Abstract
In a sample of 273 adult women and their families, we examined the effects of women’s psychopathology history, their social support, their husbands’ and children’s symptomatology, family stress, and neighborhood environment on their alcohol problems, antisocial behavior, and depression over a 12-year period during their ‘30s and early ‘40s. Women’s alcohol problems and antisocial behavior decreased but their depression symptoms increased over time. Women’s disorder history and their partners’ parallel symptomatology were associated with their symptoms. For women’s antisocial behavior, their own history of alcoholism and their partners’ alcohol problems were also significant risk factors. Higher levels of social support were associated with lower levels of depression in women. Children’s externalizing behavior was positively correlated with their mothers’ alcohol problems and antisocial behavior, whereas children’s internalizing behavior was positively correlated with their mothers’ depression. Neighborhood residential instability was associated with higher levels of alcoholic and depressive symptomatology in women. Intervention efforts might target women with young children by improving social support, educational or professional training opportunity, access to family counseling, and neighborhood environment.
Keywords: women, neighborhood, alcoholism, antisociality, depression
Introduction
Although developmental theorists frequently pay tribute to the fact that individual behavior always emerges and is maintained in a social environment, the opportunity to evaluate the contributions of multilevel influences from the individual, family, and neighborhood on longitudinal outcomes is rare. Longitudinal studies of individual patterns of development and psychopathology are expensive in their own right, and measurement of interpersonal effects, even without considering possible effects of the more distal environment, is daunting. The added analytic complexity, expense, and logistic problems of sustaining contact with more than one person at a time have generally constrained the literature to use personal report of interpersonal experience as a proxy for interpersonal effects, even with all the biases such a procedure brings (e.g. Merline, Schulenberg, O’Malley, Bachman, & Johnston, 2008; Sher, Gershuny, Peterson, & Raskin, 1997). Family studies (e.g. Leonard & Mudar, 2004) offer a special advantage here because of the greater likelihood that they will move together as a unit, although this is far from universal and when the unit disintegrates one is tracking not one, but two or more individuals who will thereafter enter into new social environments and relationships. The present study, based on an ongoing multi-wave prospective study on families at high risk for substance use disorder spanning more than twenty years (Fitzgerald & Zucker, 2006; Zucker et al., 2000), is one of a handful currently active studies that have been able to sustain such a multilevel longitudinal measurement structure. Thus the database offers the opportunity to evaluate these relationships with initially married women at three levels of analysis: the individual, the proximal interpersonal (involving effects of both partners and their children), and the more distal social environment of the neighborhood.
A Developmental Cumulation Model of Risk
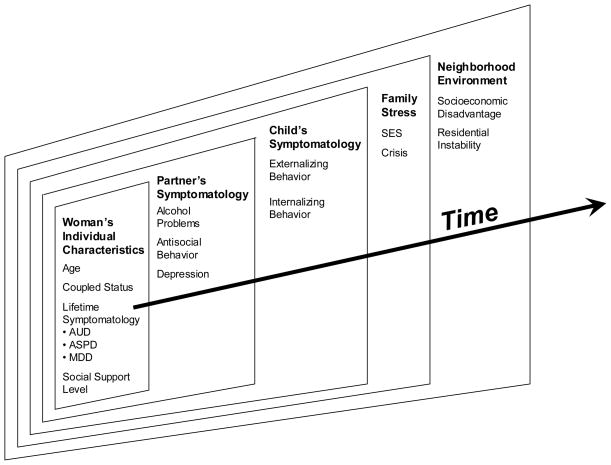
Within the context of a developmental cumulation model of risk (Zucker, 1994, 2006), the present study examines the individual and social-contextual factors which contribute to stability and change in symptomatology in three major domains of adult life: alcohol problems, antisociality, and depression. The model we utilize is a proximal to distal one, namely that “closer” influences, which have the potential for more immediate impact, should be evaluated before examining the possible effects of more distant ones, whose effect is likely to be indirect and of smaller magnitude at any one point in time. Figure 1 illustrates this theoretical framework. We hypothesize an autostability effect, that is, continuity of symptomatology over time. As a second level effect, partner influences are seen as potential shapers of ongoing behavior, and we specifically focus on isomorphism of husband’s symptomatology as a shaper and model for enhancement of wife’s symptomatology. Child influences (in parallel to partner influences), are conceived as more distal than partner effects, but still potentially play a role in the maintenance of symptoms. Nonsymptom-specific effects of family stress, brought on by poverty and crises, are frequently cited as macro-level influences on either the development or maintenance of psychiatric disorder. Here we evaluate these, using the proxy measures of current family socioeconomic status and family crises. Finally, the more distal influences of neighborhood socioeconomic disadvantage and residential instability are also thought to play an important role. We evaluate these effects via geocoding of residential characteristics of the neighborhoods where participants lived.
Figure 1.
A developmental cumulation model of risk.
Longitudinal Trajectories of Women’s Symptomatology
A cross-sectional survey of the U.S. population has showed that binge drinking, alcohol abuse, and alcohol dependence are higher in women younger than the age of 30 (Caetano, Ramisetty-Mikler, Floyd, & McGrath, 2006). Moreover, Karlamangla, Zhou, Reuben, Greendale, and Moore (2006) in analyzing the 22-year longitudinal data from the National Health and Nutrition Examination Survey (NHANES) found that heavy alcohol consumption declines with increasing age; such decline rate is also faster among women. A recent study analyzing data from six National Alcohol Surveys (NAS) over a 26-year period also found a steep age-related decline in binge drinking days among women over age 40 (Kerr, Greenfield, Bond, Ye, & Rehm, 2009). Although the NHANES did not find any cohort effect, the NAS found increased alcohol consumption and binge drinking days among recent cohorts.
The data on change over time in women’s antisocial behavior are considerably more limited, and also less clear about patterning. A recent review (Fontaine, Carbonneau, Vitaro, Barker, & Tremblay, 2009) noted that the majority of the literature on the developmental trajectories of antisocial behavior is based on male samples because overt and aggressive antisocial behavior is less common, less serious, and less persistent in females. Summarizing limited findings on females, the review indicated that the majority of antisocial female cases onset in adolescence, whereas very few females follow an early-onset/life-course-persistent trajectory. The same review also cautioned that most of the existing studies on females collected data in restrictive developmental periods at the end of childhood or during adolescence, so our knowledge of the development of adult women’s antisocial behavior is limited.
Women’s depression has been studied much more than their drinking problems or antisocial behavior. Not surprisingly, the majority of the literature on women’s changes in depression with age is based on cross-sectional studies which show a U-shaped trajectory, declining in early adulthood, bottoming out in middle age, and then rising again in old age (Mirowsky & Kim, 2007). However, conclusions about stability or change over time drawn from cross-sectional data are limited because of cohort effects, differential mortality, selection bias, and recall errors (Glynn, Bouchard, LoCastro, & Laird, 1985; Kasen, Cohen, Chen, & Castille, 2003). For example, Kasen et al. (2003) assessed two age-matched birth cohorts of mothers prospectively for 10 years and found declines in depression with age in more recent cohorts but increases in earlier cohorts. Moreover, a longitudinal study on women’s depression during the transition from late adolescence to early adulthood found substantial continuity of the symptomatology (Rao, Hammen, & Daley, 1999).
Spousal Influences on Women’s Symptomatology
The fact that alcoholics tend to couple with alcoholics is found in both community and nationally representative samples (Schuckit, Smith, Eng, & Kunovac, 2002; Windle, 1997). Two competing explanations for this spousal similarity are assortative mating and contagion. The theory behind assortative mating is that people tend to select or attract partners with similar phenotypes. The contagion model emphasizes the convergence of phenotypes as a result of reciprocal influences during the relationship. Both processes have been verified by longitudinal studies on marital dyads (Leonard & Mudar, 2004; Merline, et al., 2008).
Spousal similarity exists not only within but also across comorbid psychiatric disorders (Maes et al., 1998; McLeod, 1995). Due to the different social norms and prevalence of psychiatric disorders for men and women, the alcoholic status of a person can have different impact on mate selection depending on the individual’s gender (Nomura, Warner, & Wickramaratne, 2001; Vanyukov, Neale, Moss, & Tarter, 1996). For example, an alcoholic man has a higher tendency to mate with a depressed or anxious woman, but not necessarily with an alcoholic woman, whereas an alcoholic woman is more likely to couple with an alcoholic man. This pattern of a woman’s and her partner’s psychopathology affects the quality of the couple’s everyday interactions which may in turn impact the woman’s symptomatology. An earlier report by our group (Floyd, Cranford, Daugherty, Fitzgerald, & Zucker, 2006) showed that couples with an antisocial alcoholic husband had higher levels of hostile behavior regardless of wives’ alcoholism status. However, the rate of positive behavior was greatest among couples in which either both or neither of the spouses have an alcoholic diagnosis, and was lowest among alcoholic husbands with nonalcoholic wives.
A longitudinal study on couples in intimate relationships found that antisocial adolescent males and females were equally likely to pair with an antisocial partner in young adulthood (Moffitt, Caspi, Rutter, & Silva, 2001). The same study also showed that the continuity of female antisocial behavior from adolescence to adulthood was determined by partners’ antisocial behavior whereas antisocial men demonstrated continuity regardless of the behavior of their partners. Another longitudinal study on married couples demonstrated spousal similarity in both depressive symptoms and coping across 10 years (Holahan, Moos, Moerkbak, Cronkite, Holahan, & Kenney, 2007). They also observed that coping similarity strengthened depressive similarity within couples.
Children’s Influences on Women’s Symptomatology
Maternal alcohol-related problems (Christensen & Bilenberg, 2000; Dawson, Harford, & Grant, 1992), maternal depression (Goodman & Gotlib, 1999), and paternal antisocial alcoholism (Jansen, Fitzgerald, Ham, & Zucker, 1995; Zucker, Ellis, Fitzgerald, & Bingham, 1996) predict offspring behavioral and emotional problems. Moreover, assortative mating for psychiatric disorders may increase the risk for transmission of psychopathology to offspring through both direct and indirect genetic effects as well as environmental influences (Clark, Cornelius, Wood, & Vanyukov, 2004; Dierker, Merikangas, & Szatmari, 1999; Merikangas, Weissman, Prusoff, & John, 1988; Nomura et al., 2001; Vanyukov et al., 1996).
Women living with children who have behavior problems may experience more family conflict and stress, which in turn may increase the level of their own symptomatology. Although the association between maternal psychopathology and child behavior problems is reciprocal, very few studies have examined how specific characteristics and behaviors of children may contribute to and exacerbate their mother’s symptoms. A longitudinal study of problem drinkers found that better children’s general health and child-parent relationships predicted mothers’ reduced drinking and lower levels of depression at later waves (Timko, Kaplowitz, & Moos, 2000). An earlier report by our group has also shown such child-to-mother influence in the area of aggressive behavior: child aggression in early childhood predicted parent-to-child aggression in middle childhood (Fuller, Chermack, Cruise, Kirsch, Fitzgerald, & Zucker, 2003). Another longitudinal study using a sample of male toddlers from predominantly low-income families showed that early child noncompliance (at 18 month old) predicted more chronic and elevated trajectories of maternal depression over the course of 8 years (Gross, Shaw, Burwell, & Nagin, 2009). In a laboratory setting, Pelham et al. (1997) has found higher levels of adult distress, hostility, and alcohol consumption as a result of interactions with child actors trained to enact deviant behavior.
Influences of Family Poverty, Stress, and Social Support on Women’s Symptomatology
Poverty is one of the most consistent predictors of depression in women (Belle & Doucet, 2003). The social causation theory posits that people with low socioeconomic status (SES) are at greater risk for mental health problems as a result of living with adversity, including frequent stressful life events and limited social and economic resources (Dohrenwend et al., 1992). This theory has been supported by the findings of a longitudinal study on depressive symptoms in rural low-income women (Simmons, Braun, Charnigo, Havens, & Wright, 2008). Furthermore, a 9-year-long study on a nationally representative sample of children has established an association between low SES and a wide range of psychopathology including anxious/depressed, somatic complaints, thought problems, delinquent, and aggressive syndromes (Wadsworth & Achenbach, 2005). The same study also showed that low SES appeared to limit access to mental health care for individuals with relatively high levels of symptomatology.
Stressful life events precede the majority of depressive episodes (Brown & Harris, 1989). Women are especially vulnerable to the effects of family stressors or negative interpersonal life events because they have a higher tendency to relate their happiness and self-worth to interpersonal relationships (Hammen, 2003). A longitudinal study found that stressful life events and low family support were significant predictors of alcohol problems, delinquent activities, and depressive symptoms for adolescent girls but not for adolescent boys (Windle, 1992). Longitudinal studies on disadvantaged women also found that the effect of life stressors on problem drinking is largely mediated by depression and anxiety (Hill & Angel, 2005; Mulia, Schmidt, Bond, Jacobs, & Korcha, 2008).
In contrast, higher levels of social support are associated with recovery from alcohol problems (Bond, Kaskutas, & Weisner, 2003; Kaskutas, Bond, & Humphreys, 2002) and less depressive symptomatology in women (Israel, Farquhar, Schulz, James, & Parker, 2002; Wade & Kendler, 2000). Higher levels of social support have been hypothesized to “buffer” the impact of life stressors on alcohol consumption and depressive symptomatology in women, but there is little evidence to suggest the presence of such a buffering effect (Mulia et al., 2008; Wade & Kendler, 2000).
Neighborhood Influences on Women’s Symptomatology
Neighborhood influences upon social and individual behavior are the most proximal of macro-level effects. They include broader socio-environmental characteristics that provide the social climate within which interpersonal relationships and individual functioning are embedded. Two very different data sources –census and self-report questionnaire data –have been used in the literature to characterize women’s neighborhood environments which can impact their mental health outcomes. Variables derived from census data mainly index neighborhood socioeconomic disadvantage, such as unemployment rate and residents’ education and income levels. A disadvantaged neighborhood tends to provide low-quality schools and housing and has fewer services or employment opportunities for its residents. Thus, such a neighborhood can have a negative impact on women’s quality of life. But, the effect of neighborhood socioeconomic disadvantage appears to weaken when individual-level factors are controlled. This was found in studies of women’s depression/anxiety (Cutrona, Russell, Hessling, Brown, & Murry, 2000; Henderson et al., 2005). However, these findings were based on cross-sectional data which are not sufficient for making an inference about neighborhood effects because they do not account for exposure time nor individual differences in choice of residence place (Buu et al., 2007).
Questionnaire studies are primarily designed to measure perceived neighborhood disorder such as violence, crime, substance use/sale, unsupervised youth, abandoned houses, and low level of police responsiveness. According to Mirowsky and Ross (2003), the short-term effect of neighborhood disorder is to arouse residents’ fear and anxiety; in the long term, such negative feelings may lead to depression. Negative influences of neighborhood disorder on women’s depression/anxiety have been found in both cross-sectional (Clark et al., 2008; Cutrona et al., 2000; Hill, Mossakowski, & Angel, 2007; Schulz et al., 2006) and longitudinal data (Cutrona et al., 2005; Kling, Liebman, & Katz, 2007). Neighborhood disorder is also associated with women’s heavy drinking (Hill & Angel, 2005). However, a design flaw as pointed out by Clark et al. (2008) with self-reported neighborhood disorder is that women who are more anxious or depressed may be more inclined to rate their neighborhood environment negatively, or to recall witnessing violence/crime at a greater rate. One recent study raised questions about making inference solely based on subjective ratings of neighborhood disorder. Bogat et al. (2005) used police reports of aggravated assault and disorderly conduct offenses geocoded and aggregated at the block group level to indicate neighborhood disorder, and found no linkage between neighborhood disorder and women’s mental health functioning.
Method
Design and Sample
The present study is part of the Michigan Longitudinal Study (MLS), an ongoing multi-wave prospective study on families at high risk for substance use disorder spanning more than twenty years (Zucker, 1987; Zucker et al., 2000). Participants were families ascertained through two interconnected population-based methods carried out in a 4-county-wide area in the Midwest. Ascertainment of the highest risk portion of the sample was by way of the father’s drunk driving conviction with a sufficiently high blood alcohol concentration (0.15%) to virtually assure a later alcoholism diagnosis would be obtained. The remaining families were systematically recruited door-to-door in the same neighborhoods as the drunk-driver’s families, thus providing a crude socio-economic match as well as controlling for neighborhood ecological influences. For the current study, 46% of the families were recruited through drunk driving records; 21% of the families were recruited through neighborhood canvassing and had a father (or both father and mother) who met the probable or definite Feighner diagnosis criteria of alcoholism (Feighner et al., 1972); the remainder of the community ascertained group (33%) consisted of families where neither the mother nor father made a lifetime substance use disorder diagnosis. The three family types represent a gradient of alcohol abuse/dependence and other substance use disorder vulnerability, and a substantial amount of other psychiatric comorbidity is present as well. The recruitment protocol also required that the father was living with a 3-5 year old son and the boy’s biological mother. The study families were originally recruited as triads but thereafter siblings within +/− eight years of the initial male target child were also recruited.
Children and parents were assessed extensively following the initial recruitment (Wave 1, child age 3–5) with primarily in-home assessment using questionnaires, semi-structured clinical interviews, and behavior observations every three years. The present study reports on the first five MLS assessment waves (child age 15-17 at Wave 5) over an interval of 12 years. The unstable nature of some of these relationships is illustrated by the fact that some couples were no longer living together by the end of the baseline assessment protocol (also see Table 1). Follow-up assessments included all the couples regardless of their partnership status. For those participants who re-coupled at later waves, their new partners who cohabited with the participants for at least nine months were also included in the assessment. A more detailed description of the study methodology is provided in an earlier report (Zucker et al., 2000). In the present report, we included the 273 women (all Caucasian) who participated in at least one follow-up assessment in addition to the baseline assessment. Ninety-four census tracts were represented. The average number of participants per census tract was 2.90. T tests showed that these 273 women were comparable with the 45 women who did not participate in any follow-up assessment, in terms of age, SES, education, and relevant neighborhood risk indicators (p>.05). A chi-squared test also found no significant group difference on lifetime AUD diagnosis at baseline (p>.05).
Table 1.
Change of women’s partnership status over 12 years (N=273).
| Partnership status | Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 |
|---|---|---|---|---|---|
| Not coupled | 0 (0%) | 21 (8%) | 20 (10%) | 29 (13%) | 42 (19%) |
| Coupled with original partner | 273 (100%) | 224 (90%) | 175 (83%) | 167 (76%) | 152 (69%) |
| Coupled with another partner | 0 (0%) | 5 (2%) | 15 (7%) | 24 (11%) | 27 (12%) |
| Total a | 273 | 250 | 210 | 220 | 221 |
Note: The numbers in each cell are number of women (within-wave percentage).
163 (60%) women completed all 5 assessments; 56 (20%) participated in 4 assessments; the rest of 54 (20%) women only had data at 2 or 3 waves.
Domains of Measurement and Instruments
Alcohol Problems and Symptomatology of Women and Their Spouses
The Drinking and Drug History Questionnaire (DDHQ; Zucker, Fitzgerald, & Noll, 1990) was used to measure alcohol problems in the past three years at each wave (T1-T5). It incorporates items from national epidemiologic studies of drugs (Johnston, Bachman, & O'Malley, 1979) and alcohol (Cahalan, Cisin, & Crossley, 1969) as well as from a structured clinical symptom questionnaire (Schuckit, 1978). In this study, we used the women’s and their partners’ alcohol problems at each wave as a time-varying outcome and a time-varying covariate, respectively.
Antisocial Symptomatology of Women and Their Spouses
The Antisocial Behavior Checklist (ASB; Zucker, 1999) was used to assess the women’s and their partners’ antisocial behavior in the past three years at each wave. The composite scores were used as a time-varying outcome and a time-varying covariate in our longitudinal models, respectively. Adequate reliability and validity of the ASB have been established by a series of studies on different populations (Zucker, 1999).
Depressive Symptomatology for Women and Their Spouses
The Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) was used as the depressive symptomatology index. The HRSD is an instrument for the clinical rating of depression; it was coded following administration of the Diagnostic Interview Schedule (DIS) by the clinician who conducted the interview. Ratings were made for “past year” and “current” depression. Inter-rater reliabilities have ranged from .80 to .90 (Hamilton, 1969). Current depression ratings for the women and their partners at time of assessment were used as a time-varying outcome and a time-varying covariate, respectively.
Women’s Lifetime Symptomatology
The Diagnostic Interview Schedule III (DIS III; Robins, Helzer, Croughan, & Ratcliff, 1980) is a well validated and widely used diagnostic instrument that allows trained interviewers to gather extensive information about psychiatric, physical, alcohol-related, and drug-related symptoms. The numbers of possible symptoms were 10 for alcohol use disorder (AUD), 9 for major depressive disorder (MDD), and 6 for antisocial personality disorder (ASPD). We calculated the percentages of lifetime symptoms on these disorders endorsed by the women at baseline, and used them as time-invariant predictors in the models to test the hypothesis of continuity of symptomatology over time. The interactions between these variables with time were also tested to see if the effect of women’s original level of psychopathology changed during the 12 years.
Women’s Social Support Level
The Norbeck Social Support Questionnaire (Norbeck, Lindsey, & Carrieri, 1981) was used to evaluate a woman’s social support using an interview format. Respondents generated a list of significant others in their life, and then answered a series of questions about those relationships. The instrument generates measures of the support network quantity, duration, and quality. Excellent reliability and validity have been documented (Norbeck et al., 1981). In this study, we used the total social support score (calculated as the product of the average support level from all sources and the total number of persons in the network) at each wave as a time-varying covariate; this effect was examined prior to spousal psychopathology because in families where the likelihood of separation/divorce is high, it is likely to be more proximal to the women.
Children’s Symptomatic Status
Because formal psychiatric symptomatology is not yet well developed in earlier childhood, we used parent reported behavioral symptomatology measures as assessed with the Child Behavior Checklist (CBCL; Achenbach, 1991) to evaluate children’s symptomatic status at each wave. A majority of the studies on children’s mental health are based on maternal-reported behavior problems (Leventhal & Brooks-Gunn, 2000). However, when examining the effects of offspring behavior problems on women’s symptomatology, reliance solely on maternal report may be problematic because of the women’s rater bias. In fact, Bartels et al.’s (2003) work on the CBCL found that each parent assessed a rater-specific aspect of the child’s behavior as well as a common view. We thus used CBCL ratings by both parents to alleviate these bias effects (each parent completed the ratings independently). Given that alcohol use disorder and antisocial personality disorder are both largely externalizing disorders, and depression is an internalizing one, the CBCL externalizing and internalizing broadband scales were used. The reliability and validity of the CBCL have been well established (Achenbach, 1991). In the current study, the internalizing and externalizing scores for each child were the averages of the ratings by the parents who lived together with the child at a particular wave. The overall child symptomatology effect on their mother’s mental health was measured by averaging scores of all the children who were living with the mother at a particular wave. These scores were employed as time-varying covariates in the longitudinal models.
Background Demographic Characteristics
A Demographic Questionnaire was used to assess the background characteristics of each person and his/her family of origin. At each wave, both partners reported their occupations which were coded for socioeconomic status (SES) based on the Duncan Socioeconomic Index, one of the best measures when our study began (Mueller & Parcels, 1981). The index is a continuous scale ranging from 0 (unemployed) to 9.04 (law professor). Family SES was calculated by averaging SES codings of both partners who lived together at a particular wave. For the wave(s) when the woman was not coupled, only her SES coding was used to measure family SES. We included family SES as a time-varying covariate in our longitudinal analysis.
Family Crisis as a Source of Family Stress
The Family Crisis List, a 40-item measure of family troubles, was developed by the staff of the Oregon Social Learning Center to record specifically family related stressors, and to document the interaction between stress and patterns of family coerciveness (Patterson, 1982). At each wave, the women and their partners independently identified events that happened during the last 6 months. Due to the concern that family crises may partly reflect the severity of participants’ psychopathology (Cutrona et al., 2005), we selected a subset of 13 events to be included in the analysis which were independent of the individual’s own actions or symptomatology such as “a major repair was necessary for household or household item,” “something stolen from the house,” etc. The average of the total events reported by the women and their partners was used as a time-varying covariate in the longitudinal models.
Residential Neighborhood Characteristics
Residential addresses of the 273 women from T1 to T5 were matched with census tract coding at the census years (April 1st of 1980April 1st of 1990, or 2000) that were closet to the assessment dates. During this period of 12 years, 146 (53%) of the women moved to different census tracts, so their neighborhood characteristics were likely to change. For participants who remained in the same census tract, census statistics for those neighborhoods also often underwent change due to changes in the local socioeconomic environment and the resident composition. The following six neighborhood variables that may relate to individual symptomatology were computed to characterize neighborhood environments: (1) adult unemployment rate; (2) poverty rate; (3) percentage of residents without a high school diploma; (4) percentage of residents living in different residence 5 years ago; (5) percentage of vacant households; and (6) percentage of rented housing units. Principal component analysis on baseline data was conducted to investigate the possibility of reducing dimensions. Results showed that there were two major components: i) the socioeconomic disadvantage component with high loadings on the first three neighborhood variables (explaining 56% of the variance); and ii) the residential instability component with high loadings on the other three variables (explaining 24% of the variance). In order to make the composite scores comparable across T1 to T5 (the loadings in each wave may vary), we constructed each of the two composite scores by averaging the three corresponding standardized census variables. We used these two composite scores at each wave as time-varying covariates to test the effect of neighborhood risk.
Analytic Approach
Linear mixed modeling (Singer & Willett, 2003; Verbeke & Molenberghs, 2000) was adopted to analyze the five-wave longitudinal data set. The major strength of this method is that it does not assume that an equal number of repeated observations are taken from each individual. This makes it highly applicable for longitudinal studies because missing data points are common in such settings. For example, 60% of women in our study completed all five assessments; 20% participated in four assessments; while the remaining 20% only had data at 2–3 waves. The second strength of the method is that it allows time-varying covariates to be included in the model. In the present case, all the individual, familial, and neighborhood variables can be expected to change over time with the exception of women’s lifetime psychopathology at baseline so this method makes it possible to model such dynamic effects. The third strength is that it allows individual differences in the trajectories of symptom development by including random effects on the initial status and change rate.
Because the multi-wave outcomes are dependent within an individual, the model specifies a correlation structure and estimates the corresponding parameters along with the effects of interest. The MLS conducts an assessment every three years, and it would be anticipated that adjacent assessments be more highly correlated than assessments farther apart in time; this was verified by the sample correlation matrices of the outcome measures. The parsimonious first-order autoregressive model was employed to model the correlation structure because more complex models did not significantly improve goodness-of-fit based on the Bayesian information criterion (BIC; Schwarz, 1978), and it is highly desirable to reserve power and efficiency for testing the individual, family, and neighborhood effects (Littell, Milliken, Stroup, Wolfinger, & Schabenberger, 2006).
Another issue is that some of the marital partnerships dissolved at later waves. Table 1 shows the distribution of partnership status at each wave. At Wave 1, all the women were coupled. At Wave 5, 69% were still with original partners, while others had re-coupled at some point after the first wave. For those who did not couple with anyone at later waves, partners’ symptomatology was missing at those waves. A simple approach to deal with this is to exclude those wave data from the analysis. But, such approach would reduce statistical power for testing the individual, family and neighborhood effects due to excluding 112 records (21+20+29+42). We adopted the multiple imputation approach (Rubin, 1987; Schafer & Graham, 2002) to impute five sets of complete data using SAS PROC MI and to aggregate five sets of linear mixed models using SAS PROC MIANALYZE. This approach preserved all the available data and the imputation was based on the missing at random (MAR) mechanism, which assumes that the probabilities of missingness depend on observed data but not on missing data. This assumption is legitimate because partners’ symptomatology tends to be associated with the women’s symptomatolgy, children’s symptomatology, and other observed risk factors. Although there is no way to test whether MAR holds in real data, empirical results from a simulation study showed that an erroneous assumption of MAR may often have only a minor impact on estimation in many realistic settings (Collins, Schafer & Kam , 2001).
We fitted a linear mixed model for each of the women’s mental health outcomes following the developmental cumulation model of risk described in the introductory section and schematically illustrated in Figure 1. We first entered in women’s wave-specific age and coupled status and then tested the effect of women’s lifetime symptomatology at baseline by entering the primary disorder first; the other comorbid disorders only remained in the model if they had additional contributions to the outcome. For those lifetime symptoms that predicted the time-varying outcomes, their interactions with time were also tested to see if the effects of women’s symptomatic history changed over time. After women’s age, coupled status, and symptomatic history were considered, the effect of women’s social support was examined and was only retained in the model if it was significant.
Conditional on the women’s individual characteristics, the effect of partners’ symptomatology was examined: the isomorphic disorder was tested first and then the other comorbid disorders in the order of their relevance to the outcome. For alcohol, antisocial, and depression outcomes, the sequences were AUD-ASPD-depression, ASPD-AUD-depression, and depression-AUD-ASPD, respectively. Given the women’s individual characteristics and their partners’ symptomatology, the additional effect of children’s symptomatology was examined –for alcohol related problems and antisocial behavior, externalizing behavior was most relevant so it entered into the model first; for depression, internalizing was tested first. After all the symptomatology variables were in the model, the effect of family stress (including family SES and crisis) was tested and retained only if it was significant. At the last stage, the effect of neighborhood environment was examined, conditional on all the individual and familial influences.
Results
Descriptive Statistics
Table 2 shows the descriptive statistics of the individual and familial characteristics, symptomatology, and neighborhood environment at baseline. The average age of the 273 women was 31(4) when they were recruited into the study. Their domestic partners were about two years older on average. They had on average 2(0.86) children in the family at baseline. The mean family SES was 3.29(1.30) corresponding to a restaurant/cafeteria/bar manager (3.25), or telephone installer/repairman (3.26).
Table 2.
Descriptive statistics of women’s individual and familial characteristics, symptomatology, and neighborhood environment at baseline (N=273).
| Variables | Mean | Standard Deviation |
|---|---|---|
| Demographic and family stress characteristics | ||
| Women’s age | 30.98 | 4.18 |
| Partners’ age | 33.01 | 5.13 |
| Number of children | 2.29 | 0.86 |
| Women’s social support level | 26.76 | 12.19 |
| Family SES | 3.29 | 1.30 |
| Family crisis | 1.03 | 0.83 |
| Women’s symptomatology | ||
| Lifetime DIS-III AUD symptom percentage | 6.63 | 12.96 |
| Lifetime DIS-III ASPD symptom percentage | 11.05 | 13.14 |
| Lifetime DIS-III MDD symptom percentage | 20.63 | 28.15 |
| Alcohol problems (DDHQ) | 1.09 | 2.36 |
| Antisocial behavior (ASB) | 4.63 | 3.44 |
| Depression (HRSD) | 5.54 | 6.30 |
| Partners’ symptomatology | ||
| Alcohol problems (DDHQ) | 4.32 | 5.43 |
| Antisocial behavior (ASB) | 9.61 | 7.58 |
| Depression (HRSD) | 4.52 | 5.86 |
| Children’s symptomatology | ||
| Externalizing behavior ratings (CBCL) | 11.76 | 5.66 |
| Internalizing behavior ratings (CBCL) | 5.19 | 3.63 |
| Neighborhood environment (census tract variables) | ||
| Adult unemployment rate a | 6.54 | 3.65 |
| Poverty rate a | 10.00 | 7.56 |
| Percentage of residents without high school diploma a | 18.19 | 7.93 |
| Percentage of residents living in different residence 5 years ago b | 45.71 | 9.89 |
| Percentage of vacant households b | 4.24 | 2.15 |
| Percentage of rented housing units b | 28.65 | 15.50 |
These variables were used to calculate the composite score of socioeconomic disadvantage.
These variables were used to calculate the composite score of residential instability.
The women had on average 7(13)%, 11(13)%, and 21(28)% of the possible AUD, ASPD, and major depressive (MDD) symptoms measured by DIS III, respectively, during their lifetime at baseline. The variances were large on all three disorders. In terms of the women’s lifetime diagnoses at baseline, 23%, 0.4%, and 14% of them met the diagnosis criteria of AUD, ASPD, and MDD, respectively. The epidemiological data from the National Comorbidity Survey in the same years showed that women’s lifetime prevalence of the three disorders were 15%, 1%, and 21%, respectively (Kessler, McGonagle, Zhao, Nelson, Hughes, Eshleman et al., 1994). We also found two patterns of diagnostic comorbidity: 6% of the sample had dual lifetime diagnoses of AUD and MDD; 0.4% had dual lifetime diagnoses of AUD and ASPD. As would be expected, partners’ current alcohol problems and antisocial behavior were higher than women’s on average. Children had more externalizing behavior problems than internalizing ones at baseline.
The baseline census variables provide a general picture of the neighborhood environment of these families. On average, these neighborhoods had 7(4)% adult residents who were unemployed, 10(8)% residents who were in poverty, 18(8)% residents who did not have a high school diploma, 46(10)% residents who lived in different residence 5 years ago, 4(2)% households that were vacant, and 29(16)% housing units that were rented.
Linear Mixed Models
Table 3 shows the fitted linear mixed models of women’s symptomatology including alcohol problems, antisocial behavior, and depression as a function of the women’s individual characteristics, partners’ and children’s symptomatology, the level of family stress and the neighborhood environment. The regression coefficients with standard errors and hypothesis testing results are listed in the table.
Table 3.
Linear mixed models of longitudinal changes in women’s symptomatology (N=273).
| Alcohol problems | Antisocial behavior | Depression | |
|---|---|---|---|
| Intercept | −0.626 (0.677) | 2.414* (0.783) | 1.800 (1.567) |
| Women’s individual characteristics | |||
| Age | 0.033* (0.015) | −0.056* (0.018) | 0.068* (0.034) |
| Partnership (binary) | −0.359 (0.254) | 0.325 (0.270) | 0.953 (0.690) |
| Lifetime AUD symptomatology | 0.148* (0.032) | 0.109* (0.037) | - |
| Lifetime AUD X Age | −0.003* (0.001) | −0.002* (0.001) | - |
| Lifetime ASPD symptomatology | - | 0.101* (0.037) | - |
| Lifetime ASPD X Age | - | −0.002* (0.001) | - |
| Lifetime Depression symptomatology | - | - | 0.050* (0.009) |
| Lifetime Depression X Age | - | - | - |
| Social support | - | - | −0.036* (0.017) |
| Partners’ symptomatology | |||
| Alcohol problems | 0.047* (0.016) | 0.043* (0.020) | - |
| Antisocial behavior | - | 0.126* (0.017) | - |
| Depression | - | - | 0.514* (0.033) |
| Children’s symptomatology | |||
| Externalizing | 0.053* | 0.060* | - |
| behavior ratings | (0.014) | (0.014) | |
| Internalizing | - | - | 0.130* |
| behavior ratings | (0.053) | ||
| Family stress | |||
| Family SES | - | - | −0.502* (0.157) |
| Family crisis | - | 0.174* (0.072) | - |
| Neighborhood environment | |||
| Socioeconomic disadvantage | - | 0.291* (0.092) | - |
| Residential instability | 0.219* (0.108) | - | 0.694* (0.277) |
The numbers in each cell are regression coefficient (standard error) with
indicating p<.05.
The Model of Alcohol Problems
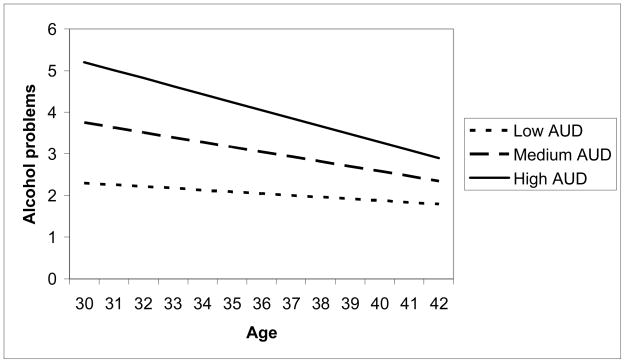
Women’s coupling status was unrelated to the level of alcohol problems experienced at the same wave. Their history of AUD predicted their alcohol problems at each wave but this effect changed over time. History of other comorbid disorders did not have an additional effect. In order to understand how their alcohol problems developed from T1 through T5, both the significant main age effect and the significant interaction between lifetime AUD and age need to be considered. Figure 2 shows the longitudinal changes in women’s alcohol problems by three levels of lifetime AUD symptomatology (low=25th percentile; medium=50th percentile; high=75th percentile). Overall, the level of alcohol problems decreased during the 12 year interval. Although women with a history of higher AUD symptomatology tended to have more alcohol problems at each wave, group differences decreased over time. Conditional on the women’s age, partnership status, and psychopathology history, their level of social support did not have a significant association with their level of alcohol problems. On the other hand, partners’ alcohol problems were positively related to their wives’ alcohol problems, but the other comorbid disorders of the partners had no significant statistical effect. Children’s externalizing behavior problems were positively correlated with their mothers’ alcohol problems, but their internalizing behavior problems were not. Conditional on women’s individual characteristics and familial symptomatology, family SES and crises were not associated with the alcohol problem level. Neighborhood residential instability was associated with a higher level of alcohol problems, even given the individual and familial influences. Neighborhood socioeconomic disadvantage, on the other hand, did not have a significant statistical effect.
Figure 2.
Longitudinal changes in women’s alcohol problems by lifetime AUD symptomatology levels at baseline.
The Model of Antisocial Behavior
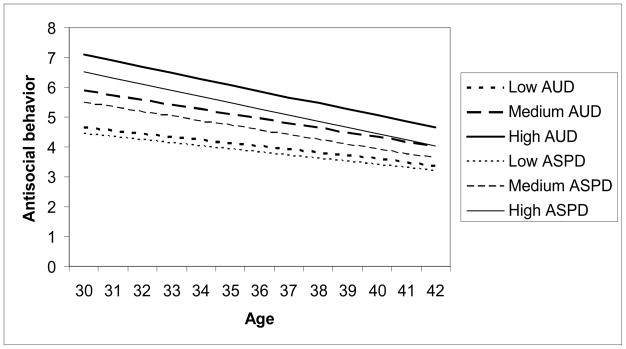
Similarly to the alcohol problem result, partnership status at each wave was not associated with antisocial behavior. However, women’s age, lifetime AUD and ASPD symptomatology, and the interactions between age and lifetime symptomatology all showed significant relationships with the antisocial behavior at each wave. Figure 3 shows the longitudinal changes in antisocial behavior by lifetime AUD and ASPD symptomatology levels. Overall, antisocial behavior decreased with aging. Although women with a history of higher AUD or ASPD symptomatology levels tended to have more antisocial behavior at each wave, group differences diminished over time. Conditional on women’s age, partnership, and psychopathology history, social support was not associated with antisocial behavior. Partners’ alcohol problems and antisocial behavior on the other hand were both positively related to women’s antisocial behavior but partners’ level of depression did not have an additional statistical effect. Children’s externalizing behavior problems were associated with more antisocial behavior in their mothers, but their internalizing behavior problems were not. Conditional on individual characteristics and familial symptomatology, family crisis was positively correlated with antisocial behavior level, whereas family SES did not have an effect. Neighborhood socioeconomic disadvantage was associated with more antisocial behavior, controlling for individual and familial influences. Neighborhood residential instability, on the other hand, did not have an effect.
Figure 3.
Longitudinal changes in women’s antisocial behavior by lifetime AUD & ASPD symptomatology levels at baseline.
The Model of Depression
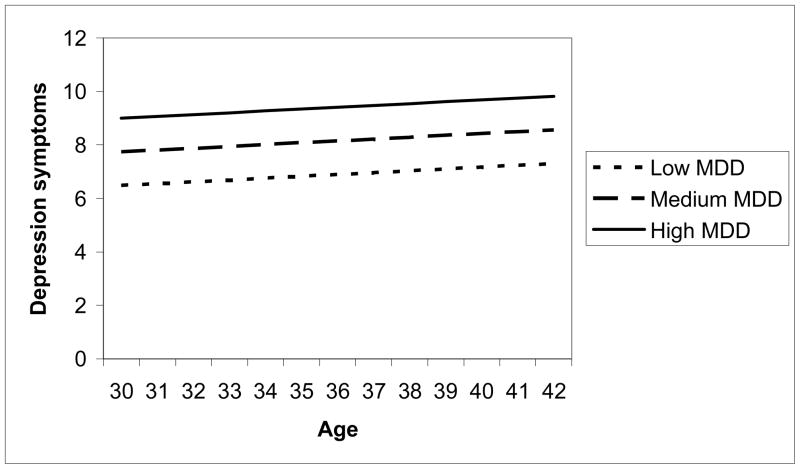
While women’s partnership status at each wave was not associated with their level of depression, their age and baseline level of lifetime depressive symptomatology were. Figure 4 shows the longitudinal changes in women’s depression by lifetime symptomatology levels at baseline. Overall, women’s depression levels increased with increasing age. Unlike alcohol problems and antisocial behavior, the effect of depression history on the level of depressive symptoms did not change over time. Women with a history of higher depressive symptomatology levels consistently had more depressive symptoms at each wave. Conditional on age, partnership status, and psychopathology history, social support was negatively associated with depression: those with poorer support had higher levels of symptoms. In addition, partners’ depressive symptom level was positively correlated with women’s symptomatology, but there was no effect for the other comorbid disorders. Children’s internalizing behavior problems were associated with higher depression levels in their mothers, but their externalizing behavior problems were not. Conditional on women’s individual characteristics and familial symptomatology, lower family SES was associated with higher depression, whereas family crisis was not. Neighborhood residential instability was associated with higher depression, controlling for individual and familial influences. Neighborhood socioeconomic disadvantage, on the other hand, did not have an association.
Figure 4.
Longitudinal changes in women’s depression by lifetime MDD symptomatology levels at baseline.
Discussion
Unique Contributions of This Study
The current study makes a unique contribution to the literature by examining the specific contributions of multilevel influences from the individual, family, and neighborhood on the longitudinal development of women’s psychopathology. All of these influences have previously been examined separately, or in small combinations, most often cross-sectionally, and to a lesser degree longitudinally. As far as we can determine, never have they been examined in a combination covering the breadth of the personal and social environment that was characterized here. The fact that these effects were examined over the course of more than a decade, adds still another level of uniqueness to the findings. Furthermore, this study tracked women’s symptomatic course during the earlier years of married life and motherhood in three major diagnostic domains: alcoholism, antisocial personality disorder, and depression. Especially, our investigation of women’s antisocial behavior during this developmental period has filled in a knowledge gap in the literature.
Longitudinal Changes and Continuity of Women’s Symptomatology
Our findings demonstrate the complexity of the drivers of maintenance and change in alcohol problems, antisociality, and depression among women during a 12 year time span in their earlier adult years. Looking most simplistically, the findings show continuity in symptomatology for all three disorders: holding all the other risk factors constant, women with a history of more symptomatology at baseline continue to have higher levels of symptomatology over the course of the 12 year interval. The patterns of longitudinal changes during the interval, as illustrated in Figures 2–4, are that overall alcohol problems and antisocial behavior decrease for women, but their depression increases.
The longitudinal trajectory of women’s alcohol problems seems to match the national data (Karlamangla et al., 2006; Kerr et al., 2009). Given the methodological shortcomings of the limited literature on developmental trajectories of antisocial behavior in women –such as relying on official crime data, covering restrictive developmental periods, and having small sample sizes (Fontaine, et al., 2009) – our data provide a new and important piece of information about the long-term development of women’s antisocial behavior in high risk family or neighborhood environments. Our data also allow us to look at the longitudinal development of women’s depression during the demanding period of their motherhood. Although cross-sectional studies have showed that depression in women at ages 30–40 is relatively low and flat (i.e. at the bottom of the U) in comparison to earlier or later developmental periods (Mirowsky & Kim, 2007), our data demonstrate that some women at this developmental stage still develop elevated depressive symptomatology, especially if they are caring for young children or living in high risk family or neighborhood environment.
Partners’ and Children’s Psychopathology
Our results show that the husband’s isomorphic symptomatology had impact on his wife’s psychopathology. In addition, husbands’ alcoholism symptomatology carried significant risk for a heightened level of antisociality in their wives. Higher children’s externalizing behavior was associated with their mothers’ elevated alcohol and antisocial symptomatology; their internalizing behavior was related to a heightened level of depression in their mothers. These findings are consistent with results from a large-scale twin study (Kendler, Prescott, Myers, & Neale, 2003) that identified two genetic factors: 1) one was an internalizing factor, related to depression and anxiety; 2) the second was an externalizing factor, related to AUD, ASPD, and externalizing behavior more broadly (impulsivity, aggression).
Our finding of the influence of partners’ antisocial behavior on women’s antisocial behavior during the course of the marriage is consistent with the finding of another longitudinal study showing that continuity of women’s antisocial behavior depends on partners’ parallel symptomatology (Moffitt et al., 2001). We have also demonstrated spousal impact on women’s AUD and depression during the course of marriage, as have the other longitudinal studies (Holahan et al., 2007, Leonard & Mudar, 2004; Merline at al., 2008). Additionally, our study has shown the negative impact of the children’s problem behavior on their mothers’ alcohol problems, antisocial behavior, and depression over a 12 year interval of family life. Given that the literature on child-to-mother influence is sparse, our study has joined a handful of existing studies (Fuller et al., 2003; Gross et al., 2009; Timko et al., 2000), which have examined these important risk factors for mothers’ psychopathology.
Neighborhood Residential Instability
Our investigation of neighborhood effects on women’s psychopathology includes not only the most commonly examined effect of neighborhood SES, but also the effect of neighborhood residential instability – an important but often ignored risk factor in neighborhood studies. We used census data instead of self-report data to construct such an index so that our results would not be confounded by participants’ subjective perception of neighborhood disorder. Our results show that living in an unstable neighborhood, where residents move in/out frequently, is a significant contributor to the development of women’s alcohol problems and depression, even when women’s social support, familial psychopathology, and family stress are controlled. These results are consistent with our previous longitudinal analysis on these women’s offspring (Buu et al., 2009), which has shown that children whose neighborhoods become more stable from early childhood to adolescence tend to develop fewer AUD symptoms, and children whose neighborhoods become less stable develop more depression symptoms in late adolescence. Thus, neighborhood residential instability has a negative impact not only upon youth but also on their mothers.
Limitations
The study sample consists of Caucasian women from families at high risk for substance use disorder so the results may not be generalizable to the general population. Because of the family study design of the MLS, the men recruited into the study needed to reside with their son and his biological mother at the time of initial recruitment. In addition, at least one son needed to be between the ages of 3 and 5 at study entry. This inclusionary criterion reduces external validity somewhat, as results can only be generalized to women with children who were born in an initially coupled relationship, and also only to families at a relatively early stage of the family life cycle. At the same time, this latter limitation is also an advantage, in that control of family life cycle stage will reduce the extraneous variance that might be anticipated because contextual effects will have different impact at different family life cycle stages.
According to the definitions in the introduction section, the effects of assortative mating and contagion can only be differentiated if both the premarital and postmarital data are available. Our study recruited married couples with children so we do not have prospective data to test the premarital process (i.e. assortative mating). The spousal influences on women’s symptomatology found in this study are likely to be the results of a combination of both processes.
Implications
The results of our longitudinal analyses indicate that unlike alcohol problems and antisocial behavior, women’s depression does not naturally “mature out.” In fact, it tends to be more elevated during the course of their marital relationship and the later years of their motherhood. Our results underscore the recent attention to serious psychological distress among women of childbearing age and reinforce the policy that intervention efforts should target this important area (Tsai, Floyd, O’Connor, & Velasquez, 2009). On the basis of our multilevel longitudinal models, such interventions might be directed at improving (1) the social support system, (2) educational or professional training opportunities, (3) the accessibility of family counseling to address issues of spousal impact and parenting stress, and (4) the neighborhood environment.
While women’s alcohol problems and depression are only affected by their isomorphic symptom history, their level of antisocial behavior is influenced by their prior history of ASPD as well as their history of AUD. This finding underscores the externalizing nature of the two disorders and the intimate connection between the two comorbidities. In order to increase the effectiveness, intervention programs for women’s antisocial behavior should address the likely comorbidity of alcohol problems.
According to Sampson, Raudenbush, and Earls (1997), neighborhood residential instability hinders the formation of social cohesion among neighbors, and weakens their willingness to intervene on behalf of the common good. The association between neighborhood residential instability and women’s/youth’s alcohol problems and depression may be largely mediated by such low “collective efficacy.” Community efforts to improve the neighborhood environment, such as by providing support networks for residents and by building community-level institutions to supervise and monitor the behavior of residents, may usefully reduce women’s/youth’s risk for alcohol problems and depression.
Acknowledgments
This work was supported by National Institute on Alcohol Abuse and Alcoholism Grants K01 AA016591 to A. Buu and R37 AA07065 to R. A. Zucker. The first author and the senior author contributed equally to the development of this paper. The authors would like to thank Susan Refior, Brenton Nier, and Shauncie Skidmore for their help with the manuscript.
References
- Achenbach TM. Manual for the child behavior checklist / 4–18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Bartels M, Hudziak JJ, Boomsma DI, Rietveld MJH, Van Beijsterveldt TCEM, Van den Oord EJCG. A study of parent ratings of internalizing and externalizing problem behavior in 12-year-old twins. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1351–1359. doi: 10.1097/01.CHI.0000085755.71002.5d. [DOI] [PubMed] [Google Scholar]
- Belle D, Doucet J. Poverty, inequality, and discrimination as sources of depression among U.S. women. Psychology of Women Quarterly. 2003;27:101–113. [Google Scholar]
- Bogat GA, Leahy K, von Eye A, Maxwell C, Levendosky AA, Davidson WS. The influence of community violence on the functioning of women experiencing domestic violence. American Journal of Community Psychology. 2005;36(1–2):123–132. doi: 10.1007/s10464-005-6237-2. [DOI] [PubMed] [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and alcoholics anonymous on abstinence. Journal of Studies on Alcohol. 2003;64:579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO. Depression. In: Harris GW, Harris TO, editors. Life events and illness. New York: Guilford Press; 1989. pp. 49–93. [Google Scholar]
- Buu A, DiPiazza C, Wang J, Puttler LI, Fitzgerald HE, Zucker RA. Parent, family, and neighborhood effects on the development of child substance use and other psychopathology from preschool to the start of adulthood. Journal of Studies on Alcohol and Drugs. 2009;70:489–498. doi: 10.15288/jsad.2009.70.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buu A, Mansour M, Wang J, Refior SK, Fitzgerald HE, Zucker RA. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcoholism: Clinical and Experimental Research. 2007;31(9):1545–1551. doi: 10.1111/j.1530-0277.2007.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Ramisetty-Mikler S, Floyd LR, McGrath C. The epidemiology of drinking among women of child-bearing age. Alcoholism: Clinical and Experimental Research. 2006;30:1023–1030. doi: 10.1111/j.1530-0277.2006.00116.x. [DOI] [PubMed] [Google Scholar]
- Cahalan D, Cisin I, Crossley H. American drinking practice: A national study of drinking behavior and attitudes. New Brunswick, NJ: Publications Division, Rutgers Center for Alcohol Studies; 1969. [Google Scholar]
- Christensen HB, Bilenberg N. Behavior and emotional problems in children of alcoholic mothers and fathers. European Child and Adolescent Psychiatry. 2000;9:219–226. doi: 10.1007/s007870070046. [DOI] [PubMed] [Google Scholar]
- Clark C, Ryan L, Kawachi I, Canner MJ, Berkman L, Wright RJ. Witnessing community violence in residential neighborhoods: A mental health hazard for urban women. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2008;85(1):22–38. doi: 10.1007/s11524-007-9229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DB, Cornelius J, Wood DS, Vanyukov M. Psychopathology risk transmission in children of parents with substance use disorders. American Journal of Psychiatry. 2004;161:685–691. doi: 10.1176/appi.ajp.161.4.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Schafer JL, Kam C. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods. 2001;6:330–351. [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, Gardner KA. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. Journal of Abnormal Psychology. 2005;114(1):3–15. doi: 10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Hessling RM, Brown PA, Murry V. Direct and moderating effects of community context on the psychological well-being of African American women. Journal of Personality and Social Psychology. 2000;79(6):1088–1101. doi: 10.1037//0022-3514.79.6.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Harford TC, Grant BF. Family history as a predictor of alcohol dependence. Alcoholism: Clinical and Experimental Research. 1992;16:572–575. doi: 10.1111/j.1530-0277.1992.tb01419.x. [DOI] [PubMed] [Google Scholar]
- Dierker LC, Merikangas KR, Szatmari P. Influence of parental concordance for psychiatric disorders on psychopathology in offspring. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:280–288. doi: 10.1097/00004583-199903000-00015. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Vaveh G, Link BG, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- Feighner JP, Robins E, Guze SB, Woodruff RA, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Archives of General Psychiatry. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Fitzgerald HE, Zucker RA. Pathways of risk aggregation for alcohol use disorders. In: Freeark K, Davidson WS III, editors. The crisis in youth mental health: Vol 3. Issues for families, schools, and communities. Westport, CT: Praeger Press; 2006. pp. 249–271. [Google Scholar]
- Floyd FJ, Cranford JA, Daugherty MK, Fitzgerald HE, Zucker RA. Marital interaction in alcoholic and nonalcoholic couples: Alcoholic subtype variations and wives' alcoholism status. Journal of Abnormal Psychology. 2006;115(1):121–130. doi: 10.1037/0021-843X.115.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine N, Carbonneau R, Vitaro F, Barker ED, Tremblay RE. Research review: a critical review of studies on the developmental trajectories of antisocial behavior in females. Journal of Child Psychology and Psychiatry. 2009;50:363–385. doi: 10.1111/j.1469-7610.2008.01949.x. [DOI] [PubMed] [Google Scholar]
- Fuller BE, Chermack ST, Cruise KA, Kirsch E, Fitzgerald HE, Zucker RA. Predictors of aggression across three generations among sons of alcoholics: relationships involving grandparental and parental alcoholism, child aggression, marital aggression and parenting practices. Journal of Studies on Alcohol. 2003;64:472–483. doi: 10.15288/jsa.2003.64.472. [DOI] [PubMed] [Google Scholar]
- Glynn RJ, Bouchard GR, LoCastro JS, Laird NM. Aging and generational effects on drinking behaviors in men: results from the Normative Aging Study. American Journal of Public Health. 1985;75:1413–1419. doi: 10.2105/ajph.75.12.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S, Gotlib I. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Bulletin. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Burwell RA, Nagin DS. Transactional processes in child disruptive behavior and maternal depression: a longitudinal study from early childhood to adolescence. Development and Psychopathology. 2009;21:139–156. doi: 10.1017/S0954579409000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. Standardised assessment and recording of depressive symptoms. Psychiatria, Neurologia, Neurochirurgia. 1969;72:201–205. [PubMed] [Google Scholar]
- Hammen C. Interpersonal stress and depression in women. Journal of Affective Disorders. 2003;74:49–57. doi: 10.1016/s0165-0327(02)00430-5. [DOI] [PubMed] [Google Scholar]
- Henderson C, Roux AVD, Jacobs DR, Kiefe CI, West D, Williams DR. Neighbourhood characteristics, individual level socioeconomic factors, and depressive symptoms in young adults: the CARDIA study. Journal of Epidemiology and Community Health. 2005;59(4):322–328. doi: 10.1136/jech.2003.018846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Social Science & Medicine. 2005;61(5):965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Hill TD, Mossakowski KN, Angel RJ. Relationship violence and psychological distress among low-income urban women. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2007;84(4):537–551. doi: 10.1007/s11524-007-9187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Moerkbak ML, Cronkite RC, Holahan CK, Kenney BA. Spousal similarity in coping and depressive symptoms over 10 years. Journal of Family Psychology. 2007;21:551–559. doi: 10.1037/0893-3200.21.4.551. [DOI] [PubMed] [Google Scholar]
- Israel BA, Farquhar SA, Schulz AJ, James SA, Parker EA. The relationship between social support, stress, and health among women on Detroit’s east side. Health Education & Behavior. 2002;29:342–360. doi: 10.1177/109019810202900306. [DOI] [PubMed] [Google Scholar]
- Jansen RE, Fitzgerald HE, Ham HP, Zucker RA. Pathways into risk: Temperament and behavior problems in three- to five-year-old sons of alcoholics. Alcoholism: Clinical and Experimental Research. 1995;19:501–509. doi: 10.1111/j.1530-0277.1995.tb01538.x. [DOI] [PubMed] [Google Scholar]
- Johnston LD, Bachman JG, O'Malley PM. Drugs and the class of '78: Behaviors, attitudes, and recent national trends. Washington, DC: National Institute on Drug Abuse, Division of Research, U.S. Department of Health, Education, and Welfare; 1979. [Google Scholar]
- Karlamangla A, Zhou K, Reuben D, Greendale G, Moore A. Longitudinal trajectories of heavy drinking in adults in the United States of America. Addiction. 2006;101:91–99. doi: 10.1111/j.1360-0443.2005.01299.x. [DOI] [PubMed] [Google Scholar]
- Kasen S, Cohen P, Chen H, Castille D. Depression in adult women: age changes and cohort effects. American Journal of Public Health. 2003;93:2061–2066. doi: 10.2105/ajph.93.12.2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97:891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale M. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age-period-cohort modeling of alcohol volume and heavy drinking days in the US National Alcohol Surveys: divergence in younger and older adult trends. Addiction. 2009;104:27–37. doi: 10.1111/j.1360-0443.2008.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archive of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75(1):83–119. [Google Scholar]
- Leonard KE, Mudar P. Husbands' influence on wives' drinking: Testing a relationship motivation model in the early years of marriage. Psychology of Addictive Behaviors. 2004;18(4):340–349. doi: 10.1037/0893-164X.18.4.340. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. The neighborhoods they live in: The effects of neighborhood residence on child and adolescent outcomes. Psychological Bulletin. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. Moving to Opportunity: an experimental study pf neighborhood effects on mental health. American Journal of Public Health. 2003;93:1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for Mixed Models. 2. North Carolina: SAS Publishing; 2006. [Google Scholar]
- Maes HHM, Neale MC, Kendler KS, Hewitt JK, Silberg JL, Foley DL, et al. Assortative mating for major psychiatric diagnoses in two population-based samples. Psychological Medicine. 1998;28(6):1389–1401. doi: 10.1017/s0033291798007326. [DOI] [PubMed] [Google Scholar]
- McLeod JD. Social and psychological bases of homogamy for common psychiatric disorders. Journal of Marriage and the Family. 1995;57:201–214. [Google Scholar]
- Merikangas KR, Weissman MM, Prusoff BA, John K. Assortative mating and affective disorders: psychopathology in offspring. Psychiatry. 1988;51:48–57. doi: 10.1080/00332747.1988.11024379. [DOI] [PubMed] [Google Scholar]
- Merline AC, Schulenberg JE, O'Malley PM, Bachman JG, Johnston LD. Substance use in marital dyads: premarital assortment and change over time. Journal of studies on alcohol and drugs. 2008;69(3):352–361. doi: 10.15288/jsad.2008.69.352. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Kim J. Graphing age trajectories: vector graphs, synthetic and virtual cohort projections, and cross-sectional profiles of depression. Sociological Methods & Research. 2007;35:497–541. [Google Scholar]
- Mirowsky J, Ross C. Social causes of psychological distress. Hawthorne: Aldine de Gruyter; 2003. [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva PA. Sex differences in antisocial behavior: conduct disorder, delinquency, and violence in the Dunedin Longitudinal Study. Cambridge, UK: Cambridge University Press; 2001. [Google Scholar]
- Mueller CW, Parcels TL. Measures of socioeconomic status: Alternatives and recommendations. Child Development. 1981;52:13–80. [Google Scholar]
- Mulia N, Schmidt L, Bond J, Jacobs L, Korcha R. Stress, social support and problem drinking among women in poverty. Addiction. 2008;103:1283–1293. doi: 10.1111/j.1360-0443.2008.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura Y, Warner V, Wickramaratne P. Parents concordant for major depressive disorder and the effect of psychopathology in offspring. Psychological Medicine. 2001;31:1211–1222. doi: 10.1017/s0033291701004585. [DOI] [PubMed] [Google Scholar]
- Norbeck JS, Lindsey AM, Carrieri VL. The development of an instrument to measure social support. Nursing Research. 1981;30:264–269. [PubMed] [Google Scholar]
- Patterson G. Coercive family process. Eugene, Oregon: Castilia; 1982. [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, et al. Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology. 1997;25:413–424. doi: 10.1023/a:1025789108958. [DOI] [PubMed] [Google Scholar]
- Rao U, Hammen C, Daley SE. Continuity of depression during the transition to adulthood: a 5-year longitudinal study of young women. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:908–915. doi: 10.1097/00004583-199907000-00022. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- Robins L, Helzer J, Croughan J, Ratcliff KS. The NIMH Diagnostic Interview Schedule: Its history, characteristics and validity. St. Louis, MO: Washington University School of Medicine; 1980. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Schuckit MA. Research questionnaire. San Diego, CA: Alcoholism Treatment Program, V. A. Medical Center, University of California, San Diego; 1978. [Google Scholar]
- Schuckit MA, Smith TL, Eng MY, Kunovac J. Women who marry men with alcohol-use disorders. Alcoholism: Clinical and Experimental Research. 2002;26:1336–1343. doi: 10.1097/01.ALC.0000029585.63550.33. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Israel BA, Zenk SN, Parker EA, Lichtenstein R, Shellman-Weir S, et al. Psychosocial stress and social support as mediators of relationships between income, length of residence and depressive symptoms among African American women on Detroit's eastside. Social Science & Medicine. 2006;62(2):510–522. doi: 10.1016/j.socscimed.2005.06.028. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Gershuny BS, Peterson L, Raskin G. The role of childhood stressors in the intergenerational transmission of alcohol use disorders. Journal of Studies on Alcohol. 1997;58:414–427. doi: 10.15288/jsa.1997.58.414. [DOI] [PubMed] [Google Scholar]
- Simmons LA, Braun B, Charnigo R, Havens JR, Wright DW. Depression and poverty among rural women: a relationship of social causation or social selection? The Journal of Rural Health. 2008;24:292–298. doi: 10.1111/j.1748-0361.2008.00171.x. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Timko C, Kaplowitz MS, Moos RH. Children’s health and child-parent relationships as predictors of problem-drinking mothers’ and fathers’ long-term adaptation. Journal of Substance Abuse. 2000;11:103–121. doi: 10.1016/s0899-3289(99)00023-1. [DOI] [PubMed] [Google Scholar]
- Tsai J, Floyd RL, O’Connor MJ, Velasquez MM. Alcohol use and serious psychological distress among women of childbearing age. Addictive Behavior. 2009;34:146–153. doi: 10.1016/j.addbeh.2008.09.005. [DOI] [PubMed] [Google Scholar]
- Vanyukov MM, Neale MC, Moss HB, Tarter RE. Mating assortment and the liability to substance abuse. Drug and Alcohol Dependence. 1996;42:1–10. doi: 10.1016/0376-8716(96)01255-0. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York: Springer Verlag; 2000. [Google Scholar]
- Wade TD, Kendler KS. Absence of interactions between social support and stressful life events in the prediction of major depression and depressive symptomatology in women. Psychological Medicine. 2000;30:965–974. doi: 10.1017/s0033291799002251. [DOI] [PubMed] [Google Scholar]
- Wadsworth ME, Achenbach TM. Explaining the link between low socioeconomic status and psychopathology: testing two mechanisms of the social causation hypothesis. Journal of Consulting and Clinical Psychology. 2005;73:1146–1153. doi: 10.1037/0022-006X.73.6.1146. [DOI] [PubMed] [Google Scholar]
- Windle M. A longitudinal study of stress buffering for adolescent problem behaviors. Developmental Psychology. 1992;28:522–530. [Google Scholar]
- Windle M. Mate similarity, heavy substance use and family history of problem drinking among young adult women. Journal of Studies on Alcohol. 1997;58:573–580. doi: 10.15288/jsa.1997.58.573. [DOI] [PubMed] [Google Scholar]
- Zucker RA. The four alcoholisms: a developmental account of the etiologic process. In: Rivers PC, editor. Alcohol and Addictive Behaviors Nebraska Symposium on Motivation, 1986. Vol. 34. Lincoln, NE: University of Nebraska Press; 1987. pp. 27–83. [PubMed] [Google Scholar]
- Zucker RA. Pathways to alcohol problems and alcoholism: a developmental account of the evidence for multiple alcoholisms and for contextual contributions to risk. In: Zucker RA, Howard J, Boyd GM, editors. The development of alcohol problems: Exploring the biopsychosocial matrix of risk (NIAAA Research Monograph No. 26) Chapt 13. Rockville, MD: U.S. Department of Health and Human Services; 1994. pp. 255–289. [Google Scholar]
- Zucker RA. Manual for the antisocial behavior checklist. Ann Arbor, MI: IPA Associates; 1999. [Google Scholar]
- Zucker RA. Alcohol use and the alcohol use disorders: a developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 3. Risk, disorder and adaptation. 2. New York: Wiley; 2006. pp. 620–656. [Google Scholar]
- Zucker RA, Ellis DA, Fitzgerald HE, Bingham CR. Other evidence for at least two alcoholism. II. Life course variation in antisociality and heterogeneity of alcoholic outcome. Development & Psychopathology. 1996;8:831–848. [Google Scholar]
- Zucker RA, Fitzgerald HE, Noll RB. Drinking and drug history (version 4) East Lansing, MI: Michigan State University; 1990. [Google Scholar]
- Zucker RA, Fitzgerald HE, Refior SK, Puttler LI, Pallas DM, Ellis DA. The clinical and social ecology of childhood for children of alcoholics: description of a study and implications for a differentiated social policy. In: Fitzgerald HE, Lester BM, Zuckerman BS, editors. Children of Addiction. New York: Garland Press; 2000. pp. 109–141. [Google Scholar]