrug users had higher rates of mania, histrionic personality disorder, and antisocial personality disorder.
TABLE 4.
Non-addictive psychiatric disorders among ecstasy users and non-ecstasy drug users in NESARC (N = 9140)
| Lifetime prevalence: Column % (95% CI) |
C1: ecstasy–polydrug users |
C2: ecstasy–marijuana– stimulant users |
C3: ecstasy– marijuana users |
Non-ecstasy drug users |
χ2(df =3) P value |
|---|---|---|---|---|---|
| Sample size | 217 | 178 | 167 | 8578 | |
| Any mood problem | 45.8 (37.7–54.3) | 42.5 (34.6–50.8) | 32.0 (24.2–40.9) | 35.0 (33.5–36.5) | NS |
| Major depression | 36.2 (28.6–44.5) | 37.4 (29.8–45.6) | 25.0 (18.3–33.3) | 30.4 (29.0–31.9) | NS |
| Dysthymia | 12.2 (8.2–17.6) | 13.1 (8.4–19.8) | 2.2 (0.7–6.2) | 9.7 (8.9–10.5) | <0.001 |
| Mania | 17.3 (12.4–23.8) | 10.9 (6.5–17.7) | 7.2 (3.7–13.7) | 7.9 (7.1–8.7) | 0.01 |
| Hypomania | 5.9 (3.0–11.0) | 7.0 (3.8–12.5) | 7.4 (4.2–12.9) | 4.0 (3.5–4.5) | NS |
| Any anxiety problem | 31.1 (24.8–38.7) | 24.8 (18.2–32.7) | 26.1 (18.6–35.3) | 27.3 (25.8–28.8) | NS |
| Any panic disorder | 11.1 (7.3–16.6) | 5.8 (3.0–11.1) | 4.8 (2.2–10.1) | 7.2 (6.6–7.9) | NS |
| Panic disorder with agoraphobia | 4.1 (1.9–8.8) | 3.6 (1.5–8.4) | 1.7 (0.5–5.6) | 2.4 (2.2–2.8) | NS |
| Panic disorder w/out agoraphobia | 0.3 (0.0–2.2) | 0 | 0.5 (0.1–3.7) | 0.4 (0.2–0.6) | NS |
| Social phobia | 6.9 (4.0–11.8) | 7.4 (4.1–12.8) | 10.6 (5.5–19.4) | 8.7 (7.9–9.7) | NS |
| Specific phobia | 18.8 (13.5–25.5) | 12.8 (8.4–19.3) | 12.5 (7.9–19.4) | 14.6 (13.6–15.8) | NS |
| Generalized anxiety disorder | 7.9 (4.7–13.0) | 6.1 (3.3–10.9) | 5.1 (2.5–10.1) | 8.0 (7.3–8.8) | NS |
| Any personality disorder | 45.8 (37.7–54.2) | 40.9 (32.4–50.1) | 27.2 (19.8–36.1) | 26.3 (24.9–27.8) | <0.001 |
| Avoidant | 3.8 (1.9–7.3) | 3.7 (1.6–8.2) | 3.9 (1.8 – 8.5) | 4.5 (4.0–5.2) | NS |
| Dependent | 1.8 (0.6–5.1) | 0.4 (0.1–2.4) | 1.7 (0.5–5.6) | 0.9 (0.7–1.2) | NS |
| Obsessive–compulsive | 13.9 (9.5–19.9) | 17.1 (11.6–24.5) | 9.9 (5.7–16.7) | 12.4 (11.5–13.3) | NS |
| Paranoid | 12.6 (8.4–18.2) | 12.0 (6.4–21.4) | 7.2 (3.8–13.3) | 12.0 (6.4–21.4) | NS |
| Schizoid | 6.9 (4.0–11.7) | 4.6 (2.2–9.3) | 4.7 (2.2–9.9) | 5.5 (4.9–6.2) | NS |
| Histrionic | 10.9 (7.0–16.6) | 6.2 (3.2–11.7) | 5.8 (2.9–11.3) | 3.6 (3.1–4.1) | 0.01 |
| Antisocial | 30.6 (23.8–38.2) | 21.3 (14.6–30.0) | 9.6 (5.8–15.6) | 10.5 (9.6–11.5) | <0.001 |
CI: confidence interval. NS: p > 0.01.
DISCUSSION
This study reports new findings concerning the heterogeneity of ecstasy users in a large nationally representative sample of American adults. Approximately 1.6% of adults reported ecstasy use; of them, 31% and 6% met criteria for lifetime hallucinogen abuse and dependence, respectively. This study extends previously unaddressed questions26 by elucidating specific SUD affecting ecstasy users and by applying LCA to identify three subtypes of ecstasy users: ecstasy–polydrug users, ecstasy–marijuana–stimulant users, and ecstasy–marijuana users. Ecstasy–polydrug users exhibited the highest prevalence of disorders related to the use of tobacco, marijuana, amphetamines, opioids, sedatives, and tranquilizers; they also had a higher rate of dysthymia and antisocial personality disorder than did ecstasy–marijuana users. These findings provide impressive evidence that ecstasy users are not homogeneous in nature and that a large proportion of such users are likely to be relatively poor and affected by multiple psychiatric disorders. The high prevalence of psychiatric disorders among ecstasy users is likely, in turn, to result in significantly curtailed occupational, interpersonal, and other life opportunities.
Ecstasy–Polydrug Users
The study’s most salient findings concern the very high prevalence of lifetime SUDs among ecstasy–polydrug users (37% of all ecstasy users), who on average met criteria for five SUDs. Of this most compromised group, the majority met criteria for disorders related to use of tobacco, alcohol, and marijuana. Approximately one half had disorders related to the use of cocaine and hallucinogens; more than one third exhibited disorders related to the use of four prescription drug classes; and close to one third met criteria for an antisocial personality disorder. Polysubstance abuse by members of this group may be due to their use of multiple substances to intensify or modulate the effects of drug use, attenuate the discomfort or negative affect associated with the after-effects of ecstasy or other drug use, or to self-medicate health problems resulting from polysubstance abuse.4,8,17,20,35 Participants’ level of drug use may also increase in scope or variety due to their tolerance or cross-tolerance of different drugs,36,37 the emergence of negative affect and distress, and the dysregulation of brain reward function (eg, compulsive drug-seeking and loss of control in limiting intake).38 While the extent of their ecstasy use may also intensify, the survey does not collect data concerning the amount of ecstasy taken to allow us to further test this question. Studies, nonetheless, have suggested a dose–response relationship between the quantity of lifetime ecstasy use and current psychiatric and cognitive difficulties.39,40
This group’s significant associations with antisocial personality disorder, family history of substance abuse, and high lifetime prevalence rates of using multiple substances suggest that early behavioral problems or family factors (eg, dysfunctional family, poor parenting, school difficulties, and affiliating with drug-using peers), co-occurrences of substance use, and the neurotoxic effects of polysubstance use on the brain may interact to elevate these users’ risk of multiple SUDs.41–45 While this cross-sectional study cannot determine causality, common risk factors may explain their high rates of substance use and disorders.41–43 Members of this group also were likely to live in a low-income family, which could be related to their disadvantaged family backgrounds or to their usage of multiple substances that result in schooling, occupational, and financial problems.45,46
Ecstasy–Marijuana–Stimulant Users
This group (29% of all ecstasy users) reported high rates of lifetime use of marijuana and cocaine and moderate use of amphetamines. The majority of them also met criteria for disorders related to the use of tobacco, alcohol, and marijuana; close to one half exhibited a cocaine use disorder; and about one third reported a hallucinogen use disorder. Because their rates of SUDs were lower than those of ecstasy–polydrug users, this group can be viewed as comprising moderately problematic drug users who on average met criteria for 3.2 SUDs. Their profile is also consistent with their lower odds of low-income and history of substance abuse treatment and familial substance abuse as compared to ecstasy–polydrug users. However, this group still manifested much higher rates of alcohol, marijuana, cocaine, and amphetamine use disorders than did non-ecstasy drug users, suggesting that their drug use might be more advanced than non-ecstasy drug users in general.
Ecstasy–Marijuana Users
This third group (34% of all ecstasy users) exhibited a high lifetime use of marijuana and some use of prescription-type drugs (ie, opioids). The majority met criteria for nicotine and alcohol use disorders, and close to one half exhibited a marijuana use disorder. Compared with the first two ecstasy groups, this group on average had fewer SUDs, was less likely to have a personal history of substance abuse treatment, and had a lower prevalence of dysthymia. Members of this group resembled non-ecstasy drug users in having an average of two SUDs. They, however, had never used cocaine or heroin, had a lower prevalence of dysthymia, but exhibited a higher rate of marijuana use disorders (49% vs. 35%) than non-ecstasy drug users. In comparison, 11% of non-ecstasy drug users had a cocaine use disorder and 1% had a heroin use disorder. The results suggest that cocaine-using ecstasy users are more advanced in their substance abuse than non-cocaine-using ecstasy users. A next step would be to compare the role of cocaine and ecstasy use, alone or in combination, in the risk for SUDs.
Implications
The presence of different subgroups of lifetime ecstasy users has important implications for prevention efforts. The variations in their patterns of substance use behaviors suggest that the three groups may be located on a continuum of drug use, ranging from less extensive users of mainly marijuana and ecstasy to the middle group, which uses stimulants in addition, and then to the high group, which uses multiple drugs. The generally high rate of substance use among ecstasy users suggests that prevention programs that primarily seek to reduce ecstasy use may be ineffective if they do not also address other substance use (eg, marijuana and cocaine use). Additionally, substance abuse is associated with a long list of medical illnesses involving multiple organs and cognitive impairment, and medical problems are likely to persist even after the abuse itself is terminated.47 The comparatively high rates of multiple SUDs in the first two groups of ecstasy users indicate that, in a clinical setting, ecstasy use may serve as a useful indicator to identify high-risk patients for substance abuse screening and, as appropriate, referral for treatment. It would be of clinical relevance to test whether adding ecstasy use to a routine assessment of substance use in clinical settings would be more helpful in detecting patients in need of medical interventions than a routine assessment of alcohol or cigarette use alone. This practice may be of particular value to the majority of ecstasy users with multiple comorbid disorders who are at risk for adverse effects of drug abuse.4,5,7
In addition, the finding that pure ecstasy users are rare has several implications for research. We found that marijuana was the drug most commonly used by ecstasy users (98%), followed by stimulants (cocaine and amphetamines). Prior research has found that probably 90–98% of ecstasy users also take marijuana.48 It is worth noting that both drugs can contribute independently to cognitive deficits and other adverse health effects, and the overall effects of drug combinations are complex depending on their cumulative usage and whether they are being taken separately and together.7,48 Similarly, stimulants are neurotoxic to neurons, and they may act synergistically with ecstasy to enhance their long-term adverse effects.5 These findings thus support past assumptions that observed neurotoxic effects among ecstasy users are confounded by other substance abuse, particularly marijuana and stimulants.5,7,49
Another area of research that deserves more studies concerns the impact of comorbid alcohol use disorder and nicotine dependence on medical consequences for ecstasy/MDMA users.7 Like marijuana use disorders, they are prevalent in this national sample of ecstasy users, and both have harmful effects on health.47 Co-usage of nicotine and MDMA may have an addictive effect on memory deficits.7 Further, recent studies on rats have begun to suggest that alcohol use may enhance MDMA-related neurotoxicity and liability for abuse because it could increase brain and blood concentrations of MDMA.50,51 Together, these findings demonstrate an inherent methodological challenge in conducting research on neurotoxicitys of ecstasy use.5,7,48,49 Ideally, a longitudinal study of a large cohort of young people who are never users of drugs at baseline would be needed in order to better evaluate the long-term effects of subsequent ecstasy and/or other drug use on psychological functions and cognitive performance.5 Finally, studies have suggested that ecstasy use is particularly prevalent among gay/bisexual men.52,53 Our next step is to examine whether subtype of ecstasy use is associated with sexual orientation and to pinpoint subgroups of gay/bisexual men at risk for exhibiting a severe pattern of psychiatric disorders.
Study Limitations and Strengths
These findings should be interpreted with the following limitations in mind. The cross-sectional design of the NESARC survey precludes making inferences of causal relationships from our findings. In addition, the survey relies on participants’ self-reports, which may be influenced by biases related to both under-reporting and memory errors. A very small proportion of the institutionalized population (eg, homeless, hospitalized, or incarcerated individuals) was not included in the survey. Individuals who suffered severe consequences from their substance abuse may be less likely to have been sampled by the household survey, or may otherwise have been unable to participate. The results also are limited by the fact that the quantity of specific drug used is not assessed by NESARC. Previous research indicates that extensive polydrug use is associated with greater usage of ecstasy/MDMA.54 This limitation also indicates that the data from epidemiologic surveys of drug use and disorders can be improved further by adding questions regarding the quantity of drugs used.
The NESARC data also have noteworthy strengths. Because the very large sample represents the domiciled U.S. adult population, it has a high degree of generalizability. Perhaps the most important characteristic of the data source is its inclusion of the most comprehensive assessments of psychiatric disorders available, which supports the comparison of specific psychiatric disorders among subtypes of ecstasy and other drug users.
CONCLUSIONS
This first national investigation of the variety of ecstasy users adds new evidence to the field by identifying at least three subtypes of ecstasy users, who are differentiated by patterns of psychiatric disorders, family income, and history of familial substance abuse. The results suggest that the two groups of ecstasy users (66%) who also used cocaine may abuse more substances than ecstasy users who had never used cocaine and non-ecstasy drug users. Ecstasy–polydrug users are more likely than other groups to live in a low-income family and to manifest antisocial behaviors. The recent resurgence in ecstasy use and high rates of SUDs among ecstasy users underscores the need to monitor trends in ecstasy use and to investigate further how focused prevention and early case finding and intervention efforts may help reduce substance abuse among ecstasy users.14,55
Acknowledgments
NESARC was sponsored and conducted by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health, with supplemental support from the National Institute on Drug Abuse. This work was supported by grant awards R01DA019623 and R01DA019901 from the National Institute on Drug Abuse of the National Institutes of Health, Bethesda, Md (Dr. Wu).
We thank Ms. Amanda McMillan for her editorial assistance.
Footnotes
The opinions expressed in this paper are solely those of the authors, and not of any sponsoring agency.
Declaration of interest
The authors report no conflict of interest.
REFERENCES
- 1.Parrott AC. Drug-related harm: a complex and difficult concept to scale. Hum Psychopharmacol. 2007;22:423–425. doi: 10.1002/hup.874. [DOI] [PubMed] [Google Scholar]
- 2.Montoya AG, Sorrentino R, Lukas SE, Price BH. Long-term neuropsychiatric consequences of ‘ecstasy’ (MDMA), a review. Harv Rev Psychiatry. 2002;10:212–220. [PubMed] [Google Scholar]
- 3.Cowan RL. Neuroimaging research in human MDMA users: a review. Psychopharmacology. 2007;189:539–556. doi: 10.1007/s00213-006-0467-3. [DOI] [PubMed] [Google Scholar]
- 4.Reneman L, de Win MM, van den Brink W, Booij J, den Heeten GJ. Neuroimaging findings with MDMA/ecstasy: technical aspects, conceptual issues and future prospects. J Psychopharmacol. 2006;20:164–175. doi: 10.1177/0269881106061515. [DOI] [PubMed] [Google Scholar]
- 5.Gouzoulis-Mayfrank E, Daumann J. The confounding problem of polydrug use in recreational ecstasy/MDMA users: a brief overview. J Psychopharmacol. 2006;20:188–193. doi: 10.1177/0269881106059939. [DOI] [PubMed] [Google Scholar]
- 6.Medina KL, Shear PK. Anxiety, depression, and behavioral symptoms of executive dysfunction in ecstasy users: contributions of polydrug use. Drug Alcohol Depend. 2007;87:303–311. doi: 10.1016/j.drugalcdep.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parrott AC. MDMA in humans: factors which affect the neuropsychobiological profiles of recreational ecstasy users, the integrative role of bioenergetic stress. J Psychopharmacol. 2006;20:147–163. doi: 10.1177/0269881106063268. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., Text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 9.Koesters SC, Rogers PD, Rajasingham CR. MDMA (“ecstasy”) and other “club drugs.” The new epidemic. Pediatr Clin North Am. 2002;49:415–433. doi: 10.1016/s0031-3955(01)00012-8. [DOI] [PubMed] [Google Scholar]
- 10.Maxwell JC. Party drugs: properties, prevalence, patterns, and problems. Subst Use Misuse. 2005;40:1203–1240. doi: 10.1081/JA-200066736. [DOI] [PubMed] [Google Scholar]
- 11.Patel MM, Wright DW, Ratcliff JJ, Miller MA. Shedding new light on the “safe” club drug: methylenedioxymethamphetamine (ecstasy)-related fatalities. Acad Emerg Med. 2004;11:208–210. [PubMed] [Google Scholar]
- 12.Substance Abuse and Mental Health Services Administration. Club drugs, 2001 update. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2002. [Google Scholar]
- 13.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Ann Arbor, MI: University of Michigan News Service; 2007. [Accessed March 30, 2008]. Overall, illicit drug use by American teens continues gradual decline in 2007. [online]; Available at: www.monitoringthefuture.org. [Google Scholar]
- 14.Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2008. [Google Scholar]
- 15.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Ann Arbor, MI: University of Michigan News Service; 2008. [Accessed on March 23, 2009]. Various stimulant drugs show continuing gradual declines among teens in 2008, most illicit drugs hold steady. http://www.monitoringthefuture.org/pressreleases/08drugpr.pdf. [Google Scholar]
- 16.Carlson RG, Wang J, Falck RS, Siegal HA. Drug use practices among MDMA/ecstasy users in Ohio: a latent class analysis. Drug Alcohol Depend. 2005;79:167–179. doi: 10.1016/j.drugalcdep.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Parrott AC. Human psychopharmacology of ecstasy (MDMA),a review of 15 years of empirical research. Human Psychopharmacol. 2001;16:557–577. doi: 10.1002/hup.351. [DOI] [PubMed] [Google Scholar]
- 18.Strote J, Lee JE, Wechsler H. Increasing MDMA use among college students: results of a national survey. J Adolesc Health. 2002;30:64–72. doi: 10.1016/s1054-139x(01)00315-9. [DOI] [PubMed] [Google Scholar]
- 19.Wu LT, Schlenger WE, Galvin DM. Concurrent use of methamphetamine, MDMA, LSD, ketamine, GHB, and flunitrazepam among American youths. Drug Alcohol Depend. 2006;84:102–113. doi: 10.1016/j.drugalcdep.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Winstock AR, Griffiths P, Stewart D. Drugs and the dance music scene: a survey of current drug use patterns among a sample of dance music enthusiasts in the UK. Drug Alcohol Depend. 2001;64:9–17. doi: 10.1016/s0376-8716(00)00215-5. [DOI] [PubMed] [Google Scholar]
- 21.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24:882–889. [PubMed] [Google Scholar]
- 22.Wu LT, Blazer DG, Patkar AA, Stitzer ML, Wakim PG, Brooner RK. Heterogeneity of stimulant dependence: a National Drug Abuse Treatment Clinical Trials Network (CTN) study. Am J Addict. 2009;18:206–218. doi: 10.1080/10550490902787031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, and disability of personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2004;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- 24.Grant BF. The impact of a family history of alcoholism on the relationship between age at onset of alcohol use and DSM-IV alcohol dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. Alcohol Health Res World. 1998;22:144–147. [PMC free article] [PubMed] [Google Scholar]
- 25.Hser YI, Anglin MD, Grella C, Longshore D, Prendergast ML. Drug treatment careers: a conceptual framework and existing research findings. J Subst Abuse Treat. 1997;14:543–558. doi: 10.1016/s0740-5472(97)00016-0. [DOI] [PubMed] [Google Scholar]
- 26.Keyes KM, Martins SS, Hasin DS. Past 12-month and lifetime comorbidity and polydrug use of ecstasy users among young adults in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2008;97:139–149. doi: 10.1016/j.drugalcdep.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu LT, Ringwalt CL, Mannelli P, Patkar AA. Hallucinogen use disorders among adult users of MDMA and other hallucinogens. Am J Addict. 2008;17:354–363. doi: 10.1080/10550490802269064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorders and Associated Disabilities Interview Schedule–IV (AUDADIS IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 29.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatr. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 30.Wu LT, Howard MO, Pilowsky DJ. Substance use disorders among inhalant users: results from the National Epidemiologic Survey on alcohol and related conditions. Addict Behav. 2008;33:968–973. doi: 10.1016/j.addbeh.2008.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Research Triangle Institute. SUDAAN user’s manual, release 9.0. Research Triangle Park, NC: Research Triangle Institute; 2006. [Google Scholar]
- 32.Muthén BO, Muthén LK. Mplus: Statistical analysis with latent variables (version 4.2.1) Los Angeles, CA: Muthén and Muthén, Inc; 2007. [Google Scholar]
- 33.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classif. 1996;13:195–212. [Google Scholar]
- 34.Nylund KL, Asparouhov T, Muthén B. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Struct Equ Model. 2007;14:535–569. [Google Scholar]
- 35.Boys A, Marsden J, Strang J. Understanding reasons for drug use amongst young people: a functional perspective. Health Educ Res. 2001;16:457–469. doi: 10.1093/her/16.4.457. [DOI] [PubMed] [Google Scholar]
- 36.Parrott AC. Chronic tolerance to recreational MDMA 3,4– methylenedioxymethamphetamine) or ecstasy. J Psychopharmacol. 2005;19:71–83. doi: 10.1177/0269881105048900. [DOI] [PubMed] [Google Scholar]
- 37.Parrott AC, Morinan A, Moss M, Scholey A. Understanding drugs and behaviour. Chichester: Wiley; 2004. [Google Scholar]
- 38.Koob GF, Le Moal M. The neurobiology of addiction. Elsevier, MA: Academic Press; 2006. [Google Scholar]
- 39.Soar K, Turner JJ, Parrott AC. Psychiatric disorders in ecstasy (MDMA) users: a literature review focusing on personal predisposition and drug history. Hum Psychopharmacol. 2001;16:641–645. doi: 10.1002/hup.350. [DOI] [PubMed] [Google Scholar]
- 40.Thomasius R, Petersen KU, Zapletalova P, Wartberg L, Zeichner D, Schmoldt A. Mental disorders in current and former heavy ecstasy (MDMA) users. Addiction. 2005;100:1310–1319. doi: 10.1111/j.1360-0443.2005.01180.x. [DOI] [PubMed] [Google Scholar]
- 41.Jessor R. New perspectives on adolescent risk behavior. In: Jessor R, editor. New perspectives on adolescent risk behavior. Cambridge, United Kingdom: Cambridge University Press; 1998. pp. 1–10. [Google Scholar]
- 42.McGue M, Iacono WG. The association of early adolescent problem behavior with adult psychopathology. Am J Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- 43.Newcomb MD, Felix-Ortiz M. Multiple protective and risk factors for drug use and abuse: cross-sectional and prospective findings. J Pers Soc Psychol. 1992;63:280–296. doi: 10.1037//0022-3514.63.2.280. [DOI] [PubMed] [Google Scholar]
- 44.Rogers RD, Robbins TW. Investigating the neurocognitive deficits associated with chronic drug misuse. Curr Opin Neurobiol. 2001;11:250–257. doi: 10.1016/s0959-4388(00)00204-x. [DOI] [PubMed] [Google Scholar]
- 45.Wilens TE, Biederman J, Bredin E, et al. A family study of the high-risk children of opioid- and alcohol-dependent parents. Am J Addict. 2002;11:41–51. doi: 10.1080/10550490252801620. [DOI] [PubMed] [Google Scholar]
- 46.Topp L, Hando J, Dillon P, Roche A, Solowij N. Ecstasy use in Australia: patterns of use and associated harm. Drug Alcohol Depend. 1999;55:105–115. doi: 10.1016/s0376-8716(99)00002-2. [DOI] [PubMed] [Google Scholar]
- 47.Brick J. Handbook of the medical consequences of alcohol and drug abuse. New York: The Haworth Press; 2004. [Google Scholar]
- 48.Parrott AC, Milani RM, Gouzoulis-Mayfrank E, Daumann J. Cannabis and Ecstasy/MDMA (3,4-methylenedioxymethamphetamine): an analysis of their neuropsychobiological interactions in recreational users. J Neural Transm. 2007;114:959–968. doi: 10.1007/s00702-007-0715-7. [DOI] [PubMed] [Google Scholar]
- 49.Thomasius R, Zapletalova P, Petersen K, et al. Mood, cognition and serotonin transporter availability in current and former ecstasy (MDMA) users: the longitudinal perspective. J Psychopharmacol. 2006;20:211–225. doi: 10.1177/0269881106059486. [DOI] [PubMed] [Google Scholar]
- 50.Hamida SB, Tracqui A, de Vasconcelos AP, et al. Ethanol increases the distribution of MDMA to the rat brain: possible implications in the ethanol-induced potentiation of the psychostimulant effects of MDMA. Int J Neuropsychopharmacol. 2008:1–11. doi: 10.1017/S1461145708009693. [DOI] [PubMed] [Google Scholar]
- 51.Izco M, Orio L, O’Shea E, Colado MI. Binge ethanol administration enhances the MDMA-induced long-term 5-HT neurotoxicity in rat brain. Psychopharmacology (Berl) 2007;189:459–470. doi: 10.1007/s00213-006-0602-1. [DOI] [PubMed] [Google Scholar]
- 52.Klitzman RL, Pope HG, Jr, Hudson JI. MDMA (“ecstasy”) abuse and high-risk sexual behaviors among 169 gay and bisexual men. Am J Psychiatry. 2000;157:1162–1164. doi: 10.1176/appi.ajp.157.7.1162. [DOI] [PubMed] [Google Scholar]
- 53.Klitzman RL, Greenberg JD, Pollack LM, Dolezal C. MDMA (“ecstasy”) use, and its association with high risk behaviors, mental health, and other factors among gay/bisexualmen in NewYork City. Drug Alcohol Depend. 2002;66:115–125. doi: 10.1016/s0376-8716(01)00189-2. [DOI] [PubMed] [Google Scholar]
- 54.Parrott AC, Milani RM, Parmar R, Turner JJD. Recreational ecstasy/MDMA and other drug users from the UK and Italy: psychiatric symptoms and psychobiological problems. Psychopharmacology. 2001;159:77–82. doi: 10.1007/s002130100897. [DOI] [PubMed] [Google Scholar]
- 55.Wu LT, Parrott AC, Ringwalt CL, Patkar AA, Mannelli P, Blazer DG. The high prevalence of substance use disorders among recent MDMA users compared with other drug users: Implications for intervention. Addict Behav. 2009;34:654–661. doi: 10.1016/j.addbeh.2009.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]