Abstract
Purpose
Serum biomarker-based screening for pancreatic cancer could greatly improve survival in appropriately targeted high-risk populations.
Experimental Design
Eighty-three circulating proteins were analyzed in sera of patients diagnosed with pancreatic ductal adenocarcinoma (PDAC) (n=333), benign pancreatic conditions (n=144), and healthy control individuals (n=227). Samples from each group were split randomly into training and blinded validation sets prior to analysis. A Metropolis algorithm with Monte Carlo simulation (MMC) was used to identify discriminatory biomarker panels in the training set. Identified panels were evaluated in the validation set and in patients diagnosed with colon (n=33), lung (n=62), and breast (n=108) cancers.
Results
Several robust profiles of protein alterations were present in sera of PDAC patients compared to the Healthy and Benign groups. In a training set (n=160 PDAC, 74 Benign, 107 Healthy), the panel of CA 19-9, ICAM-1, and OPG discriminated PDAC patients from Healthy controls with a sensitivity/specificity (SN/SP) of 88/90%, while the panel of CA 19-9, CEA, and TIMP-1 discriminated PDAC patients from Benign subjects with a SN/SP of 76/90%. In an independent validation set (n=173 PDAC, 70 Benign, 120 Healthy), the panel of CA 19-9, ICAM-1 and OPG demonstrated a SN/SP of 78/94 while the panel of CA19-9, CEA, and TIMP-1 demonstrated a SN/SP of 71/89%. The CA19-9, ICAM-1, OPG panel is selective for PDAC and does not recognize breast (SP=100%), lung (SP=97%), or colon (SP=97%) cancer.
Conclusions
The PDAC-specific biomarker panels identified in this investigation warrant additional clinical validation to determine their role in screening targeted high-risk populations.
Keywords: Pancreatic Cancer, PDAC, Early Detection, Diagnosis, Serum Biomarkers, CA 19-9, Multimarker Panel
Introduction
Pancreatic cancer is the fourth leading cause of cancer death in the United States. In 2010, an estimated 43,140 people will be diagnosed with pancreatic cancer with a staggering 36,800 perishing from the disease 1. Although a variety of tumors can arise in the pancreas, the vast majority of pancreatic tumors, 85–90%, are represented by a specific histological subtype termed pancreatic ductal adenocarcinoma (PDAC) 2. The poor prognosis from PDAC is largely due to our inability to detect the cancer at an early stage when the option of curative resection remains available. Factors contributing to this difficulty include the inaccessible location of the pancreas deep in the abdomen, late-presenting clinical manifestations (e.g., weight loss, epigastric pain, or obstructive jaundice), and the early development of metastasis. As a result, the majority of pancreatic cancer patients present with unresectable disease leading to a median survival of 6 months and an overall 5-year survival of <5%3. In contrast, those few who present with small, surgically-resectable cancers have a realistic chance of cure and a 5-year survival rate of 20–30%4. Owing to the low prevalence of PDAC, it is currently neither advisable nor cost effective to screen the general population 5. Efforts are focused on early screening of selected high-risk-cohorts (more than 10-fold increased risk), who account for approximately 10% of patients with PDAC. These mainly consist of patients with a genetic predisposition for developing PDAC including individuals with a family history in multiple family members, patients with hereditary pancreatitis, Peutz-Jeghers syndrome, hereditary breast-ovarian cancer syndrome, or familial atypical multiple mole melanoma 6. It has been calculated that a screening test with a sensitivity (SN) and specificity (SP) above or near 90% would benefit high-risk groups 5.
There are no reliable screening tests, either molecular or imaging based, for detecting pancreatic cancer in asymptomatic persons and the deep anatomic location of the pancreas makes detection of small localized tumors unlikely during routine abdominal examination. Tumor resolution is a critical factor in the early detection of pancreatic cancer as tumors as small as 2cm in diameter are frequently associated with metastatic disease 7. Commonly used imaging studies (e.g., abdominal CT or MRI) in the setting of a high clinical suspicion of having PDAC are inadequate for diagnosing pancreatic cancer at an early stage since they do not reliably detect pancreatic tumors <1–2 cm in size 8. More accurate tests such as endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS) are inappropriate for screening asymptomatic patients due to their invasiveness, cost and attendant clinical risks 9. The mucin-associated carbohydrate antigen CA 19-9 is a biomarker of PDAC with limited clinical utility in the screening setting. CA 19-9 has demonstrated modest effectiveness in the screening of symptomatic individuals on an outpatient basis with a median SN of 79% (range 70–90%) and median SP of 82% (range 68–91%), however it has been shown to be ineffective in the mass screening of asymptomatic subjects 10. The principal limitations of CA 19-9 include its frequent elevation associated with non-malignant conditions such as pancreatitis and obstructive jaundice, and its inability to detect many early stage malignancies 11. CA 19-9 is also unsuitable for use in the estimated 5 to 10% of patients who are carriers of the Lewis-negative genotype and develop tumors that do not express the antigen 12.
These limitations of CA 19-9 have led investigators to search for alternative biomarkers for use in screening for PDAC. Such alternative serum biomarkers include TPA/TPS, macrophage inhibitory cytokine-1 (MIC-1), IGFBP-1, haptoglobin, SAA, TIMP-1, osteopontin (OPN), HE4, NGAL and others, however none of these have been clinically proven to be superior to CA 19-9 11, 13–19. Several groups have also reported on the performance of combinations of these markers19–21. These multiplexed biomarker approaches have demonstrated improved SN and SP for the detection of pancreatic cancer. For example, in a recent study, a panel of seven proteins (ALCAM, ICAM-1, LCN2, TIMP-1, REG1A, REG3, and IGFBP-4) with or without the addition of CA 19–9, selected based on findings in a mouse model, was able to discriminate human pancreatic cancer cases from matched controls in a small group of pre-symptomatic and pre-diagnostic blood samples 19. In efforts to diagnose pancreatic cancer from benign and healthy controls, TIMP-1 was evaluated along with its target MMP-9 21, while serum levels of OPN were capable of discriminating resectable PDAC from controls with a SN/SP of 80/97 20.
Biomarker profiles indicative of a specific cancer include not only those factors produced by the tumor itself but also represent the systemic response to the growing tumor including acute phase reactants, inflammatory cytokines, growth and angiogenic factors, etc. Additionally, it is likely that levels of proteins secreted or released by the tumor will correlate together and therefore mitigate the advantage of their use in combination. We hypothesize that combinations of biomarkers originating from multiple tumoral and extratumoral sites could offer superior diagnostic ability. Proteins representing the systemic response to malignancy may also reflect advancements in tumor development since the tumor relies on these exogenous factors for growth and spreading. In this study we utilized an extensive array of bead-based assays for a broad range of circulating proteins to evaluate serological alterations present in a diverse group of patients diagnosed with PDAC, non-malignant pancreatic disease, and healthy controls. We identify a number of significant differences in biomarker profiles associated with each diagnosis. Our underlying objective was the identification of a panel of serum biomarkers capable of detecting PDAC with high SN and SP. Such a panel would offer a non-invasive means of screening in appropriately targeted high-risk populations.
Materials and Methods
Patient populations
The study population was comprised of 333 patients with histologically diagnosed pancreatic ductal adenocarcinoma (PDAC), 144 patients with benign pancreatic conditions including acute or chronic pancreatitis, benign pancreatic cysts, or other benign pancreatic neoplasms, 227 healthy controls without a history of pancreatic diseases, and patients diagnosed with colon (n=33), lung (n=62), and breast (n=108) cancer (Table 1). The diagnoses of the patients with benign pancreatic diseases were clinical and guided by standard radiological imaging tests and determined by an experienced pancreatic expert. None of the patients with benign pancreatic diseases or the healthy controls had a history of any malignancies. Samples were obtained prior to any treatments from multiple sources (University of Pittsburgh, Sloan-Kettering Cancer Center, NorthShore University HealthSystems (NUH) -formerly known as Evanston Northwestern Healthcare, University of Alabama Birmingham, Fox Chase Cancer Center, Gynecological Oncology Group, Duke University) and were annotated with information regarding age, diagnosis, disease stage, histology, and grade. Written informed consent was obtained from each subject and the local institutional review boards approved theprotocols for use of each sample collection. All collection sites utilized a standardized protocol for sample collection. Samples were stored at −70°C or colder and shipped on dry ice overnight to UPCI. No more than 2 freeze/thaws were allowed. The Healthy, Benign, and PDAC subjects were randomly assigned to either the training or validation sets (Table 1) and validation samples were blinded until completion of the multivariate analysis.
Table 1.
Clinical Characteristics of Study Population
| Training Set | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Healthy | Benign | PDAC | ||||||||
| Source | Age Range (Median) | Gender | Source | Age Range (Median) | Gender | Dx | Source | Age Range (Median) | Gender | Stage |
| UPCI n = 45 |
24–69 (53) | M = 36 F = 9 |
UAB n = 57 |
32–83 (55) | M = 23 F = 34 |
C = 31 P = 17 O = 9 |
NUH n = 57 |
49–91 (73) |
M = 29 F = 28 |
I = 2 II = 18 III = 1 IV = 34 U = 2 |
| FCCC n = 35 |
39–87 (66) | M = 1 F = 34 |
NUH n = 17 |
23–83 (66) | M = 6 F = 11 |
C = 1 P = 8 O = 8 |
UAB n = 49 |
42–89 (68) | M = 20 F = 29 |
I = 1 II = 3 III = 2 IV = 3 U = 40 |
| NUH n = 19 |
33–77 (55) | M = 6 F = 13 |
SKCC n = 36 |
45–83 (64) | M = 17 F = 19 |
I = 0 II = 12 III = 5 IV = 6 U = 13 |
||||
| GOG n = 8 |
18–61 (44) | M = 0 F = 8 |
UPCI n = 18 |
49–87 (70) | M = 9 F = 9 |
I = 1 II = 0 III = 8 IV = 1 U = 8 |
||||
| Total Healthy n = 107 |
18–87 (58) | M = 43 F = 64 |
Total Benign n = 74 |
23–83 (56) | M = 29 F = 45 |
C = 32 P = 25 O = 17 |
Total PDAC n = 160 |
42–91 (69) | M = 75 F = 85 |
I = 4 II = 33 III = 16 IV = 44 U = 63 |
|
Validation Set | ||||||||||
| Healthy | Benign | PDAC | ||||||||
| Source | Age Range (Median) | Gender | Source | Age Range (Median) | Gender | Dx | Source | Age Range (Median) | Gender | Stage |
| UPCI n = 46 |
20–76 (51) | M = 34 F = 12 |
UAB n = 54 |
43–85 (57) | M = 35 F = 19 |
C = 16 P = 19 O = 19 |
UAB n = 55 |
44–91 (67) | M = 36 F = 29 |
I = 0 II = 6 III = 4 IV = 6 U = 39 |
| FCCC n = 37 |
37–84 (65) | M = 6 F = 31 |
NUH n = 16 |
35–86 (75) | M = 7 F = 9 |
C = 2 P = 8 O = 6 |
SKCC n = 52 |
45–83 (65) | M = 22 F = 30 |
I = 0 II = 16 III = 10 IV = 2 U = 24 |
| NUH n = 27 |
34–87 (54) | M = 5 F = 22 |
NUH n = 46 |
42–92 (74) | M = 22 F = 24 |
I = 3 II = 14 III = 0 IV = 29 U = 0 |
||||
| GOG n = 10 |
39–56 (51) | M = 0 F = 10 |
UPCI n = 20 |
29–82 (64) | M = 8 F = 12 |
I = 1 II = 1 III = 6 IV = 4 U = 8 |
||||
| Total Healthy n = 120 |
20–87 (54) | M = 45 F = 75 |
Total Benign n = 70 |
35–86 (66) | M = 42 F = 28 |
C = 18 P = 27 O = 25 |
Total PDAC n = 173 |
29–92 (68) | M = 88 F = 95 |
I = 4 II = 37 III = 20 IV = 41 U = 71 |
|
Non-PDAC Cancer Set | ||||||||||
| Colon | Lung | Breast | ||||||||
| Source | Age Range (Median) | Gender | Source | Age Range (Median) | Gender | Dx | Source | Age Range (Median) | Gender | Dx |
| UPCI n = 33 |
47–89 (64.5) | M = 18 F = 15 |
UPCI n = 62 |
46–99 (68) | M = 30 F = 32 |
Ad = 33 Sq = 29 |
Duke n = 108 |
52–82 (63) | F = 108 | IDC = 108 |
Sources: UPCI – University of Pittsburgh Cancer Institute; FCCC – Fox Chase Cancer Center; NUH – NorthShore University HealthSystems; GOG – Gynecological Oncology Group; UAB – University of Alabama-Birmingham; SKCC – Sloan-Kettering Cancer Center; Duke – Duke University; Benign Dx: C – Benign Cyst; P – Pancreatitis;O – Other benign neoplasm; PDAC Dx: U – stage unknown; Ad – adenocarcinoma; Sq – squamous cell carcinoma; IDC – invasive ductal carcinoma
Sources of bead-based immunoassays
The xMAP™ bead-based technology (Luminex Corp., Austin, TX) permits multiplexed analysis of several analytes in one sample. Eighty-three bead-based xMAP™ immunoassays for a diverse set of serum biomarkers were utilized in this study (Table 2). The immunoassays were either obtained from commercial suppliers or developed by the UPCI Luminex Core Facility as described previously 22. Overall, 14 different multiplexed panels were used. For the UPCI core-developed assays, the intra-assay variability of each assay was 3.5–5% and inter-assay variability was 11–15%. Additional quality control data for each core-developed assay, including correlation with commercial ELISA can be found on the UPCI Luminex Core Facility website. All assays were performed at UPCI.
Table 2.
Complete List of Multiplexed Biomarker Assays
| Biological Groups | Markers |
|---|---|
| Tumor Markers | Alpha-fetoprotein (AFP), CA 19-9, CA 125, CA 15-3, CA72-4, CEA |
| Hormones | adrenocorticotropic hormone (ACTH), follicle stimulating hormone (FSH), Growth hormone (GH), Insulin, luteinizing hormone (LH), Prolactin (PRL), parathyroid hormone (PTH), thyroid stimulating hormone (TSH), Pancreatic Polypeptide (PP), Peptide YY (PYY) (total) |
| Apoptotic Factors | Cytokeratin 19 (Cyfra 21-1), DR5, sFas, sFasL |
| Cell Adhesion | ICAM-1, VCAM-1 |
| Proteases/Inhibitors | Kallikrein 10, MMP-2, 3, 9, TIMP-1-4 |
| Cytokines/Chemokines/Receptors | CD40L (TRAP), Eotaxin-1, Fractalkine, IFNγ, IL-10, IL-12p70, IL-13, IL- 1b, IL-1Rα, IL-2, IL-2R, IL-4, IL-5, IL-6, IL-6R, IL-7, IL-8, IP-10, Macrophage inhibitory factor (MIF), MIP-1b, TGFα, TNFα, TNF-RI, TNF- RII |
| Growth/Angiogenesis Factors/Receptors | Angiostatin, EGFR, Endostatin, ErbB2, GM-CSF, IGFBP-1, Thrombospondin |
| Adipokines | Adiponectin, Leptin |
| Apolipoproteins | ApoAI, ApoAII, ApoB, ApoCII, ApoCIII, ApoE |
| Other | CRP, Ghrelin (active), Gastric inhibitory polypeptide (GIP) (total), Glucagon like peptide 1(GLP-1) (active), HE4, Mesothelin, Osteocalcin (OC), osteoprotegerin (OPG), Osteopontin (OPN), Serum amyloid A (SAA), Serum amyloid P (SAP), Transglutaminase II (TG II), total Plasminogen activator inhibitor 1 (tPAI 1), myeloperoxidase (MPO) |
Multiplex biomarker analysis
The bead-based multiplex serum assays were performed in 96-well microplate format. All purchased assays were performed according to appropriate manufacturer’s protocols. In-house assays, sample analysis, and curve-fitting were performed as previously described 22. All biomarker data was normalized prior to statistical analysis according to a scaling procedure developed by our group to specifically account for variation acquired throughout repeated experiments. A complete description of this procedure is provided in the Supplemental Material.
Statistical analysis of data
Descriptive statistics for serum concentrations of each of the tested biomarkers were calculated for each subject group using GraphPad Prism software (GraphPad Software, Inc., San Diego, CA). A 1-way Analysis of Variance (ANOVA) with Tukey’s multiple comparison test was used to determine significance of any observed differences in serum biomarker concentrations between the groups. The minimum level of significance was taken as p<0.05. The False Discovery Rate (FDR) was controlled at 5% according to the method described by Benjamini and Hochberg23. Briefly, the individual p-values for each biomarker comparison were ranked from most to least significant. The ranked, unadjusted p-values were then compared to the statistic i*q/m, where i is the p-value rank, q is the FDR (0.05), and m is the total number of biomarker comparisons tested.
Multivariate analysis
All development of statistical models for distinguishing cases from controls was restricted to the training set until one panel and one model of combining the candidate biomarkers in the panel were selected. A Metropolis algorithm with Monte Carlo simulation (MMC) was utilized for analysis of the data as previously described 22. Using this algorithm, all possible panels consisting of 2, 3 and 4 biomarkers were evaluated for SN at 90% SP in the training set. For each panel size, the 500 panels with the best SN at 95% SP on the full data set we re-estimated the SN with cross-validation. For cross-validation, 20% of subjects were randomly excluded from the data set and the rest used as at training set to build the optimal Scoring Function (SF). The resultant model was applied to the excluded subjects, and this process was repeated 400 times which was sufficient to obtain a smooth averaged ROC curve. For each comparison (PDAC vs. Healthy, PDAC vs. Benign), a single multimarker panel demonstrating the best SN at 90% SP as determined from the ROC curves was validated in an independent, blinded validation set. Following the classification of each sample in the validation set, the samples were unblinded and the diagnosis assigned by the MMC algorithm was compared to the actual diagnosis for calculation of SN/SP. The top performing multimarker panels for the discrimination of PDAC vs. Healthy were further evaluated for cancer selectivity in patients diagnosed with colon, lung, and breast cancer.
Results
Univariate analysis of biomarker levels in patients diagnosed with PDAC, benign pancreatic disease, and healthy controls
Serum levels of each biomarker were compared between the PDAC, Benign, and Healthy subject groups and the presented data reflect the inclusion of all subjects, after unblinding, in order to increase the statistical power of comparisons. Of the 83 biomarkers evaluated, 42 were found to differ significantly between the PDAC patients and the Healthy and Benign groups (Table 3). Of these 42 biomarkers, 33 were found to be increased in the PDAC group in comparison to the Healthy group, while 9 were found to be decreased. In the comparison between the Benign and PDAC patient groups, 15 biomarkers were observed at higher concentrations in the PDAC group while 5 biomarkers were found in lower levels. With the exception of CEA and TIMP-3 all observed trends in biomarker levels were consistent between the two comparisons.
Table 3.
Circulating Levels of Significant Biomarkers in Patients Diagnosed with Pancreatic Cancer, Benign Pancreatic Disease, and Healthy Control Individuals
| Class | Biomarker | Healthy | Benign | PDAC1 | |||
|---|---|---|---|---|---|---|---|
| Mean | Mean | Mean | vs. Healthy | vs. Benign | |||
| pg/ml | pg/ml | pg/ml | p-value2 (Trend) | ||||
| Tumor Markers | CA 19-9 | 5.424 | 2.608 | 56.04 | < 0.001 (I) | < 0.001 (I) | |
| CA-125 | 27.38 | 26.94 | 1073 | < 0.001 (I) | ns | ||
| CEA | 33271 | 621444 | 474737 | < 0.01 (I) | < 0.05 (D) | ||
| Hormones | GH | 1932 | 1167 | 2398 | < 0.001 (I) | < 0.001 (I) | |
| Prolactin4 | 618.1 | 2366 | 1410 | < 0.01 (I) | ns | ||
| PTH | 27.22 | 43.48 | 38.6 | < 0.001 (I) | ns | ||
| Apoptosis Markers | Cytokeratin 19 | 20.16 | 122.8 | 7579 | < 0.01 (I) | ns | |
| sFas | 8877 | 9273 | 13621 | < 0.001 (I) | < 0.05 (I) | ||
| sFasL | 200.2 | 190.1 | 162 | < 0.001 (D) | ns | ||
| Adhesion Mediators | MMP-24 | 37770 | 38260 | 44830 | < 0.05 (I) | ns | |
| ICAM-13 | 177.8 | 535.1 | 1011 | < 0.001 (I) | < 0.05 (I) | ||
| TIMP-13 | 116.2 | 184 | 331.5 | < 0.001 (I) | < 0.001 (I) | ||
| TIMP-23 | 9277 | 14680 | 12400 | < 0.01 (I) | ns | ||
| TIMP-3 | 707186 | 3756000 | 823150 | < 0.01 (I) | < 0.01 | (D) | |
| TIMP-4 | 77019 | 87711 | 106717 | < 0.001 (I) | < 0.001 (I) | ||
| Cytokines/Chemokines/Receptors | IL-2R | 1124 | 1938 | 3214 | < 0.001 (I) | ns | |
| IL-8 | 10.52 | 16.73 | 37.68 | < 0.001 (I) | ns | ||
| IP-10 | 189.5 | 187.6 | 230.3 | < 0.001 (I) | < 0.05 (I) | ||
| MPO3 | 289 | 481.7 | 501.7 | < 0.001 (I) | ns | ||
| TNF-a | 6.135 | 7.603 | 7.141 | < 0.05 (I) | ns | ||
| TNF-RI | 6093 | 8102 | 10604 | < 0.001 (I) | < 0.05 (I) | ||
| TNF-RII | 4255 | 5309 | 9016 | < 0.001 (I) | ns | ||
| Growth/Angiogenesis Factors | Angiostatin3 | 6604000 | 6005000 | 6037000 | < 0.01 (D) | ns | |
| EGFR | 103980 | 100387 | 89214 | < 0.001 (D) | ns | ||
| Endostatin | 146542 | 169267 | 195388 | < 0.001 (I) | < 0.05 (I) | ||
| ErbB2 | 11018 | 12061 | 16458 | < 0.001 (I) | ns | ||
| IGFBP-14 | 16040 | 39060 | 50730 | < 0.001 (I) | ns | ||
| Thrombospondin4 | 16050 | 16730 | 14070 | < 0.01 (D) | ns | ||
| Adipokines | Adiponectin | 78930 | 72840 | 100400 | < 0.01 (D) | ns | |
| Leptin | 5466 | 3803 | 3099 | < 0.05 (D) | ns | ||
| Apolipoproteins | ApoAI | 226872 | 211750 | 103597 | < 0.001 (D) | < 0.001 (D) | |
| ApoAII | 3226 | 2596 | 2100 | < 0.001 (D) | < 0.01 (D) | ||
| ApoCIII | 231.3 | 223.3 | 195.6 | < 0.001 (D) | ns | ||
| ApoE | 63 | 66.48 | 95.88 | < 0.001 (I) | < 0.05 (I) | ||
| Bone Regulation | OC | 5622 | 7366 | 4869 | < 0.001 (D) | < 0.001 (D) | |
| OPG | 441.7 | 719.5 | 824.1 | < 0.001 (I) | < 0.01 (I) | ||
| OPN | 1483 | 6520 | 16151 | < 0.001 (I) | < 0.001 (I) | ||
| Other | CRP3 | 16450 | 67870 | 120500 | < 0.001 (I) | < 0.001 (I) | |
| GLP-1 (active) | 18.59 | 17.91 | 24.07 | < 0.05 (I) | ns | ||
| HE4 | 36257 | 20677 | 51142 | < 0.001 (I) | < 0.05 (I) | ||
| SAA3 | 100.2 | 1012 | 2769 | < 0.001 (I) | < 0.001 (I) | ||
| Tg II | 24674 | 48184 | 62525 | < 0.05 (I) | ns | ||
Pancreatic ductal adenocarcinoma;
significance determined by 1-way ANOVA with Tukey’s multiple comparison test;
ug/ml;
ng/ml; ns-not significant; Trend: (I) – increased in PDAC, (D) – decreased in PDAC
We noted a discrepancy in the age distribution between the Healthy, Benign, and PDAC subjects with the Healthy and Benign groups tending to be younger (Table 1). To further assess this discrepancy we conducted an analysis of age-related biomarker levels within the Healthy and Benign subjects. None of the biomarkers were differed significantly between the age-defined subgroups (cutoff of 55 years) of Benign subjects. Significant differences were identified between subgroups of healthy controls defined as ≥55 years of age and <55 years of age for endostatin, LH, MIF, and TNF-RI (Supplemental Table S1, Figure S1).
Evaluation of Source Bias
To analyze bias associated with variations in sample collection procedures at different centers, circulating levels of the 12 most informative biomarkers: CA 19-9, OPG, OPN, ICAM-1, TIMP-1-4, SAA, ApoA1, TIMP-2, and CRP were analyzed in serum samples obtained from healthy individuals by 1-Way ANOVA with Tukey’s Multiple Comparison Test (Supplementary Figure S2). Only CRP was significant in this analysis, however the magnitudes of the biases (6–7%) were small compared to the differences between cancers and control subjects (86%). All observed trends in biomarker differences observed in the univariate analysis of PDAC vs. Healthy were consistently present throughout the sampling sites. We concluded from this analysis that source bias was a minimal factor in our analysis.
Multivariate Analysis of Biomarker Levels
The PDAC, Benign, and Healthy subject groups were each split into two sets termed training and validation on a random basis (Table 1). All development of multimarker panels using the MMC algorithm was restricted to the training sets. Our analysis identified the highest performing 2, 3, and 4-biomarker panels trained on either the PDAC (cases) vs. Healthy (controls) groups or the PDAC (cases) vs. Benign (controls) groups. The 21 best 3-biomarker panels for each comparison are shown in Table 4 along with the performance of CA19-9 alone. Each of these panels outperformed all possible 2-biomarker combinations while the addition of a fourth biomarker did not improve performance (Supplementary Table S2). Seven of the panels were identified in both comparisons and these are designated by italics in Table 4. One optimal panel was chosen for each comparison which demonstrated the highest SN at 90% SP. The performance of each of these panels in the training set was compared to CA 19-9 alone by ROC analysis (Figure 1A, B). In the comparison of PDAC vs. Healthy, the selected combination of CA19-9, ICAM-1 and OPG demonstrated improved performance over CA 19-9 alone in terms of AUC (0.93 vs. 0.83) and SN (87.5% vs. 57.2%) at 90% SP. In the comparison of PDAC vs. Benign, the selected combination of CA 19-9, CEA and TIMP-1 demonstrated an improvement over CA 19-9 alone in terms of AUC (0.86 vs. 0.82) and SN (75.8% vs. 56.4%) at 90% SP.
Table 4.
Top Performing Biomarker Panels Identified by MMC Algorithm Applied to the Training Set
| PDAC vs. Healthy | PDAC vs. Benign | ||||||
|---|---|---|---|---|---|---|---|
| %SN at 90% SP | %SN at 90% SP | ||||||
| CA 19-9 | 57.2 | CA 19-9 | 56.4 | ||||
| CA 19-9 | ICAM-1 | OPG | 88.1 | CA 19-9 | CEA | TIMP-1 | 75.8 |
| CA 19-9 | TIMP-1 | OPG | 87.5 | CA 19-9 | TIMP-3 | TIMP-4 | 75.6 |
| CA 19-9 | OPN | TIMP-1 | 86.9 | CA 19-9 | TIMP-4 | CRP | 74.4 |
| CA 19-9 | ICAM-1 | TIMP-1 | 86.3 | CA 19-9 | SAA | ApoAI | 73.1 |
| CA 19-9 | CA-125 | TIMP-1 | 85 | CA 19-9 | SAA | CRP | 72.5 |
| CA 19-9 | ICAM-1 | OPN | 85 | CA 19-9 | Tg II | TIMP-4 | 72.5 |
| CA 19-9 | SAA | TIMP-1 | 84.4 | CA 19-9 | ApoAI | TIMP-3 | 71.9 |
| CA 19-9 | CEA | TIMP-1 | 84.4 | CA 19-9 | TIMP-3 | CRP | 71.9 |
| CA 19-9 | TIMP-1 | CRP | 83.8 | CA 19-9 | SAA | CA-125 | 71.3 |
| CA 19-9 | TIMP-1 | TIMP-2 | 83.8 | CA 19-9 | CEA | TIMP-4 | 71.3 |
| CA 19-9 | Tg II | TIMP-1 | 83.8 | CA 19-9 | ICAM-1 | SAA | 71.3 |
| CA 19-9 | OPG | CRP | 83.1 | CA 19-9 | TIMP-1 | TIMP-4 | 71.3 |
| CA 19-9 | TIMP-1 | TIMP-4 | 82.5 | CA 19-9 | CA-125 | TIMP-1 | 70.6 |
| CA 19-9 | ApoAI | TIMP-1 | 82.5 | CA 19-9 | CEA | SAA | 70.6 |
| CA 19-9 | OPN | CRP | 82.5 | CA 19-9 | SAA | TIMP-1 | 70.6 |
| CA 19-9 | TIMP-1 | TIMP-3 | 81.9 | CA 19-9 | OPG | CRP | 70.6 |
| CA 19-9 | ICAM-1 | SAA | 81.3 | CA 19-9 | SAA | TIMP-4 | 70.6 |
| CA 19-9 | ICAM-1 | Apo AI | 80.6 | CA 19-9 | ICAM-1 | TIMP-1 | 70 |
| CA 19-9 | ICAM-1 | CRP | 80 | CA 19-9 | TIMP-2 | TIMP-4 | 70 |
| CA 19-9 | ICAM-1 | Tg II | 78.8 | CA 19-9 | SAA | TIMP-3 | 70 |
| CA 19-9 | ICAM-1 | TIMP-4 | 77.5 | CA 19-9 | ApoAI | TIMP-4 | 69.4 |
Panels listed in italics identified in both comparisons, panels listed in bold selected for independent validation
Figure 1. Receiver operator characteristic curves (ROC) for diagnosis of PDAC vs. Healthy controls and Benign cases.
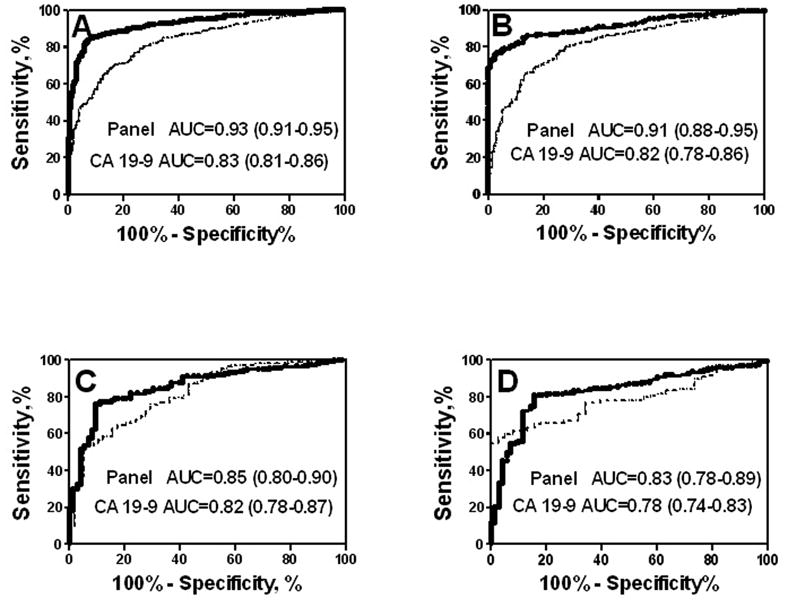
A,B, The diagnostic performance of the CA 19-9, ICAM-1, OPG combination (solid line) and CA 19-9 alone (dotted line) for the discrimination of PDAC vs. Healthy in the training set (A) and in the independent validation set (B). C,D, The diagnostic performance of the CA 19-9, CEA, TIMP-1 combination (solid line) and CA 19-9 alone (dotted line) for the discrimination of PDAC vs. Benign disease in the training set (A) and in an independent validation set (B). Areas under curve (AUC) with 95% CI are presented.
Next, the two optimal panels were validated in an independent blinded validation set (Table 1) containing Healthy, Cancer, and Benign samples (Figure 1C, D). Each validation sample was diagnosed as cancer or control (non-cancer) using the scoring function (SF) assigned to each biomarker panel following the MMC training analysis, and each diagnosis was compared with the clinical diagnosis after unblinding. The diagnostic performance of each panel in the validation set was compared to CA 19-9 alone by ROC analysis (Figure 1C, D). In the independent validation set, the combination of CA19-9, ICAM-1 and OPG offered SN=78% at 94.1% SP (AUC=0.91) for the discrimination of PDAC vs. Healthy compared to SN=51.4% at 90% SP (AUC=0.82) for CA 19-9 alone. In the comparison of PDAC vs. Benign, the combination of CA 19-9, CEA and TIMP-1 demonstrated an improvement over CA 19-9 alone in terms of AUC (0.83 vs. 0.78) and SN/SP (71.2%/88.6% vs. 52.1%/90.2%).
Cancer Selectivity of Multimarker Panels for Pancreatic Cancer
We utilized the MMC algorithm to evaluate the cancer specific selectivity of the biomarker panels identified in the multivariate analysis of PDAC vs. Healthy (Table 4). Each panel was applied to several groups of sera obtained from patients diagnosed with colon (n=33), lung (n=62), and breast (n=108) cancer and the percentage of each group diagnosed as non-PDAC was determined using the MMC algorithm (Table 5). In this analysis, the validated panel of CA 19-9, ICAM-1, and OPG classified 97% of colon cancer sera, 97% of lung cancer sera, and 100% of breast cancer sera as non-PDAC. Several additional panels performed equally well in this analysis.
Table 5.
Cancer Selectivity of Multimarker Panels for PDAC (%)
| Panel | Colon N=33 | Lung N=62 | Breast N=108 | ||
|---|---|---|---|---|---|
| CA 19-9 | ICAM-1 | OPG | 97.0 | 97.0 | 100 |
| CA 19-9 | TIMP-1 | OPG | 97.0 | 97.0 | 100 |
| CA 19-9 | OPN | TIMP-1 | 97.0 | 97.0 | 100 |
| CA 19-9 | ICAM-1 | TIMP-1 | 97.0 | 97.0 | 100 |
Values List are % classified as Non-PDAC
Discussion
In the present study, we identify several 3-biomarker panels offering high SN/SP and significant improvement over CA 19-9 alone for the discrimination of PDAC from healthy controls and benign subjects. To the best of our knowledge, these results represent the most advanced validated biomarker discovery effort aimed at the development of improved screening methodologies for the detection of pancreatic cancer. Since the incidence of pancreatic cancer in the general population (~1% lifetime risk) is too low to warrant screening, strategies are being investigated to define patient cohorts in which the positive predictive value for early-stage pancreatic cancers and advanced precursor lesions is high enough to justify more costly and invasive testing 24. Therefore, our study intended to develop a panel of biomarkers that can be used to screen populations at an increased risk for the development of pancreatic cancer.
At present, high risk populations are not readily available for the purpose of pancreatic cancer screening. Pancreatic cancer-prone families are the most widely accepted population of this type to date, but only account for 5 to 10% of all pancreatic adenocarcinomas. Furthermore, the genetic factors underlying this predisposition are uncharacterized in the majority of these families. As it would take many years to follow a cohort of these patients to determine which unaffected individuals in these familial pancreatic cancer kindreds would develop PDAC, it is not practical to use this population for biomarker discovery. However, many centers are actively investigating risk stratification models that will take into account genetic factors along with epidemiological information, such as smoking and alcohol use, or clinical history including diabetic status or history of gastric ulcer. This should provide appropriate populations with a high enough incidence of pancreatic adenocarcinoma to warrant surveillance.
The multimarker panels identified in our analysis were highly discriminatory for PDAC vs. Healthy subjects demonstrating sensitivities ranging from 77–88% with 90% SP and a lower discriminatory power of 70–76% with 90% SP for PDAC vs. Benign. The optimal panel identified in the comparison of PDAC vs. Healthy comprised of CA 19-9, ICAM-1 and OPG demonstrated significant improvement over CA 19-9 by ROC analysis, whereas the best panel for discrimination of Benign from PDAC did not offer a substantial improvement in terms of SN over CA 19-9 at a level of SP above 80% (Figure 1). The AUC values we observed for CA 19-9 were within the reported range (0.72–0.84) of several recent studies25–26. The panel of CA 19-9, ICAM-1 and OPG also demonstrated a high level of cancer selectivity when applied to colon, lung, and breast cancers. The relative performance of these biomarker panels coupled with the small number of analytes required to achieve that performance make them attractive candidates in the development of early detection strategies.
In the course of our evaluation, we have identified number of proteins that differ significantly in the sera of patients diagnosed with PDAC and healthy controls, and many of these were also significant in comparison to the Benign group with considerable reproducibility in biomarker trends across the multiple sampling sites. To the best of our knowledge, 19 of the observed associations between serum biomarker levels and PDAC have not been described previously: GH, PRL, PTH, sFas, sFasL, MMP-2, TIMP 2-4, MPO, EGFR, ApoAI-II, ApoCIII, OC, GLP-1, HE4, and TGII. Although recent reports have described significant associations between serum levels of OPG 27 and pancreatic cancer, to the best of our knowledge, our report is the first to characterize its diagnostic capacity. The significant biomarkers include representatives from a diverse set of biological families, particularly proteins with functions in such critical aspects of tumor development as growth, angiogenesis, metastasis, inflammation, etc., and encompass an array of factors likely to originate from the developing tumor, the tumor microenvironment and components of the systemic host response to the malignancy.
In the current study, PDAC was associated with circulating alterations of a number of known mediators of inflammatory processes and acute phase reactants. The relationship between tumorigenesis and inflammation has become a central theme in anticancer research and is the focus of increasing interest within the setting of pancreatic cancer. Malignant transformation can be closely associated with chronic infection and inflammation, while elevated levels of pro-inflammatory proteins could play a role as tumor promoters 28. It has also been clear for some time now that a number of pro-inflammatory gene products including acute-phase reactants can also be produced by components or tumor microenvironment and tumor cells themselves to further mediate tumor growth 29. For example, elevated circulating levels of SAA could reflect not only hepatic synthesis as part of the acute-phase response, but also increased release of these proteins by cancer cells, and a possible role for SAA in tumor growth, metastasis, and neovascularization has been investigated 30–31. Therefore, these pro-inflammatory proteins could potentially be utilized as cancer biomarkers. In fact, it has been demonstrated that serum SAA levels are elevated in a broad spectrum of neoplastic diseases 5, 32 suggesting that it could act at least as a non-specific tumor marker. The combination of CRP, another acute-phase reactant, and sIFNα/βR was demonstrated to diagnose gastrointestinal and hepatobiliary-pancreatic cancer with a SN/SP of 94.6/88 33. The production of pro-inflammatory cytokines by tumor and stromal cells, regulated by NF-kB, has been observed to mediate tumorigenic effects in the pancreas as part of a characteristic desmosplastic reaction 34. We observed altered levels of the NF-kB responsive cytokines TNFα and IL-8 which have been specifically shown to inhibit apoptosis and increase invasiveness of pancreatic cancer cells, respectively 35–36. Also notably altered was the ROS-mediating enzyme, MPO. MPO has demonstrated involvement in the generation of DNA strand breaks, sister chromatid exchanges, mutations, and the formation of DNA adducts 37, and is associated with smoking, a known risk factor of pancreatic cancer 38.
Our findings also support several hypotheses regarding the role of specialized pathways related to obesity, bone homeostasis, and tissue remodeling, in pancreatic cancer. These findings include alterations in number of apolipoproteins and adipokines, modulators of lipid and insulin metabolism. ApoA1 may represent an emerging biomarker of malignancy as circulating levels of ApoA1 have recently been linked to several cancer types including pancreatic 39. The adipokines, Adiponectin and Leptin are currently under intense scrutiny stemming from links to obesity, inflammation and malignancy 40. We observed altered serum levels of OPN, a biomarker previously associated with pancreatic cancer 11, and several other bone related factors, OC and OPG. OPG is a secreted member of the tumor necrosis factor receptor superfamily, and altered serum levels of OPG have been associated with several malignancies including colorectal cancer, pancreatic cancer, liver metastases, multiple myeloma, Hodgkin’s disease, and non-Hodgkin’s lymphoma 27. We report dysregulation of several metastasis-related proteins in PDAC. The MMPs and their natural inhibitors, TIMPs, have well-described tumorigenic roles and our observations regarding MMP-2 and TIMPs 1-4 in pancreatic cancer patients are consistent with previous findings 41. The cellular adhesion mediator ICAM-1 has been previously linked to the development of PDAC 42 and was utilized as a part of multimarker panel for the classification of PDAC from healthy controls 19. The expression of ICAM-1 is associated with PDAC cell sensitivity to T-cell-based immunotherapy in vitro 43, and prognostic significance of preoperative sICAM-1 levels in several cancers has been demonstrated 44–46. Correlation of TGII with metastatic properties of several cancers has been suggested 47–48, and its role as a tumor marker in the development and progression of pancreatic cancer has been well documented 49–50. We also observed the dysregulation of a number of growth factors, receptors and mediators of angiogenesis including EGFR, ErbB2, Angiostatin, Endostatin, Thrombospondin, and IGFBP-1.
In summary, an extensive analysis of circulating biomarkers in patients diagnosed with PDAC and benign pancreatic conditions resulted in a robust profile of alterations in biomarkers in PDAC patients, offering improved insights into the network of factors involved in the process of pancreatic tumorigenesis. A number of the alterations we identify are novel with regard to associations with PDAC as is the expanded use of several previously characterized serum biomarkers for diagnostic purposes. Although the ideal biomarker test would recognize premalignant conditions, to the best of our knowledge, such requisite retrospective samples are presently not available for biomarker discovery. Therefore, the current study was guided by the assumption that a subset of those biomarkers demonstrating differential expression in developed cancer would also be altered in premalignant conditions. Thus, our analysis of biomarker alterations present in serum at the time of diagnosis should pave the way for the subsequent identification of biomarkers of preneoplastic disease. Additionally, biomarker panels discriminating PDAC from benign disease may offer a high level of clinical utility in combination with conventional imaging modalities to provide a diagnostic role as opposed to the aforementioned screening application. This study presents proof-of-principle of the utility of a multiplexed evaluation of circulating biomarkers for the identification and validation of multimarker panels with high classification power for PDAC. Further studies employing this type of approach may result in the identification of more robust panels for both screening and diagnosis of PDAC.
These findings represent an evaluation of biomarkers potentially related to pancreatic cancer and do not promote the use of any individual biomarker considered herein for diagnostic purposes. Moreover, while the nature of our investigation does not permit the identification of specific mechanistic links between any particular biomarker and the development of pancreatic cancer, our results do provide a sound basis for subsequent targeted analyses of pancreatic cancer biomarkers.
Statement of Translational Relevance.
Specific challenges associated with pancreatic cancer including ubiquitous symptomatic presentation, deep anatomical location, and aggressive etiology, have greatly hindered efforts to combat the disease. Although the low incidence of the disease in the general population renders population-based screening impractical, screening could greatly improve survival in appropriately targeted high-risk populations. The current absence of reliable biomarker testing for pancreatic cancer mandates the development of novel strategies for identifying and characterizing additional biomarkers. The evaluation of serum biomarker levels in patients diagnosed with pancreatic cancer and a spectrum of benign pancreatic conditions presented here provides compelling evidence for the emerging role of blood-based screening in the clinical management of this disease. These findings not only include the identification of multimarker panels capable of discriminating pancreatic cancer from benign conditions and healthy controls with high sensitivity and specificity, but also offer improved insight into the complex network of factors involved in pancreatic tumorigenesis.
Supplementary Material
Acknowledgments
This work was supported by NIH grants: U01CA117452 (EDRN), RO1 CA098642, R01 CA108990, P50 CA083639, CA086381, CA105009, UPCI Hillman Fellows Award, and The Frieda G. and Saul F. Shapira BRCA Cancer Research Program Award (AEL).
List of Abbreviations
- ACTH
adrenocorticotropic hormone
- AFP
alpha-fetoprotein
- CRP
C-reactive protein
- FSH
follicle stimulating hormone
- GH
growth hormone
- GIP
gastric inhibitory polypeptide
- GLP-1
glucagon-like peptide
- GM-CSF
granulocyte macrophage colony stimulating factor
- ICAM-1
inter-cellular adhesion molecule 1
- IGFBP-1
insulin-like growth factor binding protein 1
- LH
luteinizing hormone
- MIF
macrophage inhibitory factor
- MMC
Metropolic algorithm with Monte Carlo simulation
- MMP
matrix metalloproteinase
- MPO
myeloperoxidase
- OC
osteocalcin
- OPG
osteoprotegerin
- OPN
osteopontin
- PDAC
pancreatic ductal adenocarcinoma
- PP
pancreatic polypeptide
- PRL
Prolactin
- PTH
parathyroid hormone
- PYY
peptide YY
- ROC AUC
receiver operator characteristic area under curve
- SAA
serum amyloid A
- SAP
serum amyloid P
- SN
sensitivity
- SP
specificity
- TGII
tissue transglutaminase (transglutaminase II)
- TIMP
tissue inhibitor of metalloproteinases
- tPAI-1
tissue plasminogen activator inhibitor 1
- TSH
thyroid stimulating hormone
- VCAM-1
vascular cell adhesion molecule 1
Contributor Information
Randall E. Brand, Email: reb53@pitt.edu.
Brian M. Nolen, Email: nolanb@upmc.edu.
Herbert J. Zeh, Email: zehxhx@upmc.edu.
Peter J. Allen, Email: allenp@mskcc.org.
Mohamad A. Eloubeidi, Email: Eloubeidi@uab.edu.
Michael Goldberg, Email: mgoldberg@northshore.org.
Eric Elton, Email: eelton@northshore.org.
Juan P. Arnoletti, Email: parnolet@uab.edu.
John D. Christein, Email: jdc16@uab.edu.
Selwyn M. Vickers, Email: Vickers@umn.edu.
Christopher J. Langmead, Email: cjl+@cs.cmu.edu.
Douglas P. Landsittel, Email: landsitteldp@upmc.edu.
David C. Whitcomb, Email: whitcomb@pitt.edu.
William E. Grizzle, Email: wgrizzle@uab.edu.
Anna E. Lokshin, Email: lokshina@upmc.edu.
References
- 1.SEER Cancer Statistics Review. National Cancer Institute; 1975–2006. (Accessed at http://seer.cancer.gov/csr/1975_2006/.) [Google Scholar]
- 2.Grantzdorffer I, Carl-McGrath S, Ebert MP, Rocken C. Proteomics of pancreaticcancer. Pancreas. 2008;36:329–36. doi: 10.1097/MPA.0b013e31815cc452. [DOI] [PubMed] [Google Scholar]
- 3.Michaud DS. Epidemiology of pancreatic cancer. Minerva Chir. 2004;59:99–111. [PubMed] [Google Scholar]
- 4.Sohn TA, Lillemoe KD. Surgical palliation of pancreatic cancer. Adv Surg. 2000;34:249–71. [PubMed] [Google Scholar]
- 5.Pannala R, Basu A, Petersen GM, Chari ST. New-onset diabetes: a potential clue to the early diagnosis of pancreatic cancer. Lancet Oncol. 2009;10:88–95. doi: 10.1016/S1470-2045(08)70337-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larghi A, Verna EC, Lecca PG, Costamagna G. Screening for pancreatic cancer in high-risk individuals: a call for endoscopic ultrasound. Clin Cancer Res. 2009;15:1907–14. doi: 10.1158/1078-0432.CCR-08-1966. [DOI] [PubMed] [Google Scholar]
- 7.Morganti AG, Valentini V, Macchia G, et al. Adjuvant radiotherapy in resectable pancreatic carcinoma. Eur J Surg Oncol. 2002;28:523–30. doi: 10.1053/ejso.2002.1289. [DOI] [PubMed] [Google Scholar]
- 8.Brand RE, Matamoros A. Imaging techniques in the evaluation of adenocarcinoma of the pancreas. Dig Dis Sci. 1998;16:242–52. doi: 10.1159/000016872. [DOI] [PubMed] [Google Scholar]
- 9.Hanbidge AE. Cancer of the pancreas: the best image for early detection--CT, MRI, PET or US? Can J Gastroenterol. 2002;16:101–5. doi: 10.1155/2002/184370. [DOI] [PubMed] [Google Scholar]
- 10.Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol. 2007;33:266–70. doi: 10.1016/j.ejso.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Koopmann J, Rosenzweig CN, Zhang Z, et al. Serum markers in patients with resectable pancreatic adenocarcinoma: macrophage inhibitory cytokine 1 versus CA19-9. Clin Cancer Res. 2006;12:442–6. doi: 10.1158/1078-0432.CCR-05-0564. [DOI] [PubMed] [Google Scholar]
- 12.Locker GY, Hamilton S, Harris J, et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol. 2006;24:5313–27. doi: 10.1200/JCO.2006.08.2644. [DOI] [PubMed] [Google Scholar]
- 13.Argani P, Iacobuzio-Donahue C, Ryu B, et al. Mesothelin is overexpressed in the vast majority of ductal adenocarcinomas of the pancreas: identification of a new pancreatic cancer marker by serial analysis of gene expression (SAGE) Clin Cancer Res. 2001;7:3862–8. [PubMed] [Google Scholar]
- 14.Eskelinen M, Haglund U. Developments in serologic detection of human pancreatic adenocarcinoma. Scand J Gastroenterol. 1999;34:833–44. doi: 10.1080/003655299750025273. [DOI] [PubMed] [Google Scholar]
- 15.Hustinx SR, Cao D, Maitra A, et al. Differentially expressed genes in pancreatic ductal adenocarcinomas identified through serial analysis of gene expression. Cancer Biol Ther. 2004;3:1254–61. doi: 10.4161/cbt.3.12.1238. [DOI] [PubMed] [Google Scholar]
- 16.Slesak B, Harlozinska-Szmyrka A, Knast W, Sedlaczek P, van Dalen A, Einarsson R. Tissue polypeptide specific antigen (TPS), a marker for differentiation between pancreatic carcinoma and chronic pancreatitis. A comparative study with CA 19-9. Cancer. 2000;89:83–8. doi: 10.1002/1097-0142(20000701)89:1<83::aid-cncr12>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 17.Zhou W, Sokoll LJ, Bruzek DJ, et al. Identifying markers for pancreatic cancer by gene expression analysis. Cancer Epidemiol Biomarkers Prev. 1998;7:109–12. [PubMed] [Google Scholar]
- 18.Moniaux N, Chakraborty S, Yalniz M, et al. Early diagnosis of pancreatic cancer: neutrophil gelatinase-associated lipocalin as a marker of pancreatic intraepithelial neoplasia. Br J Cancer. 2008;98:1540–7. doi: 10.1038/sj.bjc.6604329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Faca VM, Song KS, Wang H, et al. A mouse to human search for plasma proteome changes associated withpancreatic tumor development. PLoS Med. 2008;5:e123. doi: 10.1371/journal.pmed.0050123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koopmann J, Fedarko NS, Jain A, et al. Evaluation of osteopontin as biomarker for pancreatic adenocarcinoma. Cancer Epidemiol Biomarkers Prev. 2004;13:487–91. [PubMed] [Google Scholar]
- 21.Mroczko B, Lukaszewicz-Zajac M, Wereszczynska-Siemiatkowska U, et al. Clinical significance of the measurements of serum matrix metalloproteinase-9 and its inhibitor (tissue inhibitor of metalloproteinase-1) in patients with pancreatic cancer: metalloproteinase-9 as an independent prognostic factor. Pancreas. 2009;38:613–8. doi: 10.1097/MPA.0b013e3181a488a0. [DOI] [PubMed] [Google Scholar]
- 22.Yurkovetsky Z, Skates S, Lomakin A, et al. Development of a Multimarker Assay for Early Detection of Ovarian Cancer. J Clin Oncol. 2010 doi: 10.1200/JCO.2008.19.2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B (Methodological) 1995;57:289–300. [Google Scholar]
- 24.Brand RE. Screening for familial pancreatic cancer: is doing something better than doing nothing? Gut. 2009;58:1321–2. doi: 10.1136/gut.2009.181214. [DOI] [PubMed] [Google Scholar]
- 25.Joergensen MT, Brunner N, De Muckadell OB. Comparison of circulating MMP-9, TIMP-1 and CA19-9 in the detection of pancreatic cancer. Anticancer Res. 30:587–92. [PubMed] [Google Scholar]
- 26.Sandblom G, Granroth S, Rasmussen IC. TPS, CA 19-9, VEGF-A, and CEA as diagnostic and prognostic factors in patients with mass lesions in the pancreatic head. Ups J Med Sci. 2008;113:57–64. doi: 10.3109/2000-1967-214. [DOI] [PubMed] [Google Scholar]
- 27.Lipton A, Ali SM, Leitzel K, et al. Serum osteoprotegerin levels in healthy controls and cancer patients. Clin Cancer Res. 2002;8:2306–10. [PubMed] [Google Scholar]
- 28.Keibel A, Singh V, Sharma MC. Inflammation, microenvironment, and the immune system in cancer progression. Current pharmaceutical design. 2009;15:1949–55. doi: 10.2174/138161209788453167. [DOI] [PubMed] [Google Scholar]
- 29.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gutfeld O, Prus D, Ackerman Z, et al. Expression of serum amyloid A, in normal, dysplastic, and neoplastic human colonic mucosa: implication for a role in colonic tumorigenesis. J Histochem Cytochem. 2006;54:63–73. doi: 10.1369/jhc.5A6645.2005. [DOI] [PubMed] [Google Scholar]
- 31.Mullan RH, Bresnihan B, Golden-Mason L, et al. Acute-phase serum amyloid A stimulation of angiogenesis, leukocyte recruitment, and matrix degradation in rheumatoid arthritis through an NF-kappaB-dependent signal transduction pathway. Arthritis Rheum. 2006;54:105–14. doi: 10.1002/art.21518. [DOI] [PubMed] [Google Scholar]
- 32.Weinstein PS, Skinner M, Sipe JD, Lokich JJ, Zamcheck N, Cohen AS. Acute-phase proteins or tumour markers: the role of SAA, SAP, CRP and CEA as indicators of metastasis in a broad spectrum of neoplastic diseases. Scand J Immunol. 1984;19:193–8. doi: 10.1111/j.1365-3083.1984.tb00919.x. [DOI] [PubMed] [Google Scholar]
- 33.Miyake K, Imura S, Nishioka M, et al. Serum evaluation of soluble interferon-alpha/beta receptor and high-sensitivity C-reactive protein for diagnosis of the patients with gastrointestinal and hepatobiliary-pancreatic cancer. Cytokine. 2010;49:251–5. doi: 10.1016/j.cyto.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 34.Garcea G, Dennison AR, Steward WP, Berry DP. Role of inflammation in pancreatic carcinogenesis and the implications for future therapy. Pancreatology. 2005;5:514–29. doi: 10.1159/000087493. [DOI] [PubMed] [Google Scholar]
- 35.McDade TP, Perugini RA, Vittimberga FJ, Jr, Carrigan RC, Callery MP. Salicylates inhibit NF-kappaB activation and enhance TNF-alpha-induced apoptosis in human pancreatic cancer cells. J Surg Res. 1999;83:56–61. doi: 10.1006/jsre.1998.5560. [DOI] [PubMed] [Google Scholar]
- 36.Kuwada Y, Sasaki T, Morinaka K, Kitadai Y, Mukaida N, Chayama K. Potential involvement of IL-8 and its receptors in the invasiveness of pancreatic cancer cells. Int J Oncol. 2003;22:765–71. [PubMed] [Google Scholar]
- 37.Jackson AL, Loeb LA. The contribution of endogenous sources of DNA damage to the multiple mutations in cancer. Mutat Res. 2001;477:7–21. doi: 10.1016/s0027-5107(01)00091-4. [DOI] [PubMed] [Google Scholar]
- 38.Talamini G, Bassi C, Falconi M, et al. Alcohol and smoking as risk factors in chronic pancreatitis and pancreatic cancer. Dig Dis Sci. 1999;44:1303–11. doi: 10.1023/a:1026670911955. [DOI] [PubMed] [Google Scholar]
- 39.Yan L, Tonack S, Smith R, et al. Confounding effect of obstructive jaundice in the interpretation of proteomic plasma profiling data for pancreatic cancer. J Proteome Res. 2009;8:142–8. doi: 10.1021/pr800451h. [DOI] [PubMed] [Google Scholar]
- 40.Ballantyne GH, Gumbs A, Modlin IM. Changes in insulin resistance following bariatric surgery and the adipoinsular axis: role of the adipocytokines, leptin, adiponectin and resistin. Obes Surg. 2005;15:692–9. doi: 10.1381/0960892053923789. [DOI] [PubMed] [Google Scholar]
- 41.Jones L, Ghaneh P, Humphreys M, Neoptolemos JP. The matrix metalloproteinases andtheir inhibitors in the treatment of pancreatic cancer. Ann N Y Acad Sci. 1999;880:288–307. doi: 10.1111/j.1749-6632.1999.tb09533.x. [DOI] [PubMed] [Google Scholar]
- 42.van Grevenstein WM, Hofland LJ, Jeekel J, van Eijck CH. The expression of adhesion molecules and the influence of inflammatory cytokines on the adhesion of human pancreatic carcinoma cells to mesothelial monolayers. Pancreas. 2006;32:396–402. doi: 10.1097/01.mpa.0000220865.80034.2a. [DOI] [PubMed] [Google Scholar]
- 43.Liu Z, Guo B, Lopez RD. Expression of intercellular adhesion molecule (ICAM)-1 or ICAM-2 is critical in determining sensitivity of pancreatic cancer cells to cytolysis byhuman gammadelta-T cells: implications in the design of gammadelta-T-cell-based immunotherapies for pancreatic cancer. J Gastroenterol Hepatol. 2009;24:900–11. doi: 10.1111/j.1440-1746.2008.05668.x. [DOI] [PubMed] [Google Scholar]
- 44.Toiyama Y, Miki C, Inoue Y, et al. Soluble intercellular adhesion molecule-1 as a prognostic marker for stage II colorectal cancer patients. Ann Surg Oncol. 2008;15:1617–24. doi: 10.1245/s10434-008-9874-5. [DOI] [PubMed] [Google Scholar]
- 45.Ozer G, Altinel M, Kocak B, Balci M, Altan A, Gonenc F. Potential value of soluble intercellular adhesion molecule-1 in the serum of patients with bladder cancer. Urol Int. 2003;70:167–71. doi: 10.1159/000068773. [DOI] [PubMed] [Google Scholar]
- 46.Ogawa Y, Hirakawa K, Nakata B, et al. Expression of intercellular adhesion molecule-1 in invasive breast cancer reflects low growth potential, negative lymph node involvement, and good prognosis. Clin Cancer Res. 1998;4:31–6. [PubMed] [Google Scholar]
- 47.van Groningen JJ, Klink SL, Bloemers HP, Swart GW. Expression of tissue-type transglutaminase correlates positively with metastatic properties of human melanoma cell lines. Int J Cancer. 1995;60:383–7. doi: 10.1002/ijc.2910600319. [DOI] [PubMed] [Google Scholar]
- 48.Zirvi KA, Keogh JP, Slomiany A, Slomiany BL. Transglutaminase activity in human colorectal carcinomas of differing metastatic potential. Cancer Lett. 1991;60:85–92. doi: 10.1016/0304-3835(91)90052-j. [DOI] [PubMed] [Google Scholar]
- 49.Mehta K. Biological and therapeutic significance of tissue transglutaminase in pancreatic cancer. Amino Acids. 2009;36:709–16. doi: 10.1007/s00726-008-0128-4. [DOI] [PubMed] [Google Scholar]
- 50.Cheung W, Darfler MM, Alvarez H, et al. Application of a global proteomic approach to archival precursor lesions: deleted in malignant brain tumors 1 and tissue transglutaminase 2 are upregulated in pancreatic cancer precursors. Pancreatology. 2008;8:608–16. doi: 10.1159/000161012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


