Abstract
Context
Patients who have received solid organ transplants continue to experience a myriad of complex symptoms related to their underlying disease and to chronic immunosuppression that reduce the quality of life. Beneficial non-pharmacologic therapies to address these symptoms have not been established in the transplant population.
Objective
Assess the efficacy of Mindfulness-Based Stress Reduction (MBSR) in reducing symptoms of anxiety, depression, and poor sleep in transplant patients.
Design, Setting and Patients
Controlled trial with a 2-staged randomization. Recipients of kidney, kidney/pancreas, liver, heart or lung transplants were randomized to MBSR (n=72) or Health Education (n=66) initially or after serving on a waitlist. Mean age was 54 (range 21–75 years); 55% were men and 91% were white.
Interventions
MBSR, a mindfulness meditation training program consisting of 8 weekly 2.5 hour classes; Health Education, a peer-led active control.
Primary Outcome Measures
Anxiety (STAI), depression (CES-D), and sleep quality (PSQI) scales assessed by self-report at baseline, 8 weeks, 6 months and 1 year.
Results
Benefits of MBSR were above and beyond those afforded by the active control. MBSR reduced anxiety and sleep symptoms (Ps<0.02), with medium treatment effects (0.51 and 0.56) at 1 year compared to Health Education in intention-to-treat analyses. Within the MBSR group anxiety, depression and sleep symptoms decreased and quality of life measures improved by 8 weeks (Ps <0.01, all), and benefits were retained at 1 year (Ps<0.05, all). Initial symptom reductions in the Health Education group were smaller and not sustained. Comparisons to the waitlist confirmed the impact of MBSR on both symptoms and quality of life, whereas Health Education improvements were limited to quality of life ratings.
Conclusions
MBSR reduced distressing symptoms of anxiety, depression and poor sleep and improved quality of life. Benefits were sustained over 1 year. A health education program provided fewer benefits, and effects were not as durable. MBSR is a relatively inexpensive, safe and effective community-based intervention.
INTRODUCTION
About 28,000 solid organ transplants are performed in the United States annually, and most recipients return to the community to be cared for by physicians in primary care and sub-specialty practices.1 Transplant recipients experience health problems even when they have excellent function of their transplanted organs, as immunosuppressive medications can generate adverse effects and spawn new complications, such as hypertension, hypercholesterolemia and osteoporosis. 2–3 Given the stressors inherent in managing complex chronic health problems, it is not surprising that troublesome anxiety, depression and insomnia symptoms are prevalent in the transplant population.4–6 A recent study of transplant recipients found that 41% had poor psychosocial outcomes, characterized by psychological stress, depression and anxiety, and reduced health-related quality of life up to 2 years after transplantation.7 Interventions to reduce symptoms and improve quality of life after transplantation are needed, and drug-free strategies may be preferred due to the complexity of transplant medication regimens.8–10 In a pilot study, transplant recipients who attended a Mindfulness-Based Stress Reduction (MBSR) program reported fewer symptoms of anxiety, depression and poor sleep over 6 month follow-up.11–12 MBSR had not been tested in a controlled trial with transplant recipients.
Mindfulness-based Stress Reduction
Mindfulness-based Stress Reduction (MBSR) is an 8-week program designed to facilitate adaptation to the stressors of chronic illness.13–14 Mindfulness meditation, the foundation of MBSR, is a method for self-regulation of attention, described as paying attention on purpose, moment-by-moment, and without forming judgments.14 Mindfulness training increases awareness of inner thoughts, emotions and bodily sensations, and fosters an attitude of acceptance. Practice of mindfulness is expected to reduce symptom distress and improve well-being.15
The standard MBSR program is led by a teacher in a classroom format. MBSR has a curriculum with assignments and techniques for participants, plus training programs, certification and continuing education for teachers to provide a consistent program that can be delivered in a community setting.13 MBSR classes primarily concentrate on training participants to focus attention through a variety of meditative techniques, such as following the breath and yoga. Participants learn to perceive their immediate emotional and physical state, including pain or discomfort, and to let thoughts come and go in awareness with no attempt to change, suppress or elaborate on them. Participants learn to respond mindfully to day-to-day stressors with appropriate action, as opposed to reacting “on automatic pilot” with conditioned responses that can be emotionally arousing or unhelpful. The goal is lifelong self-management.
Mindfulness Meditation and Health
Mindfulness meditation training has been shown to improve health outcomes for patients with medical conditions such as cancer16 or psoriasis17, and psychological disturbances such as depression18 or anxiety.19–20 The most reproducible impact of the MBSR program is on stress-related disorders, depression and anxiety symptoms.21–22 Mindfulness training is hypothesized to impact health outcomes through cognitive and behavioral mechanisms such as changing one’s perspective on thoughts and events (i.e., thoughts are mental events and not facts), and by reducing physiologic arousal.21, 23
To address the symptom burden experienced by transplant recipients, we conducted a randomized, actively controlled clinical trial to test the effectiveness of a MBSR program to reduce symptoms and improve quality of life. The MBSR program was compared to two control groups: an active Health Education program and a usual care waitlist that was later re-randomized to MBSR or Health Education. The inclusion of an active control, Health Education, allowed us to test the specificity of MBSR by controlling for non-specific elements of MBSR such as instructor attention and group support, and also for participant characteristics such as motivation, expectations and time. The waitlist group enabled us to confirm that treatment effects (from either MBSR or Health Education program) exceeded usual care. The primary hypothesis was that the MBSR group would report better outcomes than the Health Education group on self-report measures of anxiety, depression, and sleep quality. Secondary hypotheses were that the MBSR group would report better mental health, physical health, and quality of life outcomes. The assumption that MBSR and Health Education were both active interventions was tested by comparing each intervention to the waitlist.
METHODS
Setting and Participants
Transplant recipients living in a Midwestern metropolitan area were recruited through clinician referral, direct mailings from patient advocacy groups, and brochures placed in outpatient clinics and pharmacies. Inclusion criteria were a functioning solid-organ transplant (i.e., kidney, kidney/pancreas, pancreas, lung, liver, heart or heart-lung), age 18 or older, ability to read and write English, and willingness to attend classes. To avoid the confounding effects of surgical recovery, patients were at least 6 months post-transplant. Exclusions were being medically unstable or on dialysis, having serious preexisting mental health issues, or having previously taken MBSR.
This trial was approved by the Institutional Review Boards of the University of Minnesota and Hennepin County Medical Center. All participants signed consent and HIPAA forms.
Randomization and Interventions
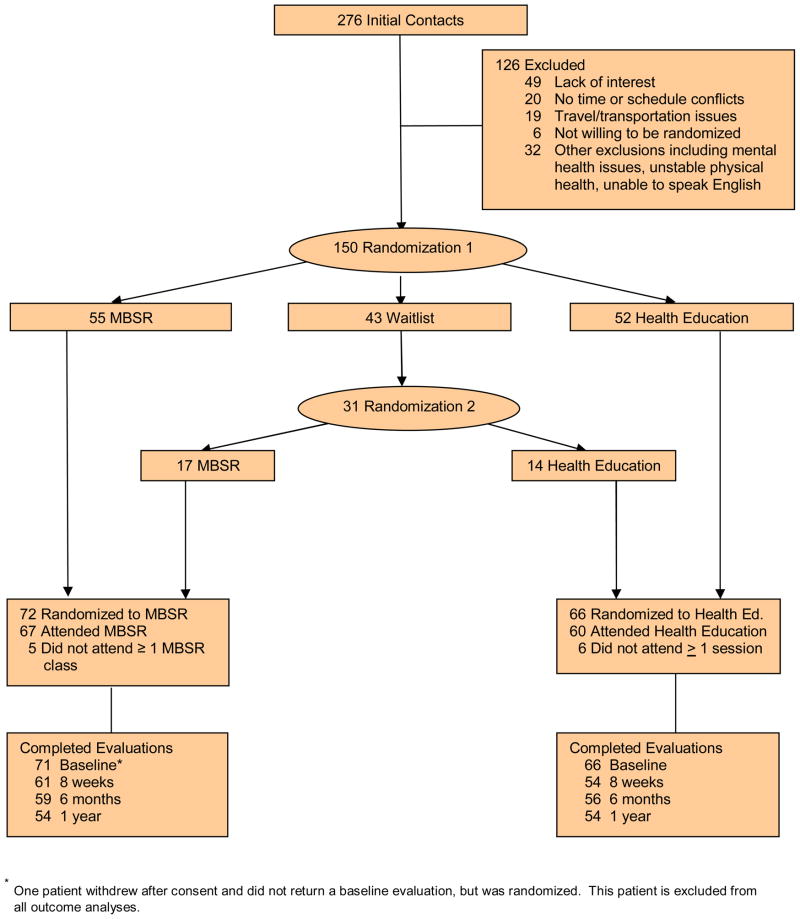
Patients were stratified by type of transplant (kidney or kidney-pancreas; liver; and heart or lung), type 1 diabetes, and use of medications for anxiety, depression or sleep disturbances in the past year, and randomized equally within strata to three groups: MBSR, Health Education, or waitlist (Randomization 1 in Figure 1). To maximize the number of transplant recipients for comparisons between active interventions, a two-stage randomization scheme was used. Patients initially randomized to the waitlist were randomized again after 6 months to either MBSR or Health Education (Randomization 2 in Figure 1). Randomization lists were computer-generated and maintained by the study statistician. To avoid confusion between the study-designed waitlist and the United Network for Organ Sharing waiting list for transplant candidates, the waitlist arm was referred to as the “delayed intervention group” in all study materials. Patients and staff working with patients were unaware of treatment assignments until after enrollment. The study design and procedures are detailed elsewhere in the literature.24
Figure 1.
Study participation and follow-up.
MBSR and Health Education classes were conducted in parallel. Both interventions were comprised of 8 weekly 2.5 hour classes. The MBSR program included a daylong retreat held on a weekend day between weeks 6 and 7. There was no retreat in Health Education. Study staff called participants to encourage meditation practice (MBSR) or make inquiries about health (Health Education) between study months 2 and 6. Calls were made weekly for 1 month, biweekly for 1 month, and then monthly. MBSR and Health Education groups were invited to a “booster” session in study month 4. The MBSR booster was a regular class. The Health Education booster was a social event with refreshments.
MBSR was conducted according to the class-by-class outline of activities, handouts and assignments from the 2002 MBSR curriculum guide.25 MBSR students learn four formal techniques to foster mindful awareness: (1) body scan; (2) sitting meditation; (3) gentle Hatha yoga; and (4) walking meditation. 14, 26 As a preface and foundation for these techniques, students are introduced to diaphragmatic or “belly” breathing. Done mindfully, this technique is called “breath awareness.” In the Body Scan, students are guided to notice the sensations in each part of the body, from the toes of one foot to the top of the head. Sitting meditation begins with breath awareness. The student is instructed to notice interrupting thoughts, feelings or sensations, and to let them go and return the focus to the breath. Mindful Hatha yoga is a form of meditation in movement. By doing gentle yoga mindfully, the student relaxes, improves strength and flexibility, and comes to accept the body and mind together. Walking meditation is the practice of walking experientially. This means walking slowly, noticing the sensations as the foot makes contact with, rises and lifts from the ground, the shifting of weight, and the cycle of the other foot.
For these practices, the emphasis is on staying in the present moment, with a non-judging, non-striving attitude of acceptance. Initially, students use recorded audio instructions as a guide, later learning to maintain practice without recordings. Practicing formal techniques progresses to incorporation of mindfulness into daily activities (informal practice) like mindful eating and breath awareness during times of stress.
Course materials included recordings of guided meditations and the text, Full Catastrophe Living by Kabat-Zinn.14 Seven sets of MBSR classes (median class size = 8 participants) were led by one of two teachers who trained at the Center for Mindfulness in Medicine, Health Care and Society.13 To promote consistency of MBSR delivery, the second teacher observed the first teacher lead two courses prior to independently conducting a course, and class handouts and assignments were prepared and distributed weekly by study staff.
The core of the Health Education intervention was the chronic disease self-management program developed by Lorig et al.27 Participants met in groups with trained peer leaders to problem solve, set personal goals and devise a weekly action plan such as getting a hearing test. Peer facilitators followed scripted presentations from a detailed course manual.28 The standard program was followed by two sessions focused on transplant-specific issues to match the duration of the MBSR course. Three kidney recipients were peer leaders; all were trained and supervised by the study psychologist, a certified trainer. The psychologist attended all Health Education sessions and documented that classes were conducted according to protocol. Seven Health Education programs were conducted (median size = 7 participants).
Outcomes and Follow-Up
The primary outcomes were self-report scales for assessing symptoms of anxiety and depression and the quality of sleep. Anxiety was measured by the State-Trait Anxiety Inventory - State Version (STAI) 29; depression was measured by the Center for Epidemiological Studies -Depression Scale (CES-D) 30; and sleep was measured by the Pittsburgh Sleep Quality Index (PSQI).31 The STAI was designed to measure anxiety at the present time, and consists of 20 brief questions such as “I am tense”, rated from 1 = not at all to 4 = very much so. 29 Scores range from 20 to 80, and cut-points have been proposed for mild (<40), moderate (40–59), and severe (≥ 60) anxiety symptoms. The STAI has been extensively validated and found to have strong psychometric properties.32 CES-D consists of 20 questions such as “I was bothered by things that don’t usually bother me,” with responses graded from 1 = rarely or none at all to 4 = most or all of the time. 30 Scores range from 0 to 60, and a score of 16 or higher has been proposed to identify clinically meaningful depression symptoms. 32 The PSQI is the most widely used, standardized measure of sleep quality.31 The PSQI has 18 self-report questions that are combined to provide an overall score based on 7 domains of sleep: quality, latency, duration, efficiency (hours asleep divided by hours in bed), disturbances (like awakening to use the toilet), use of sleep medications, and daytime dysfunction. PSQI scores range from 0 to 21, and a score greater than 8 has been proposed to identify poor sleepers among those with chronic illness, based on a validation study that included kidney transplant recipients. 33 Accepted benchmarks for clinically meaningful symptoms, or poor sleep among those with chronic illness, are STAI scores ≥ 40, CES-D scores ≥ 16, and PSQI scores > 8. 29, 32–33 Cronbach’s α reliability coefficients for the STAI, CES-D and PSQI were .95, .91 and .77, respectively, for the patients in this study at baseline.
Secondary outcomes were measures of quality of life and perceived health. Measures included the mental and physical health summary scores of the SF-12 version 2 34, the SF-36 version 2 bodily pain and vitality subscales 35, and visual analogue scales (VAS) for health and quality of life. The SF-12 is a brief version of the widely used SF-36 generic health profile.11, 34–35 The SF-12 mental and physical health summary scores are unbiased, close approximations to their SF-36 counterparts. The SF-36 vitality subscale consists of four questions (feel full of life; have a lot of energy; feel worn out; feel tired) each rated on a 5-point scale from all of the time to none of the time. The SF-36 pain subscale combines responses to two questions; one a rating of the intensity of bodily pain and the other the extent to which pain interferes with normal work (including housework). The SF-12 and SF-36 scores are reported as T-scores (mean =50, SD =10) with higher scores representing better states of health. Minimally important differences on the summary scores and the pain and vitality subscales are 2–3 points.
A global rating of health was based on one question, “How good or bad your health state is today” with responses marked on a line from 0 = death to 100 = complete health. 36 Quality of life was measured with one item, “Considering your life as a whole, please rate your quality of life today”, with responses recorded on a line marked 0 = worst possible to 100 = best possible quality of life. Test-retest reliability coefficients for these single item VAS scales are typically about 0.70. 32
Three potential mediators of the impact of MBSR were measured: class attendance, home meditation practice, and mindful awareness, measured by the Mindful Attention Awareness Scale (MAAS).37 The MAAS measures awareness of the presence or absence of attention to the present moment, based on 15 items such as “I snack without being aware that I’m eating” that are rated from 1 = almost always to 6 = almost never. 37 Higher MAAS scores indicate greater levels of dispositional mindfulness. The reliability of the MAAS was high for the transplant patients in this study at baseline (Cronbach’s α=.91). Attendance was collected on-site, home practice minutes were recorded in diaries, and the MAAS was collected in the outcome questionnaires. Overall scores were computed for standardized scales when some item-level missing data were present, according to the rules for coding provided by the developers of the scales.
Demographics and transplant history were collected during a screening interview. At the end of the interview, a baseline questionnaire was given to patients to complete at home and return by mail. Outcome questionnaires and practice diaries were distributed and returned by mail at 8-weeks, 6-months and one-year. Questionnaires completed 6 months after the first randomization provided pre-intervention baseline data for waitlist patients entering MBSR or Health Education after Randomization 2. The numbers of patients who completed each outcome assessment are shown in Figure 1. MBSR and Health Education groups had similar rates of missing outcome questionnaires. Lack of time or interest were typical reasons given for not returning study questionnaires.
Statistical Analysis
A sample of 150 patients was estimated to have 80% power to detect a medium treatment effect between MBSR and the Health Education groups with an unpaired t-test, at α=0.05, 2-tailed, allowing for 20% attrition. Over 80% power was assumed for the primary analysis, a linear mixed model regression for repeated measures, because outcome information derives from multiple observations over one year and adjustments for stratification variables and influential covariates (e.g., baseline scores) reduces the amount of unexplained variation. A medium effect size (ES) 38 was anticipated based on an active-controlled trial of mindfulness-enhanced therapy compared to standard therapy alone for depression relapse prevention.18 A medium effect corresponds to a difference of 1.2, 3.0, and 3.6 points on the PSQI, CES-D, and STAI, respectively, based on the variance of changes at week 8.
Demographics and baseline values were compared between groups using t-tests, chi-square or Wilcoxon tests. Longitudinal analyses tested primary and secondary hypotheses. Linear mixed models for repeated measures compared the impact of MBSR to Health Education across all measured follow-ups. Models included adjustments for the baseline value of the outcome, course cycle, randomization strata, prior waitlist service, and the interaction between time and treatment impact. In these models, random effects for patient account for correlations among repeated measurements on a single patient. Adjustment for the course cycle accounts for possible cohort effects among groups of persons attending a course together. Treatment effects for MBSR relative to Health Education were estimated by differences between covariate-adjusted means divided by the square root of the common error variance. These longitudinal analyses allow unequal numbers of observations per subject and assume missing data to be dependent on observed data, but otherwise missing at random.
A separate analysis of 8-week outcomes following Randomization 1 tested the assumption that treatment outcomes exceeded usual care. Each intervention group was compared to the usual care waitlist using a priori contrasts tested at α=0.05, 2-tailed, with generalized linear models adjusted for baseline values and randomization strata. Treatment versus waitlist effect sizes were estimated by mean differences divided by the root mean square error of the model. 39 Confidence intervals for effect sizes were estimated using the bootstrap percentile method from 1,000 replications.
All analyses were conducted according to the intention-to-treat principle, based on all measured outcomes, without imputation of missing values. Where outcome values were skewed, log transformations were used to approximate a normal distribution. Relationships among outcomes and putative mediators of MBSR were investigated using correlations. The responses to treatment of former waitlist patients were examined and no evidence of bias favoring MBSR or Health Education was detected (results not shown). P values less than 0.05, 2-sided were considered statistically significant. SAS (Version 9.2, SAS Institute, Cary, NC) and SPSS v14.0 (SPSS, Inc., Chicago, IL) were used.
RESULTS
One hundred fifty transplant recipients were enrolled between July 2003 and March 2007, and randomly assigned to MBSR, Health Education or the waitlist. Follow-up ended in May 2008. There were fewer patients in the waitlist than in the active groups because participants randomized prior to the final set of classes were not allocated to the waitlist. Patients were mainly older adults with kidney transplants. Baseline scores on the outcome scales did not differ by group. Accepted benchmarks for clinically meaningful symptoms were exceeded at baseline by 39%, 38% and 42% of patients on the anxiety, depression, and sleep scales, respectively. After Randomization 1, patient characteristics were generally well-balanced, although the Health Education arm included more patients with only a high school education and fewer married ones.24 After 6 months, 31 waitlist patients were re-randomized to MBSR or Health Education, and as shown in Table 1, no notable imbalances in patient demographics remained between the intervention groups. Of those randomized to MBSR or Health Education, 74% attended 5 or more classes, a benchmark for course completion. Eleven patients (5 MBSR and 6 Health Education) did not attend a single class. One patient assigned to MBSR withdrew prior to the start of classes and withheld baseline data submission, and was therefore omitted from all outcome analyses. With this modification, our intention-to-treat sample contained 137 patients in MBSR (n=71) or Health Education (n=66) with randomizations 1 and 2 combined. (See Figure 1) Outcome analyses included all randomized patients who completed one or more follow-up evaluations (n=122). No adverse events related to the interventions occurred at any point during this trial.
Table 1.
Patient Characteristics at Enrollment, Randomizations 1 and 2 combined
| Characteristic | MBSR (n=71)1 | Health Education (n=66) | P Value2 |
|---|---|---|---|
| Age, mean (SD) | 55 (11.3) | 52 (10.4) | .13 |
| Gender Male, No. (%) | 38 (54%) | 37 (56%) | .77 |
| Race (self-reported), No. (%) | |||
| White | 65 (91%) | 62 (94%) | .59 |
| Black/African American, Asian or American Indian/Alaska Native | 9 (8%) | 9 (6%) | |
| Married, No. (%) | 46 (65%) | 36 (55%) | .22 |
| Employment, No. (%) | |||
| Full- or Part-time | 35 (49%) | 39 (59%) | .25 |
| Education, No. (%) | |||
| High school or less | 3 (4%) | 10 (15%) | .18 |
| Some college | 24 (34%) | 21 (32%) | |
| College graduate | 29 (41%) | 24 (36%) | |
| Post-graduate | 15 (21%) | 11 (17%) | |
| Transplant type, No. (%) | |||
| Kidney or Kidney/Pancreas | 49 (69%) | 41 (62%) | .45 |
| Liver | 11 (16%) | 12 (18%) | |
| Heart | 6 (8%) | 5 (8%) | |
| Lung(s) | 5 (7%) | 5 (8%) | |
| Pancreas | 0 | 3 (4%) | |
| Years since first transplant, mean (SD) | 5.8 (6.0) | 7.1 (6.9) | .27 |
| Type 1 Diabetes, Number (%) | 9 (13%) | 8 (12%) | .92 |
| Treated in past year or current medication for sleep, depression and/or anxiety, Number (%) | 32 (45%) | 29 (44%) | .89 |
One patient was excluded. This patient did not return a baseline evaluation and withdrew from the study without attending any classes. (See Figure 1).
P values from t-tests, Wilcoxon tests (skewed continuous variables) or chi-square tests (discrete variables).
Comparisons between MBSR and Health Education
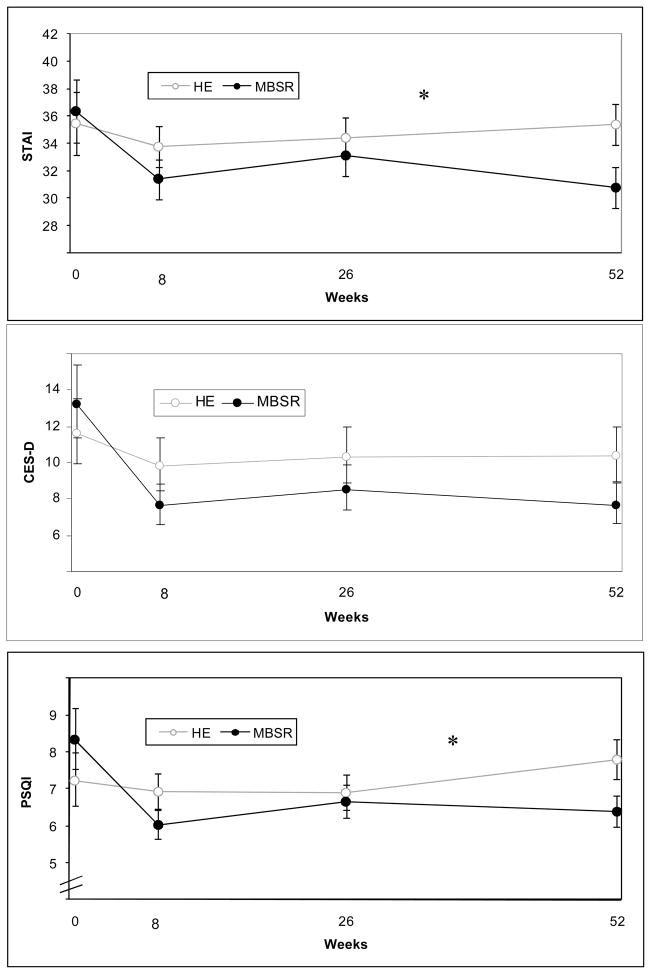
Patients randomized to MBSR or Health Education initially or after serving on the waitlist were compared to test the primary hypotheses. As hypothesized, the MBSR group reported fewer symptoms throughout follow-up than patients allocated to Health Education, a time and attention control. The MBSR group reported less anxiety (F(1,108) = 5.21, P=0.02) and fewer sleep problems (F(1, 106)= 5.28, P=0.02) than the HE group over time. (Figures 2a and 2c) Within the MBSR group, anxiety and sleep symptoms were reduced by 8 weeks, and remained significantly below baseline levels at 1 year (Table 2). Symptom reductions following Health Education were smaller and not maintained. At 1 year, MBSR was more effective than Health Education in decreasing anxiety and sleep problems, with effect sizes in the medium range (ES=0.56 and 0.51, respectively). The trajectories of depression symptoms are shown in Figure 3b. At 1 year, depression symptoms remained significantly reduced from baseline levels only in the MBSR group; however, the MBSR versus Health Education difference did not reach statistical significance (ES = 0.41, P=0.08).
Figure 2.
Trajectory of symptoms over time.
Figure 2a. Anxiety symptoms over time in MBSR and Health Education groups.
Figure 2b. Depression symptoms over time in MBSR and Health Education groups.
Figure 2c. Sleep symptoms over time in MBSR and Health Education groups Means (± SE) over time for STAI (anxiety), CESD (depression) and PSQI (sleep) scales are plotted for the MBSR and Health Education (HE) groups in the intention-to-treat sample after Randomization 2, without imputation of missing values (MBSR, n=63; HE, N=59). Asterisks indicate significant between group differences: the MBSR group reported fewer symptoms of poor sleep and anxiety over time (Ps=0.02, both) than the Health Education group. The difference between groups in depression trajectories was not significant (P=0.10). Values were calculated using linear mixed models with adjustments for baseline value, course cycle, randomization strata, prior waitlist service, interaction between time and treatment impact, and intra-correlations among repeated measurements within subjects and among subjects within a course cycle.
Table 2.
Symptom and quality of life values over time in the MBSR (n=63) and Health Education (n=59) Groups1
| Outcomes | Baseline, mean (95% CI) | Within-Group Comparisons2 |
Between-Group Comparisons3 |
|||
|---|---|---|---|---|---|---|
| 8 Week, mean (95% CI) | 6 Month, mean (95% CI) | 1 Year, mean (95% CI) | Treatment Effect at 1 year | Overall P value | ||
| Primary Outcome Measures 4 | ||||||
| State-Trait Anxiety Inventory | ||||||
| MBSR | 36.4 (31.8, 40.9) | 31.4 (28.5, 34.2)*** | 33.1 (30.2, 36.0) | 30.8 (27.8, 33.7)** | 0.56** | 0.02 |
| Health Education | 35.5 (30.9, 40.1) | 33.8 (30.8, 36.7) | 34.4 (31.4, 37.3) | 35.4 (32.4, 38.4) | ||
| Center for Epidemiologic Studies Depression Scale | ||||||
| MBSR | 13.2 (9.8, 17.8) | 7.6 (5.7, 10.1)** | 8.5 (6.4, 11.3) | 7.7 (5.8, 10.2)** | 0.41 | 0.10 |
| Health Education | 11.6 (8.6, 15.7) | 9.8 (7.4, 13.1)* | 10.3 (7.7, 13.8) | 10.3 (7.7, 13.8) | ||
| Pittsburgh Sleep Quality Index | ||||||
| MBSR | 8.3 (6.9, 10.1) | 6.0 (5.3, 6.9)*** | 6.7 (5.8, 7.6)** | 6.4 (5.6, 7.3)* | 0.51** | 0.02 |
| Health Education | 7.2 (6.0, 8.8) | 6.9 (6.1, 7.9)* | 6.9 (6.0, 7.9)** | 7.8 (6.8, 8.9) | ||
| Secondary Outcome Measures5 | ||||||
| Mental Health Summary, SF-12 | ||||||
| MBSR | 45.7 (41.6, 49.9) | 54.3 (51.5, 57.1)*** | 52.0 (49.2, 54.8)*** | 52.9 (50.1, 55.7)*** | 0.19 | 0.29 |
| Health Education | 46.6 (42.4, 50.7) | 52.9 (50.0, 55.8)*** | 51.2 (48.3, 54.1)** | 51.5 (48.6, 54.4)** | ||
| Physical Health Summary, SF-12 | ||||||
| MBSR | 39.6 (35.4, 43.7) | 42.1 (39.2, 45.0) | 41.5 (38.5, 44.4) | 44.3 (41.4, 47.3) | 0.20 | 0.61 |
| Health Education | 40.3 (36.1, 44.5) | 43.2 (40.2, 46.2) | 43.8 (40.8, 46.8) | 42.7 (39.7, 45.7) | ||
| Vitality, SF-36 | ||||||
| MBSR | 44.4 (40.5, 48.3) | 50.3 (47.5, 53.1)*** | 48.0 (45.1, 50.9) | 51.8 (49.0, 54.7)*** | 0.59** | 0.29 |
| Health Education | 44.4 (40.5, 48.4) | 50.0 (47.0, 52.9)** | 49.0 (46.1, 51.9)** | 47.1 (44.1, 50.0)* | ||
| Bodily Pain, SF-36 | ||||||
| MBSR | 43.2 (39.6, 46.7) | 47.6 (44.2, 50.9) | 46.2 (42.9, 49.6) | 47.3 (43.9, 50.6) | 0.00 | 0.92 |
| Health Education | 45.5 (42.0, 49.1) | 47.7 (44.3, 51.1) | 46.6 (43.2, 50.0) | 47.3 (43.9, 50.7) | ||
| Health VAS | ||||||
| MBSR | 65.9 (59.5, 72.2) | 75.6 (70.4, 80.8) | 74.2 (68.9, 79.4) | 77.2 (72.0, 82.5)** | 0.40 | 0.73 |
| Health Education | 69.2 (62.8, 75.6) | 75.3 (69.9, 80.6)* | 74.6 (69.3, 80.0)* | 71.7 (66.3, 77.1) | ||
| Quality of Life VAS | ||||||
| MBSR | 69.6 (63.8, 75.3) | 79.1 (75.0, 83.1)* | 76.3 (72.3, 80.3) | 79.3 (75.3, 83.4)*** | 0.25 | 0.49 |
| Health Education | 72.2 (66.4, 78.0) | 78.9 (74.8, 83.0)** | 77.7 (73.7, 81.8)* | 76.4 (72.3, 80.5)* | ||
The sample consisted of all patients with one or more follow-up evaluations who were randomized to MBSR or Health Education initially or after serving on the waitlist (n=122).
Mean (95% CI) values are based on linear mixed model regression for repeated measures adjusted for baseline value, type of transplant, diabetes, and use of medications for anxiety, depression or sleep disturbances in the past year, prior waitlist service, time by treatment interactions and the intra-correlations within subject and among the cohort of subjects in a course cycle. Differences between baseline and each follow-up time within-group were tested using contrasts in the model. Significance is indicated by asterisks as follows:
P<.05,
P<.01, and
P<.001
Positive treatment effects indicate better outcomes in the MBSR group than in the Health Education group and the overall P value is from the test of the overall treatment effect between MBSR and Health Education in the linear mixed model regression across all follow-ups.
Higher score indicates more symptoms.
Higher score indicates better function or greater well-being.
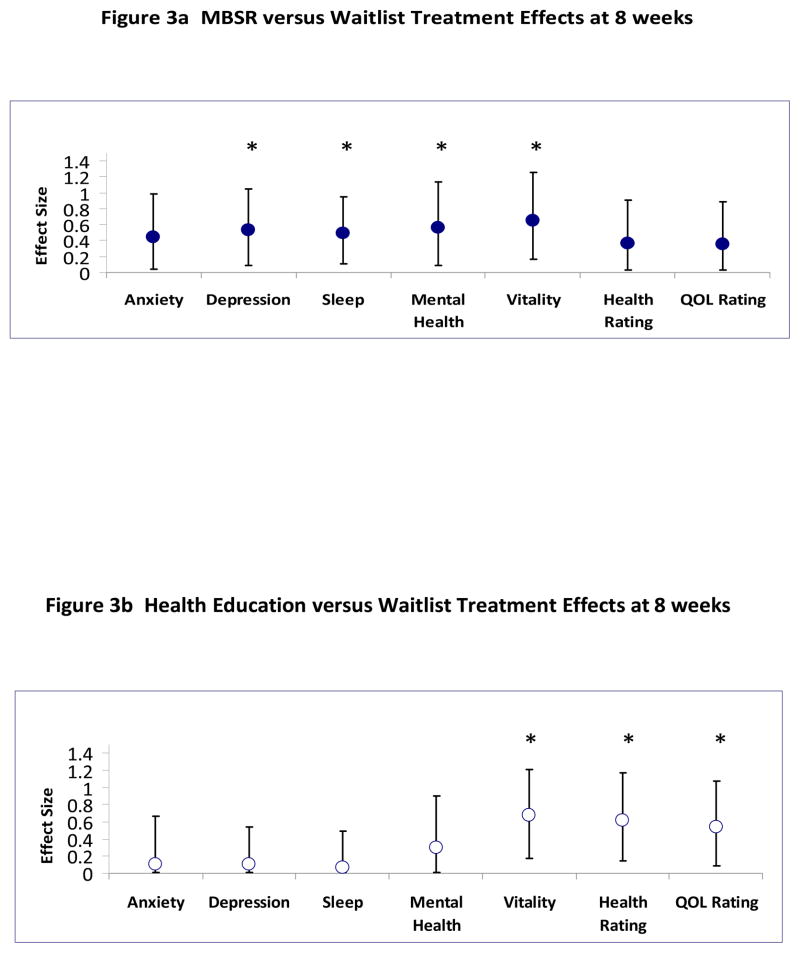
Figure 3.
Treatment effects versus the Waitlist
Figure 3a. Treatment effects for MBSR group versus the Waitlist.
Figure 3b. Treatment effects for Health Education versus the Waitlist.
Effect sizes at 8 weeks from generalized linear models with adjustments for baseline values and randomization strata in the intention-to-treat sample after Randomization 1, without imputation of missing values (MBSR, n = 47; Waitlist, n = 29; and Health Education, n=41). Effects significantly different from 0 are indicated by an asterisk. The Physical Health Summary and SF-36 Pain subscale had small non-significant treatment effects (<0.20), and are not shown.
MBSR and Health Education groups reported 8-week improvements on several secondary outcomes, but benefits were more durable within the MBSR group (Table 2). Improvements in vitality scores were similar initially, but at 1 year the groups diverged, and the MBSR group reported higher levels of vitality (ES =0.59, P<0.01). Physical health and pain reports were unchanged.
Comparisons to the Waitlist: Confirming Treatments are Active
MBSR significantly reduced symptoms relative to the waitlist. As shown in Figure 3a, those allocated to MBSR reported fewer depression symptoms, better sleep quality, and increased mental health and vitality relative to the waitlist at the 8-week follow-up. These treatment effects (ES = 0.49 to 0.65) were in the medium range by Cohen’s criteria.38 MBSR’s treatment effect on anxiety symptoms approached significance (ES = 0.44, P=0.06). As shown in Figure 3b, a different profile of benefits emerged following Health Education. Health Education did not impact symptoms relative to the waitlist. Health Education was indeed active, however, as vitality and health and quality of life ratings significantly increased compared to the waitlist (ES = 0.55 to 0.68). Bodily pain and physical health were unchanged within both the Health Education and MBSR groups. Within the waitlist group changes were small and not significant for all outcomes.
Possible Mechanisms of Mindfulness: Home Practice and Mindfulness
For participants who completed MBSR (attended 5 or more classes, n=53), home meditation practice time averaged 29 minutes per day (range 4 to 61 minutes) between the first MBSR class and the end of the 8th study week. This represents 75% of the recommended practice time. More practice was correlated with reduced anxiety symptoms, increased vitality, and also increased mindfulness over these 8 weeks (correlation coefficients = .3 to.4, P’s<0.01). Correlations between home practice and changes in sleep, depression, and mental health were in the expected directions (more practice, better outcomes), but smaller and not significant (correlation coefficients = .2 to .3, Ps=0.06 to 0.10). Increased mindfulness, measured by the MAAS, was strongly correlated with improvements in sleep, anxiety, depression, mental health, vitality and quality of life (correlation coefficients = .4 to .7, Ps<0.01, all) among those who completed MBSR.
DISCUSSION
This randomized, controlled trial demonstrates that MBSR reduces distressing symptoms and improves mental health and vitality in solid organ transplant recipients. Compared to the waitlist, patients randomized to MBSR reported fewer depression symptoms, better sleep quality, and increased vitality and mental health post-intervention. Compared to active controls, patients randomized to MBSR reported less anxiety, better sleep quality, and more vitality at 1 year follow-up. Medium treatment effects, based on intention-to-treat analyses, were comparable to published meta-analyses of the health impacts of mindfulness training in other clinical populations, based mainly on waitlist-controlled trials.22, 40 Durability of MBSR impact was notable. Anxiety, depression, sleep quality, mental health, vitality, health and quality of life outcomes remained significantly improved from baseline levels at 1 year within the MBSR arm. In the active control arm the scope of benefit was narrower, and impacts were less durable. Because benefits were obtained with no evidence of adverse events, these findings suggest that clinicians should consider recommending MBSR to transplant recipients who are bothered by these symptoms, particularly anxiety or poor sleep. We speculate that MBSR may also benefit patients managing other chronic conditions with complex medication regimens.
This is the first randomized controlled trial of MBSR in transplant recipients. Benefits from a non-pharmacologic intervention are particularly important for this chronically ill population dependent on lifelong immune-suppression because 40–50% of transplant recipients report elevated anxiety and depression symptoms and reduced quality of life during the first few years after transplantation.5–7 Corticosteriods, a key component of many immune suppressive regimens, may worsen anxiety and depression symptoms, while neuropathies and osteoporosis, conditions common among transplant recipients, may cause or exacerbate sleep problems. Depressed mood, anxiety and sleep problems are risk factors for morbidity, noncompliance, and mortality.41–42
This is the first controlled trial to find that a standard MBSR program provides specific and sustained benefits to sleep. Reduced arousal and interruption of sleep-incompatible cognitions such as worries and rumination have been proposed to account for the impact of MBSR on sleep.43 Comments written in study questionnaires illustrated how patients used their MBSR training to deal with poor sleep and other stressors: “I am using the body scan at bedtime. It is hectic to go to sleep with a bipap, however the body scan helps.”; “This class has provided me with several ways of coping with my severe itching”, “I can sleep better because I can use the breathing to help me get to sleep.” Participants also commented on mindfulness helping them deal with side effects and stressful situations: “I tend to turn to mindfulness thinking when I’m having severe side effects.”; “I have learned to find peace & quiet in places I never thought [possible].”
Reasons for lack of improvement in physical health reports or pain symptom perceptions are unclear, but not wholly unexpected. The impairments to physical health experienced by transplant recipients include conditions such as amputations due to diabetes or fractures due to osteoporosis. These conditions limit the capacity for improvement on objective items assessing physical function (i.e., climbing stairs) that are heavily weighted in the physical health summary. In this context, the vitality results which are based on questions about feeling full of life and energy as opposed to feeling tired and worn out are particularly encouraging.
This was an unblinded trial, and the primary outcomes were self-reports. These limitations reflect the nature of the interventions and symptom outcomes. Other limitations were attrition and missing evaluations. These problems were evenly distributed across the interventions, however, suggesting participants did not prefer one program over the other, or have differing expectations of benefit. We have some confidence that our trial attracted a representative sample of transplant recipients. There were few exclusion criteria, and more than half of those who inquired about the study were enrolled. Consistent with transplant demographics, our trial included more men than women. Methodological concerns raised in recent reviews of MBSR, including format variations, and lack of active controls were addressed. 44–46
Based on findings reported in this trial, health care providers should consider recommending that solid organ transplant recipients who are in stable health and receiving regular medical care consider enrolling in a standard MBSR program. The MBSR program appears to be particularly beneficial to those with poor sleep quality and anxiety. It would be prudent to regularly screen all transplant recipients for treatable sleep disorders such as obstructive sleep apnea and restless legs syndrome, and evaluate recipients for clinical depression or anxiety disorders, to ensure appropriate therapies are instituted, in addition to recommending this complementary therapy for self-management.
Acknowledgments
Funding sources: National Institutes of Health, National Institute of Nursing Research grant R01 NR008585 and National Center for Research Resources grant M01 RR00400.
We thank Pat Koppa, MPH, Henry Emmons, MD and Terry Pearson, RPh for their contributions to the preparation and delivery of the study interventions.
LIST OF ABBREVIATIONS
- CES-D
Center for Epidemiologic Studies - Depression Scale
- CI
confidence interval
- ES
effect size
- ITT
intention-to-treat
- MAAS
Mindful Attention Awareness Scale
- MBSR
Mindfulness-Based Stress Reduction
- PSQI
Pittsburgh Sleep Quality Index
- QOL
quality of life
- SF-12
Short Form-12 Health Survey, Version 2
- SF-36
Short Form-36 Health Survey, Version 2
- STAI
State-Trait Anxiety Inventory
- VAS
visual analogue scale
Footnotes
Work was performed at the University of Minnesota, Minneapolis, MN
Trial Registration: ClinTrials.gov identifier NCT00367809
References
- 1.UNOS. Annual Report of the US Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1997–2006. Department of Health and Human Services Rockville MD United Network for Organ Sharing Richmond VA Arbor Research Collaborative for Health; Ann Arbor, MI: 2007. [Google Scholar]
- 2.Gross CR, Limwattananon C, Matthees B, Zehrer JL, Savik K. Impact of transplantation on quality of life in patients with diabetes and renal dysfunction. Transplantation. 2000;70(12):1736–1746. doi: 10.1097/00007890-200012270-00013. [DOI] [PubMed] [Google Scholar]
- 3.Gross CR, Malinchoc M, Kim RW, et al. Quality of life before and after liver transplantation for cholestatic liver disease. Hepatology. 1999;29:356–364. doi: 10.1002/hep.510290229. [DOI] [PubMed] [Google Scholar]
- 4.Cohen L, Littlefield C, Kelly P, Maurer J, Abbey S. Predictors of quality of life and adjustment after lung transplantation. Chest. 1998;113(3):633–644. doi: 10.1378/chest.113.3.633. [DOI] [PubMed] [Google Scholar]
- 5.Dew MA, Kormos RL, DiMartini AF, et al. Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics. 2001;42(4):300–313. doi: 10.1176/appi.psy.42.4.300. [DOI] [PubMed] [Google Scholar]
- 6.Russell RT, Feurer ID, Wisawatapnimit P, Salomon RM, Pinson C. The effects of physical quality of life, time and gender on change in symptoms of anxiety and depression after liver transplantation. J Gastrointest Surg. 2008;12:138–144. doi: 10.1007/s11605-007-0382-x. [DOI] [PubMed] [Google Scholar]
- 7.Goetzmann L, Ruegg L, Stamm M, Ambuhl P, Boehler A, et al. Psychosocial profiles after transplantation: A 24-month follow-up of heart, lung, liver, kidney and allogeneic bone-marrow patients. Transplantation. 2008;86(5):662–668. doi: 10.1097/TP.0b013e3181817dd7. [DOI] [PubMed] [Google Scholar]
- 8.Baines LS, Joseph JT, Jindal RM. Prospective randomized study of individual and group psychotherapy versus controls in recipients of renal transplants. Kidney International. 2004;65:1937–1942. doi: 10.1111/j.1523-1755.2004.00594.x. [DOI] [PubMed] [Google Scholar]
- 9.Keown P. Improving quality of life--the new target for transplantation. Transplantation. 2001;72(12 Suppl):S67–74. [PubMed] [Google Scholar]
- 10.Fusar-Poli P, Lazzaretti M, Ceruti M, et al. Depression after lung transplantation: causes and treatment. Lung. 2007;185:55–65. doi: 10.1007/s00408-006-0093-1. [DOI] [PubMed] [Google Scholar]
- 11.Gross CR, Kreitzer MJ, Russas V, Treesak C, Frazier PA, Hertz MI. Mindfulness meditation to reduce symptoms after organ transplant: A pilot study. Alternative Therapies in Health and Medicine. 2004;10(3):58–66. [PubMed] [Google Scholar]
- 12.Kreitzer MJ, Gross CR, Ye X, Russas V, Treesak C. Longitudinal impact of mindfulness meditation on illness burden in solid-organ transplant recipients. Progress in Transplantation. 2005;15(2):166–172. doi: 10.1177/152692480501500210. [DOI] [PubMed] [Google Scholar]
- 13.Anonymous. [Accessed March, 2009];Center for Mindfulness in Medicine, Health Care and Society, UMass. 2009 www.umassmed.edu/cfm/index.aspx/
- 14.Kabat-Zinn J. Full Catastrophe Living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing; 1990. [Google Scholar]
- 15.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. Journal of Clinical Psychology. 2006;82(3):373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- 16.Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosomatic Medicine. 2000;62(5):613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Kabat-Zinn J, Wheeler E, Light T, et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA) Psychosomatic Medicine. 1998;60(5):625–632. doi: 10.1097/00006842-199809000-00020. [DOI] [PubMed] [Google Scholar]
- 18.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 19.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 20.Miller J, Fletcher K, Kabat-Zinn J. Three year follow-up and clinical implications of a mindfulness-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- 21.Bishop S. What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine. 2002;64:71–84. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 23.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. 1. New York: Guilford; 2002. [Google Scholar]
- 24.Gross CR, Kreitzer MJ, Reilly-Spong M, Winbush N, Schomaker E, Thomas W. Mindfulness meditation training to reduce symptom distress in transplant patients: Rationale, design and experience with a recycled waitlist. Clinical Trials. 2009;6:76–89. doi: 10.1177/1740774508100982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santorelli SF, Kabat-Zinn J. Mindfulness-based Stress Reduction Professional Training: MBSR Curriculum Guide and Supporting Materials. Worcester, MA: Center for Mindfulness in Medicine, Health Care and Society; 2002. [Google Scholar]
- 26.Baer R. Mindfulness-Based Treatment Approaches: A clinician’s guide to evidence-base and applications. Elsevier Academic Press; Amsterdam: 2006. [Google Scholar]
- 27.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Medical Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Lorig K, Holman H, Sobel D, Laurent D, Gonzalez V, Minor M. Living a Healthy Life with Chronic Conditions: self-management of heart disease, arthritis, diabetes, asthma, bronchitis, emphysema and others. 2. Palo Alto, CA: Bull Publishing; 2000. [Google Scholar]
- 29.Spielberger C. Manual for the State-Trait Anxiety Inventory (Form Y) Redwood City, CA: Mind Garden, Inc; 1983. [Google Scholar]
- 30.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;3:385–401. [Google Scholar]
- 31.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 32.McDowell I. Measuring Health: A Guide to Rating Scales and Questionnaires. 3. New York: Oxford University Press; 2006. [Google Scholar]
- 33.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of Psychosomatic Research. 1998;45(1):5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 34.Ware JE, Jr, Kosinski MA, Turner-Bowker DM, Gandek B. How to score Version 2 of the SF-12 Health Survey. Boston MA: QualityMetric Inc. and Health Assessment Lab; 2002. [Google Scholar]
- 35.Ware J, Kosinski M, Dewey J. How to score version 2 of the SF-36(R) Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- 36.Kind P. The EuroQoL Instrument: an index of health-related quality of life. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2. Philadelphia, PA: Lippincott-Raven Publishers; 1996. pp. 191–201. [Google Scholar]
- 37.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 38.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 39.Algina J, Keselman HJ. Approximate confidence intervals for effect sizes. Educational and Psychological Measurement. 2003;63(4):537–553. [Google Scholar]
- 40.Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology Science and Practice. 2003;10(2):125–143. [Google Scholar]
- 41.Dew MA, Kormos RL, Roth LH, Murali S, DiMartini A, Griffith BP. Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. The Journal of Heart and Lung Transplantation. 1999;18(6):549–562. doi: 10.1016/s1053-2498(98)00044-8. [DOI] [PubMed] [Google Scholar]
- 42.Noohi S, Khaghani-Zadeh M, Javadipour M, et al. Anxiety and depression are correlated with higher morbidity after kidney transplantation. Transplant Proceedings. 2007;39:1074–1078. doi: 10.1016/j.transproceed.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 43.Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin Psychol Rev. 2005;25(5):629–644. doi: 10.1016/j.cpr.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 44.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- 45.Ospina M, Bond T, Karkhaneh M, et al. Meditation Practices for Health: State of the Research. Rockville, MD: Agency for Healthcare Research and Quality; Jun, 2007. [Google Scholar]
- 46.Toneatto T, Nguyen L. Does mindfulness meditation improve anxiety and mood symptoms? A review of controlled research. La Revue Canandienne de Psychiatrie. 2007;52(4):260–266. doi: 10.1177/070674370705200409. [DOI] [PubMed] [Google Scholar]