Abstract
Objectives
To describe the prevalence of hysterectomy for women aged 18-45 seeking treatment at a chronic pain clinic, to describe patient characteristics (pain intensity, age, smoking status, hormone replacement status, and psychosocial factors) based on opioid and hysterectomy status, and to determine whether hysterectomy status predicted receipt of opioid prescription.
Design
Retrospective cross-sectional chart review.
Participants
Total 323 new female patients aged 18-45 who completed the Brief Pain Inventory-Short Form at initial evaluation at a chronic pain clinic during a 12-month period (July 2008- June 2009).
Measures
Data were collected from the Brief Pain Inventory and medical charts. Variables included opioid prescription, average pain intensity, pain type, age, hysterectomy status, smoking status, and pain-related dysfunction across domains measured by the Brief Pain Inventory. The association of opioid prescription with hysterectomy and other factors were determined by logistic regression.
Results
Prevalence of hysterectomy was 28.8%. Average pain intensity was not associated with either hysterectomy or opioid prescription status. However, hysterectomy and high levels of pain-related dysfunction were significantly and independently associated with opioid prescription after adjusting for age and pain intensity. More than 85% of women with hysterectomy and high pain-related dysfunction had opioid prescription.
Conclusions
Hysterectomy may confer risk for pain-related dysfunction and opioid prescription in women 45 and younger. More research is needed to understand (1) how patient characteristics influence prescribing patterns; and (2) the specific medical risks and consequences of chronic opioid therapy in this population.
Keywords: hysterectomy, chronic pain, opioids, pain-related dysfunction, hormone replacement
Introduction
Hysterectomy is the most common non-obstetric medical procedure performed on U.S. women younger than 45 years of age,1 and nearly 1 in 5 women of reproductive age have had the surgery.2 Although pain is a commonly reported symptom prior to3 and following hysterectomy,4 little is known about the experience and impact of chronic pain in the post-hysterectomy years, or pain treatment patterns such as opioid prescription. It is important to understand the pathways by which women may arrive at opioid prescription. For instance, hysterectomy may confer risk for opioids that could be driven by patient characteristics, medical complexity, hormonal factors, or a combination of these factors. In addition to the possibility that women with hysterectomy may have distinct pathways to opioid prescription, they may also experience unique consequences from chronic opioid use. Long term opioid use is associated with medical risks such as hormonal disturbance5, 6 and hyperalgesia,7-12 and young women with hysterectomy may at heightened risk for iatrogenic effects given that their hormonal milieu is already compromised.
Indeed, research suggests the opioid-induced effects of impaired adrenal production and hypogonadism may be compound existing hormonal dysregulation in women with hysterectomy. One study found that women with oophorectomy (removal of ovaries) who were taking long-acting opioids had free testosterone levels that were 39% lower than oophorectomized women who were not taking opioids.13 Sex-steroid variation and hormonal perturbation has long been associated with pain,1, 14-17 and therefore it follows that the potential negative effects of hysterectomy (hormonal disruption) and chronic opioid therapy (hormonal dysregulation6, hyperalgesia7-12) may either compound or synergize in women with both hysterectomy and chronic opioid use. In terms of pain, the implications of these associations might include the experience of greater pain intensity, pain progression (as manifested by a greater number of pain conditions), and/or greater use of opioids.
While it is clearly important to understand better the medical risks and consequences of opioid therapy in women with and without hysterectomy, the question remains: How might hysterectomy relate to opioid prescribing in the post-surgical years? The broader pain literature demonstrates that individual characteristics and psychosocial factors strongly predict medical decision making, such as prescription for long term opioid therapy.18, 19 Therefore, it is possible that individual characteristics may influence presurgical treatment patterns and may increase the likelihood of hysterectomy. In terms of opioid prescribing and use, relevant individual characteristics include psychiatric diagnoses,20 frequency of medical service utilization,21, 22 pain behaviors exhibited during medical visits,19 smoking status,23 and pain-related functional impairment.19 How hysterectomy might relate to these factors is unknown and, to our knowledge, unreported.
To date, the prevalence of historical hysterectomy in younger women with chronic pain is also unknown, as is the relationship between hysterectomy status and opioid prescription, a primary treatment for chronic pain. Women 45 and younger comprise a critical age cohort to examine the association of hysterectomy and opioid prescribing patterns given their relatively young age and the impact of pain treatment choices over a potentially large number of years. Gaining a better understanding of the associations between chronic pain, opioid prescription, and hysterectomy in women of reproductive age may inform the treatment needs in this subpopulation.
Accordingly, this study first aimed to describe the prevalence of hysterectomy for women aged 18-45 presenting for evaluation at a chronic pain clinic. The second aim was to describe sample characteristics (pain intensity, age, smoking status, hormone replacement therapy (HRT) status, and psychosocial factors) for women based on opioid and hysterectomy status. The third aim was to determine whether hysterectomy status predicted opioid prescription status. We hypothesized that women with hysterectomy would have greater levels of pain and likelihood for opioid prescription, given their history of surgical intervention and hormonal dysregulation; however, we also aimed to examine how patient characteristics might influence the relationship between hysterectomy and opioid prescription. We hypothesized that greater pain-related dysfunction would predict opioid prescription, particularly for women with hysterectomy.
Methods
Study Design and Study Population
The study was conducted in compliance with the Human Subjects Committee of the Institutional Review Board of Oregon Health & Science University (OHSU). The design was a retrospective cross-sectional chart review for all new female patients aged 18-45 seen for initial medical evaluation in a multidisciplinary chronic pain clinic (the OHSU Comprehensive Pain Center, Portland, OR) during a 12-month period extending between 2008-2009 (N=444). Patients were referred by primary care physicians for chronic pain evaluation. Data for the Brief Pain Inventory-Short Form were available for 323 women and therefore these women comprised our final sample (the remaining 121 women were mainly evaluated at satellite clinics that did not administer the measure). Data were abstracted by one person (BD) using an abstraction form developed prior to the study. To ensure accuracy, data were double-checked and verified by a research assistant for 10% of the sample (N=32). In addition to the Brief Pain Inventory, data abstracted from the initial visit with the pain physician included hysterectomy status, age, smoking status (yes/no), current opioid prescription (yes/no), hormone replacement status (yes/no), pain type(s), and pain diagnoses. Pain diagnoses were abstracted from active problem list and number of pain complaints was quantified; information regarding the primary pain complaint for which patients were seeking treatment from the pain clinic was not reliably abstractable. Therefore, because pelvic pain is of particular relevance to women who undergo hysterectomy, we specifically recorded the number of women who have active pelvic pain in their chart, with the limitation being that we do not know whether they were being treated for pelvic pain that day. We abstracted the number and type of diagnosed pain complaints in the problem list of the patients' charts. The vast majority of women had multiple active pain conditions and therefore we did not break down the pain conditions into categories, given the lack of information regarding the association between pain complaints and the reason for their pain clinic medical evaluation. Similar to prior work, current opioid prescription was evaluated as a dichotomous variable (yes/no); distinctions were not made for dosage levels, classes of opioids (e.g. long vs. short-acting), or prescription type (e.g., scheduled vs. PRN).19 Opioid prescription included the following medications: methadone, fentanyl, morphine, codeine, hydrocodone (with and without acetaminophen), oxycodone (with and without acetaminophen), and oxycodone. Tramadol and propoxyphene, considered weaker opioids, were excluded in accordance with the World Health Organziation pain ladder. Non-opioid prescription data were not abstracted.
Measure
Brief Pain Inventory-Short Form (BPI-SF)24
The BPI-SF is a self-report measure of pain intensity and pain interference widely used in clinical settings. Participants rate their current, worst, least and average pain intensities using an 11-point Numeric Rating Scale anchored by 0 = none and 10 = worst pain imaginable. The BPI-SF also assesses pain-related interference with functioning. Patients rate the degree to which pain interferes with functioning in the following life domains: mood, walking and other physical activity, work, relations with others, life enjoyment, sexual activity and sleep; higher ratings indicate greater degree of pain-related dysfunction. The combined mean of the functional items was used as a total pain-related dysfunction score. In previous research, the BPI-SF has been shown to discriminate among pain intensity levels and to be sensitive to change over time.24
Statistical Analyses
All analyses were performed using SAS software 9.2 (SAS Institute). Continuous variables were examined for normality using Q-Q plot, and variables with skewed distribution were categorized to dichotomous variables based on its median value such as average pain level and average of pain-related dysfunction scores. Factors that potentially associated with opioid prescription and patients characteristics by hysterectomy status were examined using Chi square for categorical variables and two-sample t test or Wilcoxon test for continuous variables. Multiple logistic regression analysis with stepwise model selection procedure was performed to identify the factors that may be independently associated with opioid prescription. A djusted odds ratios and their 95% CI were estimated based on the maximum likelihood method. Since the average score for the eight pain-related dysfunction domains was used in analyses above, we further evaluated the association of opioid prescription and hysterectomy with each of eight domains using a proportional odds logistic regression model. We further explored opioid prescription between hysterectomy groups by HRT status using the Chi Square test. All reported p values were two-sided, and p values less than 0.05 were considered significant.
Results
Study sample
Mean age for the sample was 35.6 (median=37.0; range=18-45). In terms of pain diagnoses, 53 women had diagnosed fibromyalgia or diffuse body pain. Of the remaining 265 women, 136 had one discrete pain condition (e.g., lumbosacral pain or cervical neck pain), 82 had two discrete pain conditions, 32 had three discrete pain conditions, 9 had four pain conditions, and six women had ≥ 5 pain conditions. Median pain intensity for the sample was 6.5 (range = 0-10), and half of the sample had pain intensity 7 or higher. Chronic non-pelvic pain was reported by 297 (92.0%) of the sample, and 26 women (8.0%) reported chronic pelvic pain. More than one-third of the sample were smokers. Opioid prescription was found for 66.2% of the sample. Prevalence of hysterectomy for the sample was 28.8% (N=93); median age of women with hysterectomy was 37.0 years. Date for hysterectomy was found for only 60% of the women who had the procedure (n=74). Of those, 61 (82%) underwent hysterectomy at least one year prior to pain clinic evaluation (surgical date range = 1-22 years since hysterectomy).
Sample characteristics by opioid prescription status
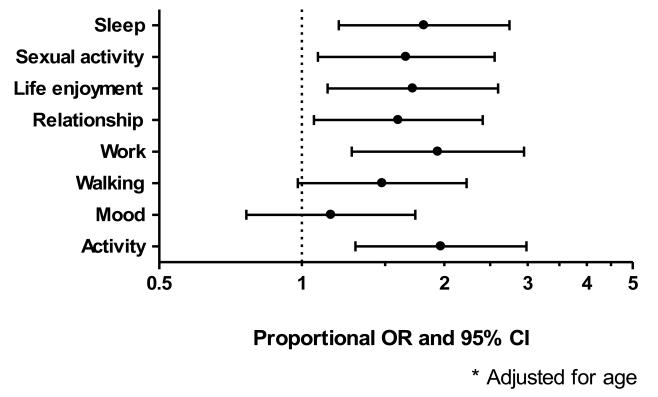
Table 1 provides results for the associations between the study variables and opioid prescription status. [insert table 1 about here] Hysterectomy (p=0.007), age (p=0.03), and average pain-related dysfunction (p=0.002) were significantly related to opioid prescription. There was no difference for HRT status between opioid prescription groups. The relationship between the individual components of this composite variable (activity, mood, walking, work, relationships with others, life enjoyment, sexual activity, and sleep) and opioid prescription were also examined and data are presented in Figure 1; opioid prescription was significantly associated with higher level of all components except for mood. [insert Figure 1 about here] We examined the relationship between hormone replacement therapy and opioid prescription. Similar results were found from logistic regression model for those taking and those not taking hormone replacement. We found that opioid prescription for hysterectomy with HRT was lower than for women with hysterectomy who were not taking HRT. We also found that average pain level was similar among groups.
Table 1.
Sample characteristics by opioid prescription status
| Opioid Prescription |
||||
|---|---|---|---|---|
| Factor | Overall | No Opioids | Opioids | P value |
| Participants | 323 | 109 (35.6) | 214 (66.3) | |
| Hysterectomy | 93 (28.8) | 21 (20.0) | 72 (33.6) | 0.007 |
| Hormone replacement therapy (HRT) | 37 (11.6) | 13 (11.5) | 24 (11.7) | 0.96 |
| Age (Range 18-45 years old) | ||||
| Median (inter-quartile) | 37 (30-42) | 34.5 (28.0-42.0) | 37.0 (31.0-43.0) | 0.03 |
| Age > 35 | 180 (56.3) | 52 (48.2) | 128 (60.4) | 0.04 |
| Average pain intensity (0-10) | ||||
| Median (Inter-quartile) | 6.0 (5.0- 7.0) |
6.0 (5.0-7.0) | 6.3 (5.0-8.0) | 0.09 |
| ≥7 | 157 (48.6) | 50 (48.9) | 107 (50) | 0.48 |
| Pelvic pain | 26 (8.1) | 10 (9.2) | 16 (7.5) | 0.60 |
| Smoking | 111 (34.4) | 31 (28.4) | 80 (37.4) | 0.11 |
| Average pain-related dysfunction score (0-10) |
||||
| Median (Inter-quartile) | 7.1 (5.4- 8.4) |
6.5 (4.8-7.9) | 7.4 (5.6-8.5) | 0.002 |
| ≥7 | 171 (53.4) | 47 (43.1) | 124 (58.8) | 0.008 |
Figure 1.
The association between opioid prescription and hysterectomy status by level of pain-related dysfunction
Comparison of study variables by hysterectomy status
Data in table 2 showed hysterectomy was potentially associated with opioid prescription (p=0.007), older age (p<.0001), and smoker status (p=0.04). [insert Table 2 about here] Table 2 also provides results for variables of interest from the BPI by hysterectomy status. Average pain intensity did not significantly differ by hysterectomy status. The average score for pain-related dysfunction did not achieve statistical significance (p=0.09). The relationship between hysterectomy status and each individual component of pain-related dysfunction was also examined. Hysterectomy was only associated with higher level of pain-related sexual dysfunction (Data not shown).
Table 2.
Comparison of study variables by hysterectomy status
| Factor | No Hysterectomy | Hysterectomy | P value |
|---|---|---|---|
| Participants | 230 | 93 (28.8) | |
| Opioid prescription | 138 (60.0) | 70 (75.3) | 0.007 |
| Hormone replacement therapy (HRT) | 10 (4.4) | 27 (29.0) | <.0.0001 |
| Age (Range 18-45 years old) | |||
| Median (inter-quartile) | 34 (29-40) | 40 (36-44) | <0.0001 |
| Age > 35 | 109 (48.0) | 71 (76.3) | <0.0001 |
| Average pain (1-10 scale) | |||
| Median (Inter-quartile) | 6.5 (5.0-8.0) | 6.0 (5.0-7.0) | 0.42 |
| 7 or higher | 115 (50.0) | 42 (45.2) | 0.43 |
| Pelvic pain | 17 (7.4) | 9 (9.8) | 0.50 |
| Smoking | 71 (30.9) | 40 (43.0) | 0.04 |
| Average pain-related dysfunction score (1-10) |
|||
| Median (Inter-quartile) | 7.0 (5.3-8.3) | 7.4 (5.8-8.5) | 0.10 |
| 7 or higher | 115 (50.4) | 56 (60.9) | 0.09 |
Factors associated with opioid prescription
Table 3 provides the odds ratios of opioid prescription for variables of interest (hysterectomy status, HRT status, age, smoking status, average pain intensity, and pelvic pain). [insert table 3 about here] Results showed hysterectomy, older age, and high levels of pain-related dysfunction were potentially associated with opioid prescription. Significant independent associations were detected for hysterectomy and high levels of pain-related dysfunction. Women with hysterectomy and high levels of pain-related dysfunction were almost twice as likely to have opioid prescription. More than 85% of women with hysterectomy and a high level of pain-related dysfunction were found to have opioid prescription.
Table 3.
Factors associated with opioid prescription
| Factor | Unadjusted OR | Adjusted OR | ||
|---|---|---|---|---|
| (95% CI) | P value | (95% CI) | P value | |
| Hysterectomy | 2.13 (1.22, 3.70) | 0.008 | 1.94 (1.12, 3.35) | 0.02 |
| Age > 35 | 1.64 (1.03, 2.62) | 0.04 | --- | --- |
| Smoking | 1.50 (0.91, 2.48) | 0.11 | --- | --- |
| Average pain intensity level ≥ 7 | 1.18 (0.74, 1.87) | 0.48 | --- | --- |
| Pelvic pain | 0.80 (0.35, 1.84) | 0.60 | --- | --- |
| Average pain-related dysfunction ≥ 7 | 1.88 (1.18, 3.00) | 0.008 | 1.70 (1.06, 2.70) | 0.03 |
| Hormone replacement therapy | 1.02 (0.50, 2.10) | 0.95 | --- | --- |
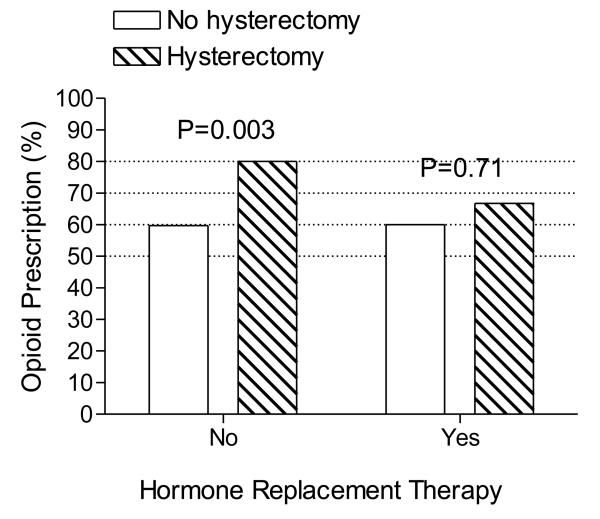
Based on previous reports that ovariectomy in rodents produced delayed and prolonged hyperalgesia, which was reversed by estrogen supplementation,25 we further explored this relationship in our study. We tested differences in pain intensity among four groups (Hysterectomy status by HRT status) and found no differences among the groups. However, in terms of opioid prescription, we found a significant difference for hysterectomy status (Hysterectomy and No hysterectomy) in women without HRT, but no significant difference for women taking HRT (see Figure 2). [insert Figure 2 about here] The proportion of opioid prescription in hysterectomy seems lower for women who were on HRT (66.8%) than for those who were not on HRT (80.0%) although this finding is not statistically significant. Insufficient sample size precluded formal examination of this relationship.
Figure 2.
The association between opioid prescription and hysterectomy status by HRT group.
Discussion
This study examined history of hysterectomy, chronic pain characteristics, pain-related dysfunction, HRT status, smoking status and opioid prescription for a sample of 323 women aged 18-45 seeking (but not yet receiving) specialized care in a chronic pain clinic. The prevalence of hysterectomy for this chronic pain sample was roughly 40% greater than for women in the same age range in the general population (28.8% and 17.5%, respectively). This finding suggests an overrepresentation of historical hysterectomy in young women referred for specialty chronic pain care. While one might suspect that increased pain intensity would account for the overrepresentation, our data did not support this hypothesis. We found that the average level of pain intensity were similar between women with hysterectomy and women who had not had the surgery, suggesting that other factors accounted for the disparity in referral patterns.
The primary pain type (lumbosacral) was similar between women with hysterectomy and women who had not had the surgery. While one perspective might hold that the hysterectomy may have influenced the development of a new pain condition via hormonal perturbation, it is equally possible that the non-pelvic pain reported by women with hysterectomy predated their surgery. Some research suggests that a chronic pain diathesis which predates hysterectomy significantly predicts post-surgical persistence of pain. Brandsborg et al reported results for 90 women who were followed 4-months after hysterectomy showed that 15 women (16.7%) reported persistent pelvic pain that affected daily living.26 Of those with post-hysterectomy chronic pelvic pain, 93.3% endorsed having preoperative non-pelvic pain. The strongest predictor for pelvic pain at 4 month follow-up was non-pelvic pain (coded as “pain problems elsewhere”) (p=0.004); age, previous pelvic surgery, Uterine Fibroid Symptom Score, type of hysterectomy and anesthesia were not associated with pain at 4-month follow-up. Among the 15 women with postsurgical pelvic pain, 11 had “pain likely to be continuing before the surgery” and 4 women reported “newly acquired pain” (scar pain or hematoma related to the surgery). The pain levels described in this sample were relatively low, with only 27% reporting pain ≥ 5 (0-10 Numeric Rating Scale). Therefore, while this study reports interesting information regarding predictors for post-hysterectomy pain, this sample may have milder pain than is typically seen for patients referred to specialty pain clinics.
We found that opioid prescription was independently associated with hysterectomy status, and pain-related dysfunction, but not with pain intensity. While the contribution of our description between historical hysterectomy and opioid prescription is novel, the other reported findings confirm prior work showing an association between opioid prescription and age,27 pain-related disability,28 and lack of an association with opioid prescription and pain intensity.19 Our hypothesis concerning hysterectomy and opioid prescription was confirmed in that hysterectomy was positively associated with opioid prescription, despite the lack of association with pain intensity. Results showed that pain-related dysfunction was significantly different for opioid vs. non-opioid prescription groups, such that greater levels of pain-related dysfunction were positively associated with opioid prescription. This finding dovetails with previous research in chronic pain populations that found that patient characteristics, such as pain-related functional impairment, significantly influenced receipt of opioids. One study on a sample of men and women seeking treatment in a pain clinic has underscored the influence of patient characteristics on physician prescribing patterns for opioids.19 The authors reported that while pain intensity did not predict opioid prescription in the sample, observed pain behaviors were a significant predictor for receipt of opioids. Given that other researchers have shown a significant association between pain behaviors and pain-related disability,29 it is possible that the association we found for opioid prescription and pain-related dysfunction was at least partially moderated by pain behaviors exhibited during medical visits. Future research may explore further the extent to which pain behaviors or other individual factors may influence physician decision making in prescribing opioids to women with hysterectomy. Therefore, the current findings may be added to the growing body of literature which suggests that individual characteristics strongly influence physician prescription for opioids; in this sense, the current findings are not new. However, our findings are novel in suggesting that women with hysterectomy are at greater risk for experiencing bias for prescription based on factors of dysfunction than other women seeking specialty chronic pain care. Interestingly, the absence of HRT in women with hysterectomy was related to opioid prescription, but this association was unrelated to pain intensity. However, it is possible that other factors known to be mediated by estrogen, such as anxiety, may influence patient behavior and therefore increase likelihood for opioid prescription.
Another factor of consideration is the possibility that women with hysterectomy may be more likely to be on chronic opioid therapy for pain prior to their hysterectomy, and would therefore support the ‘medical complexity’ hypothesis as a pathway to opioid prescription. We did not have relevant data available to examine this association. However, if true, the association between hysterectomy and opioid prescription may be the result of either pre-existing treatment patterns being carried forward, or potentially the synergistic effect between the negative effects of opioids (hyperalgesia and hormonal perturbation) and the negative hormonal effects from hysterectomy. One study of 1,135 women with hysterectomy (ages 33-88), showed an increased prevalence of opioids 4 months following hysterectomy (3.8% presurgery compared to 6.1% at 4-month follow-up).4 These figures may underestimate the association between hysterectomy and opioids, as longer follow-up is likely needed to document increases in pain and the development of new pain problems. Additionally, the age range for this sample was 33-88, with the vast majority of women already being post-menopausal and therefore having a history of hormonal disruption at time of their surgery. This distinction limits the ability to generalize the study findings to women who experienced abrupt hormonal changes at an unnaturally young age.
In contrast, however, the Brandsborg study reported that of 90 women with hysterectomy, only 3 were taking opioids preoperatively. This finding may be interpreted two ways. First, either women with hysterectomy are more likely to be prescribed chronic opioids in the post-surgical years (versus presurgically). A second possibility is that the pain clinic sample represents the subset of women with hysterectomy who are the most symptomatic, the most distressed by their pain, and the most likely to be prescribed opioids in the post-surgical years. As alluded to earlier, it is possible that women with hysterectomy and chronic pain may be more medically complex and more likely to access medical services and surgical intervention; however, these relationships remain empirically untested. Future research may study the differences between women with hysterectomy who develop chronic pain and women with hysterectomy who do not develop chronic pain to better determine the factors associated with chronic pain, as well as the patient, provider, and treatment factors which predict opioid prescription for the treatment of chronic pain.
The significance of our findings related to pain patient care are largely four-fold. First, our described overrepresentation of young women with hysterectomy presenting for chronic pain care is noteworthy and suggests that further research is needed to confirm this finding and describe the contributing factors. Second, we found that young women with hysterectomy are more likely to be prescribed opioids. While we acknowledge that more research is needed, prescribers may wish to more strongly consider alternatives to opioid prescription for these young women, given the specific negative effects of opioids in women with hysterectomy.13 Third, we found that pain-related dysfunction predicted opioid prescription in women with hysterectomy. The domains of pain-related dysfunction include interference with mood, sleep, relationships with others, sexual activity, general activity, walking and work. Efficacious non-pharmacologic pain interventions should be considered as preferrable alternatives to opioids, particularly for young women with hysterectomy. We highlight here that cognitive behavioral therapy has been shown to improve function in persons with chronic pain30 and may be particularly useful for subpopulations at high-risk for the iatrogenic effects of opioids. Fourth and last, our data suggest that hormone replacement is associated with lower likelihood for opioid prescription. Given the limitations of our sample size, further research is needed to confirm this association.
Our findings should be interpreted with caution, given that we describe associations only and not causal relationships. Regarding opioid prescription patterns, abstracted data did not include dosages or scheduling information. Therefore, one is cautioned against drawing conclusions regarding interpretation of opioid use versus prescription. Further research is needed to understand whether history of hysterectomy affects level of opioid use and/or response to opioid medication. Another limitation of the study is that abstracted hysterectomy data were not detailed enough to distinguish between surgical type (e.g., bilateral salpingo-oophorectomy vs. partial hysterectomy). As such, the association between hysterectomy, chronic pain, and opioid prescription may vary by surgical type. Finally, our findings regarding hysterectomy, HRT status, and opioid prescription are preliminary and only replication of results in future studies will firmly establish the associations described in this report.
In summary, close to one-third of younger women presenting for specialty pain care have had hysterectomy. Proper chronic pain care may include attention to the influence of hormonal factors on the pain experience, the heightened risk for the iatrogenic effect of opioids for these women, and the patient characteristics which influence prescribing patterns. Women with history of hysterectomy and high levels of pain-related dysfunction are significantly more likely to have an opioid prescription. More research is needed to clarify the factors which mediate opioid prescribing patterns, and to clarify the risks associated with opioid therapy in this relatively young subpopulation. Future research may determine best practices for chronic pain care considering the specific medical vulnerabilities of younger women with hysterectomy.
Acknowledgments
Funded by the Office of Research on Women's Health and the National Institute of Child Health and Human Development, Oregon BIRCWH grant number HD043488-06 (BD Darnall). We also wish to thank reviewers of an earlier version of this manuscript for their very helpful comments.
Contributor Information
Beth Darnall, Dept of Anesthesiology & Perioperative Medicine Oregon Health & Science University 3181 Sam Jackson Park Road, UHN-2 Portland, OR 97239.
Hong Li, Oregon Clinical and Translational Research Institute Biostatistics and Design Program Oregon Health & Science University 3181 Sam Jackson Park Road Portland, OR 97239.
References
- 1.National Institute for Health Statistics [Google Scholar]
- 2.Merrill RM. Hysterectomy surveillance in the United States, 1997 through 2005. Med Sci Monit. 2008 Jan;14(1):CR24–31. [PubMed] [Google Scholar]
- 3.Merrill RM, Layman AB, Oderda G, Asche C. Risk estimates of hysterectomy and selected conditions commonly treated with hysterectomy. Ann Epidemiol. 2008 Mar;18(3):253–260. doi: 10.1016/j.annepidem.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 4.Brandsborg B, Nikolajsen L, Hansen CT, Kehlet H, Jensen TS. Risk factors for chronic pain after hysterectomy: a nationwide questionnaire and database study. Anesthesiology. 2007 May;106(5):1003–1012. doi: 10.1097/01.anes.0000265161.39932.e8. [DOI] [PubMed] [Google Scholar]
- 5.Oltmanns KM, Fehm HL, Peters A. Chronic fentanyl application induces adrenocortical insufficiency. J Intern Med. 2005 May;257(5):478–480. doi: 10.1111/j.1365-2796.2005.01483.x. [DOI] [PubMed] [Google Scholar]
- 6.Vuong C, Van Uum SH, O'Dell LE, Lutfy K, Friedman TC. The effects of opioids and opioid analogs on animal and human endocrine systems. Endocr Rev. 2010 Feb;31(1):98–132. doi: 10.1210/er.2009-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch JL, Banks WA. Opiate modulation of IL-1alpha, IL-2, and TNF-alpha transport across the blood-brain barrier. Brain Behav Immun. 2008 Oct;22(7):1096–1102. doi: 10.1016/j.bbi.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Liang D, Shi X, Qiao Y, Angst MS, Yeomans DC, Clark JD. Chronic morphine administration enhances nociceptive sensitivity and local cytokine production after incision. Mol Pain. 2008;4:7. doi: 10.1186/1744-8069-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King T, Ossipov MH, Vanderah TW, Porreca F, Lai J. Is paradoxical pain induced by sustained opioid exposure an underlying mechanism of opioid antinociceptive tolerance? Neurosignals. 2005;14(4):194–205. doi: 10.1159/000087658. [DOI] [PubMed] [Google Scholar]
- 10.Hutchinson MR, Bland ST, Johnson KW, Rice KC, Maier SF, Watkins LR. Opioid-induced glial activation: mechanisms of activation and implications for opioid analgesia, dependence, and reward. ScientificWorldJournal. 2007;7:98–111. doi: 10.1100/tsw.2007.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gardell LR, King T, Ossipov MH, et al. Opioid receptor-mediated hyperalgesia and antinociceptive tolerance induced by sustained opiate delivery. Neurosci Lett. 2006 Mar 20;396(1):44–49. doi: 10.1016/j.neulet.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Fishbain DA, Cole B, Lewis JE, Gao J, Rosomoff RS. Do opioids induce hyperalgesia in humans? An evidence-based structured review. Pain Med. 2009 Jul-Aug;10(5):829–839. doi: 10.1111/j.1526-4637.2009.00653.x. [DOI] [PubMed] [Google Scholar]
- 13.Daniell HW. Opioid endocrinopathy in women consuming prescribed sustained-action opioids for control of nonmalignant pain. J Pain. 2008 Jan;9(1):28–36. doi: 10.1016/j.jpain.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Cairns BE. The influence of gender and sex steroids on craniofacial nociception. Headache. 2007 Feb;47(2):319–324. doi: 10.1111/j.1526-4610.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 15.Chapman CR, Tuckett RP, Song CW. Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions. J Pain. 2008 Feb;9(2):122–145. doi: 10.1016/j.jpain.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fillingim RB, Edwards RR. The association of hormone replacement therapy with experimental pain responses in postmenopausal women. Pain. 2001 May;92(1-2):229–234. doi: 10.1016/s0304-3959(01)00256-1. [DOI] [PubMed] [Google Scholar]
- 17.Fillingim RB, Ness TJ. Sex-related hormonal influences on pain and analgesic responses. Neurosci Biobehav Rev. 2000 Jun;24(4):485–501. doi: 10.1016/s0149-7634(00)00017-8. [DOI] [PubMed] [Google Scholar]
- 18.Braden JB, Sullivan MD, Ray GT, et al. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. Gen Hosp Psychiatry. 2009 Nov-Dec;31(6):564–570. doi: 10.1016/j.genhosppsych.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turk DC, Okifuji A. What factors affect physicians' decisions to prescribe opioids for chronic noncancer pain patients? Clin J Pain. 1997 Dec;13(4):330–336. doi: 10.1097/00002508-199712000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Sullivan MD, Edlund MJ, Zhang L, Unutzer J, Wells KB. Association between mental health disorders, problem drug use, and regular prescription opioid use. Arch Intern Med. 2006 Oct 23;166(19):2087–2093. doi: 10.1001/archinte.166.19.2087. [DOI] [PubMed] [Google Scholar]
- 21.Masson CL, Sorensen JL, Batki SL, Okin R, Delucchi KL, Perlman DC. Medical service use and financial charges among opioid users at a public hospital. Drug Alcohol Depend. 2002 Mar 1;66(1):45–50. doi: 10.1016/s0376-8716(01)00182-x. [DOI] [PubMed] [Google Scholar]
- 22.Cicero TJ, Wong G, Tian Y, Lynskey M, Todorov A, Isenberg K. Co-morbidity and utilization of medical services by pain patients receiving opioid medications: data from an insurance claims database. Pain. 2009 Jul;144(1-2):20–27. doi: 10.1016/j.pain.2009.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hooten WM, Townsend CO, Bruce BK, et al. Effects of smoking status on immediate treatment outcomes of multidisciplinary pain rehabilitation. Pain Med. 2009 Mar;10(2):347–355. doi: 10.1111/j.1526-4637.2008.00494.x. [DOI] [PubMed] [Google Scholar]
- 24.Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004 Sep-Oct;20(5):309–318. doi: 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Sanoja R, Cervero F. Estrogen modulation of ovariectomy-induced hyperalgesia in adult mice. Eur J Pain. 2008 Jul;12(5):573–581. doi: 10.1016/j.ejpain.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 26.Brandsborg B, Dueholm M, Nikolajsen L, Kehlet H, Jensen TS. A prospective study of risk factors for pain persisting 4 months after hysterectomy. Clin J Pain. 2009 May;25(4):263–268. doi: 10.1097/AJP.0b013e31819655ca. [DOI] [PubMed] [Google Scholar]
- 27.Williams RE, Sampson TJ, Kalilani L, Wurzelmann JI, Janning SW. Epidemiology of opioid pharmacy claims in the United States. J Opioid Manag. 2008 May-Jun;4(3):145–152. doi: 10.5055/jom.2008.0019. [DOI] [PubMed] [Google Scholar]
- 28.Turk DC, Okifuji A, Sinclair JD, Starz TW. Pain, disability, and physical functioning in subgroups of patients with fibromyalgia. J Rheumatol. 1996 Jul;23(7):1255–1262. [PubMed] [Google Scholar]
- 29.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain. 2000 Sep;87(3):325–334. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 30.Turner JA, Mancl L, Aaron LA. Short- and long-term efficacy of brief cognitive-behavioral therapy for patients with chronic temporomandibular disorder pain: a randomized, controlled trial. Pain. 2006 Apr;121(3):181–194. doi: 10.1016/j.pain.2005.11.017. [DOI] [PubMed] [Google Scholar]