Abstract
BACKGROUND:
Sport- and recreation-related injuries are a major source of morbidity in the paediatric population. Long-term trends for these injuries are largely unknown.
METHODS:
A traumatic injury surveillance system (the Canadian Hospitals Injury Reporting and Prevention Program) was used to examine the demographics and trends of paediatric sports injuries in children who presented to or were directly admitted to the British Columbia Children’s Hospital (Vancouver, British Columbia) emergency department or intensive care unit from 1992 to 2005.
RESULTS:
Over the 14-year study period, there was a significant increase in sport- and recreation-related injuries among patients who presented to the British Columbia Children’s Hospital. Of 104,414 injuries between 1992 and 2005, 27,466 were related to sports and recreational activities. The number of sport-related injuries increased by 28%, while all-cause injuries did not change significantly. Males comprised 68% of the sport-related injuries, and both sexes displayed an increasing trend over time. Cycling, basketball, soccer and ice hockey were the top four injury-causing activities. The main body parts injured were the face, head and digits.
CONCLUSIONS:
Paediatric sports injuries significantly increased at the British Columbia Children’s Hospital over the 14-year study period. This is likely due to increased sport participation, increased risk associated with certain sports, or both. Trends in paediatric sports injury may be predicted by changes in popular media, possibly allowing prevention programs to help to avoid these injuries before they occur.
Keywords: Athletic injuries, Epidemiology, Injuries, Paediatrics, Sports, Wounds
Abstract
HISTORIQUE :
Les blessures liées aux activités sportives et de loisir constituent une importante source de morbidité au sein de la population pédiatrique. On ne sait pas grand-chose des tendances à long terme de ces blessures.
MÉTHODOLOGIE :
Les chercheurs ont recouru à un système de surveillance des blessures traumatiques (le Système canadien hospitalier d’information et de recherche en prévention des traumatismes) pour examiner la démographie et les tendances des blessures sportives des enfants qui ont consulté au département d’urgence ou à l’unité de soins intensifs du British Columbia Children’s Hospital (de Vancouver, en Colombie-Britannique) ou y ont été admis entre 1992 et 2005.
RÉSULTATS :
Pendant les 14 ans de l’étude, on a constaté une augmentation significative des blessures causées par des activités sportives et de loisir chez les patients qui consultaient au British Columbia Children’s Hospital. Sur les 104 414 blessures subies entre 1992 et 2005, 27 466 étaient liées à des activités sportives et de loisir. Le nombre de blessures liées à une activité sportive a augmenté de 28 %, tandis que les blessures toutes causes confondues n’ont pas changé de manière significative. Les personnes de sexe masculin ont subi 68 % des blessures liées à une activité sportive, mais on a remarqué une augmentation de la tendance au fil du temps chez les deux sexes. Le vélo, le basketball, le soccer et le hockey sur glace étaient les quatre principales activités responsables de blessures. Les parties les plus touchées étaient le visage, la tête et les doigts.
CONCLUSIONS :
Les blessures causées par une activité sportive en pédiatrie ont considérablement augmenté au British Columbia Children’s Hospital pendant les 14 ans de l’étude. C’est probablement attribuable à une participation accrue aux activités sportives, à un risque accru associé à certaines activités sportives ou à ces deux phénomènes. On pourrait prévoir les tendances des blessures sportives en pédiatrie en apportant des changements dans les médias populaires, qui permettent aux programmes de prévention de contribuer à éviter ces blessures avant qu’elles se produisent.
Sport- and recreation-related injuries are a major source of morbidity in the paediatric population in Canada and the United States (US). In the US, sport-related visits to the emergency department are predominantly made by children and adolescents (1–3). More than 44 million children and adolescents participate in organized sports in the US every year (4), and this number is increasing (5). Approximately 2.4 million paediatric sport- and recreation-related injuries present to US emergency departments annually (3).
The impact of paediatric sport-related injuries on families, schools, teams, health care systems and the children themselves is significant. They cause physical pain, emotional stress and a considerable financial burden (5–7). The large numbers of sport-related injuries that occur in Canada generate valuable epidemiological and preventive research (8).
Sport- and recreation-related injuries account for many emergency visits to the British Columbia Children’s Hospital (BCCH; Vancouver, British Columbia [BC]), Canada’s second largest paediatric health facility. The epidemiology of these injuries can be examined using data from the Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP) (9,10).
The present study determined trends in paediatric sport injury using data from BCCH, and tested the hypothesis that sport-related injuries are seen more frequently over time at this hospital. Using BCCH CHIRPP data from 1992 to 2005, we analyzed reported injury trends within sport-related injury as a whole, and then by individual sports. Understanding these trends supports the development of specific prevention programs. Furthermore, these trends can be used for public education purposes.
METHODS
CHIRPP is a computerized surveillance system operated by the Public Health Agency of Canada that began collecting emergency department trauma data in 1990. Unique to BCCH, direct admissions to the intensive care unit are also included in CHIRPP data. On arrival to BCCH, the accompanying adult indicates the patient’s sex and age, time and place of injury, cause of injury, and activity at the time of injury on a CHIRPP data form. Medical staff specify the nature of the injury, affected body parts and the treatment provided. The forms are sent to a central data entry facility at the Public Health Agency of Canada in Ottawa, Ontario, where the data are coded with more than 40 searchable variables (11).
All records in which the cause of trauma was related to sport participation were extracted. A sport or recreational activity was defined as increased physical exertion for the purposes of competition or recreation (1), thereby including activities such as cycling, dodgeball and others.
Trends and linear regression outputs were generated for each sport as a function of the 14-year period, as well as for sex, age group, time, body part and treatment. Statistical significance was established at P≤0.05. Due to the under-representation of 15- to 19-year-old adolescents in CHIRPP data – likely because of nearby general hospitals – age group injuries were reported as proportions of total injuries sustained by that age group (12). Of the 84 sports coded and analyzed, the present report highlights those with the highest injury numbers, or those that demonstrated changing trends. The results are presented for all sports as a group and then according to individual sports. The injury frequency and trends, injured body parts, age group distribution and admission risk are analyzed and described for each sport, followed by the discussion in the same sport order. The study was approved by the University of BC Clinical Research Ethics Board (Vancouver).
RESULTS
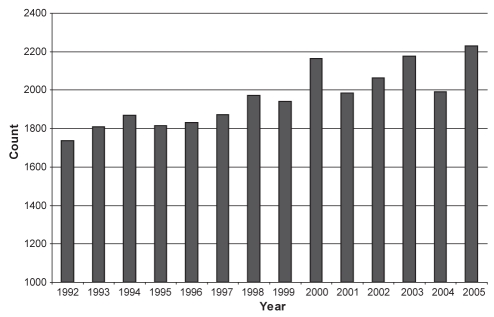
The complete BCCH CHIRPP dataset from 1992 to 2005 was comprised of 104,414 injuries. Of these, 27,466 (26.3%) were identified as sport-related injuries. The number of reported sports injuries significantly increased from 1737 in 1992, to 2231 in 2005 (P<0.001) (Figure 1), representing a 28.4% increase over the 14-year period. In contrast, the total number of injuries seen in the emergency room or intensive care unit did not change significantly over the course of the study (P=0.80) (annual average: 7458 injuries). Males experienced more sports injuries than females (68% versus 32%), and injuries for both sexes increased significantly over time (male P<0.001; female P=0.02). Injuries most frequently occurred at school (29.6%) and in public parks (11.1%).
Figure 1).
Paediatric sport-related injuries in children presenting to the British Columbia Children’s Hospital (Vancouver, British Columbia) emergency department from 1992 to 2005. The total sport-related injury count was 27,466, and showed an increasing trend over time (28.4% increase; P<0.001). Injuries due to all causes did not significantly increase or decrease over time (n=104,414; P=0.80)
The body parts most frequently injured were the face (12.7%), head (11.2%) and digits (11.0%). Between 1992 and 2005, face injuries decreased from 289 to 226 (P<0.001), while head injuries increased from 196 to 284 (P=0.008 for linear regression of head injury counts). As a proportion of total injuries, head injuries also increased from 11.3% to 12.7%, but did not reach statistical significance (P=0.3). Digit injuries remained stable. Overall, the leading types of injuries that resulted in admission to hospital were to the head (20.6%) and forearm (17.3%). Admissions to hospital for sport-related head injuries increased from 21 in 1992, to 34 in 2005 (P=0.11). Face and digit injuries resulted in 5.3% and 2.3% of admissions, respectively.
Children were admitted to hospital for 6.6% (n=1810) of all sport-related injury visits to BCCH, while admission for all-cause injuries was 7.1% (n=7368). The sports with the highest injury and admission numbers are shown in Table 1. By age group, only children 10 to 14 years of age showed a significant upward trend from 1992 (489/1000 injuries) to 2005 (565/1000 injuries) (P<0.001).
TABLE 1.
The top 10 paediatric sport/recreation injuries presenting to the British Columbia Children’s Hospital (Vancouver, British Columbia) from 1992 to 2005 according to sex and admission risk
| Sport: total (%) | Trend | Sport: male (%) | Sport: female (%) | Admission risk (%) |
|---|---|---|---|---|
| Cycling (13.5) | NC (P=0.15) | Cycling (14.7) | Cycling (11.3) | Alpine skiing (13.8) |
| Basketball (11.7) | NC (P=0.77) | Basketball (12.6) | Soccer (10.3) | Trampoline (12.7) |
| Soccer (10.7) | I (P<0.001) | Soccer (10.9) | Basketball (10.0) | Snowboarding (12.0) |
| Ice hockey (5.4) | I (P<0.001) | Ice hockey (7.7) | Ice skating (5.3) | Cycling (11.3) |
| Baseball (4.7) | D (P=0.002) | Football (5.1) | Trampoline (5.0) | Skateboarding (9.2) |
| Ice skating (3.8) | D (P<0.001) | Baseball (4.6) | Baseball (5.0) | Inline skating (9.2) |
| Football (3.8) | NC (P=0.46) | Skateboarding (3.9) | Gymnastics (4.6) | Tag (6.8) |
| Inline skating (3.5) | D (P=0.003) | Inline skating (3.1) | Inline skating (4.4) | Physical education (6.7) |
| Trampoline (3.2) | I (P=0.013) | Ice skating (3.0) | Volleyball (3.6) | Gymnastics (4.5) |
| Skateboarding (3.0) | I (P<0.001) | Rugby (3.0) | Physical education (3.1) | Rugby (4.2) |
D Decreasing trend; I Increasing trend; NC No change
Cycling, with the highest number of injuries (n=3719; 13.5% of all sports injuries), showed no significant change over time (mean of 266 injuries/year; P=0.15). Most cycling injuries were sustained by males (73%). Male injuries did not significantly change over time (P=0.88), while female injuries decreased from 97 to 56 from 1992 to 2005 (P=0.001). The body parts injured most frequently were the face (15.3%), head (13.1%) and forearm (11.5%). For head injuries, there were 33 per year from 1992 to 1996, a minimum of 17 in 1997, then an average of 39 per year from 1998 to 2005. In records with safety equipment information (52%), 77% occurred while the child was recorded as wearing a helmet. Similar to the head injury pattern, the number of injuries recorded with helmet use averaged 84 per year from 1992 to 1996, was a minimum of 30 in 1997, and had a higher average of 129 per year from 1998 to 2005. This pattern was not found for injuries recorded without a helmet. Age groups were well distributed: 10 to 14 years (56/1000 injuries), five to nine years (56/1000 injuries), 15 to 19 years (36/1000 injuries), and two to four years (14/1000 injuries). Admission risk was 11.3%, mostly for head injuries (29%). Cycling helmet users had a nonsignificant (P=0.22) trend toward a lower all-cause admission rate (11.1%) compared with nonhelmet users (13.2%).
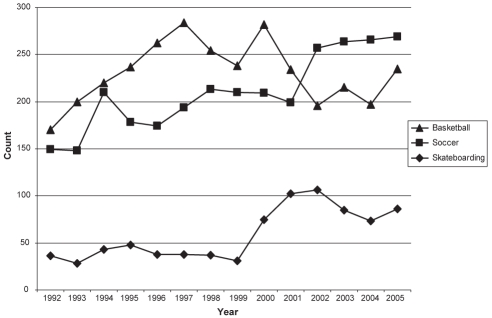
Basketball had the second highest number of injuries with 3224 visits (11.7%), but there was no significant increase or decrease over time (mean of 230 injuries/year; P=0.77) (Figure 2). The annual injury counts from 1995 to 2001 were all above the mean (mean of 256 per year), while they were below the mean before 1995 and after 2001. Males comprised 73% of the visits, most injuries occurred in January and February, and the body parts most frequently injured were the digits (22%), ankles (16%) and head (11%). The 15- to 19-year-old age group was proportionately injured the most (95/1000 injuries), followed by the 10- to 14-year-old (78/1000 injuries) and five- to nine-year-old (10/1000 injuries) groups. In adolescents 15 to 19 years of age, the ankle was the most frequently injured body part (24%). In children five to 14 years of age, the digits and hand were injured most frequently (34%). Admission risk was 3.5%.
Figure 2).
Basketball, soccer and skateboarding injuries in children presenting to the British Columbia Children’s Hospital (Vancouver, British Columbia) from 1992 to 2005. The total injury count for basketball was 3224, and did not significantly increase or decrease over time (P=0.77). The total injury count for soccer was 2940, and showed an increasing trend over time (P<0.001). The average number of skateboarding injuries from 1992 to 1999 was 37 per year, and was 88 per year from 2000 to 2005
Soccer injuries (n=2940; 10.7%) nearly doubled from 149 in 1992, to 269 in 2005 (Figure 2). Males comprised 69% of the injuries. However, the number of injuries for both sexes increased (P<0.001). The number of female injuries increased from 33 in 1992, tripling to 101 in 2005. Most injuries occurred in September and October. Although both sexes primarily injured their ankles, females suffered a higher proportion of lower limb injuries, while males experienced more hand and head injuries. Age groups with the most injuries were 15 to 19 years (66/1000 injuries), 10 to 14 years (59/1000 injuries) and five to nine years (27/1000 injuries), all of which increased. Admission risk was 3.2%.
Ice hockey injuries (n=1489; 5.4%) increased from 65 in 1992, to 161 in 2005. Males comprised 96% of the injuries, and displayed a 140% increase (P<0.001). Female injuries increased by approximately 230% (P=0.008), although the numbers were comparatively low. Head and face injuries were the most common for both sexes (22%) and the main age groups. Face injuries decreased during the time period (P=0.003), while head injuries increased (P<0.001). Age groups with the most injuries included 15 to 19 years (45/1000 injuries) and 10 to 14 years (36/1000 injuries). Both significantly increased over time (10 to 14 years: P<0.001; 15 to 19 years: P=0.003). Admission risk was 4.1%.
Lacrosse, with 121 injuries, was stable from 1992 to 2001, with 4.3 injuries/year. Then, the injury numbers increased from six in 2001, to 28 in 2005. Males comprised 96% of the injuries and also showed an increasing trend, while females did not. Main body parts injured were the forearm (15%), head (13%) and wrist (13%). Age groups with the most injuries were 15 to 19 years (4/1000 injuries) and 10 to 14 years (3/1000 injuries). A significant upward trend was found only for the 10- to 14-year-old age group (P=0.003). Admission risk was 5.8%.
Skateboarding injuries (n=826; 3.0%) showed an upward trend (P<0.001). The injuries were clustered into two stable groups: from 1992 to 1999 (37 injuries/year) and from 2000 to 2005 (88 injuries/year) (Figure 2).
DISCUSSION
The 27,466 paediatric sport-related injuries seen at BCCH over the 14-year period from 1992 to 2005 presented several trends relevant to clinicians and injury prevention practitioners. Sport injury frequency at BCCH increased over the study period, while total injury counts did not. Whether this was the result of changing behaviours, public education programs or improved safety devices remains unclear. Other possible causes include an increased paediatric population, an increased tendency to present to hospital when injured, an increased preference for BCCH over other hospitals, increased sport participation or increased risk/danger associated with certain sports.
An increased paediatric population is not a convincing explanation for the increased number of sports injuries at BCCH. BC Statistics (13) reported that from 1992 to 2005, zero- to 19-year-old individuals showed an overall 6.4% increase in population, which is substantially lower than the 28.4% increase in reported sport-related injuries at BCCH. Furthermore, the fact that sport-related injuries in our data increased while the total number of injuries remained constant suggests that this trend may have been less influenced by population growth in this region. It also indicates that there was no increased tendency to present to BCCH during this time period. BCCH functions as the tertiary paediatric hospital for the province, and also delivers primary paediatric care for the greater Vancouver region. Over the study period, our hospital’s mandate as the only tertiary paediatric hospital has remained unchanged, with no systemic changes to paediatric referral patterns or care (outpatient or inpatient). This leaves the possibilities of increased sport participation and/or increased riskiness of some sports, several of which are discussed below.
Helmets protect cyclists from head, brain and facial injuries (14–18). In areas with bicycle helmet legislation, helmet use has significantly increased (19–25), while cycling-related head injuries have decreased (26). BC was the first Canadian province to pass mandatory bicycle helmet legislation in 1996. The following year, a clear decrease in head injuries and helmeted cyclist injuries was observed in our data, while this pattern was not observed for non-helmeted cyclist injuries (see Results). However, this decrease was short-lived and injuries began increasing thereafter. This pattern was also observed in the present study among male cyclists. Nevertheless, the annual average of injuries from 1992 to 1996 (prehelmet legislation) was 286, which decreased to 255 from 1997 to 2005. Reflecting the severity of cycling head injuries, 25% of head injuries were admitted, while only 6% of face and 12% of forearm injuries were admitted.
In the present study, female cycling injuries decreased between 1992 and 2005, while male injuries remained stable. Although the proportion of males wearing helmets at the time of injury was greater than the proportion of females (39% versus 33%), it may be that female helmet wearers did not get injured as often – at least not severely enough to warrant a hospital visit. Given the increase in male head injuries despite increased helmet use, the question of safety perception arises. Children may be receiving the safety message, believing that helmets will protect them from serious injury. Armed with this belief and their helmets, they may engage in more high-risk cycling, leading to higher numbers of injuries even with helmet use. Research in other sports addresses this point (27–29). The implications of this point, however, are a topic of debate (30), but should encourage further examination.
In the present study, the number of basketball injuries did not increase. According to Basketball BC, which oversees participation at all levels in this province, participation of five- to 13-year-old children increased evenly throughout BC from approximately 3000 in 1996/1997, to 11,000 in 2006/2007 (M Hind, Executive Director, Basketball BC; personal communication, 2007). They noted a dramatic increase in participation after Vancouver established a professional men’s basketball team in 1995. Interestingly, in our data, the only years in which basketball injuries were above the mean of 230 injuries/year were during this team’s existence between 1995 and 2001 (Figure 2), supporting an important potential link between paediatric sport involvement and subsequent injury, and the media.
The BC Soccer Association, which oversees organized soccer leagues in the province, reported a participation increase of approximately 149% for players younger than 18 years of age from 1992 (n=40,500) to 2005 (n=101,000) (M Reinkens, Player Development, BC Soccer Association; personal communication, 2008). Soccer injuries that presented to BCCH increased 81% over these same 14 years (Figure 2). Without considering informal soccer participation, it appears that participation increased in excess of the rate of BCCH injuries. Therefore, although soccer-related injuries were seen more frequently at BCCH, it is possible that soccer’s emerging popularity has been accompanied by a decrease in associated participation injury risk. This represents an area of success in injury prevention and an opportunity to determine what factors have made it so.
BC hockey participation for 11- to 19-year-old males increased by 20% from 1993/1994 to 2005/2006 (31), while injuries seen at BCCH increased by 140%. Female participation in BC for the five- to 19-year-old group increased by 623% from 1993/1994 to 2005/2006, while injuries at BCCH increased by only 230%. Therefore, it appears that ice hockey increased in popularity and riskiness/danger for males, while it increased only in popularity for females.
Most hockey injuries occur during body checking (28,32–35), and lowering the allowable body checking age lowers the age at which serious injuries may occur (35,36). In Canada, body checking is only permitted for males older than 10 years of age. BC changed their rule in the 2002/2003 season, reducing the minimum allowable body checking age from 14 to 11 years. Apart from a slightly more dramatic increase in injuries seen in 10- to 14-year-old children at BCCH since 2002 and the predominance of injuries in the 10- to 19-year-old group over other age groups in our data, no obvious trends up to 2005 were noted. Despite increased hockey participation in BC, the number of face injuries seen at BCCH declined, supporting the effectiveness of mandatory facial protection. Conversely, head injuries were seen more frequently despite mandatory helmet use. Therefore, head injury among the 10- to 19-year-old age group is an important focus, especially because they were the only age group with significant upward trends, they are body checking and often sustain the most injuries (34).
The dramatic 6.5-fold increase in lacrosse injuries treated at BCCH between 2001 and 2005 likely reflects increased lacrosse popularity (37). The year 2002 marked the first year that Vancouver had a professional lacrosse team. BC registration numbers increased significantly starting in 2001, doubling for males and almost tripling for females by 2006 (R Winterton, Executive Director, BC Lacrosse Association; personal communication, 2007). Therefore, lacrosse serves as another example in which prominence of a sport in media may predict an increase in sport popularity and concomitant injury frequency.
Our skateboarding and dodgeball data further emphasize the link between sport injury and media. Skateboarding injuries increased from 37 injuries/year from 1992 to 1999, to 88 injuries/year from 2000 to 2005 (Figure 2). The first exceedingly popular professional skateboarder, Tony Hawk, gained his fame in 1999 by appearing in widely viewed televised competitions, with the first of his many videogames released that same year. Similarly, dodgeball injuries increased from six injuries/year from 1992 to 2004, to 22 in 2005 – the year after the movie Dodgeball was released. While the cause-and-effect link between these correlations is far from conclusive, further research to verify the relationships between sport participation and injury, and the prominence of that sport or sport personality/role model in the media is warranted.
Male children 10 to 14 years of age comprised twice the number of female injuries in our data, were the age group most commonly admitted to BCCH, were the only age group in which sport injuries significantly increased over time and were the only group in which head injuries were most common. This suggests they are a principal target for sport-related injury prevention, particularly for head injuries, regardless of the sport.
The CHIRPP dataset presents some limitations. Given the difficulty of obtaining accurate hospital catchment populations by year and age, and of determining denominators for paediatric populations participating in sports and recreational activities informally, it is not possible to make incidence conclusions. Our dataset is based on one institution and, hence, our conclusions are not necessarily generalizable to populations. We attempt to place these results in the context of changing paediatric participation in organized sport. This is often on a provincial level and ignores informal participation. Furthermore, our dataset has limitations in reporting specific indicators of interest. For example, only 52% of cycling injury entries provided safety equipment information. Unorganized cycling is particularly challenging because denominator data do not exist, limiting the conclusions drawn from trends. It is also recognized that CHIRPP data, on a population basis, has more comprehensive inclusion of younger children (younger than 14 years of age) and those admitted to hospital (38,39). Our injuries of interest might, therefore, be somewhat under-represented in the CHIRPP data, compared with injury frequencies in the childhood population as a whole. However, this effect is perhaps systematically present throughout the study period, and does not detract from the essential finding of the study – in our institution, sport-related injuries increased consistently over time.
CONCLUSION
Paediatric sport injury frequency steadily increased at BCCH, while all-cause injuries remained stable. In some sports, injury frequency increased more rapidly than reported participation. An understanding of these injury trends and their relationship with the social environment is key for the clinician’s role in injury prevention and education. By paying close attention to popularity trends in paediatric sports and cues from the popular media, one may anticipate changes in paediatric sport injury and, thus, prevention efforts can be commenced in advance. This may be a more effective way of addressing sport injury than playing ‘catch-up’ once a noticeable problem has developed. It is hoped that this report encourages further study into injury patterns, including possible relationships to popular culture events, with the ultimate goal of enabling children to safely participate in sports with a decreased risk of injury.
Acknowledgments
The authors thank Dr Ian Pike for his assistance and review of this manuscript.
REFERENCES
- 1.Burt CW, Overpeck MD. Emergency visits for sports-related injuries. Ann Emerg Med. 2001;37:301–8. doi: 10.1067/mem.2001.111707. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Non-fatal sports- and recreation-related injuries treated in emergency departments, United States, July 2000–June 2001. MMWR Morb Mortal Wkly Rep. 2002;51:736–40. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Nonfatal traumatic brain injuries from sports and recreation activities – United States, 2001–2005. MMWR Morb Mortal Wkly Rep. 2007;56:733–7. [PubMed] [Google Scholar]
- 4.National Council of Youth Sports Report on trends and participation in organized youth sports. < www.ncys.org/pdfs/2008/2008-ncys-market-research-report.pdf> (Accessed on January 24, 2011).
- 5.Goldberg AS, Moroz L, Smith A, Ganley T. Injury surveillance in young athletes – a clinician’s guide to sports injury literature. Sports Med. 2007;37:265–78. doi: 10.2165/00007256-200737030-00005. [DOI] [PubMed] [Google Scholar]
- 6.Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33:75–81. doi: 10.2165/00007256-200333010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Caine D, Caine C, Maffulli N. Incidence and distribution of pediatric sport-related injuries. Clin J Sport Med. 2006;16:500–13. doi: 10.1097/01.jsm.0000251181.36582.a0. [DOI] [PubMed] [Google Scholar]
- 8.Molcho M, Harel Y, Pickett W, et al. The epidemiology of non-fatal injuries among 11-, 13- and 15-year old youth in 11 countries: findings from the 1998 WHO-HBSC cross national survey. Int J Inj Contr Saf Promot. 2006;13:205–11. doi: 10.1080/17457300600864421. [DOI] [PubMed] [Google Scholar]
- 9.Babul S, Nolan S, Nolan M, Rajabali F. An analysis of sport-related injuries: British Columbia children’s hospital emergency department 1999–2003. Int J Inj Contr Saf Promot. 2007;14:192–5. doi: 10.1080/17457300701440659. [DOI] [PubMed] [Google Scholar]
- 10.Macarthur C, Dougherty G, Pless IB. Reliability and validity of proxy respondent information about childhood injury: An assessment of a Canadian surveillance system. Am J Epidemiol. 1997;145:834–41. doi: 10.1093/oxfordjournals.aje.a009177. [DOI] [PubMed] [Google Scholar]
- 11.Public Health Agency of Canada Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP): A unique source of child injury information. < www.phac-aspc.gc.ca/injury-bles/chirpp/index.html> (Accessed on January 24, 2011).
- 12.Mackenzie SG, Pless IB. CHIRPP: Canada’s principal injury surveillance program. Inj Prev. 1999;5:208–13. doi: 10.1136/ip.5.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.British Columbia Statistics, Ministry of Labour and Citizens’ Services British Columbia, Other Provincial and Territorial Populations: 1971–2006. < www.bcstats.gov.bc.ca/data/pop/pop/estspop.asp#agesex> Accessed on January 24, 2011.
- 14.Attewell RG, Glase K, McFadden M. Bicycle helmet efficacy: A meta-analysis. Accid Anal Prev. 2001;33:345–52. doi: 10.1016/s0001-4575(00)00048-8. [DOI] [PubMed] [Google Scholar]
- 15.Finnoff JT, Laskowski ER, Altman KL, Diehl NN. Barriers to bicycle helmet use. Pediatrics. 2001;108:e4. doi: 10.1542/peds.108.1.e4. [DOI] [PubMed] [Google Scholar]
- 16.Finvers KA, Strother RT, Mohtadi N. The effect of bicycling helmets in preventing significant bicycle-related injuries in children. Clin J Sport Med. 1996;6:102–7. doi: 10.1097/00042752-199604000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Thompson DC, Rivara FP, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev. 2000;2:CD001855. doi: 10.1002/14651858.CD001855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thompson RS, Rivara FP, Thompson DC. A case-control study of the effectiveness of bicycle safety helmets. N Engl J Med. 1989;320:1361–7. doi: 10.1056/NEJM198905253202101. [DOI] [PubMed] [Google Scholar]
- 19.Coté TR, Sacks JJ, Kresnow M, et al. Bicycle helmet use among Maryland children: Effect of legislation and education. Pediatrics. 1992;89:1216–20. [PubMed] [Google Scholar]
- 20.Dannenberg A, Gielen AC, Beilenson PL, Wilson MH, Joffe A. Bicycle helmet laws and educational campaigns: An evaluation of strategies to increase children’s helmet use. Am J Public Health. 1993;83:667–74. doi: 10.2105/ajph.83.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foss RD, Beirness DJ. Bicycle helmet use in British Columbia: Effects of the helmet use law. University of North Carolina Highway Safety Research Center. < www.hsrc.unc.edu/research_library/bibliography_2000.cfm> (Accessed on January 24, 2011).
- 22.Hagel BE, Rizkallah JW, Lamy A, et al. Bicycle helmet prevalence two years after the introduction of mandatory use legislation for under 18 year olds in Alberta, Canada. Inj Prev. 2006;12:262–5. doi: 10.1136/ip.2006.012112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LeBlanc JC, Beattie TL, Culligan C. Effect of legislation on the use of bicycle helmets. CMAJ. 2002;166:592–5. [PMC free article] [PubMed] [Google Scholar]
- 24.Ni H, Sacks JJ, Curtis L, Cieslak PR, Hedberg K. Evaluation of a statewide bicycle helmet law via multiple measures of helmet use. Arch Pediatr Adolesc Med. 1997;151:59–65. doi: 10.1001/archpedi.1997.02170380063010. [DOI] [PubMed] [Google Scholar]
- 25.Parkin PC, Khambalia A, Kmet L, Macarthur C. Influence of socioeconomic status on the effectiveness of bicycle helmet legislation for children: A prospective observational study. Pediatrics. 2003;112:e192–6. doi: 10.1542/peds.112.3.e192. [DOI] [PubMed] [Google Scholar]
- 26.Macpherson AK, To TM, Macarthur C, Chipman ML, Wright JG, Parkin PC. Impact of mandatory helmet legislation on bicycle-related head injuries in children: A population-based study. Pediatrics. 2002;110:e60. doi: 10.1542/peds.110.5.e60. [DOI] [PubMed] [Google Scholar]
- 27.Murray TM, Livingston LA. Hockey helmets, face masks, and injurious behavior. Pediatrics. 1995;95:419–21. [PubMed] [Google Scholar]
- 28.Reid SR, Losek JD. Factors associated with significant injuries in youth ice hockey players. Pediatr Emerg Care. 1999;15:310–3. doi: 10.1097/00006565-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Tator CH, Edmonds VE. National survey of spinal injuries in hockey players. CMAJ. 1984;130:875–80. [PMC free article] [PubMed] [Google Scholar]
- 30.Pless IB, Magdalinos H, Hagel B. Risk-compensation behavior in children: Myth or reality? Arch Pediatr Adolesc Med. 2006;160:610–4. doi: 10.1001/archpedi.160.6.610. [DOI] [PubMed] [Google Scholar]
- 31.Hockey Canada. Male to Female Registration Comparison < www.hockeycanada.ca/index.php/ci_id/60781/la_id/1.htm> (Accessed on January 24, 2011).
- 32.Emery CA, Meeuwisse WH. Injury rates, risk factors, and mechanisms of injury in minor hockey. Am J Sports Med. 2006;34:1960–9. doi: 10.1177/0363546506290061. [DOI] [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics, Committee on Sports Medicine and Fitness Safety in youth ice hockey: The effects of body checking. Pediatrics. 2000;105:657–8. doi: 10.1542/peds.105.3.657. [DOI] [PubMed] [Google Scholar]
- 34.Hostetler SG, Xiang H, Smith GA. Characteristics of ice hockey-related injuries treated in US emergency departments, 2001–2002. Pediatrics. 2004;114:e661–6. doi: 10.1542/peds.2004-1565. [DOI] [PubMed] [Google Scholar]
- 35.Macpherson A, Rothman L, Howard A. Body-checking rules and childhood injuries in ice hockey. Pediatrics. 2006;117:e143–7. doi: 10.1542/peds.2005-1163. [DOI] [PubMed] [Google Scholar]
- 36.Hagel BE, Marko J, Dryden D, Couperthwaite AB, Sommerfeldt J, Rowe BH. Effect of bodychecking on injury rates among minor ice hockey players. CMAJ. 2006;175:155–60. doi: 10.1503/cmaj.051531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lincoln AE, Hinton RY, Almquist JL, Lager SL, Dick RW. Head, face, and eye injuries in scholastic and collegiate lacrosse: A 4-year prospective study. Am J Sports Med. 2007;35:207–15. doi: 10.1177/0363546506293900. [DOI] [PubMed] [Google Scholar]
- 38.Macarthur C, Pless IB. Sensitivity and representativeness of a childhood injury surveillance system. Inj Prev. 1999;5:214–6. doi: 10.1136/ip.5.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Macpherson AK, White HL, Mongeon S, et al. Examining the sensitivity of an injury surveillance program using population-based estimates. Inj Prev. 2008;14:262–5. doi: 10.1136/ip.2008.018374. [DOI] [PubMed] [Google Scholar]