Abstract
Background:
To compare breast volume measurement techniques in terms of accuracy, convenience, and cost.
Methods:
Breast volumes of 30 patients who were scheduled to undergo total mastectomy surgery were measured preoperatively by using five different methods (mammography, anatomic [anthropometric], thermoplastic casting, the Archimedes procedure, and the Grossman-Roudner device). Specimen volume after total mastectomy was measured in each patient with the water displacement method (Archimedes). The results were compared statistically with the values obtained by the five different methods.
Results:
The mean mastectomy specimen volume was 623.5 (range 150–1490) mL. The breast volume values were established to be 615.7 mL (r = 0.997) with the mammographic method, 645.4 mL (r = 0.975) with the anthropometric method, 565.8 mL (r = 0.934) with the Grossman-Roudner device, 583.2 mL (r = 0.989) with the Archimedes procedure, and 544.7 mL (r = 0.94) with the casting technique. Examination of r values revealed that the most accurate method was mammography for all volume ranges, followed by the Archimedes method.
Conclusion:
The present study demonstrated that the most accurate method of breast volume measurement is mammography, followed by the Archimedes method. However, when patient comfort, ease of application, and cost were taken into consideration, the Grossman-Roudner device and anatomic measurement were relatively less expensive, and easier methods with an acceptable degree of accuracy.
Keywords: breast density, mammography-negativity, macromastia, oncoplastic surgery, reduction mammaplasty
Introduction
Breast volume measurement is of significance in terms of the following:
Measurement of breast volume is an objective criterion for establishing the diagnosis and classification of macromastia.1
In order to establish the medical indication for breast reduction surgery other than cosmetic concerns in macromastia cases, and to calculate specimen volume preoperatively, which is essential information required by insurance and social security companies, breast volume should be measured.1,2
Macromastia may lead to some lesions being-overlooked on mammography and has a higher false-negative rate (Kayar et al. EJC 2010; 8(3Suppl):237, poster: 611).
Breast volume should be measured in breast cancer because the tumor/breast volume ratio is of significance with respect to breast-conserving surgery; breast volume measurement is necessary in order to establish the indication for breast-conserving surgery and to predict the tumor/breast volume ratio.3,4
Breast volume measurement is a determining factor for selecting the approach to be used in all types of breast surgery (reduction, augmentation, reconstructive, and oncoplastic) in order to obtain symmetry of both breasts.1,5
Breast volume measurement is necessary to evaluate the cosmetic results more objectively following breast surgery.1,5
Although breast volume is particularly important, breast volume measurements have not been carried out on a routine basis because there is still no commonly accepted standard method. There are six main methods of breast volume measurement (Table 1). Although the biosterometric method could also be classified under the imaging subset, we decided to address it separately because it is a rather distinct approach.
Table 1.
Main methods of breast volume measurement.
| Archimedes (displacement of water)9 |
| Anthropometry (anatomic) measurement8 |
| Imaging (mammography,6 MRI,12 CT, and US18) |
| Grossman-Roudner device method7 |
| Casting10 |
| Biostereometrics (3-D surface scanning)5,17 |
Abbreviations: MRI, magnetic resonance imaging; CT, computed tomography; US, ultrasonography; 3-D, three-dimensional.
Although several methods have claimed to be accurate in breast volume measurement, they have failed to gain acceptance as routine due to high costs, technical difficulties, and patient discomfort.5 Another important reason for not routinely measuring breast volume is the limited number of studies that have compared the proven methods of breast volume determination and not selecting specimen volume as the control in these studies (Table 2). There exist only three studies that have been conducted with specimen volume as the control, but only a single measurement method was evaluated in these studies.
Table 2.
Characteristics of breast volume measurement series in the literature.
| Author | NP | NM | MRI | Casting | Mam | GRD | Anthropometric | Archimedes | 3-D | Controls |
|---|---|---|---|---|---|---|---|---|---|---|
| Katariya16 | 15 | 1 | – | – | + | – | – | – | – | SV |
| Palin11 | 30 | 1 | – | + | – | + | – | – | – | – |
| Fowler12 | 80 | 4 | + | – | – | – | – | + | – | – |
| Kalbhen6 | 32 | 2 | – | – | + | – | – | – | – | SV |
| Bulstrode4 | 20 | 1 | + | + | + | – | + | + | – | Mam |
| Losken17 | 19 | 2 | – | – | – | – | – | – | + | SV |
| Caruso13 | 5 | 3 | + | + | – | + | – | – | – | – |
| Kovacs5 | 6 | 10 | + | + | – | – | + | – | + | MRI |
| Sigurdson15 | 101 | 1 | – | – | – | – | + | – | – | Archim. |
| Present study | 30 | 1 | – | + | + | + | + | + | – | SV |
Abbreviations: Archim, Archimedes; NP, number of patients; NM, number of measurements; MRI, magnetic resonance imaging; Mam, mammography; GRD, Grossman-Roudner device; SV, specimen volume; 3-D, biostereometry.
In the present study, mastectomy specimen volume was accepted as the control group, and five different breast volume determination methods (excluding three-dimensional imaging) were compared in terms of accuracy, cost, application time, convenience, and patient comfort.
Materials and Methods
Thirty women scheduled for mastectomy (simple or modified radical) due to breast cancer at our clinic between January 2003 and September 2007 were enrolled in this prospective study. The women participated voluntarily and signed informed consent forms.
Breast volume measurement methods were administered in the following order:
Mammography
Grossman-Roudner device
Anatomic (anthropometry)
Archimedes procedure
Casting
For the first examination, the results of the preoperative mammography performed on admission to hospital were used. The mammography technician was consulted regarding the measurement and recording of the compression thickness in the craniocaudal plane. The Grossman-Roudner device and anatomic measurements were performed during or after the physical examination. Measurements using the Archimedes procedure and casting were performed either on the day of physical examination or the next day in the preoperative period. Each measurement in this study was made only once. Ethics Committee approval was obtained for the study.
Mammographic volume measurement
We used the following formula proposed by Kalbhen et al6 because its superiority has been demonstrated in previous studies:
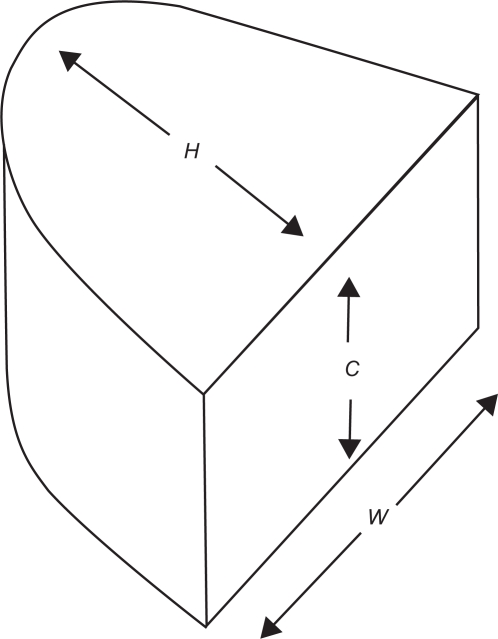
where W = breast width, H = breast height, and C = compression thickness in craniocaudal mammography. The parameters in this formula are shown in Figure 1.
Figure 1.
Mammographic breast volume measurement method (8).
The measurements were performed on the craniocaudal mammograms using a ruler. Compression thickness was measured by the mammography technician.
Grossman-Roudner device
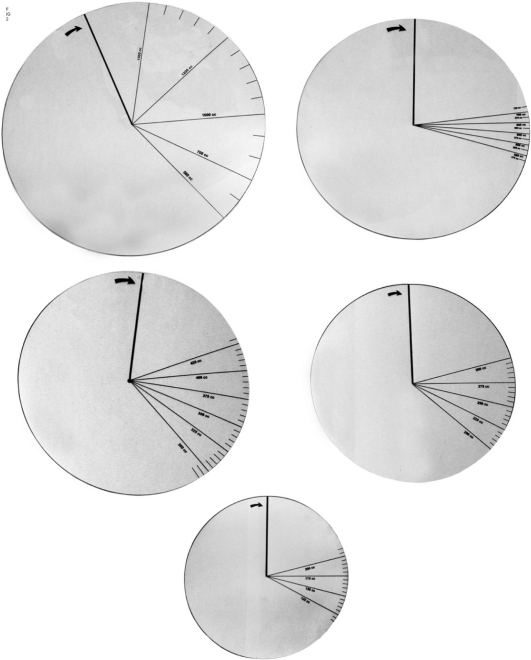
The original three-disc set consisted of a 16 cm disc to measure volumes up to 150–200 mL, 18 cm disc to measure volumes up to 200–300 mL, and a 20 cm disc to measure volumes up to 300–425 mL.7 Two discs, 24 and 28 cm in diameter, were custom-prepared by us in order to measure larger volumes (500–700 mL and 700–1500 mL, respectively).
The Grossman-Roudner device is a graduated disc made of hard transparent polyvinyl chloride material, which can be formed into a cone-shaped device by means of a cut to the center along a radius line (Fig. 2). Patients should be in sitting position with their arms at their sides (if the breasts are large or pendulous, the hands should be elevated to the neck) during the measurement procedure. One-fifth of the area on the disc has markings. The graduated scale of the disc is aligned with the upper outer aspect of the breast and at the same time the lower end of the disc is placed according to the lower breast contour. Then, by pressing gently on the breast, the disk is converted into a cone by its cut edge covering the breast tissue. The breast should be supported from below and lifted gently into the cone. The cone should be filled completely. If the cone cannot cover the breast completely, then a larger size disc should be used. The volume can be read from the calibrations marked on the disc (Fig. 3).
Figure 2.
Grossmann-Roudner-Disks.
Figure 3.
Measurement with GR discs.
Anatomic (anthropometric) measurement
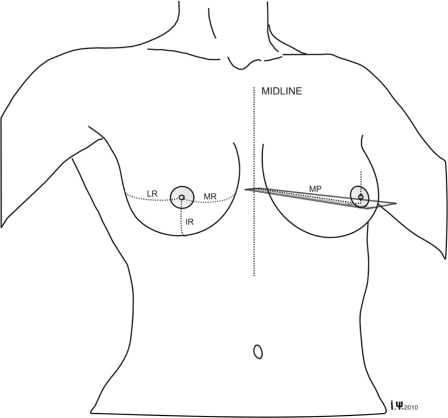
According to the anatomic method, breast volume is measured using anatomic dimensions and a geometric volume formula. The most common formula is the one proposed by Qiao et al,8 as follows:
where MP = mammary projection, MR = medial breast radius, LR = lateral breast radius, and IR = inferior breast radius. The measurements should be performed when the patient is in a sitting or standing with her arms at her sides (Fig. 4).
Figure 4.
Anatomic (anthropometric) measurement.
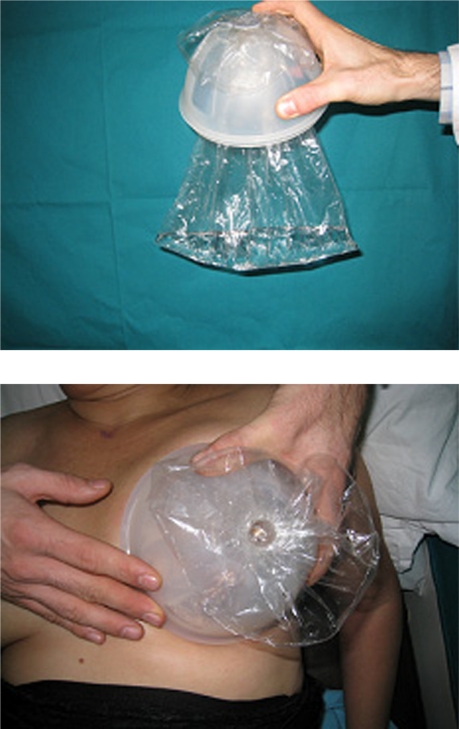
Archimedes (water displacement) procedure
The Archimedes method involves submersion of the breasts into a water-filled container to calculate the amount of displaced water. Although it was first defined by Bouman, we used here a modified version developed by Tezel et al,9 to avoid patient contact with water. In this version, a half-elastic container, an appropriately sized plastic bag, and a plug to seal the bag are used for measurement while the patient is in a half-seated position (Fig. 5). After placing the breast in the container, the difference between the container volume and the water that can be filled into the plastic bag reveals the breast volume (Fig. 6). There are three containers with different capacities (800, 1300, and 1800 mL) according to breast size, and the volume of the plastic bag is 1000 mL.
Figure 5.
Measurement with Archimedes method.
Figure 6.
Measurement with casting method.
Casting method
Gypsum, paraffin, and thermoplastic materials are used in this method, based on forming a cast around the breast together with the chest wall. This method was first applied by Ingleby in 1949.10 Thermoplastic material was chosen in the present study. However, the material we had considered first was Orfit® causing a temperature of 55 °C and being uncomfortable for the patients, we decided to use synthetic gypsum (Policast II). Material contact with the body was avoided using a thin plastic film. Breast volume was measured by filling the cast with water up to the plane passing through the two points at the base.
Surgical technique and specimen volume measurement
Simple mastectomy specimens, before being fixed, were directly put into a graduated cylinder (Fig. 7) and the volumes were determined by the water displacement method. If the axilla was not removed separately by the modified radical mastectomy, axillary tissues were separated by the surgeon from the mastectomy specimens, and the specimen volume was determined afterwards.
Figure 7.
The scaled cylinders for specimen volume measurement.
Density calculation
After determining the mastectomy specimen volume, the specimens were weighed via scale, which enabled us to calculate the breast tissue density for each patient. The relationship between breast density and the mammographic patterns was investigated.
Statistical analysis
Using SPSS version 16.0 (SPSS Inc, Chicago, IL) software, reliability, analysis of variance, and Duncan tests were performed for the comparison between breast density and mammographic pattern. Breast volume values for the five different methods were compared with the surgical specimen volume in each patient. The absolute agreement between them was evaluated by calculating “intraclass correlation coefficient r”. The significance level was accepted as p values lower than 0.05 at a 95% confidence interval.
Results
The mean age of the patients was 51.7 (range 33–84) years, mean height was 158.3 (range 149–169) cm, mean weight was 68.1 (range 49–89) kg, and mean body mass index was 27.1 (range 19.9–35.2) kg/m2. Twenty-nine patients had invasive ductal cancer and one had ductal carcinoma in situ.
The mean mastectomy specimen volume was 623.5 (range 150–1490) mL. The mean breast volume was calculated to be 645.4 (160–1642) mL using the anthropometric method, 615.7 (range 141–1531) mL using the mammographic method, 583.8 (range 145–1400) mL using the Archimedes procedure, 565.8 (range 175–1250) mL using the Grossman-Roudner device, and 544.7 (range 140–1300) mL using the casting method (Table 3).
Table 3.
Reliability (r) of different breast volume measurement methods according to specimen volume.
| Method | Mean volume (mL) | r | Range (r) |
|---|---|---|---|
| Specimen volume | 623.5 ± 340.3 | – | – |
| Anthropometry | 645.4 ± 357.3 | 0.975 | 0.947–0.988* |
| Mammography | 615.7 ± 348.8 | 0.997 | 0.993–0.998* |
| Archimedes | 583.8 ± 314.3 | 0.989 | 0.768–0.997* |
| GRD | 565.8 ± 284.1 | 0.934 | 0.822–0.972* |
| Casting | 544.7 ± 284.9 | 0.946 | 0.532–0.984* |
Note:
P value < 0.001.
Abbreviation: GRD, Grossman-Roudner device.
In order to evaluate the relationship between calculated values and mastectomy specimen volume, the specimen volumes were categorized into five subgroups/subsets as follows: 0–300 mL (six cases), 301–500 mL (six cases), 501–700 mL (nine cases), 700–1000 mL (five cases), and >1000 mL (four cases). We re-evaluated the reliability for those ranges (Table 4). For all volume ranges, with the exception of 0–300 mL, mammography was established to be superior to the other methods. The most accurate method (an [r] value nearest to 1.0) was the Archimedes method for the 0–300 mL range. In fact, the Archimedes method was observed to be the second best method overall, because it revealed quite accurate results for most volume ranges.
Table 4.
Relationship between mastectomy specimen volume subgroups and different breast volume measurement methods.
| Specimen volume (mL) | n | Mammography | Anthropometric | GRD | Archimedes | Casting |
|---|---|---|---|---|---|---|
| 0.871 | 0.872 | 0.815 | 0.968 | 0.881 | ||
| 0–300 | 6 | 0.987–0.047 | 0.986–0.140 | 0.979–0.083 | 0.997–0.054 | 0.989–0.034 |
| 0.912 | 0.687 | 0.916 | 0.937 | 0.862 | ||
| 301–500 | 6 | 0.984–0.620 | 0.938–0.005 | 0.985–0.634 | 0.992–0.007 | 0.981–0.370 |
| 0.941 | 0.047 | 0.457 | 0.856 | 0.513 | ||
| 501–700 | 9 | 0.986–0.772 | 0.633–0.803 | 0.832–0.116 | 0.978–0.008 | 0.875–0.104 |
| 0.890 | 0.688 | 0.351 | 0.757 | 0.342 | ||
| 701–1000 | 5 | 0.988–0.225 | 0.963–0.455 | 0.874–0.139 | 0.974–0.006 | 0.870–0.129 |
| 0.985 | 0.892 | 0.113 | 0.867 | 0.554 | ||
| >1000 | 4 | 0.999–0.782 | 0.992–0.280 | 0.878–0.490 | 0.991–0.034 | 0.956–0.051 |
Abbreviations: GRD, Grossman-Roudner device; n, number of patients.
In order to determine the impact of experience on breast volume measurement, we compared the first 15 measurements with the following 15 measurements. There was no significant statistical difference.
Evaluation of the relationship between the mammographic pattern and breast density (Table 5) revealed that the mean breast density was approximately 0.8 g/cm3 in lipomatous breasts, approximately 0.9 g/cm3 in liposclerotic breasts, and approximately 1.0 g/cm3 in sclerotic breasts.
Table 5.
Relationship between mammographic pattern and breast density.
| Mammographic pattern | Subjects (n) | Mean breast density (g/cm3) |
|---|---|---|
| Lipomatous | 9 | 0.808 ± 0.085 |
| Liposclerotic | 15 | 0.889 ± 0.060 |
| Sclerotic | 6 | 0.963 ± 0.096 |
Note: P < 0.002, analysis of variance and Duncan test.
Comparison of the methods in terms of ease of application, duration, and cost, revealed that the shortest methods were the Grossman-Roudner device and anthropometric method. Mammography and the Archimedes procedure took a relatively longer time (10 minutes). Casting was the longest method, taking approximately 25 minutes (Table 6). In terms of costs, the Grossman-Roudner device, anthropometric method, and the Archimedes procedure were the most economic methods, while casting (mean cost, 20 USD) and mammography (60 USD) were rather expensive methods (Table 6). The Grossman-Roudner device was the most convenient method, followed by anthropometry. Mammography and the Archimedes procedure were relatively more complicated to perform, while casting was the most difficult and uncomfortable method for breast volume determination.
Table 6.
Characteristics of breast volume measurement methods in our study.
| Methods | Duration (min) | Cost (USD) | Convenience | Accuracy |
|---|---|---|---|---|
| GRD | 3 | 1 | +++ | ++ |
| Anthropometric | 5 | 1 | ++ | ++ |
| Mammography | 10 | 60 | + | +++ |
| Archimedes | 10 | 1 | + | +++ |
| Casting | 25 | 20 | – | + |
Abbreviations: USD, United States Dollars; GRD, Grossman-Roudner device.
Discussion
Although breast volume determination is of great importance in the diagnosis and treatment of breast disease, it has not been fully appreciated by many clinicians. The main reason why such an important measurement has not been routinely applied is the absence of a standardized simple, inexpensive, and accurate method.
In the present study, an approach was planned to provide a solution to these problems. We investigated five different methods of breast volume determination in terms of accuracy, convenience, and cost. We evaluated reproducibility from the literature, because it was overlooked in our study.
The studies carried out so far (Table 2) did not have control groups11,13 or used another method as a control.5,14,15 In studies that used specimen volume as the control group,6,16,17 only a single method was evaluated. There was no control group in one of the three studies comparing more than one method,13 while one study used mammography14 and the other study used magnetic resonance imaging as the control group.5
The most significant feature of the present study is that mastectomy specimen volume was used as the control group, and the results of five classical measurement methods, except three-dimensional imaging, were compared.
Thus far, no study has been reported comparing the six different methods of breast volume measurement. The only study available compared four different methods,14 and used mammography as the control group, making it difficult to draw a meaningful conclusion. Bulstrode et al reported that anthropometric and casting methods yielded results similar to mammographic values, while magnetic resonance imaging and the Archimedes procedure were less accurate. Because mammographic volume calculation was made by the formula of a cone in this study instead of the formula of a half-elliptic cylinder, which has a wide acceptance,6 the validity of the study results are debatable.
Of the three studies that used specimen volume as the control group, three6,16 confirmed the high accuracy of the mammographic method and one17 confirmed the accuracy of three-dimensional imaging (r = 0.975). The study conducted by Kovacs et al,5 in which magnetic resonance imaging served as the control group, showed that three-dimensional imaging was the best method. They also reported that the anthropometric method was adequate, but the casting method was relatively less accurate.
Caruso et al13 investigated magnetic resonance imaging, casting, and Grossman-Roudner device methods in terms of costs, but did not make comparisons because they did not have a control group. Mammography was determined to be the most accurate method in this study, followed by the Archimedes procedure and the anthropometric method. While the results yielded by the Grossman-Roudner device were moderately accurate, the results of casting method were less accurate (Table 4).
Each measurement was repeated 10 times in the study by Kovacs et al,5 four times by Fowler et al,12 three times by Caruso et al,13 twice by Losken et al,17 Kalbhen et al,6 and Edsander-Nord et al,10 while we and other authors11,14–16 performed volume measurements only once (Table 2). Reproducibility could not be assessed in studies with a single measurement. In terms of reproducibility, magnetic resonance imaging,12 mammography,6 and three-dimensional imaging17 were demonstrated to be adequate.
Kovacs et al5 demonstrated breast volume measurement using magnetic resonance imaging to be more reproducible when compared with three-dimensional imaging, anthropometry, and casting methods. Caruso et al13 also established magnetic resonance imaging to be the most reproducible method, while the Grossman-Roudner device had moderate reproducibility and the casting method had the lowest level of reproducibility. Edsander-Nord et al10 reported a 6% standard deviation (SD) after two measurements with the casting method, and claimed that casting was a quite reproducible method. Similarly, Malini et al18 claimed that ultrasound had good reproducibility, with an 8% SD in three measurements.
Bulstrode et al4 investigated and scored the acceptability of five different methods by patients and doctors. The most convenient method was the anthropometric measurement for patients. While the patients reported that mammography was intolerable, MRI, the Archimedes procedure, and casting methods were moderately tolerable. For the doctors, on the other hand, the anthropometric and casting methods were reported to be the easiest, while mammography was moderately difficult, and magnetic resonance imaging and the Archimedes procedure were difficult. Evaluation of the combined scores of patients and doctors revealed that the best method was the anatomic method, followed by casting, magnetic resonance imaging, the Archimedes procedure, and mammography. Unfortunately, the Grossman-Roudner device method was not included in this study. Although Kovacs et al5,19 did not compare the four different methods in terms of convenience and comfort, they claimed that three-dimensional imaging was the ideal method because it was simple and did not require pressure on the breast or contact with the patient. In our study, the most comfortable method was the Grossman-Roudner device, followed by anthropometry. Mammography and the Archimedes procedure were rather uncomfortable, and casting was the most uncomfortable one.
The only study comparing breast volume measurement methods in terms of duration was reported by Caruso et al13 (Table 7). They showed that the shortest method was the Grossman-Roudner device. In our study, the Grossman-Roudner device was also the shortest, and the anatomic method was the second shortest procedure. Mammography and the Archimedes procedure were slightly longer procedures as a volume measurement method. Kovacs et al claimed that although three-dimensional imaging was time-consuming initially, when performed by experienced staff and with sufficient technical infrastructure, three-dimensional imaging took very little time.5,19 We believe that this claim needs to be confirmed by other authors.
Table 7.
Time required for breast volume measurement in different methods.
| Methods | Caruso et al13 (min) | Present study (min) |
|---|---|---|
| GRD | 10 | 3 |
| Anthropometric | – | 5 |
| Mammography | – | 10 |
| Archimedes | – | 10 |
| Casting | 120 | 25 |
| MRI | 30 | – |
Abbreviations: GRD, Grossman-Roudner device; MRI, magnetic resonance imaging.
The only available data concerning the cost of the procedure was reported in a study performed by Caruso et al13 (Table 8). The Archimedes, anthropometric, and Grossman-Roudner device methods were reported to have almost no cost. We confirmed that the same results in our study. The cost changing to the selected material of casting method, is approximately 20 USD.15 Although mammography has a considerable cost, it has been suggested that its cost should be accepted as zero in a routine screening program.8 However, cost becomes a problem if mammography is performed for younger women (<40 years of age) with no prior mammographic studies. Moreover, it has been claimed that volume measurement by ultrasound may lead to additional cost,6 but providing the required software and experienced staff may decrease the cost.18 Magnetic resonance imaging is a very expensive method, and causes problems for claustrophobic patients.12
Table 8.
Cost of breast measurement methods in US dollars.
| Methods | Caruso et al13 | Present study |
|---|---|---|
| Mammography | – | 60 |
| Anthropometry | – | 1 |
| GRD | 1 | 1 |
| Archimedes | – | 1 |
| Casting | 20 | 20 |
| MRI | 1400 | – |
Abbreviations: GRD, Grossman-Roudner device; MRI, magnetic resonance imaging.
In the present study, a significant correlation was established between mammographic pattern and mean breast density (Table 5). The studies in the literature on breast density also reported similar results; specifically Katariya et al16 reported breast density to be 0.8–0.95–1.0, which is consistent with our results (Table 9), although Aslan et al20 reported parenchymal density to be approximately 2.5 g/cm3 in gynecomastia and proposed that this fact must be taken into consideration in breast volume calculations. Their suggestion has not been supported by other investigators as yet.
Table 9.
Relationship between mammographic pattern and breast density.
| Mammographic pattern | Katariya et al16 | Present study |
|---|---|---|
| Lipomatous | 0.916 | 0.808 |
| Liposclerotic | 0.944–0.972 | 0.889 |
| Sclerotic | 1.0 | 0.963 |
In the present study, the overall evaluation of breast volume measurement methods was performed based on data gathered from the literature. Data on the methods were scored by us as best (3 points), moderate (2 points), and worst (1 point, Table 10).
Table 10.
Overall evaluation of different breast volume measurement methods.
| Methods | Bulstrode et al14 | Caruso et al13 | Kovacs et al5 | Present study | Overall | Mean |
|---|---|---|---|---|---|---|
| GRD | – | 3 | – | 3 | 6 | 3.00 |
| 3-D imaging | – | – | 3 | – | 3 | 3.00 |
| Anthropometry | 3 | – | 1 | 3 | 7 | 2.30 |
| Mammography | 2 | – | – | 2 | 4 | 2.00 |
| MRI | 1 | 2 | 3 | – | 6 | 2.00 |
| Archimedes | 1 | – | – | 2 | 3 | 1.50 |
| Casting | 2 | 1 | 1 | 1 | 5 | 1.25 |
Our scoring: best (3 points), worst (1 point).
Abbreviations: GRD, Grossman-Roudner disc; MRI, magnetic resonance imaging; 3-D, three-dimensional imaging.
Magnetic resonance imaging and three-dimensional imaging methods are ideal in terms of accuracy and reproducibility. However, these methods are complex and expensive.
Although mammography offers a high level of accuracy and reproducibility, it leads to additional costs for patients <40 years of age, because compression thickness is not reported routinely in mammography reports. On the other hand, Fung et al developed a formula for accurate mammographic measurement which did not need compression thickness. 21 However, this will need to be confirmed by future studies. Furthermore, the mammographic method is associated with poor patient tolerability.
Although anatomic methods are quite accurate and reproducible, selection of the appropriate formula is still a problem, and doing calculations is impractical.
Casting and water displacement methods have not become routine practices due to low patient comfort, complications in their application, and additional costs, as well as their relatively low levels of accuracy. The Grossman-Roudner device, on the other hand, is a simple, rapid, and painless measurement method, which does not lead to additional costs. Moreover, the Grossman-Roudner device offers a high level of accuracy, especially for breast volumes below 500 mL.
We suggest that the Grossman-Roudner device method can be accepted as the standard approach in breast volume measurement because it yields results that are very close to actual values and it is a simple, pain-free, and rapid method. The most common objection to using the Grossman-Roudner device in breast volume measurement is the difficulty in performing measurements over 425 mL with the original three-disc set. We tried to overcome this problem by preparing two custom discs with diameters of 24 cm and 28 cm for volumes of 700 mL and 1500 mL, respectively, similar to the additional disc for 600 mL described by Caruso et al.13 However, the high-volume breast (over 500 mL) is still a problem for the accuracy of the Grossman-Roudner device.
We also suggest that the anthropometric method, and the mammographic method when appropriate, should be used in addition to the routine Grossman-Roudner device procedure. We maintain that this triple measurement method may provide interesting and valuable information, especially for research clinics.
The accuracy of the Grossman-Roudner device for measurement in cases of macromastia and in rigid breasts, such as those with capsular contracture, postirradiation breast thickening has been reported to be poorer.11 Removing those cases from this study resulted in a satisfactory level of accuracy. In conclusion, we suggest that further prospective studies using specimen volume as a control group should be conducted to compare several methods. In this way, we can determine an ideal method of breast volume measurement that becomes a part of routine breast examination.
Acknowledgments
The authors thank Dr. Cemalettin Topuzlu, Medical Faculty, Başkent University, for his scientific contribution to the text, Dr. Mehmet N Orman, Biostatistics Department, Medical Faculty, Ege University, for statistical evaluation, and İlker Yardimci, Dokuz Eylul University, for his contribution to preparation of the figures.
Footnotes
Disclosure
This manuscript has been read and approved by all authors. This paper is unique and is not under consideration by any other publication and has not been published elsewhere. The authors and peer reviewers of this paper report no conflicts of interest. The authors confirm that they have permission to reproduce any copyrighted material.
References
- 1.Kayar R, Catal H. Macromastia and breast cancer. Izmir Tepecik Hstn Derg. 2007;17:121–30. [Google Scholar]
- 2.Brown RW, Cheng Y, Kurtay M. A formula for surgical modifications of the breast. Plast Reconstr Surg. 2000;106:1342–5. doi: 10.1097/00006534-200011000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Cochrane RA, Valasiadou P, Wilson ARM, Al-Chazal SK, Mcmillan RD. Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. Br J Surg. 2003;90:1505–9. doi: 10.1002/bjs.4344. [DOI] [PubMed] [Google Scholar]
- 4.Bullstrode NW, Shrotria S. Prediction of cosmetic outcome following conservative breast surgery using breast volume measurements. Breast. 2001;10:124–6. doi: 10.1054/brst.2000.0197. [DOI] [PubMed] [Google Scholar]
- 5.Kovacs L, Eder M, Hollweck R, et al. Comparison between breast volume measurement using 3 D surface imaging and classical techniques. Breast. 2007;16:137–45. doi: 10.1016/j.breast.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Kalbhen CL, McGill J, Fendley PM, Corrigan KW, Angelats J. Mammographic determination of breast volume: Comparing different methods. Am J Roentgenol. 1999;173:1643–9. doi: 10.2214/ajr.173.6.10584814. [DOI] [PubMed] [Google Scholar]
- 7.Grossman A, Roudner LA. A simple means for accurate breast volume determination. Plast Reconstr Surg. 1980;66:851–2. doi: 10.1097/00006534-198012000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Qiao Q, Zhon G, Ling Y. Breast volume measurement in young Chinese women and clinical applications. Aesthetic Plast Surg. 1997;21:362–8. doi: 10.1007/s002669900139. [DOI] [PubMed] [Google Scholar]
- 9.Tezel E, Numanoglu A. Practical do-it yourself device for accurate volume measurement of breast. Plast Reconstr Surg. 2000;105:1019–23. doi: 10.1097/00006534-200003000-00028. [DOI] [PubMed] [Google Scholar]
- 10.Edsander-Nord A, Wickman M, Jurell G. Measurement of breast volume with thermoplastic casts. Scand J Plast Reconstr Surg Hand Surg. 1996;30:129–32. doi: 10.3109/02844319609056394. [DOI] [PubMed] [Google Scholar]
- 11.Palin WE, von Fraunhofer JA, Smith DJ. Measurement of breast volume: Comparison of techniques. Plast Reconstr Surg. 1986;78:253–6. doi: 10.1097/00006534-198602000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Fowler PA, Casey CE, Cameron GG, Foster MA, Knight CH. Cyclic changes in composition and volume of the breast during the menstrual cycle, measured by magnetic resonance imaging. Br J Obstet Gynaecol. 1990;97:595–602. doi: 10.1111/j.1471-0528.1990.tb02546.x. [DOI] [PubMed] [Google Scholar]
- 13.Caruso MK, Guillot TS, Nguyen T, Greenway FL. The cost effectiveness of three different measures of breast volume. Aesthetic Plast Surg. 2006;30:16–20. doi: 10.1007/s00266-004-0105-6. [DOI] [PubMed] [Google Scholar]
- 14.Bulstrode N, Bellamy E, Shrotria S. Breast volume assessment: Comparing five different techniques. Breast. 2001;10:117–23. doi: 10.1054/brst.2000.0196. [DOI] [PubMed] [Google Scholar]
- 15.Sigurdson LJ, Kirkland SA. Breast volume determination in breast hypertrophy: An accurate method using two anthropomorphic measurements. Plast Reconstr Surg. 2006;118:313–20. doi: 10.1097/01.prs.0000227627.75771.5c. [DOI] [PubMed] [Google Scholar]
- 16.Katariya RN, Forrest APM, Gravelle IH. Breast volumes in cancer of breast. Br J Cancer. 1974;29:270. doi: 10.1038/bjc.1974.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Losken A, Seify H, Denson DD, Paredes AA, Carlson GW. Validating three-dimensional imaging of the breast. Ann Plast Surg. 2005;54:471–6. doi: 10.1097/01.sap.0000155278.87790.a1. [DOI] [PubMed] [Google Scholar]
- 18.Malini S, Smith EO, Goldzieher W. Measurement of breast volume by ultrasound during normal menstrual cycles and with oral contraceptive use. Obstet Gynecol. 1985;66:538–41. [PubMed] [Google Scholar]
- 19.Kovacs L, Eder M, Hollweck R, et al. New aspects of breast volume measurement using 3-dimensional surface imaging. Ann Plast Surg. 2006;57:602–10. doi: 10.1097/01.sap.0000235455.21775.6a. [DOI] [PubMed] [Google Scholar]
- 20.Aslan G, Terzioglu A, Tuncali D, Bingul F. Breast reduction: Weight versus volume. Plast Reconstr Surg. 2003;112:339–40. doi: 10.1097/01.PRS.0000067096.50738.56. [DOI] [PubMed] [Google Scholar]
- 21.Fung JT, Chan SW, Chiu AN, Cheung PS, Lam SH. Mammographic determination of breast volume by elliptical cone estimation. World J Surg. 2010;34:1442–5. doi: 10.1007/s00268-009-0283-0. [DOI] [PubMed] [Google Scholar]