Abstract
Objective
To identify clinical and demographic factors predictive of midurethral sling failure.
Methods
Overall treatment failure was defined by one or more of the following objective outcomes: a positive stress test, positive 24-hour pad test or re-treatment for stress urinary incontinence (SUI); subjective outcomes: self reported SUI by the Medical, Epidemiologic and Social Aspect of Aging questionnaire (MESA), incontinent episodes by 3-day diary, or retreatment for SUI, or a combination of these. Logistic regression models adjusting for sling type and clinical site were used to predict odds of overall treatment failure after univariable analysis. Models were also fit to compare factors associated with objective failure versus subjective failure only.
Results
Prior UI surgery (odds ratio [OR] [95% CI], 1.99 [1.14, 3.47]); maximum Q-tip excursion < 30° (OR 1.89 (1.16, 3.05)); MESA urge score per 10 points (OR 1.97 [1.21, 3.21]); and pad weight per 10g (OR 1.06 [1.02, 1.10]) were predictors of overall failure. Having concomitant surgery (OR=0.44 [0.22,0.90]) was predictive of subjective failure only rather than objective failure. Age per 10 years (OR=1.48 [1.14, 1.90]); Urogenital Distress Inventory score per 10 points (OR=1.09[1.02–1.17]); pad weight per 10g (OR=1.05 [1.01, 1.10]) were predictive of objective failure compared to subjective failure only. Associations of risk factors and failure were similar independent of sling type (retropubic or transobturator).
Conclusion
Twelve months after surgery, risk factors for overall and objective treatment failure were similar in women undergoing retropubic and transobturator sling procedures. This information may assist in counseling patients regarding efficacy of sling procedures and in setting expectations for women at increased odds for treatment failure.
Introduction
Midurethral slings are the most frequently performed surgeries in women with stress urinary incontinence (SUI) in the United States. Despite their popularity, information characterizing those women most likely to benefit from these surgeries is meager and conflicting. Possible reasons for this include use of a wide variety of non-comparable outcome measures, non-uniform assessment of subjects and inadequate sample size. Among clinical and demographic factors, increasing age,(1,2) preoperative use of anticholinergic medications for overactive bladder symptoms,(1) mixed incontinence,(3,4) urge incontinence and co-morbid disease,(5) concurrent surgery for pelvic organ prolapse,(1,3) bladder neck immobility,(4) obesity, (3) and prior continence surgery (2,6) have all been suggested as predictors of failure with midurethral sling surgery. These associations have not been confirmed or explored by others.(7)
Larger, prospective studies with well-characterized patients are needed to confirm factors that may predict outcomes with mesh slings. One such study, the Trial of Midurethral Slings (TOMUS), compared efficacy between the retropubic and transobuturator midurethral slings at 12 months in women with stress predominant urinary incontinence (UI). The rates of objectively assessed success (outcomes included a 24 hour pad test, bladder fill stress test and retreatment) were considered equivalent between the two approaches at 12 months. Although the rates of subjectively assessed success (outcomes included bladder diary, SUI symptoms and retreatment) were similar, they did not meet the predetermined criteria for equivalence.(8) This analysis examines baseline demographic and clinical factors as possible predictors of “overall” surgical failure (objective and/or subjective failure) versus treatment success. We also wished to explore those factors associated with objective versus subjective failure, where objective failure may define a higher threshold for failure, potentially reflecting failure more directly aligned with successful placement of the sling and the mechanism of action of the procedure itself.
Materials & Methods
The design and primary results of this two-arm randomized equivalence trial comparing retropubic (RMUS) to transobturator (TMUS) midurethral slings have been described previously.(8,9) Women aged 21 years or older planning stress incontinence surgery were invited to participate. Eligibility requirements included pure or predominant stress incontinence symptoms for at least three months and a positive urinary stress test at a bladder volume of 300 mL or less. Women were randomized to a RMUS or TMUS midurethral sling. Randomization was performed after anesthesia was administered with the use of a permuted-block randomization schedule stratified according to clinical site. Institutional Review Board approval was obtained at nine clinical sites and the coordinating center. Written informed consent was obtained. An independent data and safety monitoring board reviewed the progress, interim results and safety of the study.
Definitions of clinical terms, methods of evaluation, and key surgical elements, including cystoscopic evaluation, were standardized across 9 participating sites.(10, 11) The Tension-Free Vaginal Tape (TVT) (Gynecare™) was used as the retropubic sling, and the Tension-Free Vaginal Tape Obturator (TOT) (Gynecare™) (in-to-out) or the Monarc (American Medical System™ ) (out-to-in) was used as the transobturator midurethral sling. Surgeons declared which transobturator approach they would utilize prior to trial initiation should the subject be randomized to the TMUS arm. Concomitant vaginal surgery was permitted.
Surgical success was determined at 12 months post randomization by the following outcome measures of objective failure: a positive provocative stress test at 300 mL or a positive 24-hour pad test (≥15 mL leakage over 24 hours) or retreatment for stress incontinence and subjective measures including a self-reported stress-type UI symptoms on the Medical Epidemiological and Social Aspects of Aging (MESA) (12) questionnaire or leakage on a 3-day voiding diary or retreatment (behavioral, pharmacologic or surgical) for stress incontinence. Women were considered overall failures if they experienced either objective or subjective failure or both. Data were collected pre-operatively, 2 and 6 weeks, and 6 and 12 months post operatively by interview and clinical examination. For this analysis, potential variables thought to be associated with treatment failure were sociodemographic characteristics (age, race/ethnicity, education, marital status); medical/surgical history (body mass index, smoking status, menopausal status/hormone therapy(HT), previous prolapse surgery, estimated blood loss during sling surgery, prior UI surgery, fecal incontinence symptoms, number of vaginal deliveries); characteristics of UI (self-reported frequency of stress and urge incontinence symptoms from the MESA questionnaire (12); symptom bother and incontinence-related quality of life as measured by the Urogenital Distress Inventory (UDI) and Incontinence Impact Questionnaire (IIQ) (13); number of incontinence episodes/day by 3-day voiding diary; quantity of urine leakage from 24-hour pad test (14); physical examination findings (urethral hypermobility measured by the Q-tip test (15) with Q-tip delta and maximum straining considered; pelvic floor muscle strength (16); pelvic organ prolapse (17); post void residual at discharge (≤100 mL, >100 mL) and outcome of baseline empty bladder stress test (positive/negative)). Performance of concomitant surgery (yes/no) and number of co-morbid illnesses reported (0, 1, 2 or more) was included. (18,19)
To identify predictors of treatment failure, univariable logistic regression models were fit modeling the probability of overall failure and objective failure as a function of each covariate separately, adjusting for treatment group (RMUS and TMUS approaches) and site. The models predicting overall failure compare the women with overall failure to those with overall success. A sub-analysis of the women with objective failure was performed where models were fit to compare women with objective failure to those with subjective failure but objective success. Both continuous and categorical predictors were considered. Odds ratios (ORs) and 95% confidence intervals (CIs) described the associations between clinical parameters and the outcomes. Based on significance at the 0.05 level from the univariable logistic regression models and clinical relevance, multivariable logistic regression models were fit for each defined outcome. To assess whether the relationships between the predictors and failure were similar for each of the treatment groups, interaction terms between each predictor and treatment were considered. Interaction terms between significant main effects were also tested for inclusion in the multivariable models. Hosmer-Lemeshow goodness of fit tests were calculated to assess the fit of the models. A 5% two-sided significance level was used for all statistical testing. Data from women with missing covariate values were included when possible (e.g. available case analysis was used). Analyses were performed using SAS Version 9.2 (SAS Institute, Inc. Cary, NC).
Results
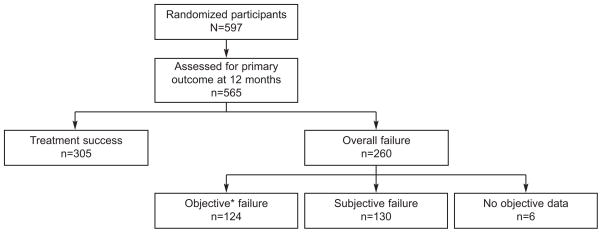
Baseline data were obtained from 597 women. Of those, 565 (95%) were assessed for surgical success at 12 months post-surgery, 280 (94%) of subjects in the RMUS arm and 285 (95%) of subjects in the TMUS arm. Overall treatment failure was seen in 260 (46.0%) subjects as compared to treatment success in 305 (54.0%) subjects (Figure 1). Of the overall failures, 130 failed by subjective measures only; 109 failed by both objective and subjective measures and 15 by objective measures only.
Figure 1.
Trial of Midurethral Slings (TOMUS) patient population with treatment failure information. Comparisons focus on 1) treatment success and overall failure; 2) objective and subjective failures. *109 were objective and subjective failures; 15 were objective failures only.
Baseline characteristics of women with overall failure compared to those with overall success are noted in Table 1. Univariable and multivariable analyses controlling for treatment group and clinical site for each of these baseline characteristics are reported in Table 2. Increasing age and body mass index, prior incontinence surgery, q-tip excursion and maximum straining angle of < 30°; as well as higher baseline leakage, Brink score, pad weight and symptom scores (UDI, IIQ, and MESA questionnaires) were each associated with increased odds of overall failure on initial bivariate analysis. Multivariable logistic regression analysis showed that women who had prior UI surgery had an increased odds of overall failure of approximately two times that of women who had no prior UI surgery controlling for other factors. Women with a maximum Q-tip excursion < 30° (less bladder neck mobility), had a nearly two-fold increased odds of failure compared to those with hypermobility. Baseline severity measures including increasing MESA urge scores and increasing pad weights were also associated with overall failure. For each 10 point increase in urge score the odds of overall failure nearly doubled and for each 10 gram increase in pad weight the odds of overall failure increased by approximately 6%.
Table 1.
Characteristics of Women with Overall Failure versus Overall Success
| Predictor | Overall Failure (n=260) | Overall Success No (n=305) |
|---|---|---|
| Treatment Group | ||
| RMUS | 122(47%) | 158(52%) |
| TMUS | 138(53%) | 147(48%) |
| Race | ||
| Hispanic | 28(11%) | 38(12%) |
| Non-hispanic White | 210(81%) | 239(78%) |
| Non-hispanic Black | 8(3%) | 9(3%) |
| Non-hispanic Other | 14(5%) | 19(6%) |
| Marital Status | ||
| Not married | 87(33%) | 85(28%) |
| Married/Living as married | 173(67%) | 220(72%) |
| Education | ||
| <HS | 10(4%) | 19(6%) |
| HS/GED | 64(25%) | 78(26%) |
| >HS | 99(38%) | 108(35%) |
| BA/BS/Grad/Prof | 87(33%) | 100(33%) |
| Smoking | ||
| Never smoked | 143(55%) | 163(53%) |
| Former smoker | 80(31%) | 103(34%) |
| Current smoker | 37(14%) | 39(13%) |
| HRT Use | ||
| No | 118(45%) | 115(38%) |
| Yes | 77(30%) | 88(29%) |
| Pre-Menopausal | 64(25%) | 101(33%) |
| Previous Prolapse Surgery | ||
| No | 245(95%) | 295(97%) |
| Yes | 14(5%) | 9(3%) |
| Prolapse Stage | ||
| Stage 0–1 | 110(42%) | 140(46%) |
| Stage 2 | 129(50%) | 140(46%) |
| Stage 3+ | 21(8%) | 25(8%) |
| Prior UI Surgery | ||
| No | 210(81%) | 278(91%) |
| Yes | 49(19%) | 26(9%) |
| Fecal Incontinence Symptoms | ||
| No | 195(75%) | 234(77%) |
| Yes | 65(25%) | 71(23%) |
| Concomitant Surgery | ||
| No | 200(75%) | 225(74%) |
| Yes | 60(25%) | 80(26%) |
| Vaginal Deliveries | ||
| Never delivered | 31(12%) | 36(12%) |
| One delivery | 50(19%) | 47(15%) |
| Two deliveries | 66(25%) | 110(36%) |
| Three deliveries | 69(27%) | 68(22%) |
| Four or more deliveries | 44(17%) | 44(14%) |
| PVR at Discharge >100 | ||
| No | 196(79%) | 221(75%) |
| Yes | 51(21%) | 75(25%) |
| Number of Comorbidities | ||
| 0 | 184(71%) | 234(77%) |
| 1 | 48(18%) | 42(14%) |
| 2+ | 28(11%) | 29(10%) |
| Qtip Delta<30 | ||
| No | 157(60%) | 225(74%) |
| Yes | 103(40%) | 80(26%) |
| Qtip Max Straining<30 | ||
| No | 201(77%) | 263(86%) |
| Yes | 59(23%) | 42(14%) |
| Empty bladder stress test | ||
| Positive | 131(51%) | 141(47%) |
| Negative | 128(49%) | 162(63%) |
| Age, years | 54.4(11.4) | 52.2(10.2) |
| BMI | 31.1(6.9) | 29.6(6.3) |
| EBL During Sling, ml | 42.9(50.4) | 43.6(40.4) |
| POPQ Ba | −1.2(1.4) | −1.3(1.6) |
| POPQ Bp | −1.9(1.3) | −2.0(1.5) |
| POPQ Gh | 3.5(1.0) | 3.4(1.1) |
| Brink score | 8.6(2.0) | 8.9(2.0) |
| UDI Total | 139.9(43.3) | 129.3(44.6) |
| IIQ Total | 163.0(98.8) | 139.4(92.5) |
| Stress Score | 20.1(4.5) | 18.8(4.7) |
| Urge Score | 7.2(4.0) | 5.6(3.7) |
| Leaks/day | 3.9(3.2) | 2.9(2.7) |
| Pad Weight, g | 50.2(88.9) | 24.7(39.7) |
RMUS-retropubic midurethral sling; TMUS-transobturator midurethral sling; HS-high school; GED-graduate equivalency degree; BA/BS-bachelors degree; Grad-post-graduate degree; Prof-professional degreel HRT-hormone replacement therapy; UI-urinary incontinence; PVR-postvoid residual; BMI-body mass index; EBL-estimated blood loss; ml-milliliter; g-grams.
Table 2.
Bivariate and Multivariable Associations of Potential Predictors of Overall Failure versus Overall Success, Controlling Treatment Group and Site
| Predictor | Univariable Analyses |
Final Multivariable Analysis* |
||
|---|---|---|---|---|
| p-value | Adjusted Odds Ratio (95%CI) | p-value | Adjusted Odds Ratio (95%CI) | |
| Treatment Group | 0.25 | 0.44 | ||
| RMUS | Reference | Reference | ||
| TMUS | 1.22(0.87–1.70) | 1.15(0.81–1.63) | ||
| Race | 0.53 | |||
| Hispanic | Reference | |||
| Non-hispanic White | 1.56 ( 0.85–2.85) | |||
| Non-hispanic Black | 1.54 ( 0.50–4.70) | |||
| Non-hispanic Other | 1.27 ( 0.52–3.12) | |||
| Marital Status | 0.15 | |||
| Not married | Reference | |||
| Married/Living as married | 0.76 ( 0.53–1.10) | |||
| Education | 0.44 | |||
| <HS | Reference | |||
| HS/GED | 1.56 ( 0.67–3.64) | |||
| >HS | 1.78 ( 0.78–4.05) | |||
| BA/BS/Grad/Prof | 1.75 ( 0.76–4.03) | |||
| Smoking | 0.79 | |||
| Never smoked | Reference | |||
| Former smoker | 0.93 ( 0.64–1.35) | |||
| Current smoker | 1.12 ( 0.67–1.87) | |||
| HRT Use | 0.11 | |||
| No | Reference | |||
| Yes | 0.87 ( 0.57–1.34) | |||
| Pre-Menopausal | 0.64 ( 0.42–0.98) | |||
| Previous Prolapse Surgery, yes | 0.12 | 1.99 ( 0.83–4.75) | ||
| Prolapse Stage | 0.60 | |||
| Stage 0–1 | Reference | |||
| Stage 2 | 1.18 ( 0.83–1.70) | |||
| Stage 3+ | 0.96 ( 0.50–1.87) | |||
| Prior UI Surgery, yes | 0.0002 | 2.69 ( 1.59–4.55) | 0.01 | 1.99(1.14–3.47) |
| Fecal Incontinence Symptoms, yes | 0.61 | 1.11 ( 0.75–1.64) | ||
| Concomitant Surgery, yes | 0.32 | 0.81 (0.54–1.22) | ||
| Vaginal Deliveries | 0.19 | |||
| Never delivered | Reference | |||
| One delivery | 1.11 ( 0.59–2.11) | |||
| Two deliveries | 0.68 ( 0.38–1.22) | |||
| Three deliveries | 1.13 ( 0.62–2.06) | |||
| Four or more deliveries | 1.00 ( 0.51–1.94) | |||
| PVR at Discharge, yes >100 | 0.21 | 0.77 ( 0.51–1.16) | ||
| Number of Comorbidities | 0.20 | |||
| 0 | Reference | |||
| 1 | 1.52 ( 0.95–2.42) | |||
| 2+ | 1.22 ( 0.69–2.15) | |||
| Qtip Delta<30, yes | 0.001 | 1.95 (1.32–2.89) | ||
| Qtip Max Straining<30, yes | 0.005 | 1.97 (1.23–3.14) | 0.01 | 1.89(1.16–3.05) |
| Empty Bladder Stress Test | 0.22 | |||
| Positive | 1.24 (0.88–1.74) | |||
| Negative | Reference | |||
| Age (10 per unit), years | 0.02 | 1.21 ( 1.03–1.42) | ||
| BMI | 0.005 | 1.04 ( 1.01–1.07) | ||
| EBL During Sling (10 per unit), ml | 0.84 | 1.00 ( 0.96–1.04) | ||
| Brink Score | 0.045 | 0.91 ( 0.84–1.00) | ||
| UDI Total (10 per unit) | 0.004 | 1.06 ( 1.02–1.10) | ||
| IIQ Total (10 per unit) | 0.006 | 1.03 ( 1.01–1.04) | ||
| Stress Score(10 per unit) | 0.002 | 1.85 ( 1.26–2.70) | ||
| Urge Score(10 per unit) | <.0001 | 2.88 ( 1.83–4.55) | 0.007 | 1.97(1.21–3.21) |
| Leaks/day | 0.0005 | 1.12 ( 1.05–1.19) | ||
| Pad Weight (10 per grams) | <.0001 | 1.07 ( 1.04–1.11) | 0.003 | 1.06(1.02–1.10) |
Hosmer and Lemeshow Goodness-of-Fit Test p-value=0.70
RMUS-retropubic midurethral sling; TMUS-transobturator midurethral sling; HS-high school; GED-graduate equivalency degree; BA/BS-bachelors degree; Grad-post-graduate degree; Prof-professional degreel HRT-hormone replacement therapy; UI-urinary incontinence; PVR-postvoid residual; BMI-body mass index; EBL-estimated blood loss; ml-milliliter; UDI-Urogenital Distress Inventory; IIQ-Incontinence Impact Questionnaire.
We also explored differences in baseline characteristics of those women with objective failure consisting of a positive stress test, pad test and retreatment (regardless of subjective report) compared to those with subjective failure only (negative stress and pad tests) (Table 3). In univariable analysis subjects with prior incontinence surgery, concomitant surgery, presence of comorbid conditions, age, and baseline UDI, IIQ, MESA urge and stress, and increasing pad weight were significantly associated with objective failure compared to subjects with only subjective failure. Multivariable analyses revealed that for each 10 year increase in age there was a nearly 50% increase in the odds of objective failure compared to subjective only failure controlling for other factors. Increased baseline UDI score and pad weight also predicted nearly a 5–10% increase in the odds of objective failure for each 10 unit increase in value. Further, women who had concomitant surgery were half as likely to fail objectively compared to women who failed subjectively (Table 4). Associations of risk factors with overall and objective/subjective failure were similar for both sling types.
Table 3.
Characteristics of Women with Objective Failure versus Subjective Failure & Objective Success
| Predictor | Objective Failure (n=124) | Subjective Failure & Objective Success (n=130) |
|---|---|---|
| Treatment Group | ||
| RMUS | 57(46%) | 64(49%) |
| TMUS | 67(54%) | 66(51%) |
| Race/ethnicity | ||
| Hispanic | 16(13%) | 12(9%) |
| Non-hispanic White | 99(80%) | 107(82%) |
| Non-hispanic Black | 4(3%) | 3(2%) |
| Non-hispanic Other | 5(4%) | 8(6%) |
| Marital Status | ||
| Not married | 46(37%) | 38(29%) |
| Married/Living as married | 78(63%) | 92(71%) |
| Education | ||
| <HS | 2(2%) | 7(5%) |
| HS/GED | 37(30%) | 26(20%) |
| >HS | 44(35%) | 52(40%) |
| BA/BS/Grad/Prof | 41(33%) | 45(35%) |
| Smoking | ||
| Never smoked | 71(57%) | 68(52%) |
| Former smoker | 33(27%) | 47(36%) |
| Current smoker | 20(16%) | 15(12%) |
| HRT Use | ||
| No | 53(43%) | 61(47%) |
| Yes | 42(34%) | 35(27%) |
| Pre-Menopausal | 28(23%) | 34(26%) |
| Previous Prolapse Surgery | ||
| No | 116(94%) | 123(95%) |
| Yes | 7(6%) | 7(5%) |
| Prolapse Stage | ||
| Stage 0–1 | 55(44%) | 50(38%) |
| Stage 2 | 60(48%) | 68(52%) |
| Stage 3+ | 9(7%) | 12(9%) |
| Prior UI Surgery | ||
| No | 92(75%) | 113(87%) |
| Yes | 31(25%) | 17(13%) |
| Fecal Incontinence Symptoms | ||
| No | 93(75%) | 96(74%) |
| Yes | 31(25%) | 34(26%) |
| Concomitant Surgery | ||
| No | 102(82%) | 92(71%) |
| Yes | 22(18%) | 38(29%) |
| Vaginal Deliveries | ||
| Never delivered | 17(14%) | 14(11%) |
| One delivery | 21(17%) | 27(21%) |
| Two deliveries | 32(26%) | 32(25%) |
| Three deliveries | 34(27%) | 33(25%) |
| Four or more deliveries | 20(16%) | 24(18%) |
| PVR at Discharge >100 | ||
| No | 101(85%) | 91(75%) |
| Yes | 18(15%) | 31(25%) |
| Number of Comorbidities | ||
| 0 | 83(67%) | 96(74%) |
| 1 | 22(18%) | 25(19%) |
| 2+ | 19(15%) | 9(7%) |
| Qtip Delta<30 | ||
| No | 75(60%) | 78(60%) |
| Yes | 49(40%) | 52(40%) |
| Qtip Max Straining<30 | ||
| No | 92(74%) | 105(81%) |
| Yes | 32(26%) | 25(19%) |
| Empty bladder stress test | ||
| Positive | 66(53%) | 62(48%) |
| Negative | 58(47%) | 67(52%) |
| Age, years | 57.0(11.7) | 52.2(10.5) |
| BMI | 30.9(6.6) | 31.3(7.1) |
| EBL During Sling, ml | 45.5(62.1) | 41.0(37.3) |
| POPQ Ba | −1.4(1.3) | −1.1(1.5) |
| POPQ Bp | −2.0(1.2) | −1.8(1.4) |
| POPQ Gh | 3.4(0.9) | 3.5(1.0) |
| Brink Score | 8.6(1.9) | 8.5(2.1) |
| UDI Total | 149.3(45.7) | 130.4(39.3) |
| IIQ Total | 180.4(99.5) | 147.7(95.9) |
| Stress Score | 20.6(4.6) | 19.6(4.4) |
| Urge Score | 7.7(4.1) | 6.7(3.8) |
| Leaks/day | 4.3(3.4) | 3.6(3.1) |
| Pad Weight, grams | 72.7(107.2) | 30.2(62.8) |
RMUS-retropubic midurethral sling; TMUS-transobturator midurethral sling; HS-high school; GED-graduate equivalency degree; BA/BS-bachelors degree; Grad-post-graduate degree; Prof-professional degreel HRT-hormone replacement therapy; UI-urinary incontinence; PVR-postvoid residual; BMI-body mass index; EBL-estimated blood loss; ml-milliliter; POPQ-pelvic organ prolapse quantification; UDI-Urogenital Distress Inventory; IIQ-Incontinence Impact Questionnaire.
Table 4.
Bivariate and Multivariable Associations of Potential Predictors of Objective Failure versus Subjective Failure & Objective Success Controlling Treatment Group and Site
| Covariable | Univariable Analyses |
Final Multivariable Analysis* |
||
|---|---|---|---|---|
| p-value | Adjusted Odds Ratio (95%CI) | p-value | Adjusted Odds Ratio (95%CI) | |
| Treatment Group | 0.43 | 0.45 | ||
| RMUS | Reference | Reference | ||
| TMUS | 1.23(0.74–2.06) | 1.24(0.71–2.17) | ||
| Race | 0.77 | |||
| Hispanic | Reference | |||
| Non-hispanic White | 0.94 (0.38–2.30) | |||
| Non-hispanic Black | 1.63 ( 0.28–9.56) | |||
| Non-hispanic Other | 0.58 ( 0.14–2.41) | |||
| Marital Status | 0.20 | |||
| Not married | Reference | |||
| Married/Living as married | 0.69 ( 0.40–1.21) | |||
| Education | 0.14 | |||
| <HS | Reference | |||
| HS/GED | 5.60 (1.01–31.0) | |||
| >HS | 3.12 ( 0.58–16.6) | |||
| BA/BS/Grad/Prof | 3.48 ( 0.64–18.8) | |||
| Smoking | 0.36 | |||
| Never smoking | Reference | |||
| Former smoking | 0.71 ( 0.39–1.27) | |||
| Current smoking | 1.21 ( 0.55–2.68) | |||
| HRT Use | 0.30 | |||
| No | Reference | |||
| Yes | 1.51 ( 0.80–2.86) | |||
| Pre-Menopausal | 0.90 ( 0.47–1.72) | |||
| Previous Prolapse Surgery, yes | 0.81 | 1.16 ( 0.37–3.65) | ||
| Prolapse Stage | 0.41 | |||
| Stage 0–1 | Reference | |||
| Stage 2 | 0.75 ( 0.43–1.30) | |||
| Stage 3+ | 0.56 ( 0.20–1.53) | |||
| Prior UI Surgery, yes | 0.005 | 2.74 ( 1.36–5.56) | ||
| Fecal Incontinence Symptoms, yes | 0.91 | 0.97 ( 0.54–1.74) | ||
| Concomitant Surgery, yes | 0.03 | 0.50 ( 0.26–0.95) | 0.02 | 0.44(0.22–0.90) |
| Vaginal Deliveries | 0.48 | |||
| Never delivered | Reference | |||
| One delivery | 0.47 ( 0.18–1.26) | |||
| Two deliveries | 0.68 ( 0.26–1.73) | |||
| Three deliveries | 0.73 ( 0.30–1.82) | |||
| Four or more deliveries | 0.46 ( 0.17–1.27) | |||
| PVR at Discharge >100, yes | 0.12 | 0.58 ( 0.29–1.15) | ||
| Number of Comorbidities | 0.04 | |||
| 0 | Reference | |||
| 1 | 1.21 ( 0.61–2.39) | |||
| 2+ | 3.15 ( 1.29–7.71) | |||
| Qtip Delta<30, yes | 0.86 | 1.05 ( 0.59–1.89) | ||
| Qtip Max Straining<30, yes | 0.06 | 1.90 (0.96–3.74) | ||
| Empty bladder stress test | 0.31 | |||
| Positive | 1.31 (0.78, 2.21) | |||
| Negative | Reference | |||
| Age (10 per unit) | 0.0004 | 1.56 ( 1.22–1.99) | 0.003 | 1.48(1.14–1.90) |
| BMI | 0.86 | 1.00 ( 0.97–1.04) | ||
| EBL During Sling (10 per unit), ml | 0.33 | 1.03 ( 0.97–1.09) | ||
| Brink Score | 0.36 | 1.06 ( 0.93–1.21) | ||
| UDI Total (10 per unit) | 0.001 | 1.11 ( 1.04–1.18) | 0.01 | 1.09(1.02–1.17) |
| IIQ Total (10 per unit) | 0.008 | 1.04 ( 1.01–1.07) | ||
| Stress Score(10 per unit) | 0.047 | 1.81 ( 1.01–3.25) | ||
| Urge Score(10 per unit) | 0.01 | 2.35 ( 1.19–4.63) | ||
| Leaks/day | 0.12 | 1.07 ( 0.98–1.16) | ||
| Pad Weight (10 per gram) | 0.0007 | 1.08 ( 1.03–1.12) | 0.02 | 1.05(1.01–1.10) |
Hosmer and Lemeshow Goodness-of-Fit Test p-value=0.99
RMUS-retropubic midurethral sling; TMUS-transobturator midurethral sling; HS-high school; GED-graduate equivalency degree; BA/BS-bachelors degree; Grad-post-graduate degree; Prof-professional degreel HRT-hormone replacement therapy; UI-urinary incontinence; PVR-postvoid residual; BMI-body mass index; EBL-estimated blood loss; ml-milliliter; POPQ-pelvic organ prolapse quantification; UDI-Urogenital Distress Inventory; IIQ-Incontinence Impact Questionnaire.
Discussion
The clinical evaluation of women with UI includes patient history, physical examination and measures of incontinence severity. An understanding of those patient factors associated with treatment failure and success can help us more robustly counsel patients regarding realistic expectations from midurethral sling surgery for stress incontinence. In this analysis we hypothesized that objective and subjective outcome measures capture different post-operative processes and those that failed objectively may be a more “severe” failure or have a greater degree of failure. Objective measures may be a more sensitive reflection of the sling procedures mechanism of action, with the dynamic urethral kinking that occurs with the TVT serving as a fulcrum reflecting surgical technique and quality of host tissue in-growth. (20) An understanding of the types of patients at risk for these types of failures may help us more effectively target patients for these or other treatment options. Subjective failures may capture urge symptoms, less severe leakage or other perceived leakage that may or may not be related to sling function in preventing SUI.
In our study, women who had prior UI surgery had nearly twice the odds of overall failure compared to women having their first surgery for SUI. Previous incontinence surgery as a risk factor for failure after MUS has been described by several authors (2,3,6) and may be due to scarring, nerve damage during periurethral dissection, or more severe neuromuscular compromise. We observed that women with less urethral mobility (Q-tip max straining angle <30 ° had about twice the odds of overall failure than patients with more urethral mobility (Q tip angle ≥30 degrees) despite the fact that pre-operative urethral hypermobility was not associated with objective failure. Others have reported similar findings. (21,22) For example, Liapis et al (21) observed that women with a less mobile urethra (maximum Q-tip straining angle < 30°) undergoing TVT for recurrent SUI had a 50% failure rate compared to 10% failure rate in patients with greater mobility (Q-tip excursion ≥30°). Therefore, patients with less mobility may have a more neurologically impaired baseline urethral function and and other treatments such as bulking agents may be a more appropriate consideration.
For every 10 point increase in the baseline MESA urge incontinence score the odds of overall failure nearly doubled. In addition, for every 10 point increase in urge incontinence bother as measured by the UDI, the odds of objective failure increased by nearly 10%. We and others have also previously described this association. (23,5,24) To this point, Holmgren reported the long-term cure rate after TVT in women with mixed urinary incontinence (MUI) was 30% at 8 years compared to an 85% cure rate in women with pure SUI.(24) However, others have found the presence of urge symptoms in stress-predominant MUI does not negatively impact success. (25,26) Whether patients with more urgency incontinence symptoms reflects a more complex neuromuscular dysfunction is not clear. Nonetheless, patients with MUI should be strongly counseled about the possibility of lower cure rates and perhaps more robust perioperative treatment with behavioral and/or medical therapy should be considered.
We found that greater pad weight at baseline increased the odds of both overall failure and objective failure after MUS and this has been corroborated by others.(2) In the current study pad weight was the only clinical measure associated with both overall and objective surgical failure. Perhaps the use of pad testing should be used more frequently in the evaluation of our patients considering midurethral sling surgery for stress incontinence.
Concomitant prolapse surgery was not associated with overall failure, but did decrease the odds of objective as compared to subjective failure by nearly 50%. Similarly, a large retrospective study showed that concomitant pelvic organ prolapse (POP) surgery decreased the likelihood of failure of retropubic or transobturator MUS (3). These data conflict with another study that reported concurrent POP surgery increased the odds of developing any recurrent incontinence.(1)
Strengths of the study included its multicenter design including sites throughout the United States, with a variety of urology and urogynecology surgeons making our study more generalizable. We included extensive preoperative clinical and demographic variables, used clearly defined validated outcome measures and had a high rate of ascertainment at 12 month post-surgery. In the patient evaluation process for urinary incontinence, after obtaining the baseline clinical evaluation and examination, urodynamic testing is often used to confirm the diagnosis or provide additional functional and/or severity information. This current report only focuses on those demographic and clinical factors that may predict failure.
In conclusion, women with prior incontinence surgery, urethral hypomobility, and more severe urge urinary incontinence symptoms demonstrated greater overall odds of failure 12 months after undergoing RMUS or TMUS surgery. Pad weight testing seems to be a powerful predictor of failure. Although surgical history and urethral mobility are not modifiable risk factors, this information will assist in counseling patients regarding the efficacy of these procedures, help identify patients who may benefit from additional or alternate therapies and assist in setting appropriate expectations for women with increased odds for treatment failure.
Supplementary Material
Acknowledgments
Supported by the National Institute of Diabetes and Digestive and Kidney Diseases U01 DK58231, U01 DK60379, U01 DK60380, U01 DK60401, U01 DK60397, U01DK58225, U01 DK60395, U01 DK58234, U01 DK60393, U01 DK58229 and 2K24-DK068389 to Holly E. Richter..
Footnotes
Presented at the American Urogynecologic Society Meeting, October 1, 2010, Long Beach, CA.
Clinical Trial Registration: ClinicalTrials.gov, www.clinicaltrials.gov, NCT00325039.
Financial Disclosure: Dr. Richter has been a consultant for Xanodyne Pharmaceuticals, Uromedica, and IDEO. She has received research grants and has been a consultant for Pfizer and Astellas. She has also received an education grant from Warner Chilcott. Dr. Lukacz has been a consultant and advisor to Pfizer and Watson. Dr. Fitzgerald has received a research grant from Astellas and speaker honorarium from Astellas, Pfizer, and Ferring. She also has been a consultant to Pfizer and Astellas. Dr. Rickey received research support from Pfizer and is a consultant for Ethicon. The other authors did not report any potential conflicts of interest.
References
- 1.Barber MD, Kleeman S, Karram MM, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol. 2008;199:666.e1–666.e7.7. doi: 10.1016/j.ajog.2008.07.050. [DOI] [PubMed] [Google Scholar]
- 2.Cammu H, Van Den Abbele E, Nagel H, et al. Factors predictive of outcome in tension-free vaginal tape procedure for urinary stress incontinence in a teaching hospital. Int Urogynecol J. 2009;20:775–780. doi: 10.1007/s00192-009-0851-8. [DOI] [PubMed] [Google Scholar]
- 3.Stav K, Dwyer PL, Rosamilia A, et al. Risk factors of treatment failure of midurethral sling procedures for women with urinary stress incontinence. Int Urogynecol J. 2010;21:149–155. doi: 10.1007/s00192-009-1020-9. [DOI] [PubMed] [Google Scholar]
- 4.Karateke A, Haliloglu B, Cam C, et al. Comparison of TVT and TVT-O in patients with stress urinary incontinence: Short-term cure rates and factors influencing the outcome. A prospective randomised study. Aust NZ J Obstet Gynaecol. 2009;49:99–105. doi: 10.1111/j.1479-828X.2009.00957.x. [DOI] [PubMed] [Google Scholar]
- 5.Paick JS, Cho MC, Oh SJ, et al. Factors influencing the outcome of mid urethral sling procedures for female urinary incontinence. J Urol. 2007;178:985–989. doi: 10.1016/j.juro.2007.05.026. discussion 989. [DOI] [PubMed] [Google Scholar]
- 6.Houwert RM, Venema PL, Aquarius AE, et al. Risk factors for failure of retropubic and transobturator midurethral slings. Am J Obstet Gynecol. 2009;201:202, e201–208. doi: 10.1016/j.ajog.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Lee K-S, Choo M-S, Doo CK, et al. The long-term (5 years) objective TVT success rate does not depend on predictive factors at multivariate analysis: a multicentre retrospective study. Europ Urol. 2008;53:176–183. doi: 10.1016/j.eururo.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 8.Richter HE, Albo ME, Zyczynski HM, et al. Retropubic versus transobturator midurethral slings for stress incontinence. NEJM. 2010;362:2066–2076. doi: 10.1056/NEJMoa0912658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Urinary Incontinence Treatment Network. The Trial of Mid-Urethral Slings (TOMUS): Design and Methodology. J Applied Res. 2008;8:1–13. [PMC free article] [PubMed] [Google Scholar]
- 10.Abrams P, Cardozo L, Fall M, et al. The standardization of terminology in lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Urology. 2003;61:37–49. doi: 10.1016/s0090-4295(02)02243-4. [DOI] [PubMed] [Google Scholar]
- 11.Schafer W, Abrams P, Liao L, et al. Good urodynamic practices: uroflowmetry, filling cystometry and pressure flow studies. Neurourol Urodyn. 2002;21:261–274. doi: 10.1002/nau.10066. [DOI] [PubMed] [Google Scholar]
- 12.Herzog AR, et al. Two-year incidence, remission, and change patterns of urinary incontinence in noninstitutionalized older adults. J Gerontol. 1990;45:M67–74. doi: 10.1093/geronj/45.2.m67. [DOI] [PubMed] [Google Scholar]
- 13.Shumaker SA, et al. Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program in Women (CPW) Research Group. Qual Life Res. 1994;3:291–306. doi: 10.1007/BF00451721. [DOI] [PubMed] [Google Scholar]
- 14.Lose G, Jorgensen L, Thunedburg P. 24-hour home pad weighing test versus 1-hour ward test in the assessment of mild stress incontinence. Acta Obstet Gynecol Scand. 1989;68:211–215. doi: 10.3109/00016348909020991. [DOI] [PubMed] [Google Scholar]
- 15.Crystle CD, Charme LS, Copeland WE. Q-tip test in stress urinary incontinence. Obstet Gynecol. 1971;38:313–315. [PubMed] [Google Scholar]
- 16.Brink CA, et al. A digital test for pelvic muscle strength in women with urinary incontinence. Nurs Res. 1994;43:352–356. [PubMed] [Google Scholar]
- 17.Bump RC, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–17. doi: 10.1016/s0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 18.Charlson ME, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Katz JN, et al. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Lo TS, Horng SG, Liang CC, et al. Ultrasound assessment of midurethral tape at three-year follow-up after tension-free vaginal tape procedure. Urology. 2004;63:671–675. doi: 10.1016/j.urology.2003.10.070. [DOI] [PubMed] [Google Scholar]
- 21.Liapis A, Bakas P, Lazaris D, et al. Tension-free vaginal tape in the management of recurrent stress incontinence. Arch Gynecol Obstet. 2004;269:205–207. doi: 10.1007/s00404-003-0530-9. [DOI] [PubMed] [Google Scholar]
- 22.Fritel X, Zabak K, Pigne A, et al. Predictive value of urethral mobility before suburethral tape procedure for urinary stress incontinence in women. J Urol. 2002;168:2472–2475. doi: 10.1016/S0022-5347(05)64171-7. [DOI] [PubMed] [Google Scholar]
- 23.Richter HE, Diokno A, Kenton K, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. J Urol. 2008;179:1024–1030. doi: 10.1016/j.juro.2007.10.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holmgren C, Nilsson S, Lanner L, et al. Long-term results with tension-free vaginal tape on mixed and stress urinary incontinence. Obstet Gynecol. 2005;106:38–43. doi: 10.1097/01.AOG.0000167393.95817.dc. [DOI] [PubMed] [Google Scholar]
- 25.Kulseng-Hanssen S, Husby H, Schiotz HA. Follow-up of TVT operations in 1,113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:391–396. doi: 10.1007/s00192-007-0449-y. [DOI] [PubMed] [Google Scholar]
- 26.Lee JH, Cho MC, Oh SJ, et al. Long-term outcome of the tension-free vaginal tape procedure in female urinary incontinence: a 6-year follow-up. Korean J Urol. 2010;51:409–415. doi: 10.4111/kju.2010.51.6.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.