Abstract
Background
Reactive oxygen species, such as hydrogen peroxide (H2O2), contribute to progression of dysfunction following myocardial infarction (MI). However, chronic overexpression studies do not agree with acute protein delivery studies. The purpose of the present study was to assess the temporal role of cardiomyocyte-derived H2O2 scavenging on cardiac function after infarction using an inducible system.
Methods and Results
We developed a tamoxifen-inducible, cardiomyocyte-specific catalase overexpressing mouse. Catalase overexpression was induced either 5 days pre or post-MI. Mice exhibited a 3-fold increase in cardiac catalase activity that was associated with a significant decrease in H2O2 levels at both 7 and 21 days. However, cardiac function improved only at the later time point. Pro-inflammatory and fibrotic genes were acutely upregulated after MI, but catalase overexpression abolished the increase, despite no acute change in function. This led to reduced overall scar formation, with lower levels of Collagen 1A and increased contractile Collagen 3A expression at 21 days.
Conclusions
In contrast to prior studies, there were no acute functional improvements with physiological catalase overexpression prior to MI. Scavenging of H2O2 however, reduced pro-inflammatory cytokines and altered cardiac collagen isoforms, associated with an improvement in cardiac function after 21 days. Our results suggest that sustained H2O2 levels, rather than acute levels immediately following MI, may be critical in directing remodeling and cardiac function at later time points.
Keywords: myocardial infarction, oxidative stress, hydrogen peroxides, catalase
Congestive heart failure is a leading cause of morbidity and mortality in the United States and worldwide. The dominant cause of congestive heart failure is loss of myocardium due to coronary artery disease and subsequent occlusion. The resulting myocardial infarction (MI) induces apoptosis, an exacerbated immune response, fibroblast proliferation, and ultimately scar formation and myocyte hypertrophy. While exact mechanisms behind these processes are still being examined, the increase in oxidative stress following MI is thought to play a critical role in many of these events. Some potential sources of the elevated reactive oxygen species (ROS) following acute MI include cardiac fibroblasts, invading neutrophils, and cardiomyocytes. Regardless of the source, scavenging ROS following acute MI remains an attractive therapeutic goal.
Hydrogen peroxide (H2O2) is a potent signaling molecule generated mainly from the dismutation of two superoxide radicals by superoxide dismutase (SOD). The normal myocardium contains antioxidant proteins that act to scavenge H2O2 mainly catalase, glutathione peroxidase, and peroxiredoxin. While not the only system that regulates H2O2 levels in the myocardium, catalase accounts for nearly 80% of all peroxidase activity in cardiomyocytes 1. Excess levels of H2O2 produce negative effects such as lipid peroxidation, apoptosis, and cardiac fibrosis in the myocardium, all of which aid in the progression to heart failure 2. Moreover, H2O2 stimulates the production of pro-inflammatory cytokines such as transforming growth factor beta (TGFβ), tumor necrosis factor alpha (TNFα), and interleukin 6 (IL-6) in activated cardiac fibroblasts 3. These cytokines alter the production of collagen deposited in the extracellular matrix (ECM) in and surrounding the injured myocardium to replace the apoptotic cardiomyocytes. The rise in collagen deposition by H2O2 may impair chronic cardiac function.
Following myocardial infarction, there is a selective change in antioxidant levels. Catalase levels, while stable initially, decrease over time, whereas glutathione peroxidase remains unchanged 4. As most of the peroxidase activity in myocytes is from catalase, this significant change can drastically alter redox balance in the myocardium and makes a strong case for the restoration of catalase levels in the myocardium as an attractive therapeutic option. Indeed, many therapies that improve cardiac function following acute MI also increase catalase levels 5, 6. Additionally, cardiac catalase overexpression was shown to prevent doxorubicin-induced cardiotoxicity and protect against ischemia/reperfusion (IR) injury in mice 1, 7. While the study demonstrated a critical role for H2O2-scavenging by catalase in the post IR setting, the mice studied had supraphysiological (90-fold) overexpression of catalase from birth, two conditions quite unlikely in the human pathology. Adding to the controversy, when catalase protein was delivered directly following IR there was no improvement noted 8, 9. Finally, in a model of heat-shock induced cardioprotection, inhibition of catalase with 3-aminotriazole (3-AT) had no effect on infarct size 10.
To determine the role for catalase in post-infarct healing, we created a cardiomyocyte-specific, tamoxifen-inducible catalase overexpressing mouse to assess the role of H2O2 on cardiac function after MI at different times along the disease process. Our results demonstrate only modest protection at early time points when catalase is induced prior to MI. When catalase is induced a few days after MI, although there is no improvement in cardiac function, acute levels of inflammatory and fibrotic genes are decreased and there is a change in collagen isoforms expression ratio. These mechanistic changes led to an improvement in function at later time points and suggest timing must be carefully considered for sustained delivery of catalase.
Methods
Generation of cardiac-specific, inducible catalase overexpressing mice
The laboratory of Dr. W. Robert Taylor has generated a transgenic mouse that expresses human catalase under the control of the CX1 promoter. In front of the catalase gene, there is a floxed green fluorescent protein (GFP) sequence with a stop codon 11. These mice were crossed with mice containing cre recombinase under control of the alpha-myosin heavy chain promoter and a mutant estrogen receptor element (Mer-Cre-Mer, Jackson Labs; Stock #005650) to create a new double-transgenic mouse. All mice were on a C57BL6 background and genotyped for presence of both human catalase and cre recombinase as described 11, 12.
Induction of catalase overexpression
Adult, male mice were injected intraperitoneally (40 mg/kg) with tamoxifen (Sigma) dissolved in sunflower oil as described 12, or sunflower oil alone for a period of 5 days.
Measurement of catalase activity
Protein extracts were incubated with 50 μmol/L hydrogen peroxide and subjected to kinetic readings of absorbance at 240 nm. Absorbance was converted to concentration using Beer’s law and rates of decomposition were determined by subtracting the 3 minute concentration from the initial reading to get a rate. One unit was defined as decomposing 1 μmol/L of hydrogen peroxide per minute.
Hydrogen peroxide measurements
Hydrogen peroxide levels were determined using Amplex Red assay (Invitrogen).
Myocardial infarction
Adult male mice 8-12 weeks old were subjected to myocardial infarction surgeries by ligation of the left anterior descending coronary artery for 30 minutes followed by reperfusion as described 13. All studies were performed in a randomized and blinded manner and were approved by the Emory University Institutional Animal Care and Use Committee.
Cardiac function
Animals were placed under light anesthesia (Isoflurane, Webster Veterinary) and both M-mode and B-mode echocardiography were performed using a Vevo 770 microimaging system (VisualSonics). Measurements were taken from at least 5 cardiac cycles at peak systole and diastole to determine fractional shortening ,ejection fraction, end-systolic and end-diastolic volume, and left ventricular mass 13.
Real-Time PCR
Tissue homogenates were prepared using Trizol (Invitrogen) and RNA extracted per manufacturers protocol. Templates of cDNA were made with a commercially available kit (Applied Biosciences) and primers were designed using PrimerExpress (Applied Biosciences). Gene expression was determined using SYBRGreen and a thermal light cycler (Roche).
Collagen evaluation
Collagen deposition was determined by Picrosirius Red (Sigma) staining as previously described 14. Briefly, 5 μm tissue sections were stained with Sirius Red and imaged using a light microscope. Total collagen area (red staining) was normalized to total LV area in 3 separate sections per animal using ImageJ.
Statistics
All statistical analyses were performed using Graphpad Prism software as described in the figure legends. To determine differences between multiple groups, one-way analysis of variance (ANOVA) was used. If significant differences were found, Tukey-Kramer post-tests were performed and reported. Data reported are mean ± SEM.
Results
Development of the inducible, cardiac-specific catalase overexpressing mouse
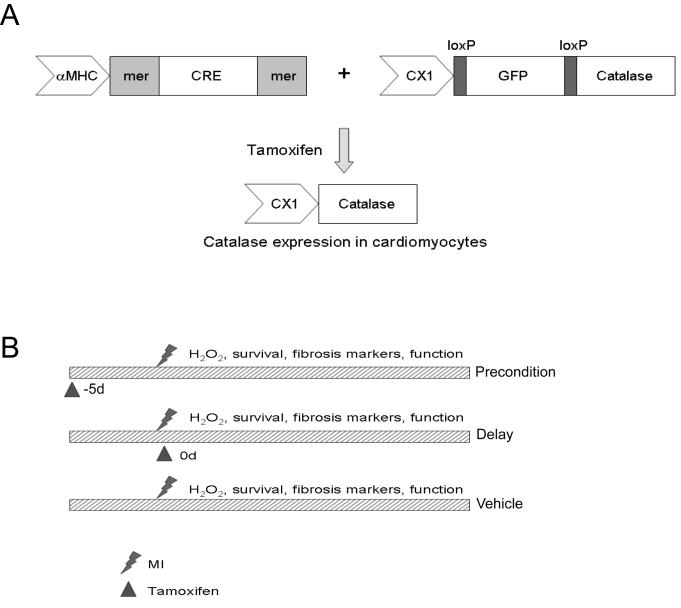
We developed an inducible, cardiac-specific catalase overexpressing mouse by crossing tamoxifen inducible, alpha myosin chain driven Mer-Cre-Mer mice with mice containing a transgene for human catalase driven by the chicken beta-actin promoter. The transgene contained a floxed green fluorescent protein and stop codon before the catalase gene, thus catalase overexpression is not active until cre-mediated excision (Figure 1A). All mice were genotyped to confirm presence of the transgenes as previously described 11, 12. Using this method, we were able to create 2 different conditions; preconditioned and delayed catalase induction (Figure 1B). Specifically, preconditioning indicates that tamoxifen was given for 5 days and surgery performed on the 7th day; delayed indicates that tamoxifen treatment was initiated immediately following MI.
Figure 1. Study design for creation of transgenic mice and catalase induction before and after myocardial infarction (MI).
A) Transgenic approach for inducible catalase overexpression in cardiomyocytes (MHC=myosin heavy chain, MER=mutant estrogen receptor; CX1=chicken β-actin promoter; GFP=green fluorescent protein). B) Schematic demonstrating overall plan for determining importance of timing in catalase therapy. Catalase overexpression was induced (triangle) at various times beforeand after infarction.
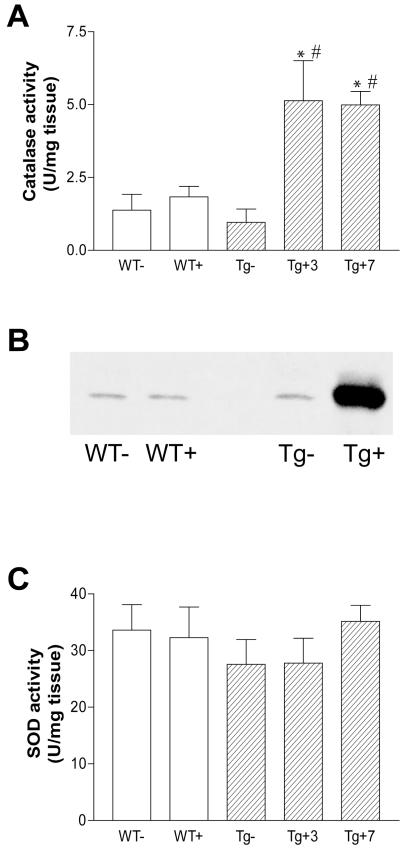
In order to determine whether these mice inducibly overexpressed catalase in the heart, we injected adult male mice with either vehicle or tamoxifen (40 mg/kg) intraperitoneally once daily for 5 days. Mice were sacrificed 3 and 7 days following cessation of tamoxifen treatment and assayed for catalase activity and protein expression. While there was no change in catalase levels in non-cardiac tissue (data not shown), catalase activity was significantly higher in the tamoxifen-treated transgenic mice compared to wild type or vehicle-treated transgenic mice and there was no significant increase between 3 and 7 days after tamoxifen cessation (Figure 2A). This increase was completely blocked by incubation of the sample with 3-AT, suggesting the increase was due to catalase and not another peroxidase (Supplemental Figure 1A). We also observed an increase in catalase protein expression in tamoxifen-treated transgenic mice, confirming that the increase in activity was due to protein overexpression (Figure 2B). To determine whether increases in catalase altered other antioxidant systems, we examined SOD activity in tamoxifen-treated animal hearts. As the data in Figure 2C demonstrate, cardiac SOD activity was equal among all groups, suggesting alterations in cardiac catalase did not affect SOD levels. Taken together, our findings demonstrate that we developed a novel, inducible murine model that overexpresses human catalase specifically in cardiomyocytes to modest levels.
Figure 2. Antioxidant enzyme activity and expression in mice after tamoxifen treatment.
A) Bar graph (mean ± SEM ) showing an increase in cardiac catalase activity only in transegenic (Tg) with tamoxifen injections (+) at multiple time points, but not in WT or nontreated (−) mice. Animals were treated with tamoxifen for 5 days prior to either a 3 day (Tg+3) or 7 day (Tg+7) waiting period. B) Representative immunoblot of cardiac homogenates demonstrate an increase in catalase protein only in tamoxifen-treated and not WT or vehicle-treated mice. C) Cardiac SOD was not affected by induction of catalase and activity was similar in all groups tested. Statistical comparisons were made by ANOVA (p=0.0002) followed by Tukey-Kramer post-test. *p<0.01 vs. WT+, #p<0.05 vs. WT. n = 4-9 hearts per group.
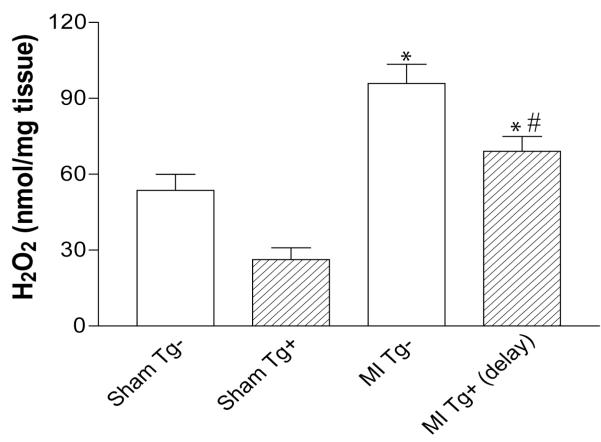
H2O2 production in myocardium
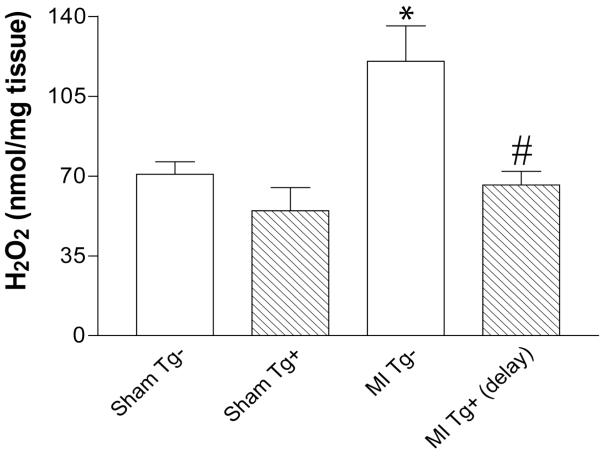
To determine whether increased cardiomyocyte catalase levels could reduce H2O2 levels, we subjected adult male mice to MI injury and examined H2O2 levels at 7 days in the left ventricular free wall (LV). Vehicle-treated transgenic mice subjected to MI surgery exhibited a significant increase in H2O2 over sham animals as measured by Amplex Red (Figure 3). Cardiomyocyte-specific catalase overexpression significantly decreased cardiac H2O2 levels to sham values (Figure 3). These data suggest that cardiomyocyte-specific overexpression of catalase completely prevents increases in H2O2 levels in the infarcted tissue following MI.
Figure 3. Scavenging of H2O2 by catalase overexpression.
H2O2 production 7 days post-MI in left ventricular free wall (mean ± SEM ). H2O2 production was measured in cardiac tissue from vehicle (Tg−) and tamoxifen (Tg+) treated mice using Amplex Red assay. MI significantly increased H2O2 levels and this was normalized in delayed catalase overexpressing mice. Statistical comparisons were made by ANOVA (p=0.002) followed by Tukey-Kramer post-test. *p<0.05 vs. respective sham; #p<0.05 vs. vehicle treated MI mice. n = 4-8 hearts per group.
Acute protective actions of myocyte-derived catalase
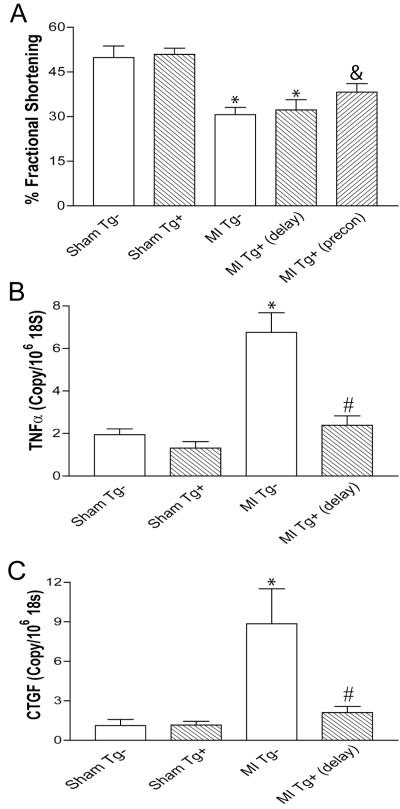
In order to evaluate the effect of timing for catalase induction, we assessed the outcome of preconditioned and delayed cardiac catalase induction on cardiac function following MI. Fractional shortening (FS) was measured as an index of cardiac function at 7 days following MI. As a prior study has suggested that the presence of cre may affect cardiac function 15, we examined vehicle-treated transgenic mice subjected to sham and MI surgery and found no significant difference in function compared to wild-type mice (Supplemental Figure 1B); thus we used vehicle-treated transgenic mice as controls in subsequent studies. We observed a significant decrease in FS at 7 days in vehicle-treated transgenic mice subjected to MI (Sham/Tg−: 49.8±3.9% vs. MI/Tg−: 30.7±2.4%; p<0.01). Delayed catalase overexpressing mice also demonstrated significantly reduced function compared to sham animals (MI/Tg+: 50.9±2.0% vs. MI/Tg+ delayed: 32.2±3.4%; p<0.01) (Figure 4A). Interestingly, the preconditioning group demonstrated a trend toward improvement but was not statistically different from vehicle-treated MI mice (MI/Tg+ preconditioned: 38.2±2.8%; p>0.05). Infarct size as measured by delayed contrast enhancement following magnetic resonance imaging 16 was not different among the groups (Supplemental Figure 2).
Figure 4. Cardiac function and gene expression 7 days post-MI in left ventricular free wall.
A) Fractional shortening as a measure of cardiac function was significantly decreased after MI in vehicle treated animals (Tg−) as compared with sham operated mice with no effect of preconditioned or delayed catalase overexpression (Tg+). B) TNFα mRNA levels were quantified in the left ventricle, and catalase induction significantly lowered the MI-induced increase of the pro-inflammatory molecule. C) The pro-fibrotic cytokine CTGF was higher in the Tg− group, but was significantly reduced by catalase overexpression. Statistical comparisons were made by ANOVA (A, p<0.05; B, p=0.0048; C, p<0.0001) followed by Tukey-Kramer post-test. *p<0.01 vs. respective sham, &p<0.05 vs. respective sham, #p<0.05 vs. vehicle-treated MI mice. n = 4-10 hearts per group. All data are mean ± SEM.
To determine whether delayed catalase induction had any biochemical benefits we examined the regulation of pro-inflammatory and pro-fibrotic genes in the LV homogenates using real-time PCR 7 days following MI. Both TNFα and connective tissue growth factor (CTGF) were both significantly upregulated in vehicle-treated MI mice compared to sham animals (Figure 4B-C). Scavenging of H2O2 significantly abolished the increase of both TNFα and CTGF by approximately 65% and 76%, respectively (Figure 4C). Taken together, these data demonstrate there is no statistically significant beneficial effect in cardiac function though even delayed reduction in H2O2 levels had underlying biochemical effects.
Chronic protective actions of myocyte-derived catalase
To determine chronic H2O2 scavenging ability of delayed cardiomyocyte-catalase overexpression, we measured H2O2 levels 21 days following infarction. Similar to the 7 day results, vehicle-treated, transgenic MI mice at 21 days exhibited a significantly greater level of H2O2 compared to the sham animals (Figure 5). While sham transgenic mice treated with tamoxifen had similar baseline levels, delayed catalase overexpression significantly (p<0.05) decreased MI-induced H2O2 levels, suggesting catalase is still active at 21 days post-treatment.
Figure 5. Chronic scavenging of H2O2 by catalase overexpression.
H2O2 production was measured in cardiac tissue (mean ± SEM) from vehicle (Tg−) and tamoxifen (Tg+) treated mice using Amplex Red assay 21 days post-MI. MI significantly increased H2O2 levels and catalase overexpression normalized this response. Statistical comparisons were made by ANOVA (p<0.0001) followed by Tukey-Kramer post test. *p<0.01 vs. respective sham, #p<0.05 vs. vehicle-treated MI mice. n = 5-9 hearts per group.
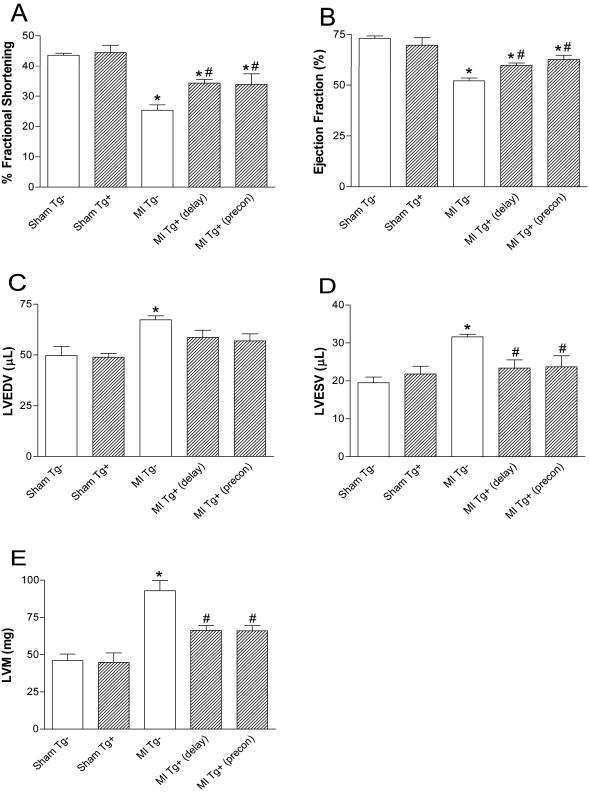
Due to the biochemical improvements seen early with a lack of functional improvements at 7 days, we sought to determine the functional effect of catalase overexpression at 21 days. Similar to 7 days, MI significantly decreased FS in vehicle-treated mice (p<0.001); however both preconditioned (p<0.05) and delayed (p<0.01) catalase overexpression significantly improved this parameter (Figure 6A). Ejection fraction was also measured in these animals and similar results were obtained (Figure 6B). While there was a trend toward an improvement in end-diastolic volume, there were no significant changes with catalase overexpression; however significant improvements in end-systolic volumes were seen with preconditioned (p<0.05) and delayed (p<0.05) catalase overexpression (Figures 6C&D). Finally, there was a significant improvement in LV mass in both preconditioned (p<0.05) and delayed (p<0.05) catalase overexpression (Figure 6E). These data demonstrate that despite no effect of catalase overexpression on acute function, both preconditioned and delayed catalase overexpression significantly improved function during the chronic phase of myocardial infarction to the same degree.
Figure 6. Cardiac function 21 days post-MI.
A) Fractional shortening, B) ejection fraction, C-D) end-systolic and end-diastolic left ventricular volume (LVESV and LVEDV), and E) left ventricular mass (LVM) between various groups as measured by small animal echocardiography. Both delayed and preconditioned (precon) catalase overexpression (Tg+) significantly improved indicated measurements of cardiac function at 21 days compared to vehicle treated MI mice (Tg−). Statistical comparisons were made by ANOVA (A, p<0.0001; B p<0.0001; C,D, p=0.005; E, p<0.0001) followed by Tukey-Kramer post test. *p<0.05 vs. respective sham; #p<0.05 vs. vehicle-treated MI. n≥5 animals per group. All data are mean ± SEM.
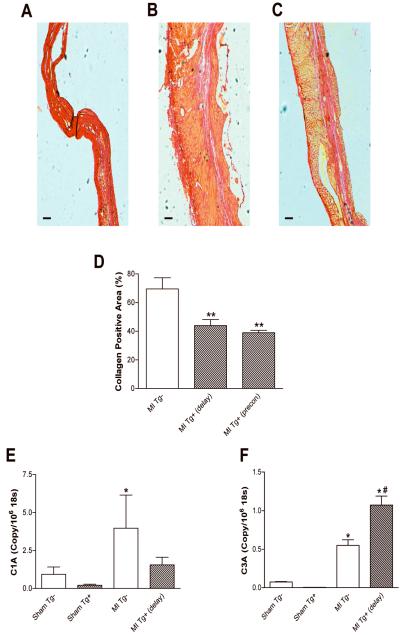
Potential mechanism of chronic improvement
To determine levels of fibrosis, heart sections were stained with Sirius Red 21 days post-infarction and fibrotic scar area was normalized to total LV area. Representative sections for MI/Tg−, MI/Tg+ delayed, and MI/Tg+ preconditioned are shown in Figures 7A-C. Grouped data demonstrate a significant reduction in scar area with both catalase overexpressing mice (Figure 7D). Collagen 1A and 3A are the two major collagen isoforms expressed in the heart and newly deposited scar tissue. We observed that the vehicle-treated, transgenic MI mice at 21 days had a significant increase in collagen 1A mRNA levels compared to the vehicle-treated, transgenic sham mice (Figure 7E). Induction of catalase showed a trend for lower collagen 1A levels compared to the vehicle-treated, transgenic mice at 21 days post-MI (MI/Tg−: 4.0±2.2 vs. MI/Tg+: 2.1±0.56; p>0.05) (Figure 7E). On the other hand, the contractile collagen 3A mRNA expression in the tamoxifen-treated MI mice at 21 days, was significantly (p<0.05) increased compared to vehicle-treated MI mice (Figure 7F). Taken together, these data demonstrate that chronic catalase overexpression not only reduces total collagen content, but alters collagen isoforms expression as well.
Figure 7. Collagen staining and subtype mRNA expression 21 days post-MI in left ventricular free wall.
A-C) Representative photographs of left ventricles from A) MI Tg−, B) MI Tg+ delay, and C) MI Tg+ precon stained with picrosirus red for collagen levels. Red = collagen fibers. Scale bar is 500 microns. D) Grouped data from Sirius red staining showing that both delayed and preconditioned (precon) catalase overexpression (Tg+) significantly decreased collagen staining at 21 days compared to vehicle treated MI mice (Tg−). E) Collagen 1A was significantly increased in vehicle-treated MI mice compared to sham with no significant effect of catalase overexpression. F) Collagen 3A, while increased significantly after MI in vehicle-treated mice, was significantly increased even further with catalase overexpression. Statistical comparisons were made by ANOVA (D, p=0.0124; E, p=0.0108; F, p=0.0003) followed by Tukey-Kramer post test. *p<0.05 vs. respective sham; **p<0.05 vs. MI Tg−; #p<0.05 vs. vehicle-treated MI. n = 3–13 hearts per group. All data are mean ± SEM.
Discussion
In this study we used an inducible, tissue-specific, transgenic mouse model to determine temporal effects of physiological catalase overexpression on post-infarct healing. Our findings indicate that physiological catalase overexpression, while decreasing cardiac H2O2 levels, had no significant effect on cardiac function at 7 days post-infarction even if the gene was induced prior to injury. If induction was delayed, there were significant changes in pro-inflammatory and pro-fibrotic gene expression, leading to functional improvements at later time points. The data suggest that there is little-to-no benefit for initiating catalase protein therapy immediately following infarction, and that sustained scavenging of H2O2 may be critical.
We generated these new double-transgenic mice by crossing two existing transgenic mice, the well established alpha myosin heavy chain Mer-Cre-Mer mouse 17, with a mouse containing a floxed stop codon between GFP and the human catalase gene 11. We found no significant changes between wild-type mice and double transgenic mice treated with vehicle, indicating very little leakage of the gene. Additionally, prior studies from the Mer-Cre-Mer mice demonstrated very low levels of leakage by reporter gene detection, less than 1% at 2 months, and less than 2% even after a year 14. Administration of tamoxifen for 5 days with a 3 day waiting period induced expression of catalase only in the heart and the increase in activity was completely abolished by 3-AT, indicating no other peroxidase was involved. Longer time periods (7 days) produced no further changes, reinforcing that leakage was very low as recombination did not continue, and there was no regression of increased catalase activity. This increase in cardiac catalase was modest in comparison to prior studies with catalase overexpression in the heart that produced >90-fold increase in catalase activity from birth 1, 7. This is especially important as our data in Figure 5 show that even with 3 weeks of physiological catalase overexpression, basal H2O2 levels were reduced.
Recent reports have shown that tamoxifen, independent of its cre translocating ability, may induce cardiomyopathy in certain mouse models 15. As this study generated a new double-transgenic mouse, Mer-Cre-Mer mice treated with tamoxifen were not examined alone. Despite this potential issue, all mice were compared to wild-type mice (Supplemental Figure 1) and recommendations of the prior study were followed including reduced dosing of tamoxifen (40 mg/kg used in this study, compared with 80 mg/kg reported to cause cardiomyopathy) and a waiting period. Despite our comparison of both tamoxifen and vehicle treated MI mice to wild-type mice and reduced dosage, it may be possible that non-specific tamoxifen effects may add confounding variables to the study and future experiments may include raloxifen-treated mice as well.
Using these mice, we created two conditions; the first we termed preconditioned as tamoxifen was given for 5 days (with a 3 day waiting period) prior to surgery and the second was termed delayed overexpression as tamoxifen treatment was initiated at the conclusion of surgery for 5 days thereafter. Levels of LV H2O2 were significantly increased at 7 days post-infarction and delayed catalase induction was able to scavenge this potentially toxic species, suggesting that even delayed catalase overexpression in cardiomyocytes was sufficient to reduce H2O2 levels in the injured myocardium. However, despite this significant decrease in H2O2 concentrations, there was no acute improvement in cardiac function in either the delayed or preconditioned mice. This is in contrast to prior studies demonstrating acute functional improvements in cardiomyocyte-catalase overexpressing mice 1. Given the strong role of H2O2 as a vital second messenger in healthy tissues, it is quite possible that these studies overexpressing catalase to such high levels for prolonged periods of time abolished basal H2O2 signaling in the heart, leading to alterations in many pathways. In fact, many contractile and calcium regulating proteins are redox sensitive, thus the potential for chronic alterations in myocyte function are significant 18-22. In keeping with our findings, catalase protein therapy studies demonstrated little effect of catalase protein delivery at acute time points in preventing myocardial injury 23, 24. Supporting the lack of effect are studies showing improvements in function with post-conditioning with no effect on myocardial catalase levels.
Although, we did not observe an improvement in cardiac function at 7 days with catalase overexpression, there were underlying biochemical changes evident in the delayed catalase overexpression group. An additional effect observed acutely after MI is the progression of inflammation localized in and around the infarcted zone. Infiltrating cells and cardiomyocytes contribute to the inflammation by synthesizing and releasing pro-fibrotic and pro-inflammatory molecules 25, 26. These inflammatory molecules are upregulated by H2O2 in a short and temporal manner to initiate the remodeling process 27-30. Therefore, we analyzed whether the reduction in H2O2 in our model altered cytokine expression. Similar to published studies, we found that both TNFα and CTGF mRNA levels were significantly increased during the acute phase of MI compared to sham animals by approximately 350% and 800%, respectively 27, 28, 31, 32. These two molecules play a critical role in LV remodeling after MI by positively regulating processes such as apoptosis and collagen deposition. Overexpression of cardiac-derived catalase abolished the increase in both of these markers and returned message levels to that of the sham group. H2O2 has been shown to be an important mediator of TNFα-induced cellular damage and dysfunction in isolated ventricular myocytes 29. It was shown that, in vitro, H2O2 is a potent stimulator of CTGF expression, and our data demonstrate a potential role for this regulation in vivo 28.
Next, we assessed chronic H2O2 scavenging ability and cardiac function with cardiomyocyte-specific overexpression of catalase following MI. Evaluation of cardiac H2O2 levels at 21 days post MI indicated that overexpression of catalase was still present and the enzyme continued to significantly scavenge elevated levels of H2O2 seen in vehicle-treated mice. The delayed MI groups expressed significantly lower H2O2 concentrations than vehicle MI mice. Our data is in agreement with prior catalase overexpression studies in which catalase overexpressing mice continued to express active catalase long term 1, 7. Interestingly, sham mice treated with tamoxifen demonstrated a reduction in basal H2O2 levels over the course of the study, though it did not reach statistical significance. These data underscore the need for inducible systems to examine the effect of catalase overexpression, as chronic basal reduction of H2O2 levels could serve as a confounding variable by altering normal signaling pathways. Chronic scavenging of H2O2 led to an improvement in several measures of cardiac function in both delayed and pretreated mice, suggesting that sustained scavenging may be more important than immediate reductions in H2O2. These data are in contrast with other oxidants such as superoxide, which peaks quite early in the injury process and immediate scavenging may be beneficial 13. Mechanistically, early scavenging of H2O2 may play more of a role in the inhibition of pro-inflammatory and pro-fibrotic signaling molecules than in acute cell death.
In addition supraphysiological overexpression of cardiac-specific catalase from birth has been found to significantly attenuate age-induced contractile dysfunction and damage to the myocardium 19. We show that these early biochemical changes resulted in an improvement in cardiac remodeling by altering both the total collagen content of the tissue as shown by Sirius Red staining, as well as the collagen isoform content of the scar tissue. In fact, regulation of CTGF is critical in determining cardiac fibrosis during hypertrophy and plays an important role in upregulating collagen 1A levels following MI 27, 31, 33-35. Moreover, H2O2 may play an important role in regulating collagen cross-linking and tensile strength during diabetes, reducing contractility 36. We show in our inducible cardiomyocyte-specific catalase overexpressing mice that the improvement in cardiac function may be the result of the collagen 1A being replaced with the less stiff collagen 3A. Prior studies demonstrate that collagen 3A:1A ratios may play an important role in the contractile function of the heart in animal and human studies and this may be a potential mechanism in the systolic functional improvements seen with catalase overexpression 33-35, 37.
In summary, we found that inducible, cardiomyocyte-specific catalase overexpression significantly upregulated the expression and activity of the enzyme to physiologically-relevant levels. MI significantly elevated H2O2 concentrations that were lowered by catalase overexpression, persisting for the duration of the study. We also demonstrated that lower H2O2 levels significantly decreased pro-inflammatory and pro-fibrotic markers acutely; although cardiac function was not improved 7 days post-MI. In contrast, improvements in cardiac function were observed at 21 days post-MI, which was associated with a change in collagen isoform expression. Cardiac-derived catalase overexpressing mice exhibited reduced scar tissue and higher amounts of the more contractile collagen 3A isoform, which may play a critical role in the improvement seen in systolic cardiac function at the later time point. We conclude that the temporal aspect of scavenging cardiac H2O2 after myocardial infarction is a critical variable, and despite lack of efficacy of protein delivery immediately following MI, efforts should be made for sustained scavenging over time to promote the healing process.
Clinical Perspective.
Congestive heart failure is a leading cause of morbidity and mortality worldwide and effective treatment options are greatly needed. Reactive oxygen species (ROS) increase greatly after myocardial infarction are thought to be a potential therapeutic target. While some studies using genetic manipulation have shown promise, protein delivery studies of antioxidants have demonstrated mixed results. One potential reason could be that genetic overexpression studies examine chronically supra-physiological levels of antioxidant therapy and could include preconditioning effects. To negate this, we created a mouse model of catalase overexpression that was both tissue-specific and inducible. By using tamoxifen, we could turn on physiologically relevant levels of catalase at different time points only in cardiomyocytes. The data in this manuscript demonstrated that there was little benefit to acute cardiac function if catalase overexpression was induced at the same time of injury. However, there were underlying biochemical changes to fibrosis-related genes that manifested in to chronic improvements in function. Regardless of when catalase was induced, overall scar formation was reduced, and more contractile collagen isoforms were present. This led to increases in ejection fraction, left ventricular mass, and end-systolic function. Taken together, our data showed that the sustained presence of catalase, rather than acute induction, could be an important modulator of post-infarction healing. Thus, for future therapy involving antioxidants, it may be prudent to improve the delivery to account for sustained release, rather than focusing efforts on acute administration.
Supplementary Material
Sources of Funding
This work was supported by grants from the NIH (HL094527; MED, HL007745; KDP and KMR, and HL090584; WRT), as well as a postdoctoral fellowship from the American Heart Association (09POST2060589; KMR).
Footnotes
Disclosures None.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Li G, Chen Y, Saari JT, Kang YJ. Catalase-overexpressing transgenic mouse heart is resistant to ischemia-reperfusion injury. Am J Physiol. 1997;273:H1090–1095. doi: 10.1152/ajpheart.1997.273.3.H1090. [DOI] [PubMed] [Google Scholar]
- 2.Sam F, Kerstetter DL, Pimental DR, Mulukutla S, Tabaee A, Bristow MR, Colucci WS, Sawyer DB. Increased reactive oxygen species production and functional alterations in antioxidant enzymes in human failing myocardium. J Card Fail. 2005;11:473–480. doi: 10.1016/j.cardfail.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Souders CA, Bowers SL, Baudino TA. Cardiac fibroblast: The renaissance cell. Circ Res. 2009;105:1164–1176. doi: 10.1161/CIRCRESAHA.109.209809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khaper N, Kaur K, Li T, Farahmand F, Singal PK. Antioxidant enzyme gene expression in congestive heart failure following myocardial infarction. Mol Cell Biochem. 2003;251:9–15. [PubMed] [Google Scholar]
- 5.Ozdemir R, Parlakpinar H, Polat A, Colak C, Ermis N, Acet A. Selective endothelin a (eta) receptor antagonist (bq-123) reduces both myocardial infarct size and oxidant injury. Toxicology. 2006;219:142–149. doi: 10.1016/j.tox.2005.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Zhu YZ, Chong CL, Chuah SC, Huang SH, Tong HT, Nai HS, Whiteman ML, Moore PK. Cardioprotective effects of nitroparacetamol and paracetamol in the acute phase of myocardial infarction in experimental rats. Am J Physiol Heart Circ Physiol. 2006;290:H517–H524. doi: 10.1152/ajpheart.00572.2005. [DOI] [PubMed] [Google Scholar]
- 7.Kang YJ, Chen Y, Epstein PN. Suppression of doxorubicin cardiotoxicity by overexpression of catalase in the heart of transgenic mice. J Biol Chem. 1996;271:12610–12616. doi: 10.1074/jbc.271.21.12610. [DOI] [PubMed] [Google Scholar]
- 8.Jeroudi MO, Triana FJ, Patel BS, Bolli R. Effect of superoxide dismutase and catalase, given separately, on myocardial “stunning”. Am J Physiol. 1990;259:H889–901. doi: 10.1152/ajpheart.1990.259.3.H889. [DOI] [PubMed] [Google Scholar]
- 9.Tang XL, Qiu Y, Turrens JF, Sun JZ, Bolli R. Late preconditioning against stunning is not mediated by increased antioxidant defenses in conscious pigs. Am J Physiol. 1997;273:H1651–1657. doi: 10.1152/ajpheart.1997.273.4.H1651. [DOI] [PubMed] [Google Scholar]
- 10.Auyeung Y, Sievers RE, Weng D, Barbosa V, Wolfe CL. Catalase inhibition with 3-amino-1,2,4-triazole does not abolish infarct size reduction in heat-shocked rats. Circulation. 1995;92:3318–3322. doi: 10.1161/01.cir.92.11.3318. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Y, Griendling KK, Dikalova A, Owens GK, Taylor WR. Vascular hypertrophy in angiotensin ii-induced hypertension is mediated by vascular smooth muscle cell-derived h2o2. Hypertension. 2005;46:732–737. doi: 10.1161/01.HYP.0000182660.74266.6d. [DOI] [PubMed] [Google Scholar]
- 12.Hsieh PC, Segers VF, Davis ME, MacGillivray C, Gannon J, Molkentin JD, Robbins J, Lee RT. Evidence from a genetic fate-mapping study that stem cells refresh adult mammalian cardiomyocytes after injury. Nat Med. 2007;13:970–974. doi: 10.1038/nm1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seshadri G, Sy JC, Brown M, Dikalov S, Yang SC, Murthy N, Davis ME. The delivery of superoxide dismutase encapsulated in polyketal microparticles to rat myocardium and protection from myocardial ischemia-reperfusion injury. Biomaterials. 2010;31:1372–1379. doi: 10.1016/j.biomaterials.2009.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sy JC, Seshadri G, Yang SC, Brown M, Oh T, Dikalov S, Murthy N, Davis ME. Sustained release of a p38 inhibitor from non-inflammatory microspheres inhibits cardiac dysfunction. Nat Mater. 2008;7:863–868. doi: 10.1038/nmat2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koitabashi N, Bedja D, Zaiman AL, Pinto YM, Zhang M, Gabrielson KL, Takimoto E, Kass DA. Avoidance of transient cardiomyopathy in cardiomyocyte-targeted tamoxifen-induced mercremer gene deletion models. Circ Res. 2009;105:12–15. doi: 10.1161/CIRCRESAHA.109.198416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oshinski JN, Yang Z, Jones JR, Mata JF, French BA. Imaging time after gd-dtpa injection is critical in using delayed enhancement to determine infarct size accurately with magnetic resonance imaging. Circulation. 2001;104:2838–2842. doi: 10.1161/hc4801.100351. [DOI] [PubMed] [Google Scholar]
- 17.Sohal DS, Nghiem M, Crackower MA, Witt SA, Kimball TR, Tymitz KM, Penninger JM, Molkentin JD. Temporally regulated and tissue-specific gene manipulations in the adult and embryonic heart using a tamoxifen-inducible cre protein. Circ Res. 2001;89:20–25. doi: 10.1161/hh1301.092687. [DOI] [PubMed] [Google Scholar]
- 18.Lefer DJ, Granger DN. Oxidative stress and cardiac disease. Am J Med. 2000;109:315–323. doi: 10.1016/s0002-9343(00)00467-8. [DOI] [PubMed] [Google Scholar]
- 19.Wu S, Li Q, Du M, Li SY, Ren J. Cardiac-specific overexpression of catalase prolongs lifespan and attenuates ageing-induced cardiomyocyte contractile dysfunction and protein damage. Clin Exp Pharmacol Physiol. 2007;34:81–87. doi: 10.1111/j.1440-1681.2007.04540.x. [DOI] [PubMed] [Google Scholar]
- 20.Dong F, Fang CX, Yang X, Zhang X, Lopez FL, Ren J. Cardiac overexpression of catalase rescues cardiac contractile dysfunction induced by insulin resistance: Role of oxidative stress, protein carbonyl formation and insulin sensitivity. Diabetologia. 2006;49:1421–1433. doi: 10.1007/s00125-006-0230-7. [DOI] [PubMed] [Google Scholar]
- 21.Murdoch CE, Zhang M, Cave AC, Shah AM. Nadph oxidase-dependent redox signalling in cardiac hypertrophy, remodelling and failure. Cardiovasc Res. 2006;71:208–215. doi: 10.1016/j.cardiores.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 22.Turdi S, Li Q, Lopez FL, Ren J. Catalase alleviates cardiomyocyte dysfunction in diabetes: Role of akt, forkhead transcriptional factor and silent information regulator 2. Life Sci. 2007;81:895–905. doi: 10.1016/j.lfs.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 23.Wolkart G, Kaber G, Kojda G, Brunner F. Role of endogenous hydrogen peroxide in cardiovascular ischaemia/reperfusion function: Studies in mouse hearts with catalase-overexpression in the vascular endothelium. Pharmacol Res. 2006;54:50–56. doi: 10.1016/j.phrs.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Schriner SE, Ogburn CE, Smith AC, Newcomb TG, Ladiges WC, Dolle ME, Vijg J, Fukuchi K, Martin GM. Levels of DNA damage are unaltered in mice overexpressing human catalase in nuclei. Free Radic Biol Med. 2000;29:664–673. doi: 10.1016/s0891-5849(00)00352-x. [DOI] [PubMed] [Google Scholar]
- 25.Herskowitz A, Choi S, Ansari AA, Wesselingh S. Cytokine mrna expression in postischemic/reperfused myocardium. Am J Pathol. 1995;146:419–428. [PMC free article] [PubMed] [Google Scholar]
- 26.Kraemer R, Seligmann B, Mullane KM. Polymorphonuclear leukocytes reduce cardiac function in vitro by release of h2o2. Am J Physiol. 1990;258:H1847–1855. doi: 10.1152/ajpheart.1990.258.6.H1847. [DOI] [PubMed] [Google Scholar]
- 27.Matsui Y, Sadoshima J. Rapid upregulation of ctgf in cardiac myocytes by hypertrophic stimuli: Implication for cardiac fibrosis and hypertrophy. J Mol Cell Cardiol. 2004;37:477–481. doi: 10.1016/j.yjmcc.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Park SK, Kim J, Seomun Y, Choi J, Kim DH, Han IO, Lee EH, Chung SK, Joo CK. Hydrogen peroxide is a novel inducer of connective tissue growth factor. Biochem Biophys Res Commun. 2001;284:966–971. doi: 10.1006/bbrc.2001.5058. [DOI] [PubMed] [Google Scholar]
- 29.Suematsu N, Tsutsui H, Wen J, Kang D, Ikeuchi M, Ide T, Hayashidani S, Shiomi T, Kubota T, Hamasaki N, Takeshita A. Oxidative stress mediates tumor necrosis factor-alpha-induced mitochondrial DNA damage and dysfunction in cardiac myocytes. Circulation. 2003;107:1418–1423. doi: 10.1161/01.cir.0000055318.09997.1f. [DOI] [PubMed] [Google Scholar]
- 30.Sun Y. Myocardial repair/remodelling following infarction: Roles of local factors. Cardiovasc Res. 2009;81:482–490. doi: 10.1093/cvr/cvn333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ohnishi H, Oka T, Kusachi S, Nakanishi T, Takeda K, Nakahama M, Doi M, Murakami T, Ninomiya Y, Takigawa M, Tsuji T. Increased expression of connective tissue growth factor in the infarct zone of experimentally induced myocardial infarction in rats. J Mol Cell Cardiol. 1998;30:2411–2422. doi: 10.1006/jmcc.1998.0799. [DOI] [PubMed] [Google Scholar]
- 32.Ono K, Matsumori A, Shioi T, Furukawa Y, Sasayama S. Cytokine gene expression after myocardial infarction in rat hearts: Possible implication in left ventricular remodeling. Circulation. 1998;98:149–156. doi: 10.1161/01.cir.98.2.149. [DOI] [PubMed] [Google Scholar]
- 33.Dean RG, Balding LC, Candido R, Burns WC, Cao Z, Twigg SM, Burrell LM. Connective tissue growth factor and cardiac fibrosis after myocardial infarction. J Histochem Cytochem. 2005;53:1245–1256. doi: 10.1369/jhc.4A6560.2005. [DOI] [PubMed] [Google Scholar]
- 34.Jensen LT, Host NB. Collagen: Scaffold for repair or execution. Cardiovasc Res. 1997;33:535–539. doi: 10.1016/s0008-6363(96)00247-7. [DOI] [PubMed] [Google Scholar]
- 35.Jugdutt BI, Joljart MJ, Khan MI. Rate of collagen deposition during healing and ventricular remodeling after myocardial infarction in rat and dog models. Circulation. 1996;94:94–101. doi: 10.1161/01.cir.94.1.94. [DOI] [PubMed] [Google Scholar]
- 36.Elgawish A, Glomb M, Friedlander M, Monnier VM. Involvement of hydrogen peroxide in collagen cross-linking by high glucose in vitro and in vivo. J Biol Chem. 1996;271:12964–12971. doi: 10.1074/jbc.271.22.12964. [DOI] [PubMed] [Google Scholar]
- 37.Jugdutt BI. Ventricular remodeling after infarction and the extracellular collagen matrix: When is enough enough? Circulation. 2003;108:1395–1403. doi: 10.1161/01.CIR.0000085658.98621.49. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.