Abstract
This study examined maternal depression, attachment avoidance, and attachment anxiety as moderators of Early Head Start's effects on four parenting outcomes assessed at age 3. Participants (N = 947) were drawn from six sites of the Early Head Start National Research and Evaluation Project, a multi-site randomized trial. Findings suggest more positive program effects for mothers with less initial attachment avoidance or attachment anxiety. First, baseline attachment avoidance moderated EHS program effects on observed maternal supportiveness, such that program mothers with lower baseline attachment avoidance were rated as more supportive of their 3-year-olds than program mothers with higher baseline attachment avoidance. Second, program effects on spanking varied depending on mothers’ baseline attachment anxiety.
Keywords: maternal depression, attachment style, parenting, Early Head Start
The past 20 years have witnessed the proliferation of Early Head Start and other publicly funded programs designed to promote early child development in at-risk families (National Research Council and Institute of Medicine, 2000). Supporting early child-parent relationships is a prominent goal of such programs. Program evaluations have demonstrated important successes, such as the modest but consistently positive effects of Early Head Start on early parenting and child outcomes (Love et al., 2005). Key challenges also exist, however. For example, Early Head Start and similar programs are broad-based in terms of the populations they serve, and no program is equally effective for all participants. An important task for researchers and program developers is to identify the sub-populations whom such programs serve well, and those whom they do not. This information can in turn be leveraged to improve program development and service delivery.
The overarching question guiding the current study is the extent to which broad-based, publicly funded programs with a mandate to support early parent-child relationships can effectively support these relationships when mothers initiate services with particular relationship challenges. Specifically, we examine maternal depression, attachment avoidance, and attachment anxiety as moderators of Early Head Start's effects on four parenting outcomes assessed at age 3.
Maternal depression has well-documented negative effects on early parenting and parent-child relationships (Downey & Coyne, 1990; Goodman & Gotlib, 2002; Lovejoy, Gracyk, O'Hare, & Neuman, 2000) and can also affect intervention program uptake (e.g., Stevens, Ammerman, Putnam, & Van Ginkel, 2002). Maternal attachment avoidance and anxiety security can be measured either via the Adult Attachment Interview (AAI) or via an adult attachment questionnaire. Although the AAI and adult attachment questionnaires both relate predictably to adult functioning and parenting (Edelstein et al., 2004; Goodman, Quas, Batterman-Faunce, Riddlesberger, & Kuhn, 1997; Mikulincer & Shaver, 2007; Rholes, Simpson, & Blakely, 1995; Rholes, Simpson, Campbell, & Grich, 2001; Roisman et al., 2007; Wilson, Rholes, Simpson, & Tran, 2007), they are weakly related to one another (Roisman et al., 2007), and likely tap different aspects of adult attachment. The current study examined mothers’ self-reported attachment avoidance and anxiety, reflecting mothers’ thoughts and feelings about emotional closeness in adult relationships. We expected these thoughts and feelings to affect mothers’ responsiveness to Early Head Start, given the program's emphasis on building closeness in the mothers’ relationships with their infants, as well as the some program sites’ use of home-visiting services that aim to build emotional closeness between mothers and their home visitors.
We had two competing hypotheses. First, we hypothesized that program effects could be weaker for mothers who are depressed and/or high on attachment avoidance or anxiety, if these characteristics interfered with mothers’ abilities to form relationships with service providers and to stay engaged in services. Support for this hypothesis comes from two studies that have found associations between attachment avoidance and a lack of self-disclosure, one using an adult attachment style questionnaire (Mikulincer & Nachshon, 1991), and one using the AAI (Dozier, 1990). A lack of self-disclosure may limit the extent to which a mother communicates her or her child's needs, which may then limit the extent to which services providers can help to address these needs. Further support for the proposed weaker program effects for mothers higher on attachment avoidance or anxiety comes from three studies that used the AAI and found greater program engagement or impacts for secure mothers (Heinicke et al., 2006; Spieker, Nelson, DeKlyen, & Staerkel, 2005), or for mothers who were not classified with the AAI as unresolved (with respect to loss or trauma; Moran, Pederson, & Krupka, 2005).
Alternatively, we hypothesized that program effects could be stronger for mothers who are depressed and/or report greater attachment avoidance or anxiety. Participating in services may prevent program mothers who report depression and/or greater attachment avoidance or anxiety from experiencing the decline in the quality of their relationships with their children that is often seen in families not receiving services (Robinson & Emde, 2004). Moreover, self-reported attachment avoidance and anxiety have both been linked to a greater propensity to self-report psychiatric symptoms (Fortuna & Roisman, 2008; Mikulincer & Shaver, 2007; Simpson & Rholes, 2004). Perceived psychiatric symptoms may in turn motivate mothers to seek and stay engaged in services. This notion has received some support from randomized studies of Olds’ widely disseminated Nurse-Family Partnership program (Olds, 2006). Specifically, effects of this program on a range of maternal and child outcomes are often stronger for mothers with fewer “psychological resources,” resources that include (but are not limited to) good mental health (Olds et al., 2002; 2008; see also Dumont et al., 2008).
Two studies have examined the role of baseline maternal depression and/or attachment style in mothers randomly assigned to Early Head Start. In the national randomized trial of 17 EHS programs (N = 3001), program impacts on child-parent interaction were greater when mothers initially reported more depressive symptoms (Administration for Children and Families [ACF], 2002). Another investigation, in two Early Head Start sites, revealed the strongest program impacts for observed maternal sensitivity and toddlers’ involvement of mother in play when mothers reported both depression and an insecure attachment style (Robinson & Emde, 2004). This study did not separately examine self-reported attachment avoidance or anxiety, however. Interestingly, although there were stronger program effects for the more depressed and insecure mothers, mothers who reported more attachment insecurity were also rated by home visitors as being less engaged in the program (Robinson, Korfmacher, Green, Snoden, & Emde, 2002).
A recent study of six Healthy Families programs examined both maternal depression and adult attachment style (self-reported attachment anxiety and discomfort with trust/dependence) as moderators of program effects (Duggan, Berlin, Cassidy, Burrell, & Tandon, 2009). Healthy Families programs provide regular home visits to new mothers and their infants for up to three years. In this study, for six of seven maternal/parenting outcomes, program effects were moderated by both maternal depression and adult attachment insecurity. Among non-depressed mothers, program effects were concentrated among those with moderate to high attachment anxiety or discomfort with trust/dependence. Among depressed mothers, program effects were concentrated among those with low to moderate attachment insecurity. For example, the program increased mothers’ sensitivity to their infants’ cues among depressed mothers with low to moderate attachment anxiety. Thus, mothers with either self-reported depression or attachment insecurity seemed to benefit most.
In sum, the existing research illustrates that both maternal depression and attachment style can moderate the effects of broad early intervention programs on parent-child interaction. There is some evidence that program effects are stronger for depressed than non-depressed mothers. The research examining mothers’ attachment style as a moderator is mixed. When examined in conjunction with depression, Duggan and her colleagues (2009) found that less maternal attachment avoidance or attachment anxiety enhances program effects, but only when mothers are depressed. Robinson and Emde's (2004) study, however, indicated stronger program effects for mothers who self-reported depression and higher attachment insecurity. These diverging findings may reflect differences in the programs (e.g., Healthy Families services are exclusively home-based, EHS services can be home- and/or center-based), and/or in each study's operationalization of attachment security (i.e., examining attachment security/insecurity along one dimension versus separately examining attachment avoidance and anxiety).
In the current study, we draw on data from a subset of the 17 EHS National Research and Evaluation Project sites, selected on the basis of their having administered a common adult attachment questionnaire at the time of enrollment. We separately examine the two dimensions of attachment insecurity indicated by the literature to be central to the construct: attachment anxiety and attachment avoidance (Mikulincer & Shaver, 2007). We examine mothers’ baseline symptoms of depression, attachment avoidance, and attachment anxiety as moderators of the effects of EHS on four aspects of parenting assessed at age 3: observed maternal supportiveness and intrusiveness, and mothers’ reports of spanking and perceptions of negative interactions with her child.
Method
Participants and Procedures
Participants (N = 947) for the current study came from six sites of the Early Head Start National Research and Evaluation Project, a 17-site, longitudinal evaluation of some of the first federally funded EHS programs for low-income infants, toddlers, and their families (N = 3001; ACF, 2002; Love et al., 2005). In accordance with EHS program eligibility rules, over 90% of participants’ family incomes were at or below the federal poverty level. Half of the participants were randomly assigned to receive EHS child and family services that began between the third trimester of pregnancy and the child's 12th month of age, continued through the child's third year, and consisted of home-based, center-based, or mixed (home- and center-based) services. The control group did not receive EHS services but could receive any other available community services. Of the six sites providing data for the current study, EHS services were home-based (two sites), center-based (two sites), and mixed (two sites).
Baseline demographic data came from interviews conducted by EHS program staff as part of their program recruitment procedures between July, 1996, and September, 1998, when mothers were pregnant or target infants were younger than 1 year old (the mean child age was 3 months). Baseline psychosocial data came from interviews conducted by local research staff shortly before or after random assignment. In-depth data on child and family development came from home-based interviews, observations, and direct child assessments conducted by centrally trained and certified research staff when the target children were approximately 1, 2, and 3 years old. All assessments were conducted in English or Spanish, according to the mother's preference.
The six EHS research sites contributing data to the present study were those who had assessed adult attachment style at the time of enrollment, all using Simpson and Rholes's adult attachment questionnaire (Simpson, 1990; Simpson, Rholes, & Nelligan, 1992). Five of the six sites administered the questionnaire at baseline. One site administered this questionnaire within six months of enrollment. The outcome measures for the present study come from the home-based maternal interview and observational assessment of mother-child interaction conducted when the children were 3 years old.
The sample for the current study includes 947 (91%) of the 1045 mothers from the six sites on the basis of their having baseline adult attachment data. At age 3, 76% of these 947 mothers were interviewed and 67% participated in the mother-child interaction assessment. These retention rates are fairly typical for longitudinal studies of high-risk families, and are somewhat higher in the current subsample than the rates for the national EHS evaluation (ACF, 2002; Love et al., 2005). In the current sample, there was some evidence of differential attrition by age 3, for the maternal interview only, with greater attrition associated with less baseline maternal education and more baseline maternal depressive symptoms (χ2 [2] = 14.09, p < .001, and t [943] = -2.22, p < .05). Retention/attrition by age 3 did not differ significantly for program and control participants, and did not differ on the basis of baseline maternal age, race/ethnicity, family income or structure, child sex, or adult attachment. In the present study, missing data were handled using full information maximum likelihood (FIML) estimation (Schafer and Graham, 2002; Widaman, 2006).
The sample was racially/ethnically diverse (47% White; 26% Black, 22% Latina, 6% other). Mothers ranged in age from 14 to 44 at the time of the pre-enrollment interview (M = 23, SD = 5.28). At this time, 40% of the mothers had not completed high school, 32% had completed high school or a GED, and 29% had completed at least some college. Most (72%) lived with at least one other adult. Approximately half (46%) of the children were male. Table 1 provides baseline demographic characteristics for the sample as a whole and by program/control group. As indicated in the table, program and control participants did not differ significantly at this time.
Table 1.
Descriptive Statistics for Key Variables by Program Group
| Full Sample (N = 947) | Program (n = 490) | Control (n = 455) | Test of Group Differences | |
|---|---|---|---|---|
| EHS participant | 52% | |||
| Maternal age | 22.60 (5.28) | 22.80 (5.43) | 22.38 (5.11) | t (941) = -1.22 |
| Maternal education†† | 1.90 | 1.91 | 1.89 | t (927) = 0.61 |
| Family income (% FPL) | 59.99 (56.55) | 57.36 (51.50) | 63.10 (61.64) | t (783) = 1.42 |
| Family structure: mother lives with partner or other adult(s) | 72% | 70% | 75% | χ2(1) = 2.56 |
| Child sex: male | 46% | 47% | 46% | χ2(1) = 0.76 |
| Maternal race/ethnicity: | χ2(3) =1.06 | |||
| White | 47% | 48% | 46% | |
| Black | 26% | 26% | 25% | |
| Hispanic | 22% | 21% | 22% | |
| Other | 6% | 5% | 7% | |
| Maternal depression | 15.72 (11.43) | 15.67 (11.64) | 15.77 (11.20) | t (943) = 0.13 |
| Attachment avoidance | 22.21(6.39) | 22.51 (6.32) | 21.88 (6.47) | t (943) = -1.50 |
| Attachment anxiety | 11.95 (4.32) | 12.08 (4.32) | 11.81 (4.31) | t (943) = -0.98 |
| Supportiveness (age 3) | 4.08 (0.92) | 4.08 (0.91) | 4.09 (0.93) | t (616) = 0.17 |
| Intrusiveness (age 3) | 1.52 (0.77) | 1.53 (0.78) | 1.52 (0.77) | t (616)= -0.16 |
| Spanked, past week (age 3) | 48% | 45% | 52% | χ2(1) = 4.31* |
| Perceived Negative Interactions (age 3) | 9.07 (3.81) | 9.40 (4.11) | 8.66 (3.37) | t (703) = -2.57* |
Note. Standard deviations are in parentheses.
Maternal education was coded on a 3-point scale (2= high school graduate/GED).
p < 0.05
Measures
Maternal Depression
We measured maternal depression with the Center for Epidemiologic Studies Depression Scale (CES-D; Husaini, Neff, Harrington, Hughes, & Stone, 1980; Radloff, 1977). The CES-D, a 20-item, self-report instrument designed to measure depressive symptoms in the general population, is the most widely used measure of depressive symptoms in community-based studies. During the baseline psychosocial interview, mothers completed the CES-D to assess the frequency of symptoms such as sadness, lethargy, and appetite loss during the week prior to the interview. Mothers responded on a 4-point scale (0 = rarely/never; 1 = some/a little; 2 = occasionally/moderately; 3 = most/all days). Responses were summed and scores ranged from 0 to 58 (α = 0.87; see Table 1).
Attachment Avoidance and Anxiety
We measured attachment avoidance and anxiety using Simpson and Rholes's 13-item, 7-point likert scale, designed to tap self-reported feelings about romantic partners (Simpson, 1990; Simpson et al., 1992). Because EHS research participants’ romantic partnerships are often unstable (e.g., at baseline, 58% of the mothers were neither married nor living with a romantic partner), after consultation with Dr. W.S. Rholes (personal communication, July 10, 1996), the questionnaire was re-worded slightly to ask mothers to report on their feelings about “people emotionally close to you.” Thus, mothers rated the extent to which they “don't like people getting too close to me,” “worry that people close to me don't really love me,” “worry about being abandoned by others,” and so on. In addition, to facilitate administration, in 3 of the 6 sites providing data to the current study, the 7 response categories were collapsed to 5 response categories. For consistency, in the present study, we collapsed all 7-point scales to 5-point scales. In all cases, mothers responded from “strongly disagree” (1) to “strongly agree” (5 or 7).
Following Simpson et al. (1992), we examined two subscales, one tapping attachment avoidance (8 items, α = 0.71), and one tapping attachment anxiety (5 items, α = 0.58; these internal consistency reliabilities are quite similar to those reported by Simpson [1990], and Simpson et al. [1992]). These two scales have been linked in theoretically predicted ways to romantic relationship quality and to self-reported and observed parenting behavior (Rholes et al., 1995; Simpson et al., 1992; Rholes et al., 2001; Wilson et al., 2007). Responses to the 8 avoidance items were summed; scores ranged from 8 to 40. Responses to the 5 anxiety items were also summed; scores ranged from 5 to 25 (see Table 1).
Observed Maternal Supportiveness and Intrusiveness
Observers’ ratings of maternal supportiveness and intrusiveness came from a 10-minute videotaped observation of mother-child interaction at age 3, the “Three Bag.” The protocol for this semi-structured play assessment was adapted from Vandell (1979) and from the NICHD Study of Early Child Care's (NICHD Early Child Care Research Network, 1999). Instructions to the mother were intentionally vague in order to elicit naturally occurring parenting behaviors. The assessor gave the mother 3 numbered cloth bags, told her that they were for her and her child, and told her that the assessment was 10 minutes long. The bags contained (1) a book, (2) a set of toys to elicit symbolic play, and (3) another set of toys.
The videotaped observations were coded using ten 7-point coding scales that address parent, child, and dyadic behaviors. Four parenting scales are relevant to the present study: sensitivity (taking the child's perspective, promptly and appropriately responding to the child); positive regard (demonstrating love, respect, and admiration); stimulation of cognitive development (teaching, actively trying to expand the child's abilities); and intrusiveness (over-involvement and over-control) (Brady-Smith et al., 2000). All videotaped data for the national EHS study were scored at the National Center for Children and Families, Columbia University. A doctoral student trained a team of coders and was the “gold standard” for all reliability tests. Coders were racially and ethnically diverse, and were randomly assigned to videotapes. Coders achieved reliability (agreement within 1 point) to a criterion of 85% with the gold standard, after which 15% of tapes were drawn randomly from the coders’ weekly assignments and checked for inter-rater reliability. Coders’ average agreement ranged from 86% to 100% across scales (Brady-Smith, Fauth, & Brooks-Gunn, 2005). All coders were unaware of mothers’ program group status. Because ratings for sensitivity, positive regard, and cognitive stimulation scales were positively correlated (r’s = .50 - .71, p's < .05), a composite score for maternal supportiveness was created by computing the mean scores for parental sensitivity, cognitive stimulation, and positive regard (α = .82). Maternal supportiveness scores ranged from 1 to 6.33; intrusiveness scores ranged from 1 to 6 (see Table 1).
Spanking
Mothers reported if they or anyone in the household had spanked the target child in the past week (see Table 1).
Mothers’ Perceptions of Negative Interactions with her Child
Mothers’ perceptions of negative interactions with the target child came from a 6-item subscale of Abidin's Parenting Stress Checklist-SF found to have strong psychometric properties for the EHS research sample (Whiteside-Mansell, et al., 2006; see also Abidin, 1990). Mothers reported on perceptions such as feeling disliked by their child and feeling that their child rarely did things to make them feel good. Mothers responded on a 5-point scale (1 = strongly agree to 5 = strongly disagree). Responses were scored so that higher scores indicated more negative perceptions, and summed. Scores ranged from 6 to 30 (α = 0.68; see Table 1).
Results
Table 2 provides the bivariate correlations between all key variables for program and control participants. In both the program and control groups, attachment avoidance and anxiety were moderately correlated with each other and with depression. In both the program and control groups, attachment avoidance was associated with being African American, of lower education, and with a greater likelihood of living with a partner or other adult. In both the program and control groups, attachment anxiety was associated with being Latina. In the program group only, attachment anxiety was associated with less education and less family income. In the control group only, both attachment avoidance and anxiety were associated with maternal age.
Table 2.
Bivariate Correlations between Key Variable by Program Group
| Variables | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. M. Age | -- | .38*** | .09 | .14** | -.02 | .04 | -.09# | .01 | .08 | .02 | .13* | .15** | .18** | -.03 | -.02 | .02 |
| 2. M. Ed. | .27*** | -- | .14* | .07 | -.01 | .21*** | -.03 | -.29*** | .11* | -.06 | -.07 | -.09 | .21*** | -.10 | -.01 | -.20** |
| 3. Fam. Income | .04 | .17*** | -- | -.21*** | .04 | -.04 | -.08 | .15** | -.04 | -.06 | -.16** | -.07 | .03 | -.05 | -.07 | -.12# |
| 4. Fam. Structure | .24*** | .12** | -.21*** | -- | -.04 | -.01 | .17*** | -.14** | -.05 | .02 | .17*** | -.04 | .04 | .03 | -.04 | .06 |
| 5. Child Male | .07 | .03 | .002 | -.04 | -- | -.02 | .001 | .05 | -.04 | .08 | .01 | -.04 | -.01 | .13* | .11# | .01 |
| 6. M. White | -.03 | .13** | .06 | -.03 | .03 | -- | -.54*** | -.49*** | -.24*** | -.12* | -.10* | -.04 | .20** | -.17** | -.01 | -.11# |
| 7. M. Black | .01 | .04 | -.18*** | .21*** | -.12** | -.57*** | -- | -.31*** | -.15** | .19*** | .22*** | -.06 | -.20** | .18** | .14* | .14* |
| 8. M. Hispanic | .03 | -.23*** | .09 | -.14** | .09* | -.50*** | -.30*** | -- | -.14** | -.04 | -.10* | .12* | -.04 | -.01 | -.06 | -.01 |
| 9. M. Other | .003 | .05 | .04 | -.09* | .01 | -.22*** | -.14** | -.12** | -- | -.02 | -.04 | -.01 | .03 | .04 | -.12* | -.01 |
| 10. M. Depression | .01 | -.17*** | -.07 | .04 | -.13** | -.26*** | .24*** | .05 | .004 | -- | .29*** | .22*** | -.02 | -.004 | -.04 | .16** |
| 11. Attachment Avoidance | .05 | -.12** | -.06 | .14** | .001 | -.09* | .12** | .007 | -.04 | .28*** | -- | .33*** | -.03 | .02 | -.001 | .15* |
| 12. Attachment Anxiety | .06 | -.15*** | -.14** | .09* | -.05 | -.09* | -.03 | .13** | .02 | .28*** | .36*** | -- | -.04 | -.07 | -.10# | .10# |
| 13. Supportiveness (age 3) | .15** | .31*** | .17** | -.04 | -.06 | .11* | -.07 | -.08 | .03 | .02 | -.19*** | -.09 | -- | -.36*** | -.08 | -.16* |
| 14. Intrusiveness (age 3) | -.14** | -.28*** | -.15* | -.03 | -.004 | -.15** | .13* | -.01 | .14* | .14* | .10 | .04 | -.41*** | -- | .18** | .09 |
| 15. Spanked (age 3) | -.14** | -.008 | -.05 | .007 | .03 | -.02 | .18*** | -.15** | -.01 | .02 | .05 | .09 | -.01 | .04 | -- | .16** |
| 16. Perceived Negative Interactions (age 3) | .005 | -.18*** | -.08 | -.04 | .03 | -.09 | .03 | .12* | -.08 | .12* | .18*** | .22*** | -.25*** | .08 | .16** | -- |
Note. Correlations below the diagonal are for the Program group, correlations above the diagonal are for the Control group.
p < .10
p < .05
p < .01
p < .001
There were also some modest correlations between depression, attachment avoidance, attachment anxiety and the four parenting outcomes. In both the program and control groups, depression, attachment avoidance, and attachment anxiety were associated with mothers’ greater perceptions of negative interactions with her child. In the program group only, depression was also associated with greater maternal intrusiveness, and attachment avoidance was associated with less maternal supportiveness. In the control group only, attachment anxiety was marginally related to more spanking.
To examine moderated program effects, we conducted regression analyses with conventional group X moderator interaction terms, with maternal depression, attachment avoidance, and attachment anxiety mean-centered and then multiplied by the program/control group variable. For all regressions, we used MPlus software (Muthén & Muthén, 2007, version 5) with FIML estimation to accommodate missing data. For the continuously scaled outcomes of maternal supportiveness, intrusiveness, and perceived negative mother-child interactions, we conducted linear regressions. For the binary outcome of spanking, because logistic regression cannot be conducted with FIML estimation, we conducted a probit regression with FIML estimation. 1
For each outcome, we began by testing a fully specified regression model incorporating all three-way interaction terms that included the program/control group variable (program X depression X avoidance, program X depression X anxiety, and program X avoidance X anxiety), all two-way interactions, and main effects. Given numerous significant bivariate associations between several maternal socio-demographic characteristics and the independent and/or dependent variables, all regressions covaried maternal age, race/ethnicity (Black/non-Black, Hispanic/non-Hispanic, and Other/non-Other), and education; family income and structure; and child sex. In no model was any three-way interaction term statistically significant.
Following Aiken and West's (1991) step-down approach, we next dropped the non-significant three-way interaction terms and re-estimated the regression models including only the two-way interaction terms of interest (program X depression, program X avoidance, program X anxiety). These models first revealed two main effects of the program (see Table 3). Specifically, consistent with findings from the national EHS Research and Evaluation Study (Love et al., 2005), in the current sample, program children were marginally less likely to be spanked than control children. Unlike the national EHS study, in the current subsample, there were no main effects of the program on maternal supportiveness. As in the national EHS study, there were no main effects of the program on maternal intrusiveness (ACF, 2002). Surprisingly, in this sample, program mothers were more likely than control mothers to report negative interactions with their children. (This subscale of the Parenting Stress Checklist-SF was not analyzed in the national EHS study).
Table 3.
Summary of Regressions Testing Moderated EHS Program Effects on Age 3 Outcomes
| Supportiveness | Intrusiveness | Spanking | Perceived Negative Interactions | |||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β | |
| M. age | 0.02 (0.01) | 0.10* | -0.003 (0.01) | -0.02 | -0.02 (0.01) | -0.09# | 0.05 (0.03) | 0.06 |
| M. Ed. | 0.24 (0.05) | 0.21*** | -0.17 (0.04) | -0.18*** | 0.04 (0.07) | 0.03 | -0.70 (0.19) | -0.15*** |
| Fam. Income | 0.03 (0.02) | 0.06 | -0.03 (0.02) | -0.07 | -0.03 (0.03) | -0.06 | -0.13 (0.09) | -0.06 |
| Fam. Struct. (lives w/others) | -0.03 (0.08) | -0.02 | -0.02 (0.07) | -0.01 | -0.13 (0.13) | -0.06 | -0.37 (0.33) | -0.04 |
| Child male | -0.07 (0.07) | -0.04 | 0.11 (0.06) | 0.07# | 0.20 (0.11) | 0.10* | 0.21 (0.28) | 0.03 |
| M. Black | -0.33 (0.09) | -0.16*** | 0.27 (0.08) | 0.15*** | 0.34 (0.14) | 0.14* | 0.54 (0.35) | 0.06 |
| M. Hispanic | -0.18 (0.10) | -0.08# | 0.03 (0.08) | 0.02 | -0.23 (0.15) | -0.09 | 0.47 (0.39) | 0.05 |
| M. Other | -0.06 (0.16) | -0.01 | 0.42 (0.14) | 0.13** | -0.19 (0.22) | -0.04 | -0.54 (0.62) | -0.03 |
| Program | -0.01 (0.07) | -0.003 | 0.03 (0.06) | 0.02 | -0.20 (0.11) | -0.09# | 0.65 (0.28) | 0.09* |
| M. depression | 0.001 (0.01) | 0.01 | -0.002 (.004) | -0.03 | -0.01 (0.01) | -0.08 | 0.04 (0.02) | 0.11# |
| Attachment avoidance | 0.01 (0.01) | 0.05 | -0.002 (0.01) | -0.02 | 0.003 (0.01) | 0.02 | 0.03 (0.04) | 0.05 |
| Attachment anxiety | -0.02 (0.01) | -0.08 | -0.01 (0.01) | -0.04 | -0.02 (0.02) | -0.10 | 0.03 (0.05) | 0.03 |
| Program × Depression | 0.01 (0.01) | 0.09 | 0.01 (0.01) | 0.07 | 0.004 (0.01) | 0.03 | -0.03 (0.03) | -0.08 |
| Program × Avoidance | -0.03 (0.01) | -0.17** | 0.01 (0.01) | 0.06 | 0.004 (0.02) | 0.02 | 0.03 (0.05) | 0.03 |
| Program × Anxiety | 0.02 (0.02) | 0.06 | 0.001 (0.02) | 0.01 | 0.06 (0.03) | 0.18* | 0.12 (0.07) | 0.10# |
| R 2 | .13*** | .09*** | .08 | .10*** | ||||
Note. Regressions conducted using FIML estimation.
p < .10
p < .05
p < .01
p < .001
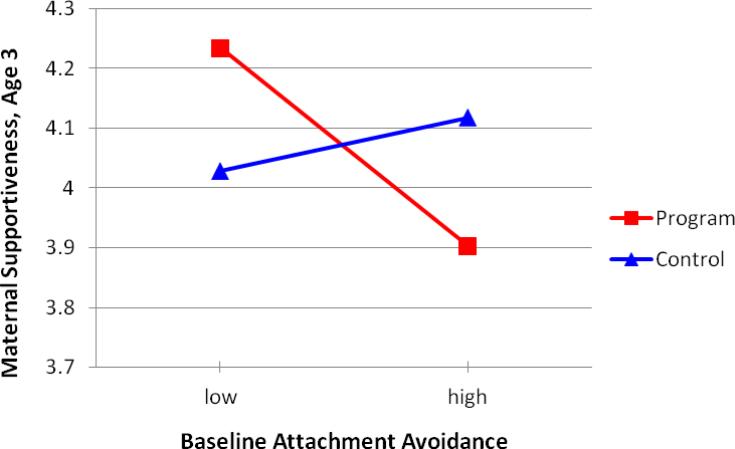
Two significant two-way interactions emerged. First, for maternal supportiveness, there was a significant interaction of the program X attachment avoidance. Following Aiken and West (1991), we plotted predicted values for program and control participants maternal supportiveness scores at 1 SD above and below the mean for attachment avoidance (see Figure 1). Follow-up tests of the simple slopes indicated that, for program mothers, higher scores for baseline attachment avoidance marginally predicted lower scores for maternal supportiveness when children were 3 years old (t [931] = -1.73, p < .10). For control mothers, baseline attachment avoidance was not related to maternal supportiveness at age 3 (t [931] = 0.78, p = .44).
Figure 1.
EHS program effects on maternal supportiveness at age 3, moderated by baseline maternal attachment avoidance.
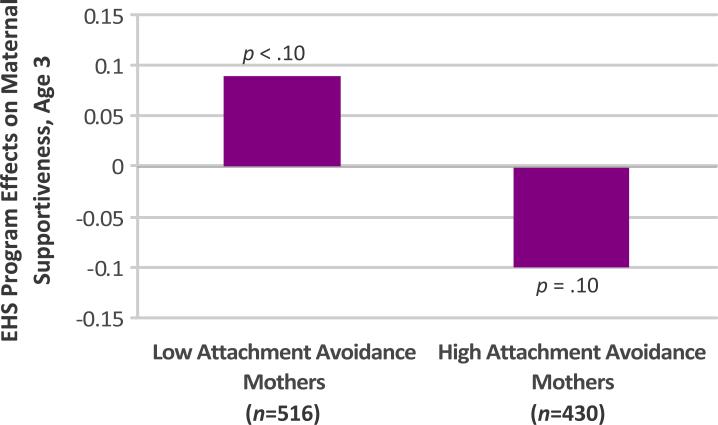
To further elucidate these findings, we re-estimated program effects on maternal supportiveness at age 3, using the same regression model (covarying maternal age, race/ethnicity, and education; family income and structure; and child sex) with the interaction terms omitted. We examined program effects on maternal supportiveness within two groups, first, a “low” attachment avoidance group, consisting of those whose scores for baseline attachment avoidance were below the mean (n = 516), and, second, a “high” attachment avoidance group, consisting of those whose scores for baseline attachment avoidance were at or above the mean (n = 430). Consistent with the full group analysis, for mothers categorized as low on baseline attachment avoidance, there was a marginally positive effect of the program on maternal supportiveness when children were 3 years old (β = 0.09, SE = 0.05, p < .10). For mothers categorized as high on baseline attachment avoidance, there was a marginally negative effect of the program on maternal supportiveness at age 3 (β = -0.10, SE = 0.06, p = .10) (see Figure 2).
Figure 2.
EHS program effects on maternal supportiveness at age 3 for mothers “low” and “high” on baseline attachment avoidance.
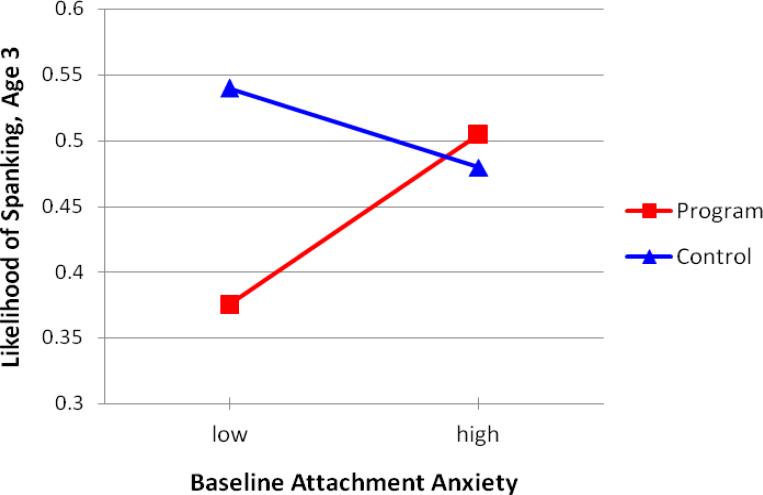
In addition, for spanking, there was a significant interaction of the program X attachment anxiety. For the purposes of plotting the interaction, we conducted a linear regression, treating spanking as a 2-point scale. We then plotted the predicted values for spanking for program and control participants at 1 SD above and below the mean for attachment anxiety (see Figure 2). Follow-up tests of the simple slopes indicated that neither was significantly different from zero (i.e., for neither program nor control mothers was baseline attachment anxiety significantly related to the likelihood of spanking, program t [931] = 1.32, p = .19, control t [931] = -1.00, p = .32).
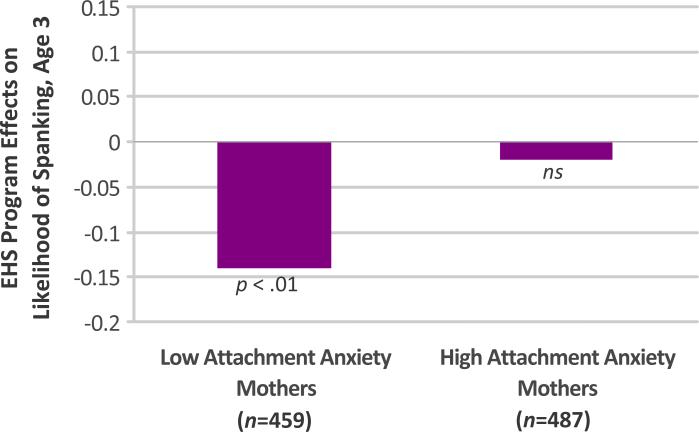
Again, to further elucidate these findings, using the prior probit regression model (covarying maternal age, race/ethnicity, and education; family income and structure; and child sex) with the interaction terms omitted, we re-estimated program effects on spanking at age 3 within two groups, a “low” attachment anxiety group, consisting of those whose scores for baseline attachment anxiety were below the mean (n = 459), and a “high” attachment anxiety group, consisting of those whose scores for baseline attachment anxiety were at or above the mean (n = 487). Consistent with the full group analysis, for mothers categorized as low on baseline attachment anxiety, the program reduced the likelihood of spanking at age 3 (β = -0.14, SE = 0.05, p < .01). For mothers categorized as high on baseline attachment anxiety, there was not a significant effect of the program on spanking at age 3 (β = -0.02, SE = 0.05, p = .77) (see Figure 4).
Figure 4.
EHS program effects on spanking at age 3 for mothers “low” and “high” on baseline attachment anxiety.
Discussion
In this study, we examined maternal depression, attachment avoidance, and attachment anxiety as moderators of EHS program effects on four parenting outcomes assessed at age 3: observed maternal supportiveness and intrusiveness, and mothers’ reports of spanking and perceptions of negative interactions with her child. We first examined bivariate correlations. In both the program and control groups, attachment avoidance and anxiety were moderately correlated with each other and with depression. These findings are consistent with those from previous studies linking self-reported attachment avoidance and anxiety to self-reported psychiatric symptoms (Fortuna & Roisman, 2008; Mikulincer & Shaver, 2007; Simpson & Rholes, 2004). In findings somewhat less consistent with those from previous studies (e.g., Edelstein et al., 2004; Wilson et al., 2007), we found few, moderate, bivariate associations between attachment avoidance and anxiety and parenting. The correlations that did emerge were expectable, however. For example, attachment avoidance predicted less maternal supportiveness. Attachment anxiety marginally predicted less spanking, perhaps reflecting tentativeness or self-absorption on the part of mothers with more attachment anxiety, which has also been related to unresolved loss on the AAI (Roisman et al., 2007; Steele, Steele, and Murphy, 2009).
We next tested all three-way interaction terms that included the program/control group variable (program X depression X avoidance, program X depression X anxiety, and program X avoidance X anxiety). No significant three-way interactions emerged. Of 12 two-way interactions tested, 2 (17%) significant interactions emerged. A rate of 17% significant findings requires caution in the interpretation of these findings. Thus, interpretations are preliminary.
Both significant interactions suggest more positive program effects for mothers with less initial attachment avoidance or attachment anxiety. First, baseline attachment avoidance moderated EHS program effects on maternal supportiveness, such that program mothers with lower baseline attachment avoidance were rated as more supportive of their 3-year-olds than program mothers with higher baseline attachment avoidance. Follow-up, within-group analyses confirmed that for mothers categorized as low on baseline attachment avoidance, there was a positive effect of the program on maternal supportiveness at age 3, whereas for mothers categorized as high on baseline attachment avoidance, there was a marginally negative effect of the program on maternal supportiveness at age 3 (p = .10).
It is consistent with what is understood about mothers who are relatively high on attachment avoidance that they would be harder to serve than less avoidant mothers, in terms of increasing supportive parenting through a broad-based early intervention program. Self-reported attachment avoidance is characterized by discomfort with interpersonal closeness, trust, depending on others (Mikulincer & Shaver, 2007). Thus, it may be that the more avoidant mothers in this study were particularly resistant to forming trusting relationships with their EHS service providers, and/or that these mothers actively disdained helping relationships. The more avoidant mothers in this study may also have been less receptive to EHS providers’ input on early parenting, which typically emphasized the importance of early attachments and of parents’ responsiveness to infants’ cues and needs (ACF, 2002). Attachment avoidance is also characterized by an emphasis on competence, achievement, and a defensively positive self-presentation (Mikulincer & Shaver, 2007). Thus, it is also possible that the more avoidant mothers in this study were over-applying the information provided by EHS staff without truly attuning to their children, resulting in less supportive behavior towards their children at age 3. Last, to the extent that EHS providers’ parenting advice directly activated avoidant mothers’ insecurities, it is also possible that mothers’ increased feelings of attachment avoidance further reduced their abilities to be emotionally supportive towards their 3-year-olds.
We also found that baseline attachment anxiety moderated program effects on spanking. Although simple slopes tests were non-significant, inspection of the pattern of findings depicted in Figure 3 suggests that program mothers with lower baseline anxiety reported a lesser likelihood of spanking than program mothers with higher baseline anxiety. Follow-up, within-group analyses confirmed that for mothers categorized as low on baseline attachment anxiety, the program reduced the likelihood of spanking at age 3, whereas for mothers categorized as high on baseline attachment anxiety, there was not a significant effect of the program on spanking at age 3.
Figure 3.
EHS program effects on spanking at age 3, moderated by baseline maternal attachment anxiety.
Self-reported attachment anxiety is characterized by fears of abandonment by significant others (Mikulincer & Shaver, 2007). Earlier we speculated that program effectiveness might be enhanced for mothers relatively high on attachment anxiety if this anxiety motivated mothers to seek services and to stay engaged with service providers. This may have been all too true for the mothers in this study. To the extent that EHS mothers were focused on their service providers as attachment figures, that is, a concern with staying close to these providers and/or pleasing them may have dominated these mothers’ experience of the program, to the exclusion of attending to their relationships with their children. The time-limited nature of the EHS program (i.e., ending at age 3) may have been especially salient for mothers relatively high on attachment anxiety. In focus groups with EHS home visitors in one site, staff reported that as services drew to a close, some mothers who had previously been highly engaged in the program became highly disengaged, as if to avoid being rejected at the time that services ended (Roggman, Cook, & Jump, 2000).
Further investigation into the quantity and quality of program participation of EHS mothers high on attachment avoidance or anxiety should help to elucidate the findings we have reported. As noted earlier, there is some evidence in the literature that adult attachment is related to participation in EHS services, showing associations between attachment security and greater program engagement (using an adult attachment questionnaire; Robinson et al., 2002) and greater program participation (using the AAI; Spieker et al., 2005). In the current sample, an examination of the program mothers receiving home-based services revealed that attachment avoidance was associated with the receipt of less intense services than were intended (n = 259, r = -.23, p < .001; Berlin & Roggman, 2009). Further inquiry into the associations among adult attachment and indices of program participation and engagement are needed. In addition, this study combined mothers receiving different types of EHS services (home, center, and mixed). Further research into adult attachment moderation of EHS program effects for different types of EHS services would be useful.
In the meantime, our findings add to the body of existing studies illustrating the importance of examining the role of adult attachment as a moderator of the effects of broad early intervention programs on parenting. Our particular findings are both consistent and inconsistent with existing studies. Our findings are consistent with those studies that have found better program participation or outcomes for more secure mothers (Heinicke et al., 2006; Moran et al., 2005; Robinson et al., 2002; Spieker et al., 2005). Our findings are inconsistent with those that have found better program participation for mothers who are depressed and/or higher on attachment avoidance or anxiety (Duggan et al., 2009; Olds et al., 2008 [for mothers with fewer “psychological resources”]; Robinson & Emde, 2004). These diverging findings may be a result of different pools of participants being targeted by different early intervention programs. For example, eligibility for Early Head Start is based principally on low family income whereas Healthy Families programs target multi-risk families, selected on the basis of their high scores on the Kempe Family Stress Checklist. If Healthy Families mothers are in fact at higher risk to begin with, it would make sense that early intervention services work differently for them than EHS mothers. Moreover, different early intervention programs provide different services (e.g., EHS services take different forms whereas Healthy Families and Nurse-Family Partnership services are exclusively home-based).
Finally, the existing studies of adult attachment as a moderator of program effects have used a range of approaches to measuring adult attachment (e.g., AAI, adult attachment questionnaire, aggregating/disaggregating the subtypes of attachment insecurity), and different outcome assessments for children of different ages, which also may account for diverging findings. As noted earlier, the AAI and adult attachment questionnaires are increasingly viewed as tapping different aspects of adult attachment (Roisman et al., 2007; Steele et al., 2009). Additional, multi-measure studies of adult attachment moderators of early intervention program effects are required.
With respect to tentative implications for program development, it may be valuable for programs to screen incoming participants’ self-reported attachment avoidance and anxiety and to use this information to inform program eligibility or at least program approach. Thus, early intervention programs might apportion resources for mothers who are high on attachment avoidance or attachment anxiety to emphasize therapeutic alliances. Likewise, services for mothers high on attachment avoidance or anxiety might emphasize stable relationships with highly sensitive, nurturing service providers, ideally those whose own defenses are not easily activated (see Fonagy, Steele, & Steele, 1995, for further discussion of this point). Mothers high on attachment avoidance appear especially difficult to reach, as evidenced by studies of avoidant adults in treatment for mental or physical problems (Ciechanowski, Katon, Russo, & Walker, 2001; Dozier, Lomax, Tyrell, & Lee, 2001; see also Green, Furrer, and McAllister, this issue, for evidence that EHS mothers higher on attachment avoidance are less responsive to naturally occurring social support than those higher on adult attachment anxiety). Not to have specially-trained providers working with these mothers may risk adverse effects, as suggested by our finding of lower maternal supportiveness among program mothers with higher baseline attachment avoidance. It may also be valuable to screen program providers on the basis of their own adult attachment security, given some evidence that providers’ attachment security also plays a role in service efficacy (Tyrell, Dozier, Teague, & Fallot, 1999). This information could in turn inform programs’ strategies for staffing and professional development. In short, as evidence accumulates about what works for whom, this evidence can inform early intervention program development to address the particular strengths and challenges vulnerable families, not only for cost-efficiency, but also so that those most in need do not get left behind.
Acknowledgments
This research was supported by NIMH K01MH70378 awarded to Lisa Berlin. The findings reported here are based on research conducted as part of the national Early Head Start Research and Evaluation Project funded by the Administration for Children and Families (ACF), U.S. Department of Health and Human Services under contract 105-95-1936 to Mathematica Policy Research, Princeton, NJ, and Columbia University's National Center for Children and Families, Teachers College, in conjunction with the Early Head Start Research Consortium, and by research conducted through grant 90-YF-0004 to Utah State University, grant 90-YF-0025 to the University of Pittsburgh, grants 90FY0009 and 90FY0017 to the University of Colorado, and grant 90-YT-0013 to the University of Washington. The research is part of the independent research these universities conducted with 6 of 17 local Early Head Start programs participating in the national Early Head Start Research and Evaluation study.
We thank Yu Bai for assistance with data analysis and Jamilah Taylor for assistance with manuscript preparation.
Footnotes
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services.
Because mothers in one of the six sites completed the adult attachment questionnaire up to six months after enrollment (as opposed to at baseline), all regression models were run with and without the data from this site. Findings were virtually identical. Thus, analyses of the data from all six sites are presented.
Contributor Information
Lisa J. Berlin, Center for Child and Family Policy Duke University
Leanne Whiteside-Mansell, University of Arkansas.
Lori A. Roggman, Utah State University
Beth L. Green, NPC Research
JoAnn Robinson, University of Connecticut-Storrs.
Susan Spieker, University of Washington.
References
- Abidin RR. Parenting Stress Index Short Form Test Manual. Pediatric Psychology Press; Charlottesville, VA: 1990. [Google Scholar]
- Administration for Children and Families . Making a difference in the lives of infants and their families: The impacts of Early Head Start. U.S. Department of Health and Human Services; Washington, DC: 2002. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- Berlin L, Roggman L. [Baseline adult attachment and Early Head Start program participation] Duke University; Durham, NC: 2009. Unpublished raw data. [Google Scholar]
- Brady-Smith C, O'Brien C, Berlin L, Ware A, Fauth J, Brooks-Gunn J. Child-parent interaction rating scales for the Three-Bag assessment: 36-month wave. Teachers College, Columbia University; New York: 2000. [Google Scholar]
- Brady-Smith C, Fauth RC, Brooks-Gunn J. Background and psychometric information for the child-parent interaction rating scales for the Three-Bag assessment: 14-, 24-, and 36-month waves. Teachers College, Columbia University; New York: 2005. [Google Scholar]
- Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. The American Journal of Psychiatry. 2001;158:29–35. doi: 10.1176/appi.ajp.158.1.29. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Dozier M. Attachment organization and treatment use for adults with serious psychopathological disorders. Development and Psychopathology. 1990;2:47–60. [Google Scholar]
- Dozier M, Lomax L, Tyrrell CL, Lee SW. The challenge of treatment for clients with dismissing states of mind. Attachment & Human Development. 2001;3:62–76. doi: 10.1080/14616730122704. [DOI] [PubMed] [Google Scholar]
- Duggan A, Berlin LJ, Cassidy J, Burrell L, Tandon D. Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at-risk mothers and infants. Journal of Consulting and Clinical Psychology. 2009;77:788–799. doi: 10.1037/a0015709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuMont K, Mitchell-Herzfeld S, Greene R, Lee E, Lowenfels A, Rodriguez M, Dorabawila V. Healthy Families New York (HFNY) randomized trial: Effects on early child abuse and neglect. Child Abuse & Neglect. 2008;32:295–315. doi: 10.1016/j.chiabu.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Edelstein RS, Alexander KW, Shaver PR, Schaaf JM, Quas JA, Lovas GS, Goodman GS. Adult attachment style and parental responsiveness during a stressful event. Attachment and Human Development. 2004;6:31–52. doi: 10.1080/146167303100001659584. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Steele M, Steele H. Attachment, the reflective self, and borderline states: The predictive specificity of the Adult Attachment Interview and pathological development. In: Goldberg S, Muir R, editors. Attachment Theory: Social, developmental and clinical perspectives. Analytic; Hillsdale, NJ: 1995. pp. 233–278. [Google Scholar]
- Fortuna K, Roisman GI. Insecurity, stress, and symptoms of psychopathology: Contrasting results from self-reports versus interviews of adult attachment. Attachment & Human Development. 2008;10:11–28. doi: 10.1080/14616730701868571. [DOI] [PubMed] [Google Scholar]
- Goodman GS, Quas JA, Batterman-Faunce JM, Riddlesberger MM, Kuhn J. Children's reactions to and memory for a stressful event: Influences of age, anatomical dolls, knowledge, and parental attachment. Applied Developmental Science. 1997;1:54–75. [Google Scholar]
- Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. American Psychological Association; Washington, DC: 2002. [Google Scholar]
- Heinicke CM, Goorsky M, Levine M, Ponce V, Ruth G, Silverman M, et al. Pre- and postnatal antecedents of a home-visiting intervention and family developmental outcome. Infant Mental Health Journal. 2006;27:91–119. doi: 10.1002/imhj.20082. [DOI] [PubMed] [Google Scholar]
- Husaini BA, Neff JA, Harrington JB, Hughes MD, Stone RH. Depression in rural communities: Validating the CES-D Scale. Journal of Community Psychology. 1980;8:20–27. [Google Scholar]
- Love JM, Kisker EE, Ross C, Raikes H, Constantine J, Boller K, et al. The effectiveness of Early Head Start for 3-year-old children and their parents: Lessons for policy and programs. Developmental Psychology. 2005;41:885–901. doi: 10.1037/0012-1649.41.6.88. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Nachshon O. Attachment styles and patterns of self-disclosure. Journal of Personality and Social Psychology. 1991;61:321–332. [Google Scholar]
- Mikulincer M, Shaver PR. Attachment in adulthood: Structure, dynamics, and change. Guilford; New York: 2007. [Google Scholar]
- Moran G, Pederson DR, Krupka A. Maternal unresolved attachment status impedes the effectiveness of interventions with adolescent mothers. Infant Mental Health Journal. 2005;26:231–249. doi: 10.1002/imhj.20045. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus users’ guide. Muthén & Muthén; Los Angeles, CA: 2007. [Google Scholar]
- National Research Council and Institute of Medicine . From neurons to neighborhoods: The science of early childhood development. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- Olds DL, Robinson J, O'Brien R, Luckey DW, Pettit LM, Henderson CR, et al. Home visiting by paraprofessionals and by nurses: A randomized, controlled trial. Pediatrics. 2002;110:486–496. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- Olds DL, Kitzman H, Hanks C, Cole R, Anson E, Sidora-Arcoleo K, et al. Effects of nurse home visiting on maternal and child functioning: Age-9 follow-up of a randomized trial. Pediatrics. 2008;120:e832–e845. doi: 10.1542/peds.2006-2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Journal of Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rholes WS, Simpson JA, Blakely BS. Adult attachment styles and mothers’ relationships with their young children. Personal Relationships. 1995;2:35–54. [Google Scholar]
- Rholes WS, Simpson JA, Campbell L, Grich J. Adult attachment and the transition to parenthood. Journal of Personality and Social Psychology. 2001;81:421–435. doi: 10.1037//0022-3514.81.3.421. [DOI] [PubMed] [Google Scholar]
- Robinson J, Emde RN. Mental health moderators of Early Head Start on parenting and child development: Maternal depression and relationship attitudes. Parenting: Science and Practice. 2004;4:73–97. [Google Scholar]
- Robinson J, Korfmacher J, Green S, Song N, Soden R, Emde RN. Predicting program use and acceptance by parents enrolled in Early Head Start. NHSA Dialog. 2002;5:311–324. [Google Scholar]
- Roggman LA, Cook GA, Jump VK. [Focus groups with Bear River Early Head Start program staff] Utah State University; Logan, UT: 2000. Unpublished raw data. [Google Scholar]
- Roisman GI, Holland A, Fortuna K, Fraley RC, Clausell E, Clarke A. The adult attachment interview and self-reports of attachment style: An empirical rapprochement. Journal of Personality and Social Psychology. 2007;92:678–697. doi: 10.1037/0022-3514.92.4.678. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Simpson JA. Influence of attachment styles on romantic relationships. Journal of Personality and Social Psychology. 1990;59:971–980. [Google Scholar]
- Simpson J, Rholes S. Anxious attachment and depressive symptoms: An interpersonal perspective. In: Rholes A, Steven W, editors. Adult attachment: Theory, research, and clinical implications. Guilford; New York: 2004. pp. 408–437. [Google Scholar]
- Simpson JA, Rholes WS, Nelligan JS. Support seeking and support giving within couples in an anxiety-provoking situation: The role of attachment styles. Journal of Personality and Social Psychology. 1992;62:434–446. [Google Scholar]
- Spieker S, Nelson D, DeKlyen M, Staerkel F. Enhancing early attachments in the context of Early Head Start: Can programs emphasizing family support improve rates of secure infant-mother attachments in low-income families? In: Berlin LJ, Ziv Y, Amaya-Jackson L, Greenberg MT, editors. Enhancing early attachments: Theory, research, intervention and policy. Guilford; New York: 2005. pp. 250–275. [Google Scholar]
- Steele H, Steele M, Murphy A. The use of the Adult Attachment Interview to measure process and change in psychotherapy. Psychotherapy Research. 2009:1–11. doi: 10.1080/10503300802609698. [DOI] [PubMed] [Google Scholar]
- Stevens J, Ammerman RT, Putnam FG, Van Ginkel JB. Depression and trauma history in first-time mothers receiving home visitation. Journal of Clinical Psychology. 2002;30:551–564. [Google Scholar]
- Tyrrell CL, Dozier M, Teague GB, Fallot RD. Effective treatment relationships for persons with serious psychiatric disorders: The importance of attachment states of mind. Journal of Consulting and Clinical Psychology. 1999;67:725–733. doi: 10.1037//0022-006x.67.5.725. [DOI] [PubMed] [Google Scholar]
- Vandell DL. A microanalysis of toddlers’ social interaction with mothers and fathers. Journal of Genetic Psychology. 1979;134:299–312. [Google Scholar]
- Whiteside-Mansell L, Ayoub C, McKelvey L, Faldowski RA, Hart RA, Shears J. Parenting stress of low-income parents of toddlers and preschoolers: Psychometric properties of a short form of the Parenting Stress Index. Parenting: Science and Practice. 2006;7:27–56. [Google Scholar]
- Widaman KF. Overton WF, Collins WA, McCartney K, Burchinal MR, Bud KL, editors. Missing data: What to do with or without them. Monographs of the Society for Research in Child Development. 2006;71(3, Serial No. 285):42–64. [Google Scholar]
- Wilson CL, Rholes WS, Simpson JA, Tran S. Labor, delivery, and early parenthood: An attachment theory perspective. Personality and Social Psychology Bulletin. 2007;33:505–518. doi: 10.1177/0146167206296952. [DOI] [PubMed] [Google Scholar]