Abstract
OBJECTIVE:
To conduct a meta-analysis of published, full-length, randomized controlled trials evaluating the efficacy of endoscopic band ligation (EBL) versus pharmacological therapy for the primary and secondary prophylaxis of variceal hemorrhage in patients with cirrhosis.
METHODS:
Literature searches were conducted using the PubMed, EMBASE and Cochrane Library databases. Eighteen randomized clinical trials that fulfilled the inclusion criteria were further pooled into a meta-analysis.
RESULTS:
Among 1023 patients in 12 trials comparing EBL with beta-blockers for primary prevention, there was no significant difference in gastrointestinal bleeding (RR 0.79 [95% CI 0.61 to 1.02]), all-cause deaths (RR 1.06 [95% CI 0.86 to 1.30]) or bleeding-related deaths (RR 0.66 [95% CI 0.38 to 1.16]). There was a reduced trend toward significance in variceal bleeding with EBL compared with beta-blockers (RR 0.72 [95% CI 0.54 to 0.96]). However, variceal bleeding was not significantly different between the two groups in high-quality trials (RR 0.84 [95% CI 0.60 to 1.17]). Among 687 patients from six trials comparing EBL with beta-blockers plus isosorbide mononitrate for secondary prevention, there was no effect on either gastrointestinal bleeding (RR 0.95 [95% CI 0.65 to 1.40]) or variceal bleeding (RR 0.89 [95% CI 0.53 to 1.49]). The risk for all-cause deaths in the EBL group was significantly higher than in the medical group (RR 1.25 [95% CI 1.01 to 1.55]); however, the rate of bleeding-related deaths was unaffected (RR 1.16 [95% CI 0.68 to 1.97]).
CONCLUSIONS:
Both EBL and beta-blockers may be considered first-line treatments to prevent first variceal bleeding, whereas beta-blockers plus isosorbide mononitrate may be the best choice for the prevention of rebleeding.
Keywords: Drug therapy, Endoscopic band ligation, Esophageal varices, Meta-analysis
Abstract
OBJECTIF :
Effectuer une méta-analyse des essais aléatoires et contrôlés complets évaluant l’efficacité de la ligature élastique endoscopique (LÉE) par rapport à la pharmacothérapie en prophylaxie primaire et secondaire des hémorragies variqueuses chez les patients atteints de cirrhose.
MÉTHODOLOGIE :
Les chercheurs ont effectué des recherches bibliographiques dans les bases de données PUBMED, EMBASE et de la Bibliothèque Cochrane. Ils ont regroupé 18 essais cliniques aléatoires dans une méta-analyse.
RÉSULTATS :
Chez les 1 023 patients ayant participé aux 12 essais comparant la LÉE aux béta-bloquants en prévention primaire, les chercheurs n’ont constaté aucune différence significative des saignements gastro-intestinaux (RR 0,79 [95 % IC 0,61 à 1,02]), des décès toutes causes confondues (RR 1,06 [95 % IC 0,86 à 1,30]) ou des décès causés par l’hémorragie (RR 0,66 [95 % IC 0,38 à 1,16]). L’hémorragie variqueuse en cas de LÉE tendait à être moins significative qu’en cas de prise de béta-bloquants (RR 0,72 [95 % IC 0,54 à 0,96]). Cependant, dans le cadre d’essais de qualité, l’hémorragie variqueuse ne différait pas de manière significative entre les deux groupes (RR 0,84 [95 % IC 0,60 à 1,17]). Chez les 687 patients tirés de six essais comparant la LÉE aux béta-bloquants associés au mononitrate d’isosorbide en prévention secondaire, les chercheurs n’ont observé aucun effet sur l’hémorragie gastro-intestinale (RR 0,95 [95 % IC 0,65 à 1,40]) ou l’hémorragie variqueuse (RR 0,89 [95 % IC 0,53 à 1,49]). Le risque de décès toutes causes confondues au sein du groupe ayant subi la LÉE était considérablement plus élevé qu’au sein du groupe médicamenté (RR 1,25 [95 % IC 1,01 à 1,55]) mais le taux de décès liés à l’hémorragie demeurait inchangé (RR 1,16 [95 % IC 0,68 à 1,97]).
CONCLUSIONS :
Tant la LÉE que les béta-bloquants peuvent être considérés comme des traitements de première ligne pour prévenir les premières hémorragies variqueuses, tandis que les béta-bloquants associés au mononitrate d’isosorbide seraient le meilleur choix pour prévenir une nouvelle hémorragie.
Esophageal variceal bleeding is a life-threatening complication of cirrhosis. The risk of bleeding among patients with cirrhosis is approximately 30%, with a mortality risk of 30% to 50% associated with each bleeding episode (1–3). Therefore, primary and secondary prophylaxis of variceal bleeding is advantageous, and improvements in current therapeutic protocols would be beneficial.
Drug therapy using nonselective beta-blockers has been found to be effective in decreasing portal pressure and preventing variceal bleeding. A reduction in the risk of variceal bleeding of 40% to 50%, and a mortality rate of 25% to 45% were observed in cirrhotic patients treated with the beta-blockers propranolol or nadolol (4,5). However, many patients have contraindications or experience severe complications, thereby making it necessary to suspend therapy. Furthermore, 30% to 40% of patients will not achieve a sufficient hemodynamic response to reduced portal pressure and prevention of bleeding (6,7). The addition of isosorbide mononitrate (ISMN) to a beta-blocker regimen has the synergistic effect of reducing intrahepatic resistance. Moreover, such combined therapy is also effective in patients who do not respond to beta-blockers alone (8).
Endoscopic techniques have been used to prevent variceal bleeding in cirrhotic patients with severe or moderate varices. In the past decade, sclerotherapy has been replaced by band ligation due to reports of increased mortality and morbidity in several trials for sclerotherapy (9). Endoscopic band ligation (EBL) is a purely mechanical method of eradicating varices, and was introduced to preclude the undesirable effects of sclerotherapy. It has been reported (10) that variceal eradication is achieved with fewer endoscopic sessions and less frequent complications with EBL than with sclerotherapy.
Recently, many investigators have compared EBL with pharmacological therapy for the primary and secondary prophylaxis of variceal bleeding in cirrhotic patients. However, the results of these studies are controversial and partly inconclusive. Therefore, we performed a meta-analysis to evaluate the efficacy and safety of EBL versus pharmacological therapy for the primary and secondary prophylaxis of variceal hemorrhage, and the improvement of survival rates in cirrhotic patients.
METHODS
Study eligibility
Studies eligible for inclusion in the present meta-analysis were required to fulfill the following criteria: randomized controlled trials (RCTs); studies examining patient populations with esophageal varices caused by cirrhosis, with or without previous history of variceal bleeding; studies comparing EBL versus pharmacological therapy interventions; and studies that examined outcomes including gastrointestinal bleeding, variceal bleeding, treatment-related complications and death from any cause. Review articles, retrospective analyses, case reports and studies that were reported only in abstract form were excluded. If a study that met the selection criteria had missing data, the authors were contacted in an attempt to reconcile these data.
Literature search
Two investigators independently searched the published English-language literature in the databases PubMed (1980 to present), EMBASE (1980 to present) and the Cochrane Library (2010, Issue 2). The following search terms were used: “adrenergic beta-antagonists” or “propranolol” or “nadolol” or “carvedilol” and “ligation” and “esophageal varices”. In PubMed and EMBASE, the following MeSH terms were used where possible: “adrenergic beta-antagonists” and “esophageal and gastric varices”. The search was limited to clinical trials published in English. Only full-length, published peer-reviewed studies were considered for inclusion. The bibliographies of all relevant studies and recent review articles were scanned to identify additional citations.
Data extraction
Data were extracted by two independent observers using standardized forms. Recorded data included patient characteristics, the details of EBL procedures, pharmacological therapy protocols, the outcome variables listed above and any reported side effects of therapy. The quality of all selected articles was ranked in accordance with the Jadad composite scale (11). Allocation concealment was assessed according to the classification of the Cochrane Collaboration. Disagreements remaining after contact with authors were resolved by consensus.
Statistical analysis
If several trials were available for a specific topic, meta-analyses were performed using RevMan version 4.2.10 (Cochrane Collaboration, United Kingdom). The RR was presented with associated 95% CIs. χ2 tests were used to assess statistical heterogeneity, and the Higgins I2 statistic was used to determine the percentage of total variation across studies due to heterogeneity. If the I2 statistic was 50% or less, the fixed-effect model was used to pool studies, otherwise, the random-effects model was used. In cases of clinical heterogeneity regarding study population and therapeutic modalities, pooling was not implemented and the results were assessed using subgroup analyses or descriptive statistics. Sensitivity analyses were performed to assess the effect of study quality.
RESULTS
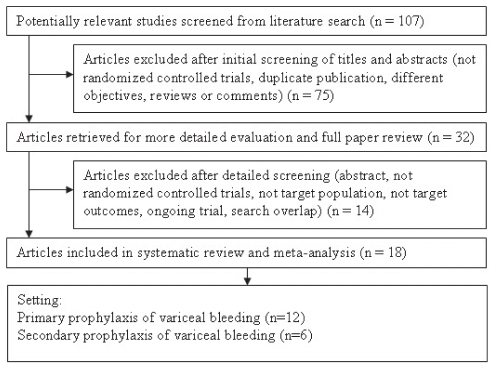
The search strategy yielded 107 studies. From these, 32 RCTs comparing EBL with medical therapy were identified; however, only 18 peer-reviewed, full-length articles (12–29) fulfilled the eligibility criteria of the present meta-analysis (Figure 1).
Figure 1).
Identification of trials for inclusion
Collectively, a total of 1710 participants were enrolled in the 18 studies (Table 1). For primary prophylaxis, a total of 1023 patients were randomly assigned to either EBL or beta-blockers (501 in the EBL arm and 522 in the beta-blocker arm) in 12 trials (12–23). The majority of patients were Child-Pugh class A or B (79.40%), and 33.09% had alcohol-related liver disease. For secondary prophylaxis, six trials (24–29) were included for analysis of EBL versus beta-blockers plus ISMN (n=345 in the EBL arm and n=342 in the beta-blockers plus ISMN arm). The majority of subjects were Child-Pugh class B or C (77.5%), and 40.92% had alcohol-related liver disease.
TABLE 1.
Demographic data of studies included in the meta-analysis
| Author (reference) | Patients, n | Age, years (mean) | Men, % | Alcoholic cirrhosis, % | Varices, grade: % | Child-Pugh class, (A/B/C), % | Follow-up duration, months |
|---|---|---|---|---|---|---|---|
|
Primary prophylaxis: Endoscopic band ligation/beta-blockers | |||||||
| Pérez-Ayuso et al (12) | 39/36 | 60/58 | 48/50 | 21/28 | – | (59/36/5)/(47/42/11) | 67/67 |
| Tripathi et al (13) | 75/77 | 55/54 | 73/70 | 72/74 | III: 11/8 | (35/25/40)/(38/24/38) | 26/26 |
| Norberto et al (14) | 31/31 | 52/52 | – | – | F2: 87/84 | ||
| F3: 13/16 | – | 17/12 | |||||
| Lay et al (15) | 50/50 | 56/55 | 76/80 | 20/22 | F2/F3 in all | (44/42/14)/(46/36/18) | 35/35 |
| Thuluvath et al (16) | 16/15 | 50/54 | 62/47 | 31/7 | F2/F3 in all | 35/45/20 | 27/27 |
| Jutabha et al (17) | 31/31 | 54/55 | 68/74 | 13/10 | – | (39/39/22)/(26/48/26) | 18//12 |
| Psilopoulos et al (18) | 30/30 | 62/59 | 73/67 | 27/23 | II: 77/77 | (43/40/17)/(50/40/10) | 27/28 |
| III: 23/23 | |||||||
| Schepke et al (19) | 75/77 | 54/57 | 67/70 | 53/49 | II: 43/46 | (45/41/14)/(48/40/12) | 34/34 |
| III: 57/54 | |||||||
| Lo et al (20) | 50/50 | 55/57 | 74/80 | 20/20 | F2: 58/64 | (44/42/14)/(48/34/18) | 22/23 |
| F3: 42/36 | |||||||
| Lui et al (21) | 44/66 | 54/55 | 61/53 | 73/62 | II: 91/82 | (31/36/33)/(27/38/35) | 18/21 |
| III: 9/18 | |||||||
| Sarin et al (22) | 45/44 | 44/39 | 73/73 | 27/41 | III: 71/77 | (16/51/33)/(20/50/30) | 13/14 |
| IV: 29/23 | |||||||
| De et al (23) | 15/15 | 42/39 | 67/80 | 14/20 | III: 13/27 | (33/53/14)/(40/47/13) | 18/18 |
| IV: 87/73 | |||||||
|
Secondary prophylaxis: Endoscopic band ligation/beta-blockers plus isosorbate mononitrate | |||||||
| Ahmad et al (24) | 39/35 | 53/52 | 64/60 | 3/0 | F1+F2: 38/34 | (18/59/23)/(6/54/40) | 9/10 |
| F3: 62/66 | |||||||
| Lo et al (25) | 60/61 | 52/51 | 77/77 | 27/36 | F1: 0/2 | (22/58/20)/(21/57/21) | 82/81 |
| F2: 68/49 | |||||||
| F3: 32/49 | |||||||
| Romero et al (26) | 57/52 | 53/51 | 67/65 | 65/58 | – | (32/58/10)/(40/44/16) | 19/17 |
| Sarin et al (27) | 51/50 | 36/36 | 72/68 | 25/23 | II: 21/26 | (31/49/20)/(28/50/22) | 12/11 |
| III: 56/47 | |||||||
| IV: 23/27 | |||||||
| Patch et al (28) | 51/51 | 51/52 | 69/69 | 63/71 | – | (16/37/47)/(13/36/51) | 12/8 |
| Villanueva et al (29) | 72/72 | 58/60 | 65/60 | 60/60 | I: 1/3 | (15/60/25)/(26/54/19) | 25/23 |
| II: 68/57 | |||||||
| III: 31/40 | |||||||
Patients whose prophylaxis failed and those who were unable to tolerate EBL or medication crossed over to alternative treatment if possible and were followed-up with intention-to-treat analysis. For primary prophylaxis, EBL had to be withdrawn and a crossover to beta-blockers was made in 17 patients. Beta-blocker treatment was suspended in 15 patients who subsequently crossed over to EBL therapy (12–14,21). For secondary prophylaxis, 10 patients who withdrew from EBL treatment were entered into a medical program, and 19 patients on beta-blockers plus ISMN treatment were entered into an EBL program (25,29).
Table 2 summarizes the quality of the included studies as assessed by Jadad score. Allocation concealment was assessed according to the classification of the Cochrane Collaboration. For primary prophylaxis, nine (12–14,17–22) of 12 trials used appropriate methods of randomization, and all trials except one (23) reported on completion of follow-up. For secondary prophylaxis, all trials reported the methods of randomization and completion of follow-up. For primary or secondary prevention of bleeding, no blinding was performed for outcome assessment in any of the trials. Allocation concealment was adequate in nine of 12 trials for primary prevention (12–17,19–21) and five of six trials for secondary prevention (24–26,28,29).
TABLE 2.
Methodological quality of trials included in the meta-analysis
| Author (reference) | Year | Randomization method | Blinding | Explanation for withdrawals/dropouts | Jadad score | Allocation concealment | Intention-to-treat analysis |
|---|---|---|---|---|---|---|---|
| Primary prophylaxis | |||||||
| Pérez-Ayuso et al (12) | 2010 | Stratified randomization | None | Yes | 3 | Sealed envelopes | Yes |
| Tripathi et al (13) | 2009 | Randomization in batches of 20 patients | None | Yes | 3 | Sealed envelopes | Yes |
| Norberto et al (14) | 2007 | Computer-generated random numbers | None | Yes | 3 | Sealed envelopes | Yes |
| Lay et al (15) | 2005 | Unclear | None | Yes | 2 | Sealed envelopes | Yes |
| Thuluvath et al (16) | 2005 | Unclear | None | Yes | 2 | Sealed envelopes | Yes |
| Jutabha et al (17) | 2005 | A block randomization for each centre | None | Yes | 3 | Sealed envelopes | Yes |
| Psilopoulos et al (18) | 2005 | Table of random numbers | None | Yes | 3 | Unclear | Yes |
| Schepke et al (19) | 2004 | A block randomization for each centre | None | Yes | 3 | Central randomization | Yes |
| Lo et al (20) | 2004 | Table of random numbers | None | Yes | 3 | Sealed envelopes | Yes |
| Lui et al (21) | 2002 | Randomization in batches of 18 patients | None | Yes | 3 | Sealed envelopes | Yes |
| Sarin et al (22) | 1999 | Table of random numbers | None | Yes | 3 | Unclear | No |
| De et al (23) | 1999 | Unclear | None | Unclear | 1 | Unclear | Yes |
| Secondary prophylaxis | |||||||
| Ahmad et al (24) | 2009 | Computer-generated random numbers | None | Yes | 3 | Sealed envelopes | No |
| Lo et al (25) | 2008 | Table of random numbers | None | Yes | 3 | Sealed envelopes | Yes |
| Romero et al (26) | 2006 | Table of random numbers | None | Yes | 3 | Sealed envelopes | Yes |
| Sarin et al (27) | 2005 | Table of random numbers | None | Yes | 3 | Unclear | Yes |
| Patch et al (28) | 2002 | Table of random numbers | None | Yes | 3 | Sealed envelopes | Yes |
| Villanueva et al (29) | 2001 | Computer-generated random numbers | None | Yes | 3 | Sealed envelopes | Yes |
Primary prophylaxis of variceal bleeding
Twelve RCTs (12–23) compared EBL versus beta-blockers for primary prophylaxis of variceal hemorrhage. Two to nine bands were placed during each endoscopic session, with sessions repeated at intervals of two to four weeks until all varices were obliterated or the residual varices were too small to be ligated. The mean number of EBL sessions required to eradicate varices in different trials varied from 2.0 to 3.8. The mean number of elastic bands applied varied from six to 20.9. Among trials, variceal obliteration was achieved in 57.33% to 100% of patients, with variceal recurrence occurring in 6.4% to 56% of patients who underwent an additional banding session (Table 3).
TABLE 3.
Intervention features for primary prophylaxis reported in the included studies
| Author (reference) |
Endoscopic band ligation |
Variceal |
Beta-blocker; dose, mg/day (mean) | ||
|---|---|---|---|---|---|
| Bands placed, n (mean) | Sessions, n (mean) | Obliteration, % | Recurrence, % | ||
| Pérez-Ayuso et al (12) | 20.9 | 3.2 | 89.74 | 35.90 | Propranolol; 87.5 |
| Tripathi et al (13) | 6.0 | 2.4 | 57.33 | 30.67 | Carvedilol; 12.5 |
| Norberto et al (14) | – | 3.0 | 93.55 | 6.45 | Propranolol; 30 |
| Lay et al (15) | 9.8 | 3.2 | 90.00 | 40.00 | Propranolol; 68.2 |
| Thuluvath et al (16) | 9.4 | 2.7 | 100.00 | 25.00 | Propranolol; 93.3 |
| Jutabha et al (17) | – | 3–4 | 70.97 | – | Propranolol; 86.9 |
| Psilopoulos et al (18) | 10.5 | 3.0 | 93.33 | 23.33 | Propranolol; 60.3 |
| Schepke et al (19) | 10.3 | 2.0 | 92.00 | 56.00 | Propranolol; 77.3 |
| Lo et al (20) | 10.8 | 2.7 | 82.00 | 22.00 | Nadolol; 60 |
| Lui et al (21) | – | 3.1 | 81.82 | 22.73 | Propranolol; 113.5 |
| Sarin et al (22) | – | 3.2 | – | – | Propranolol; 70 |
| De et al (23) | 8.6 | 3.8 | 100.00 | 20.00 | Propranolol; 73.3 |
Ten trials used propranolol as prophylactic therapy (12,14–19,21–23), one trial used nadolol (20) and one trial used carvedilol (13). Among the propranolol group, the mean daily dose in individual trials varied from 30 mg to 93.3 mg. The mean dose of nadolol was 60 mg/day. Carvedilol was used at a dose of 12.5 mg/day (Table 3).
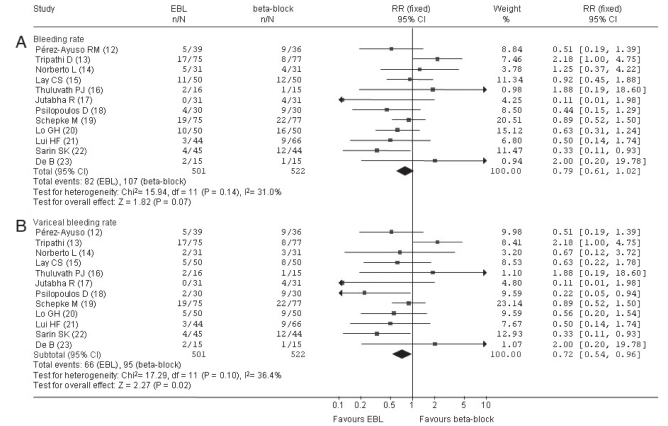
In individual trials, upper gastrointestinal bleeding from all sources occurred in 0% to 25.33% of patients in the EBL group. In the drug therapy arm, the rate of bleeding varied between 6.67% and 30% during the study period. Available information regarding the incidence of bleeding in 12 studies was included in the meta-analysis. The meta-analysis detected a nonsignificant difference in the incidence of gastrointestinal bleeding (EBL 16.37% versus beta-blockers 20.50%; RR 0.79 [95% CI 0.61 to 1.02]; RR reduction −21% [95% CI −39% to 2%]; P=0.07 [Figure 2A]), showing that EBL and beta-blocker therapy were equally effective in the primary prevention of hemorrhage. These trials also evaluated first variceal hemorrhage as an outcome. There was a reduced trend toward significance in the rate of variceal bleeding with EBL (13.17%) compared with beta-blockers (18.20%) (RR 0.72 [95% CI 0.54 to 0.96]; RR reduction −28% [95% CI −46% to −4%]; P=0.02 [Figure 2B]). Larger trials are necessary to confirm these results and to define the optimal strategies for primary prophylactic therapy. Results of statistical tests indicated that the studies were not significantly heterogeneous.
Figure 2).
Fixed-effect model of relative risk for rate of bleeding. Endoscopic band ligation (EBL) versus beta-blocks for primary prophylaxis. A Forest plots for gastrointestinal bleeding. B Forest plots for variceal bleeding. df Degrees of freedom
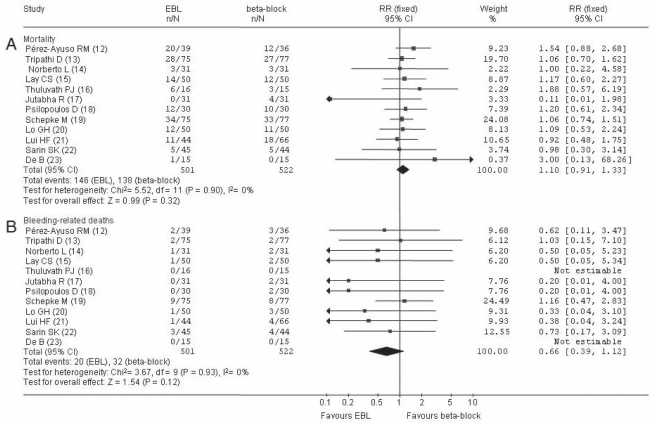
There were 146 deaths in the EBL group and 138 deaths in the beta-blockers group. The majority of patients in both treatment groups died from hepatic failure or variceal bleeding. In the EBL group, death rates in individual trials varied from 0% to 51.28%, with bleeding-related deaths occurring in 0% to 12% of patients. In the beta-blocker group, death rates in individual trials ranged from 9.68% to 42.86%, with bleeding-related deaths occurring in 0% to 10.39% of patients. All trials evaluated all-cause deaths as an outcome measure. There was no significant difference in the incidence of all-cause deaths (EBL [29.14%] versus beta-blockers [26.44%]; RR 1.10 [95% CI 0.91 to 1.33]; RR increase 10% [95% CI −9% to 33%]; P=0.32 [Figure 3A]). Bleeding-related deaths were also evaluated as an outcome measure to compare the effect of EBL versus beta-blockers. No difference was observed between the two groups (EBL [3.99%] versus beta-blockers [6.13%]; RR 0.66 [95% CI 0.39 to 1.12]; RR reduction −34% [95% CI −61% to 12%); P=0.12 [Figure 3B]). The results for all outcomes were statistically homogeneous.
Figure 3).
Fixed-effect model of RR for mortality. Endoscopic band ligation (EBL) versus beta-blocker for primary prophylaxis. A Forest plots for all-cause mortality. B Forest plots for bleeding-related mortality
Overall, complications occurred in 152 patients (30.34%) in the EBL group and in 187 (35.82%) in the medical group. The most common adverse event in the EBL group was dysphagia and chest pain, whereas the most frequent complications in the beta-blocker group were dizziness, symptomatic hypotension and symptomatic bradycardia. Severe complications were experienced by 18 patients (3.59%) treated with EBL (bleeding esophageal ulcers [n=16], subcardial varix [n=1] and perforation of the esophagus [n=1]). Among these patients, two died from uncontrolled bleeding of ligated ulcers (19), and one died from subcardial variceal bleeding (12). Sixty-seven patients (12.84%) who underwent pharmacological treatment had to discontinue beta-blocker therapy because of hypotension, bradycardia and dyspnea. Fatal bleeding occurred in three patients after propranolol withdrawal (15,19).
Secondary prophylaxis of variceal rebleeding
Six RCTs compared EBL versus beta-blockers plus ISMN for the secondary prophylaxis of variceal hemorrhage (24–29). In the EBL group, up to 10 bands per session were placed within the lower esophagus. Sessions were conducted every two to four weeks until the varices had been obliterated. The mean number of treatment sessions required to achieve obliteration varied from two to 3.5. Among the trials, variceal obliteration was achieved in 66.67% to 69% of patients, and recurrent varices occurred in 25.64% to 43.33% of patients (Table 4).
TABLE 4.
Intervention features of included studies for secondary prophylaxis
| Author (reference) | Endoscopic band ligation sessions, n (mean) |
Variceal |
Pharmacological, dose, mg (mean) |
||
|---|---|---|---|---|---|
| Obliteration, % | Recurrence, % | Beta-blocker | ISMN | ||
| Ahmad et al (24) | 3.5 | – | – | Propranolol; 50 | 33 |
| Lo et al (25) | 3.3 | 66.67 | 43.33 | Nadolol; 48 | 30 |
| Romero et al (26) | 3.4 | 69.23 | – | Nadolol; 88 | 57.7 |
| Sarin et al (27) | 3 | – | – | Propranolol; 12.4 | 34.2 |
| Patch et al (28) | 2 | – | 25.64 | Propranolol; 80 | 10–20 |
| Villanueva et al (29) | – | – | – | Nadolol; 96 | 66 |
ISMN Isosorbide mononitrate
Six trials used propranolol or nadolol plus ISMN as prophylactic therapy (24–29). Among patients in the propranolol group (24,27,28), the dose required to achieve the target pulse rate (25% reduction from baseline) varied from 12.4 mg/day to 80 mg/day. Among patients in the nadolol group (25,26,29), the mean dose varied from 48 mg/day to 96 mg/day. The mean dose of ISMN varied from 10 mg/day to 66 mg/day (Table 4).
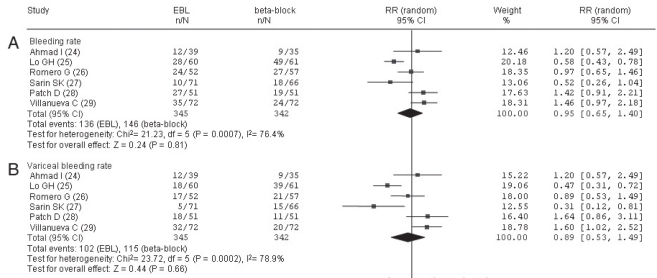
In the EBL group, the actual upper gastrointestinal bleeding rate varied from 14.08% to 52.94%. Among these patients, 7.04% to 44% experienced bleeding from esophageal varices. In the beta-blocker plus ISMN group, the bleeding rate in individual trials varied from 25.71% to 80.32%. When considering only rebleeding from esophageal varices, 21.57% to 63.93% of patients in the medical group experienced recurrent bleeding. A meta-analysis was performed for all six trials. The rate of gastrointestinal bleeding was 39.42% in the EBL group and 42.69% in the beta-blockers plus ISMN group (RR 0.95 [95% CI 0.65 to 1.40); RR reduction −5% [95% CI −35% to 40%]; P=0.81 [Figure 4A]), which was not significantly different. There was also no significant difference with respect to esophageal variceal hemorrhage between the two groups (EBL [29.57%] versus beta-blockers plus ISMN [33.63%] [RR 0.89 (95% CI 0.53 to 1.49)]; RR reduction −11% [95% CI −47% to 49%]; P=0.66 [Figure 4B]). Tests for heterogeneity indicated that the studies were statistically heterogeneous; therefore, the random-effects model was used to pool studies.
Figure 4).
Random-effect model of RR for rate of bleeding. Endoscopic band ligation (EBL) versus beta-blocks plus isosorbide mononitrate for secondary prophylaxis. A Forest plots for gastrointestinal bleeding. B Forest plots for variceal bleeding. df Degrees of freedom
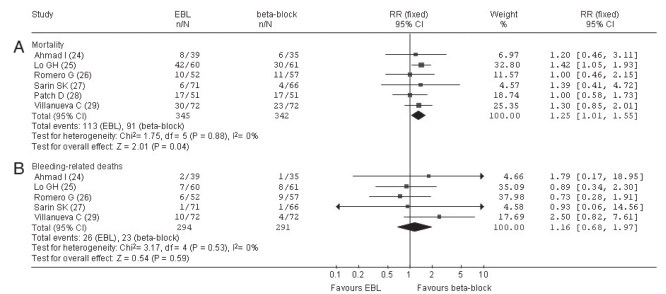
Among all trials, 204 patients died from liver-related disorders (113 in the EBL group and 91 in the beta-blockers plus ISMN group). Twenty-six patients in the EBL group and 23 in the beta-blocker plus ISMN group died from bleeding-related causes. The mortality rate ranged from 8.45% to 70% among patients in the EBL group of individual trials, of which bleeding-related causes accounted for 1.41% to 13.89% of deaths. Among patients in the medical group of individual trials, the mortality rate ranged from 6.06% to 49.18%, of which bleeding-related causes of death varied from 1.52% to 15.79%. Information regarding mortality for all six studies was included in the meta-analysis. The risk for all-cause mortality in the EBL group was significantly higher than in the medical group (EBL 32.75% versus beta-blockers plus ISMN 26.61%; RR 1.25 [95% CI 1.01 to 1.55); RR increase 25% [95% CI 1% to 55%]; P=0.04 [Figure 5A]). Five of six studies (24–27,29) also evaluated bleeding-related deaths as an outcome measure to compare the effect of EBL and drug therapy. No difference was observed between the two groups (EBL [8.84%] versus beta-blockers plus ISMN [7.90%]; RR 1.16 [95% CI 0.68 to 1.97); RR increase 16% [95% CI −32% to 97%]; P=0.59 [Figure 5B]). The results for all outcomes were statistically homogeneous.
Figure 5).
Fixed-effect model of RR for mortality. Endoscopic band ligation (EBL) versus beta-blockers plus isosorbide mononitrate for secondary prophylaxis. A Forest plots for all-cause mortality. B Forest plots for bleeding-related mortality. df Degrees of freedom
Complications developed in 97 patients (28.12%) in the EBL group and 102 patients (29.82%) in the beta-blockers plus ISMN group. Most of the treatment-related complications were mild in the two groups. The most frequent complication in the EBL group was ligation-induced esophageal ulcers, transient dysphagia and retrosternal pain, whereas the most frequent complications in the medical group were dizziness, hypotension and bradycardia. Clinically severe complications in the EBL group were noted in 28 patients (8.12%), including bleeding esophageal ulcer (n=24), perforation (n=1), stenosis (n=1) and aspiration pneumonia (n=2), none of whom died. Beta-blockers were discontinued in 20 patients (6.14%) because of hypotension and bradycardia. Seven patients (2.05%) treated with ISMN experienced hypotension and headache serious enough to discontinue therapy.
Sensitivity analysis
In a sensitivity analysis, five trials for primary prophylaxis (15,16,18,22,23) were considered to be studies of low quality due to unclear methods of randomization or inadequate allocation concealment. A meta-analysis of the remaining seven trials (12–14,17,19–21) of relatively high quality was performed to evaluate the efficacy of EBL versus beta-blockers for the primary prevention of variceal hemorrhage. There was no change in statistical significance for upper gastrointestinal bleeding (RR 0.85 [95% CI 0.63 to 1.16]; P=0.32), overall mortality (RR 1.06 [95% CI 0.85 to 1.31]; P=0.61) or bleeding-related deaths (RR 0.71 [95% CI 0.39 to 1.30]; P=0.26). However, variceal bleeding was not significantly different between the two groups in relatively high-quality trials (EBL 14.78% versus beta-blockers 17.40%; RR 0.84 [95% CI 0.60 to 1.17]; P=0.29).
One trial comparing EBL with beta-blockers plus ISMN for secondary prevention (27) was considered to be of low quality due to inadequate allocation concealment. The remaining five trials (24–26,28,29) were considered to be high-quality studies. Pooling the five trials with adequate allocation concealment resulted in a trend toward critical significance in reducing all-cause mortality with beta-blockers plus ISMN treatment (EBL [39.05%] versus beta-blockers plus ISMN [31.52%]; RR 1.24 [95% CI 1.00 to 1.54]; P=0.05). The RR for the other outcomes (upper gastrointestinal bleeding, variceal bleeding and bleeding-related deaths) remained statistically stable after excluding the low-quality trial.
DISCUSSION
Variceal bleeding is an important complication of cirrhosis and is associated with a high probability of recurrence and death. Prophylactic treatment to prevent bleeding or rebleeding is a primary goal. Over the past 20 years, significant advances in the prevention of variceal bleeding have occurred. However, further therapeutic options with higher efficacy, fewer complications and lower cost are needed (30,31).
The efficacy of EBL for prophylaxis of variceal bleeding and recurrent bleeding compared with beta-blockers remains controversial. The meta-analysis by Imperiale and Chalasani (32) concluded that EBL was superior to propranolol for the prevention of initial bleeding and demonstrated an improved survival rate. The generalizability of this result, however, has been questioned. The meta-analysis by Khuroo et al (33) showed that prophylactic EBL significantly reduced bleeding episodes and adverse severe events compared with beta-blockers, but without any effect on mortality. For secondary prevention, a meta-analysis that compared beta-blockers plus ISMN versus EBL (34) showed no significant differences between treatments in preventing rebleeding or in preventing deaths. However, in trials using a mean beta-blocker dose of less than 80 mg/day (34), EBL significantly reduced rebleeding compared with beta-blockers plus ISMN. In addition, earlier meta-analyses usually included trials in abstract form, of which complete data were not available. Therefore, a further update of studies comparing EBL and pharmacological therapy should be performed.
For primary prophylaxis of variceal hemorrhage in cirrhotic patients, the present meta-analysis demonstrated no significant differences between EBL and beta-blockers with respect to the rate of upper gastrointestinal bleeding, all-cause mortality and bleeding-related mortality. A significant reduction in variceal bleeding was observed in patients who underwent EBL compared with those in the beta-blockers group. However, in trials with adequate randomization methods and allocation concealment, variceal bleeding was not significantly different between the two groups. Of the 12 RCTs included in our meta-analysis, only two demonstrated that EBL significantly reduced variceal bleeding compared with beta-blockers. The results of these two trials might be explained by considerably higher-than-expected bleeding rates in the beta-blockers group and the lower mean dose of beta-blockers used. Therefore, additional evidence from high-quality trials with adequate sample sizes is required to determine which of the two treatments is superior. Possible reasons that the benefits of EBL in preventing first variceal bleeding did not translate into improved mortality are as follows: first, band ligation acts at the variceal bleeding site in a purely mechanical fashion without modifying the underlying pathophysiological abnormalities leading to hemorrhage; second, banding procedures are often effective only for a short period of time, and variceal bleeding recurrence is frequent because of unchanged or increased portal pressure and portal blood-flow (35); and third, EBL could lead to serious adverse events such as bleeding ulcers and esophageal perforation, which increases the risk of death. Therefore, no superiority of EBL over beta-blockers was shown for improvement of overall mortality and bleeding-related mortality in cirrhotic patients. The recommendation made by the American Association for the Study of Liver Diseases and the American College of Gastroenterology is that beta-blockers should be considered as first-line treatment in patients who are not at the highest risk of hemorrhage (ie, Child-Pugh class A and no red signs), while both EBL and beta-blockers are reserved as first-line theray in high-risk patients (Child-Pugh class B/C and medium to large varices) (36,37). Nevertheless, based on currently available data, we recommend that both EBL and beta-blockers should both be considered first-line options for the primary prevention of variceal bleeding in at-risk patients.
For secondary prophylaxis of variceal hemorrhage in cirrhotic patients, the rebleeding rate in patients treated with beta-blockers plus ISMN was similar to those treated with repeat EBL. When evaluating all-cause deaths, there is a survival advantage of combination drug treatment over EBL. Furthermore, patients who underwent drug therapy had a lower risk of dying from uncontrollable variceal rebleeding than those who underwent EBL, but the difference was not statistically significant. The results concerning secondary prevention differ from previous meta-analyses by Cheung et al (34) and Ding et al (38), which demonstrated no significant difference in the mortality rate between EBL and drug treatment. It is likely that drugs such as beta-blockers not only reduce the risk of variceal hemorrhage, but may also attenuate the development of other complications of portal hypertension (20). In contrast, increased portal pressure and aggravation of portal hypertensive gastropathy after repeat EBL might have harmful effects on improving survival (20). In addition, a recent RCT comparing drugs (nadolol plus ISMN) alone with drugs plus EBL for secondary prevention (39) found that adding EBL to drug therapy did not reduce recurrent bleeding or mortality, but did increase the number of adverse events. The disappointing results had an important influence on doctors’ and patients’ decision making regarding rebleeding prevention with adjunctive EBL. To date, the standard approach to preventing variceal rebleeding is not well established. Although the recommendations set forth by the American Association for the Study of Liver Diseases and the American College of Gastroenterology stress the importance of secondary prophylaxis with nonselective beta-blockers and EBL (36,37), the effect of combination therapy (beta-blockers and EBL) is unknown. Moreover, it remains unclear whether EBL is an effective measure that adds benefit to beta-blockers in preventing rebleeding. Therefore, based on currently available data, it appears reasonable to consider drug treatment rather than EBL for first-line rebleeding prevention.
In the studies included in the current analysis, adverse effects occurred with similar frequency in both groups. Further meta-analysis could not be conducted due to the lack of consensus regarding the classification of serious and nonserious adverse events; therefore, the treatment-related adverse effects were evaluated descriptively. There were 40 cases of esophageal bleeding caused by EBL-induced ulcerations and one case of bleeding from EBL-induced subcardial varix, most of which required hospitalization and blood transfusion, three of which were fatal. Other complications seen in the EBL group were usually mild and resolved without any specific therapy. Most patients treated with beta-blockers experienced mild adverse events (hypotension and bradycardia) that were easily managed by dose reduction, and less than 15% of patients experienced adverse events serious enough to withdraw therapy. Adverse effects to ISMN requiring discontinuation were encountered in only 2% of patients. Unfortunately, three fatal hemorrhages in the beta-blockers group occurred shortly after beta-blocker discontinuation (after 0.6 months, three months and 11.9 months, respectively), which suggests a causal relationship (15). Patients treated with EBL tended to have better tolerability throughout the long-term follow-up (15).
The present meta-analysis has several limitations. First, the studies that were included were of relatively poor quality, with three of the 18 studies scoring less than 3 on the Jadad scale (40). It is difficult to perform blinding for trials comparing an endoscopic treatment with a drug treatment. Second, several trials were under-powered or did not report sample size calculations. The inadequate sample size led to wide confidence intervals. We performed the intention-to-treat analyses on the total number of randomized participants, excepting two trials (22,24). Third, the selected RCTs had varying designs including differences in patient populations (eg, the cause or severity of cirrhosis), technical aspects of endoscopic treatment (eg, the interval between sessions and/or the number of bands placed during each session), pharmacological therapy protocols (eg, choice of drug and dose) and surveillance protocol (eg, duration of follow-up). In addition, relative to other beta blockers, carvedilol is both a nonselective beta-blocker and alpha-1 blocker, which reduces portal pressure through both an alpha- and beta-receptor blocking effect. These differences may explain the heterogeneity among and between studies. Thus, the results from the present study are limited and require further confirmation.
CONCLUSION
For primary prophylaxis, no significant differences with respect to upper gastrointestinal bleeding, bleeding-related deaths, or overall mortality were observed between the EBL and beta-blocker groups. There was a reduced trend toward significance in variceal bleeding with EBL compared with beta-blockers. However, in high-quality trials, variceal bleeding was not significantly different between the two groups. For secondary prophylaxis, there were no significant difference with respect to rebleeding rates between EBL and beta-blockers plus ISMN. However, the survival rate was significantly higher in patients treated with combination drugs. The present review suggests that both EBL and beta-blockers can be considered first-choice treatments to prevent first variceal bleeding, whereas beta-blockers plus ISMN may be the best choice for the prevention of rebleeding. However, a large, multicentre cooperative study is still needed to confirm the findings. In the future, it is hoped that innovative endoscopic techniques will be developed and more effective drugs or drug combinations will be available.
REFERENCES
- 1.Smith JL, Graham DY. Variceal hemorrhage: A critical evaluation of survival analysis. Gastroenterology. 1982;82:968–73. [PubMed] [Google Scholar]
- 2.Christensen E, Fauerholdt L, Schlichting P, Juhl E, Poulsen H, Tygstrup N. Aspects of the natural history of gastrointestinal bleeding in cirrhosis and the effect of prednisone. Gastroenterology. 1981;81:944–52. [PubMed] [Google Scholar]
- 3.McCormick PA, O’Keefe C. Improving prognosis following a first variceal haemorrhage over four decades. Gut. 2001;49:682–5. doi: 10.1136/gut.49.5.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pagliaro L, D’Amico G, Sörensen TI, et al. Prevention of first bleeding in cirrhosis: A meta-analysis of randomised trials of nonsurgical treatment. Ann Intern Med. 1992;117:59–70. doi: 10.7326/0003-4819-117-1-59. [DOI] [PubMed] [Google Scholar]
- 5.D’Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: A meta-analytic review. Hepatology. 1995;22:332–54. doi: 10.1002/hep.1840220145. [DOI] [PubMed] [Google Scholar]
- 6.Merkel C, Bolognesi M, Sacerdoti D, et al. The hemodynamic response to medical treatment of portal hypertension as a predictor of clinical effectiveness in the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2000;32:930–4. doi: 10.1053/jhep.2000.19322. [DOI] [PubMed] [Google Scholar]
- 7.Turnes J, Garcia-Pagan JC, Abraldes JG, Hernandez-Guerra M, Dell’Era A, Bosch J. Pharmacological reduction of portal pressure and long-term risk of first variceal bleeding in patients with cirrhosis. Am J Gastroenterol. 2006;101:506–12. doi: 10.1111/j.1572-0241.2006.00453.x. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Pagan JC, Villanueva C, Vila MC, et al. Isosorbide mononitrate in the prevention of first variceal bleed in patients who cannot receive beta-blockers. Gastroenterology. 2001;121:908–14. [PubMed] [Google Scholar]
- 9.Garcia-Pagan JC, Bosch J. Endoscopic band ligation in the treatment of portal hypertension. Nat Clin Pract Gastroenterol Hepatol. 2005;2:526–35. doi: 10.1038/ncpgasthep0323. [DOI] [PubMed] [Google Scholar]
- 10.Singh P, Pooran N, Indaram A, Bank S. Combined ligation and sclerotherapy versus ligation alone for secondary prophylaxis of esophageal variceal bleeding: A meta-analysis. Am J Gastroenterol. 2002;97:623–9. doi: 10.1111/j.1572-0241.2002.05540.x. [DOI] [PubMed] [Google Scholar]
- 11.Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med. 2001;135:982–9. doi: 10.7326/0003-4819-135-11-200112040-00010. [DOI] [PubMed] [Google Scholar]
- 12.Pérez-Ayuso RM, Valderrama S, Espinoza M, et al. Endoscopic band ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhotic patients with high risk esophageal varices. Ann Hepatol. 2010;9:15–22. [PubMed] [Google Scholar]
- 13.Tripathi D, Ferguson JW, Kochar N, et al. Randomized controlled trial of carvedilol versus variceal band ligation for the prevention of the first variceal bleed. Hepatology. 2009;50:825–33. doi: 10.1002/hep.23045. [DOI] [PubMed] [Google Scholar]
- 14.Norberto L, Polese L, Cillo U, et al. A randomized study comparing ligation with propranolol for primary prophylaxis of variceal bleeding in candidates for liver transplantation. Liver Transpl. 2007;13:1272–8. doi: 10.1002/lt.21083. [DOI] [PubMed] [Google Scholar]
- 15.Lay CS, Tsai YT, Lee FY, et al. Endoscopic variceal ligation versus propranolol in prophylaxis of first variceal bleeding in patients with cirrhosis. J Gastroenterol Hepatol. 2006;21:413–9. doi: 10.1111/j.1440-1746.2005.04071.x. [DOI] [PubMed] [Google Scholar]
- 16.Thuluvath PJ, Maheshwari A, Jagannath S, Arepally A. A randomized controlled trial of beta-blockers versus endoscopic band ligation for primary prophylaxis: A large sample size is required to show a difference in bleeding rates. Dig Dis Sci. 2005;50:407–10. doi: 10.1007/s10620-005-1619-8. [DOI] [PubMed] [Google Scholar]
- 17.Jutabha R, Jensen DM, Martin P, Savides T, Han SH, Gornbein J. Randomized study comparing banding and propranolol to prevent initial variceal hemorrhage in cirrhotics with high-risk esophageal varices. Gastroenterology. 2005;128:870–81. doi: 10.1053/j.gastro.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 18.Psilopoulos D, Galanis P, Goulas S, et al. Endoscopic variceal ligation vs. propranolol for prevention of first variceal bleeding: A randomized controlled trial. Eur J Gastroenterol Hepatol. 2005;17:1111–7. doi: 10.1097/00042737-200510000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Schepke M, Kleber G, Nürnberg D, et al. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology. 2004;40:65–72. doi: 10.1002/hep.20284. [DOI] [PubMed] [Google Scholar]
- 20.Lo GH, Chen WC, Chen MH, et al. Endoscopic ligation vs. nadolol in the prevention of first variceal bleeding in patients with cirrhosis. Gastrointest Endosc. 2004;59:333–8. doi: 10.1016/s0016-5107(03)02819-0. [DOI] [PubMed] [Google Scholar]
- 21.Lui HF, Stanley AJ, Forrest EH, et al. Primary prophylaxis of variceal hemorrhage: A randomized controlled trial comparing band ligation, propranolol, and isosorbide mononitrate. Gastroenterology. 2002;123:735–44. doi: 10.1053/gast.2002.35385. [DOI] [PubMed] [Google Scholar]
- 22.Sarin SK, Lamba GS, Kumar M, Misra A, Murthy NS. Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med. 1999;340:988–93. doi: 10.1056/NEJM199904013401302. [DOI] [PubMed] [Google Scholar]
- 23.De BK, Ghoshal UC, Das T, Santra A, Biswas PK. Endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleed: Preliminary report of a randomized controlled trial. J Gastroenterol Hepatol. 1999;14:220–4. doi: 10.1046/j.1440-1746.1999.01800.x. [DOI] [PubMed] [Google Scholar]
- 24.Ahmad I, Khan AA, Alam A, Butt AK, Shafqat F, Sarwar S. Propranolol, isosorbide mononitrate and endoscopic band ligation – alone or in varying combinations for the prevention of esophageal variceal rebleeding. J Coll Physicians Surg Pak. 2009;19:283–6. [PubMed] [Google Scholar]
- 25.Lo GH, Chen WC, Lin CK, et al. Improved survival in patients receiving medical therapy as compared with banding ligation for the prevention of esophageal variceal rebleeding. Hepatology. 2008;48:580–7. doi: 10.1002/hep.22358. [DOI] [PubMed] [Google Scholar]
- 26.Romero G, Kravetz D, Argonz J, et al. Comparative study between nadolol and 5-isosorbide mononitrate vs. endoscopic band ligation plus sclerotherapy in the prevention of variceal rebleeding in cirrhotic patients: A randomized controlled trial. Aliment Pharmacol Ther. 2006;24:601–11. doi: 10.1111/j.1365-2036.2006.03007.x. [DOI] [PubMed] [Google Scholar]
- 27.Sarin SK, Wadhawan M, Gupta R, Shahi H. Evaluation of endoscopic variceal ligation (EVL) versus propranolol plus isosorbide mononitrate/nadolol (ISMN) in the prevention of variceal rebleeding: Comparison of cirrhotic and noncirrhotic patients. Dig Dis Sci. 2005;50:1538–47. doi: 10.1007/s10620-005-2877-1. [DOI] [PubMed] [Google Scholar]
- 28.Patch D, Sabin CA, Goulis J, et al. A randomized, controlled trial of medical therapy versus endoscopic ligation for the prevention of variceal rebleeding in patients with cirrhosis. Gastroenterology. 2002;123:1013–9. doi: 10.1053/gast.2002.35955. [DOI] [PubMed] [Google Scholar]
- 29.Villanueva C, Miñana J, Ortiz J, et al. Endoscopic ligation compared with combined treatment with nadolol and isosorbide mononitrate to prevent recurrent variceal bleeding. N Engl J Med. 2001;345:647–55. doi: 10.1056/NEJMoa003223. [DOI] [PubMed] [Google Scholar]
- 30.Garcia-Pagan JC, De Gottardi A, Bosch J. Review article: The modern management of portal hypertension – primary and secondary prophylaxis of variceal bleeding in cirrhotic patients. Aliment Pharmacol Ther. 2008;28:178–86. doi: 10.1111/j.1365-2036.2008.03729.x. [DOI] [PubMed] [Google Scholar]
- 31.Schepke M. Drugs, ligation or both for the prevention of variceal rebleeding? Gut. 2009;58:1045–6. doi: 10.1136/gut.2009.177964. [DOI] [PubMed] [Google Scholar]
- 32.Imperiale TF, Chalasani N. A meta-analysis of endoscopic variceal ligation for primary prophylaxis of esophageal variceal bleeding. Hepatology. 2001;33:802–7. doi: 10.1053/jhep.2001.23054. [DOI] [PubMed] [Google Scholar]
- 33.Khuroo MS, Khuroo NS, Farahat KL, Khuroo YS, Sofi AA, Dahab ST. Meta-analysis: Endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleeding. Aliment Pharmacol Ther. 2005;21:347–61. doi: 10.1111/j.1365-2036.2005.02346.x. [DOI] [PubMed] [Google Scholar]
- 34.Cheung J, Zeman M, van Zanten SV, Tandon P. Systematic review: Secondary prevention with band ligation, pharmacotherapy or combination therapy after bleeding from oesophageal varices. Aliment Pharmacol Ther. 2009;30:577–88. doi: 10.1111/j.1365-2036.2009.04075.x. [DOI] [PubMed] [Google Scholar]
- 35.Bosch J, García-Pagán JC. Prevention of variceal rebleeding. Lancet. 2003;361:952–4. doi: 10.1016/S0140-6736(03)12778-X. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–38. doi: 10.1002/hep.21907. [DOI] [PubMed] [Google Scholar]
- 37.Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007;102:2086–102. doi: 10.1111/j.1572-0241.2007.01481.x. [DOI] [PubMed] [Google Scholar]
- 38.Ding SH, Liu J, Wang JP. Efficacy of beta-adrenergic blocker plus 5-isosorbide mononitrate and endoscopic band ligation for prophylaxis of esophageal variceal rebleeding: A meta-analysis. World J Gastroenterol. 2009;15:2151–5. doi: 10.3748/wjg.15.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.García-Pagán JC, Villanueva C, Albillos A, et al. Nadolol plus isosorbide mononitrate alone or associated with band ligation in the prevention of recurrent bleeding: A multicentre randomised controlled trial. Gut. 2009;58:1144–50. doi: 10.1136/gut.2008.171207. [DOI] [PubMed] [Google Scholar]
- 40.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]