Abstract
Objectives. We identified characteristics of Oregon children who were eligible for the Oregon Health Plan (OHP), the state's combined Medicaid–Children's Health Insurance Program (CHIP), but were not enrolled in January 2005. We also assessed whether parents’ confusion regarding their children's status affected nonenrollment.
Methods. We conducted cross-sectional analyses of linked statewide Food Stamp Program and OHP administrative databases (n = 10 175) and primary data from a statewide survey (n = 2681).
Results. More than 20% of parents with children not administratively enrolled in OHP reported that their children were enrolled. Parents of 11.3% of children who were administratively enrolled reported that they were not. Eligible but unenrolled children had higher odds of being older, having higher family incomes, and having employed and uninsured parents.
Conclusions. These findings reveal an important discrepancy between administrative data and parent-reported access to public health insurance. This discrepancy may stem from transient coverage or confusion among parents and may result in underutilization of health insurance for eligible children.
Medicaid and the Children's Health Insurance Program (CHIP) have extended health insurance coverage to millions of low-income children throughout the United States.1,2 An estimated 40% of US children are enrolled in Medicaid or CHIP for their health insurance coverage.3 This number is expected to rise as families unable to afford employer-sponsored coverage turn to public offerings.3–5 Medicaid expansion has been central to the recent national health care debate.6 Yet national statistics estimate that at least two thirds of uninsured children are eligible for public insurance but are not enrolled,2,7 even though many of these eligible but uninsured children participate in other public programs (e.g., food stamps).8,9
A lack of continuous health insurance adversely affects a child's health.10–19 Medicaid and CHIP expansions were included in almost all recent US health insurance reform proposals; thus, understanding why currently eligible children are not continuously enrolled in these programs is essential.20,21 The complexity of enrollment processes and a lack of aggressive retention efforts have sidelined many eligible children.21 These findings, coupled with proven administrative cost savings, have led many states to implement streamlined or simultaneous enrollment (also known as express lane eligibility) processes.21,22
To inform such efforts in Oregon, we identified low-income families who enrolled their children in the Food Stamp Program but not in the Oregon Health Plan (OHP; Oregon's combined Medicaid–CHIP program) and parents who understood their child's coverage status to be different from what was reported by the state. We examined characteristics that were unique to children who were eligible for public health insurance but were not enrolled. Secondarily, we described children with insurance status discrepancies and compared this subgroup with those clearly enrolled in public insurance programs.
METHODS
We identified Oregon children eligible for but not enrolled in public insurance in January 2005. Partnering with policymakers, we identified a state program with similar eligibility requirements to those of OHP: the Food Stamp Program. At the time of this study, both programs used a household income less than 185% of the federal poverty level and US citizenship as basic eligibility requirements. Thus, for the purposes of our study, Oregon children receiving food stamps were presumed to be eligible for OHP coverage. We linked the 2 administrative databases to determine which children receiving food stamps were not enrolled in OHP. From a total of 84 087 households in the Food Stamp Program database with at least 1 child aged 1 year or older (younger children had slightly different requirements), we selected a stratified, random sample of 10 175 households. We selected half the sample from families with at least 1 child aged 1 year or older enrolled in OHP and half from those with no children enrolled. We also ensured equal sampling from 6 regions across the state. This stratification procedure allowed us to oversample families without children enrolled in OHP and families from rural areas. In final weights, we accounted for differences in the probability of selection that resulted from this oversampling stratification technique.
Statewide Household Survey
In January 2005, we mailed surveys with postage-paid return envelopes to all 10 175 households; 1538 families had moved out of state or had no known forwarding address, leaving 8637 eligible potential respondents. We received 2681 completed surveys, for a response rate of approximately 31%. This response rate is consistent with rates for similar statewide surveys17,23 and national studies of Medicaid-eligible populations.24 We confirmed that our survey respondents had characteristics that were similar to those of the study population, and we used a 2-step weighting sequence.25,26 Our results were weighted back to this overall population.
In collaboration with state policymakers, we adapted items from widely accepted national data collection tools27–30 to create our survey. We asked parents to identify factors that affected their choices regarding their children's insurance and their experiences obtaining coverage and services during the previous year. We refined final survey questions after conducting cognitive pilot interviews with policymakers, health care providers, and low-income parents. Surveys were translated into Spanish and Russian (the most common non-English languages among this population), and then independently back-translated to ensure fidelity of translation. The result was a 63-item self-report survey written at a fifth-grade reading level. We used a 4-wave method (2 surveys and 2 reminder postcards). For budgetary reasons, telephone follow-up was not possible.
Variables and Analyses
We identified 9 variables that might influence children's access to insurance. We used the 2-tailed χ2 analysis to test for significant univariate associations between these variables and a child's OHP enrollment status. All variables—children's gender, age, and race/ethnicity; parents' employment and insurance status; household income; region of residence; whether children had special health care needs; and whether children had a usual source of care—were associated at the .1 level.
The main dependent variables pertained to children's current health insurance status. We initially determined from state data whether children were administratively enrolled in OHP (Table 1). We compared the sociodemographic characteristics of eligible children who were enrolled versus those who were not enrolled in OHP (according to state administrative data) through 2-tailed χ2 univariate analysis. We then ran a series of multivariate logistic regression models to identify factors independently associated with children being eligible but not administratively enrolled in OHP (vs OHP enrolled). For this analysis, we were limited to covariates available in the state administrative database (gender, age, race/ethnicity, region, and household income). This analysis incorporated all 10 175 households in the random sample, weighted back to the 84 087 Food Stamp Program households.
TABLE 1.
Food Stamp Program Families With Children Enrolled in the Oregon Health Plan and With Eligible but Not Enrolled Children, January 2005
| Demographic Covariates | Food Stamp Program Population (Weighted n = 84 087), % | Food Stamp Program Participants With Children Enrolled in OHP (Weighted n = 64 568), % | Food Stamp Program Participants With Children Eligible but Not Enrolled in OHP (Weighted n = 19 519), % | Likelihood of Child Being Eligible but Not Enrolled in OHP, AORa (95% CI) |
| Gender | ||||
| Women | 48.2 | 48.1 | 48.9 | 1.03 (0.93, 1.14) |
| Men (Ref) | 51.8 | 51.9 | 51.1 | 1.00 |
| Age,* y | ||||
| 1–4 (Ref) | 29.2 | 30.6 | 24.6 | 1.00 |
| 5–9 | 29.0 | 28.4 | 30.9 | 1.30 (1.14, 1.48) |
| 10–14 | 24.0 | 23.4 | 25.8 | 1.31 (1.14, 1.51) |
| 15–18 | 17.8 | 17.6 | 18.7 | 1.32 (1.14, 1.54) |
| Race/ethnicity* | ||||
| White, non-Hispanic (Ref) | 69.2 | 68.1 | 72.5 | 1.00 |
| Hispanic, any race | 19.9 | 20.2 | 18.9 | 1.40 (1.16, 1.70) |
| Non-White, non-Hispanic | 10.9 | 11.6 | 8.6 | 1.36 (1.10, 1.68) |
| Region* | ||||
| Northwest coastal | 4.3 | 4.3 | 4.3 | 1.31 (1.25, 1.38) |
| Portland area | 36.8 | 37.3 | 35.1 | 1.29 (1.22, 1.36) |
| Central western | 28.6 | 28.0 | 30.5 | 1.45 (1.38, 1.52) |
| Southwest coastal | 15.3 | 15.5 | 14.9 | 1.24 (1.18, 1.30) |
| North central, river gorge | 9.6 | 9.3 | 10.7 | 1.48 (1.41, 1.55) |
| Southern and eastern (Ref) | 5.5 | 5.8 | 4.6 | 1.00 |
| Household income/mo,* $ | ||||
| < 1000 (Ref) | 62.8 | 68.0 | 45.6 | 1.00 |
| 1001–1500 | 18.4 | 17.9 | 20.1 | 1.68 (1.48, 1.91) |
| 1501–2000 | 11.3 | 9.1 | 18.7 | 3.07 (2.64, 3.57) |
| > 2000 | 7.5 | 5.1 | 15.6 | 4.52 (3.75, 5.45) |
Note. AOR = adjusted odds ratio; CI = confidence interval; OHP = Oregon Health Plan (Oregon's Medicaid and Children's Health Insurance Program). Percentages were weighted back from sample population of 10 175 to reflect the entire Food Stamp Program population of 84 087. Columns sum to approximately 100%.
Multivariable analyses included gender, age, race/ethnicity, region, and household income.
P < .05 in demographic subgroup comparisons between children enrolled and not enrolled.
We next constructed a variable combining children's administrative status and parent-reported insurance status. This combined variable was derived from 4 survey questions. The first question asked, “At this time, what type of health insurance is YOUR child covered by?” Respondents were asked to check the most accurate box or boxes; 1 possible response was “my child is currently uninsured.” We validated responses through comparison with 3 additional questions that collected relevant information about children's current insurance status. We excluded from further analyses 24 of the 2681 returned surveys because of missing data or inconsistencies.
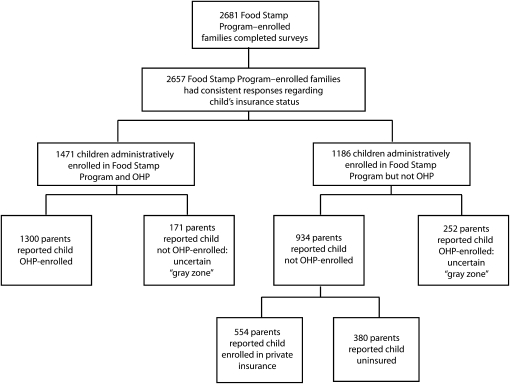
After an unanticipated finding of mismatch between parental and administrative report in more than 400 cases, we further characterized 5 subgroups, 2 of which described this uncertain “gray zone” between being insured and being uninsured (Figure 1, Table 2). The groups were
OHP stable—OHP enrolled according to both administrative data and parental report;
uncertain administrative OHP—administratively enrolled in OHP but not enrolled in OHP by parental report;
uncertain self-reported OHP—administratively not enrolled but OHP enrolled by parental report;
privately insured—private insurance by parental report, not OHP enrolled according to administrative data; and
uninsured—uninsured by parental report, not OHP enrolled according to administrative data.
FIGURE 1.
Flow diagram illustrating state and parental reports of children's public health insurance enrollment status: Oregon, January 2005.
Note. OHP = Oregon Health Plan (Oregon's Medicaid and Children's Health Insurance Program).
TABLE 2.
Factors Associated with Discrepancy Between Administrative Data and Parental Reports Regarding Children's Insurance Status: Oregon, January 2005
| “Gray Zones” |
|||
| Associated Factors | Inconsistency Between a Child's Administrative Enrollment and Parent-Reported Insurance Status, % | Likelihood That Child Was Administratively Not Enrolled in OHP but Parent-Reported Enrolleda (Unweighted n = 252; Weighted n = 3845), % or AOR (95% CI) | Likelihood That a Child Was Administratively Enrolled in OHP but Parent-Reported Not Enrolleda (Unweighted n = 171; Weighted n = 7217), % or AOR (95% CI) |
| Total | 13.2 | 4.6 | 8.6 |
| Age,* y | |||
| 1–4 (Ref) | 11.8 | 1.00 | 1.00 |
| 5–9 | 12.2 | 1.08 (0.63, 1.84) | 1.45 (0.72, 2.90) |
| 10–14 | 15.8 | 0.87 (0.49, 1.53) | 2.09 (1.07, 4.08) |
| 15–18 | 13.7 | 1.12 (0.59, 2.11) | 1.83 (0.86, 3.91) |
| Race/ethnicity,b* | |||
| White, non-Hispanic (Ref) | 12.8 | 1.00 | 1.00 |
| Hispanic, any race | 14.5 | 1.02 (0.84, 1.23) | 1.22 (0.65, 2.30) |
| Non-White, non-Hispanic | 13.8 | 1.18 (0.93, 1.48) | 0.83 (0.32, 2.21) |
| Parental employment* | |||
| Not employed (Ref) | 12.6 | 1.00 | 1.00 |
| Employed | 14.6 | 1.52 (1.03, 2.25) | 1.39 (0.86, 2.23) |
| Parental insurance status* | |||
| Insured (Ref) | 10.0 | 1.00 | 1.00 |
| Not insured | 19.4 | 2.23 (1.43, 3.48) | 2.82 (1.68, 4.69) |
| Region* | |||
| Northwest coastal | 12.6 | 0.93 (0.79, 1.10) | 0.80 (0.44, 1.45) |
| Portland area | 12.5 | 1.05 (0.86, 1.27) | 0.79 (0.41, 1.52) |
| Central western | 12.1 | 1.48 (1.20, 1.82) | 1.02 (0.53, 1.97) |
| Southwest coastal | 13.9 | 1.28 (1.07, 1.52) | 0.85 (0.45, 1.60) |
| North central, river gorge | 17.1 | 1.89 (1.60, 2.24) | 1.03 (0.53, 2.02) |
| Southern and eastern (Ref) | 15.9 | 1.00 | 1.00 |
| Household income/mo,* $ | |||
| < 1000 (Ref) | 11.7 | 1.00 | 1.00 |
| 1001–1500 | 17.1 | 1.40 (0.86, 2.27) | 1.75 (0.97, 3.14) |
| 1501–2000 | 14.3 | 2.51 (1.37, 4.58) | 1.09 (0.47, 2.53) |
| > 2000 | 14.9 | 2.92 (1.44, 5.93) | 2.09 (0.82, 5.35) |
| Child has special health care need(s)* | |||
| No (Ref) | 13.0 | 1.00 | 1.00 |
| Yes | 15.1 | 0.72 (0.41, 1.26) | 0.86 (0.41, 1.81) |
| Child has usual source of care* | |||
| Yes (Ref) | 12.3 | 1.00 | 1.00 |
| No | 22.8 | 1.87 (0.99, 3.54) | 3.22 (1.68, 6.17) |
Note. AOR = adjusted odds ratio; CI = confidence interval; OHP = Oregon Health Plan (Oregon's Medicaid and Children's Health Insurance Program). Percentages were weighted back from sample population of 10 175 to reflect the entire Food Stamp Program population of 84 087.
Versus child enrolled in OHP by both administrative data and parental report. Adjusted for age, race, parental employment, parental insurance status, region, household income, whether child had usual source of care, and child's special health care needs.
Combined variable.
P < .05 in bivariate comparisons between these sociodemographic subgroups and 1 or more of the 5 insurance enrollment groups.
To capture children eligible for public insurance but truly uninsured (Table 3), in our final analysis we attempted to freeze the frame of reference and include only children who were uninsured by all measures—children in the fifth group, whom we labeled as uninsured, with no record of administrative OHP enrollment and whose parents reported they were uninsured. We performed all statistical tests with SPSS 16.0 (SPSS Inc, Chicago, IL) with the complex samples module to account for the complex sampling design of the study and to produce accurately weighted results.
TABLE 3.
Adjusted Odds Ratios of a Child Not Enrolled in the Oregon Health Plan Being Reported by a Parent to Be Uninsured, January 2005
| Children Not Enrolled in OHPb |
||||
| Demographic Covariates | Children Enrolled in OHPa (Unweighted n = 1723), % | Privately Insuredc (Unweighted n = 554), % | Uninsuredc (Unweighted n = 380), % | Likelihood of Being Eligible for OHP but Uninsured,d AOR (95% CI) |
| Total | 81.9 | 11.0 | 7.1 | |
| Age,* y | ||||
| 1–4 (Ref) | 87.0 | 8.5 | 4.4 | 1.00 |
| 5–9 | 80.1 | 12.1 | 7.8 | 2.33 (1.41, 3.88) |
| 10–14 | 79.6 | 12.4 | 8.0 | 2.18 (1.27, 3.76) |
| 15–18 | 79.3 | 11.3 | 9.4 | 3.36 (1.80, 6.28) |
| Race/ethnicity* | ||||
| White, non-Hispanic (Ref) | 80.3 | 13.2 | 6.4 | 1.00 |
| Hispanic, any race | 84.8 | 4.7 | 10.5 | 1.40 (0.98, 2.01) |
| Non-White, non-Hispanic | 86.3 | 8.4 | 5.3 | 1.27 (0.69, 2.33) |
| Parental employment status* | ||||
| Not employed (Ref) | 88.0 | 6.5 | 5.4 | 1.00 |
| Employed | 73.3 | 17.3 | 9.4 | 1.57 (1.09, 2.28) |
| Parental insurance status* | ||||
| Insured (Ref) | 84.8 | 12.9 | 2.4 | 1.00 |
| Not insured | 74.3 | 7.9 | 17.8 | 7.71 (4.99, 11.92) |
| Region* | ||||
| Northwest coastal | 10.6 | 81.2 | 8.2 | 1.94 (1.33, 2.84) |
| Portland area | 10.1 | 82.5 | 7.4 | 1.29 (0.84, 2.00) |
| Central western | 13.5 | 80.5 | 6.0 | 2.08 (1.27, 3.43) |
| Southwest coastal | 9.4 | 82.4 | 8.2 | 1.97 (1.32, 2.94) |
| North central, river gorge | 10.7 | 80.9 | 8.4 | 2.24 (1.48, 3.39) |
| Southern and eastern (Ref) | 9.4 | 85.4 | 5.2 | 1.00 |
| Household income/mo,* $ | ||||
| < 1000 (Ref) | 89.0 | 5.3 | 5.7 | 1.00 |
| 1001–1500 | 81.5 | 10.7 | 7.7 | 1.31 (0.82, 2.09) |
| 1501–2000 | 64.1 | 25.5 | 10.4 | 1.95 (1.17, 3.26) |
| > 2000 | 52.9 | 34.8 | 12.3 | 2.62 (1.35, 5.08) |
| Child has special health care need(s)* | ||||
| No (Ref) | 80.5 | 11.9 | 7.6 | 1.00 |
| Yes | 89.0 | 6.8 | 4.2 | 0.48 (0.25, 0.93) |
| Child has usual source of care* | ||||
| Yes (Ref) | 82.9 | 12.0 | 5.1 | 1.00 |
| No | 72.0 | 5.0 | 23.0 | 3.95 (2.40, 6.49) |
Note. AOR = adjusted odds ratio; CI = confidence interval; OHP = Oregon Health Plan (Oregon's Medicaid and Children's Health Insurance Program). Percentages were weighted back from sample population of 10 175 to reflect the entire Food Stamp Program population of 84 087. Rows sum to approximately 100%.
According to administrative data, parental report, or both.
According to administrative data.
According to parental report.
Versus child being enrolled in OHP by administrative data, parental report, or both. Adjusted for age, race, parental employment, parental insurance status, region, household income, whether child had usual source of care, and child's special health care needs.
P < .05 in bivariate comparisons between these sociodemographic subgroups and ≥ 1 of the 5 insurance enrollment groups.
RESULTS
Our comparisons of the Food Stamp Program and OHP state administrative database found that approximately 23% of children enrolled in the Food Stamp Program were not enrolled in OHP (Table 1). Among Food Stamp Program enrollees, racial/ethnic minority status was associated with higher odds of being OHP eligible but not enrolled. Compared with White, non-Hispanic children, Hispanics of any race had higher odds of no enrollment (odds ratio [OR] = 1.40; 95% confidence interval [CI] = 1.16, 1.70). Non-White, non-Hispanic children also had higher odds of not being enrolled (OR = 1.36; 95% CI = 1.10, 1.68). In addition, we found an association between slightly higher household incomes and children not being enrolled, with increasing risk as monthly household income increased from $1000 to more than $2000. Children older than 4 years were also less likely than younger children to be enrolled. We found statistical differences by region, but no clear pattern.
Mismatches Between Administrative Data and Parent Reports
Figure 1 shows the distribution of state-reported and parent-reported insurance status for survey respondents. Of the 2657 children included in the final analyses, 1471 were administratively OHP enrolled (55.4%) and 1186 (44.6%) were not enrolled. When we compared parental reports with state data, we found consistency for 934 (78.8%) of the 1186 children who were OHP eligible but not administratively enrolled: 380 were not enrolled in OHP and their parents reported they had no current insurance, and 554 were not enrolled in OHP but their parents reported they had private insurance. The parents of the remaining 252 (21.2%) children presumed eligible for OHP but not administratively enrolled reported current OHP enrollment, thus revealing a mismatch. Among the 1471 children who were administratively enrolled, 1300 (88.4%) were reported by their parents to be currently enrolled in OHP, and 171 (11.6%) reported no current OHP enrollment, also a mismatch.
Although parental reports of their children's current status were consistent with state data in most cases, we observed a surprising number of discrepancies. Children most likely to have insurance status discrepancies had uninsured parents, were from families earning more than $1000 per month, had parents employed outside the home, and had no usual source of care (Table 2). In multivariate analyses, these factors remained significantly associated with children falling into an insurance gray zone. The 2 subgroups within the gray zone had slightly different characteristics; parental lack of insurance was the only predictor associated with both subgroups (Table 2).
Eligible But Unenrolled Children
For our final analysis, we attempted to describe children who were clearly uninsured, by both administrative data and parental report. We gave all other children the benefit of the doubt, combining the 1300 children with certain OHP enrollment and the 423 with mismatches between state and parental reports (total of 1723 eligible children presumed enrolled in OHP).
Compared with the 1723 children enrolled in OHP by administrative record, parental report, or both, children who appeared to be eligible for public insurance but were definitely uninsured (n = 380) were more likely to be older than 4 years, to live in a household earning more than $1500 per month, to have an uninsured parent, to have a parent working outside the home, and to have no usual source of care. Of note, children with special health care needs were less likely to be uninsured (Table 3).
DISCUSSION
Our study confirms previous reports that certain sociodemographic factors are associated with increased odds of a child being eligible for but not enrolled in public insurance.2,7,21,31,32 We further elucidated another potential reason for this phenomenon: mismatch between parental and state administrative reports of insurance status. Our findings detailing the characteristics associated with this mismatch are especially notable, because analyses of administrative data or parent-reported data alone cannot measure children in this gray zone. We did, however, confirm consistency in the factors associated with children being eligible but not enrolled, even after accounting for this gray zone group with discrepant reports of insurance status. This finding of consistency provides validation for studies that use only 1 source of data (parental or administrative) to reliably study this population.
Although this finding is reassuring for the validity of crucial future research, the large percentage of children with discrepancies in their perceived health insurance status is alarming. Multiple factors could explain these discrepancies. First, although we made every effort to recruit participants shortly after selecting our sample, survey mailing and response do not happen instantaneously. During the time between when a survey was mailed and when it was completed, a child's health insurance status might have changed. We confirmed, however, that more than 95% of surveys were returned within 30 days of initial mailing. A few families might have experienced seasonal income fluctuations or another change in circumstance such that their child no longer qualified for public coverage. In these cases, findings might represent churning, or insurance transience. In other cases it is more likely that a mismatch was attributable to parental confusion about the process of fulfilling enrollment requirements or about when their child's coverage period began or ended.22,33–35 If we assume a best-case scenario in which all state and parent-reported data were accurate, our data suggest that insurance coverage is a transient phenomenon for many low-income children. The worst-case scenario is that many families are confused about whether the state is covering their child or not.
Regardless of whether the explanation is transient coverage or a true discrepancy between the state and parents, our findings challenge the assumption that low-income children have adequate access to continuous insurance coverage simply because they meet eligibility requirements. Every year, at least 3 million children drop out of Medicaid to join the ranks of the uninsured—despite being eligible to continue their coverage.36 An increasing percentage of all uninsured children had Medicaid or CHIP during the previous year.21
Policy Implications
We report our findings in the wake of the hard-fought battle to enact the Children's Health Insurance Program Reauthorization Act (CHIPRA) of 2009 and in the midst of more extensive overall health care reform efforts, such as the recent passage of the 2010 Patient Protection and Affordable Care Act (PPACA).6,37–39 The implementation of policies outlined in the CHIPRA and the mandates of the PPACA highlight how policies can offer solutions but also challenges for eligible but unenrolled children.37,39 Regardless of how far eligibility is expanded, the complexities inherent in the system continue to erect barriers to stable enrollment. Policy solutions to improve the determination of eligibility, such as streamlining enrollment in federal programs through health information technology innovations or the elimination of mandatory uninsured waiting periods,40 do not solve the problem of confusion about a child's enrollment status. Furthermore, the insurance mandates in the PPACA could cause a parent who mistakenly believes a child to be enrolled to face a financial penalty.
The ongoing challenges faced by both states and parents in knowing which eligible children are enrolled or not enrolled and which insurance program will accept a child might intensify. For example, efforts to streamline enrollment and to automate processes to administratively enroll more children might translate into families being more confused about their children's enrollment and could actually lead to a larger percentage of children falling into a gray zone regarding their insurance status. In addition, the creation of state insurance exchanges and subsidies for families to purchase private insurance might further confuse parents, because their children's eligibility for public programs and private programs may change with even small fluctuations in family income.41
National efforts to increase coverage increasingly rely on expansions of Medicaid and CHIP; policymakers must therefore address the transient nature of public insurance, especially at the state level.6,33,39 CHIPRA 2009 includes measures to increase the enrollment of eligible but uninsured children. For example, it stipulates that states will receive a financial incentive, the Medicaid Performance Bonus, for enrolling Medicaid-eligible children above target levels.42 To qualify for this bonus, states must also enact at least 5 of 8 CHIPRA-specified policies that have been proven to boost enrollment of children: full-year coverage, no asset test, no face-to-face interview, joint application for Medicaid and CHIP, ex parte renewals, presumptive eligibility, express lane eligibility, and offerings of premium assistance.38 Policies that impede enrollment, such as waiting periods before a child can obtain CHIP coverage, must be eliminated.38
Despite these policies to ease initial enrollment, our findings suggest the need for further efforts to facilitate retention and reenrollment to avoid incurring gaps in coverage. Currently, up to half of the children enrolled in CHIP experience insurance lapses during renewal periods, which likely contribute to uncertainty about current enrollment and to the transient nature of this coverage.33 CHIPRA 2009 provisions encourage states to adopt express lane eligibility, whereby Medicaid and CHIP agencies may borrow eligibility determinations from other need-based public programs.43 CHIPRA 2009 also acknowledged the need to measure, and address, the quality of pediatric care provided.44 None of these measures, however, will ensure that a parent knows when a child is covered or not covered. Through PPACA expansion of health information technology, enrollees may have access to their records from a personal computer, their e-mail, or a cellular phone. For the time being, however, public health officials can play a crucial role in educating families about how to obtain, confirm, and maintain stable coverage, which will help to minimize this important discrepancy.
Limitations
Our sample of low-income families was drawn from Food Stamp Program data. Families enrolled in the Food Stamp Program are already connected to a system of public benefits. These families likely have higher rates of enrollment and retention in medical benefit programs and may encounter less uncertainty about how to obtain and maintain public insurance coverage than would a more general low-income population. Thus, our study likely underestimated the prevalence of discrepancies between parental report and state data in the general population. It highlighted, however, some of the characteristics associated with children who are most vulnerable to being eligible for public insurance but not enrolled.
For budgetary reasons, we administered the household survey only in English, Spanish, and Russian, and telephone follow-up was not possible. Although comparable with the response rates of similar studies of Medicaid-eligible populations, the response rate of 31% remains an important consideration. To address much of the concern about any anticipated response bias, we ensured that respondents were demographically similar to nonrespondents and used raking ratio estimation adjustments for nonresponse.
To minimize recall bias, we asked respondents to recall only events and occurrences from the past 12 months, and several questions pertained to similar topics to verify consistency in responses. In addition, the short lag period between survey mailing and return may have contributed to some of the inconsistencies between self-reported and administrative data. The cross-sectional nature of our analyses uncovered associations but precluded causal inferences. The cross-sectional study design did not allow us to determine the extent to which insurance transience played a role in the reported discrepancies.
Conclusions
Millions of uninsured children actually qualify for public coverage. Furthermore, a significant number of families whose children have health insurance may be unaware of this coverage, and other families who believe their children are covered may be mistaken. These findings reflect an important discrepancy between administrative data and parent-reported access to Medicaid and CHIP coverage. This may indicate transient coverage or confusion among parents, potentially resulting in an underutilization of health insurance coverage for children who are eligible.
Public health officials have a unique vantage point from which to witness these discrepancies and to be advocates and educators for vulnerable families. This is a historic time to advocate for policies at the national level that expand coverage to millions of uninsured people in our country and to simultaneously work at the local level to implement interventions to educate families eligible for but not enrolled in public insurance programs. If Medicaid and CHIP are to be pillars in future health insurance reforms, public health programs should continue to work toward providing stable coverage and systems that increase parental knowledge and awareness of their children's eligibility and enrollment status.
Acknowledgments
The study was funded by a grant obtained by the Office for Oregon Health Policy and Research from the US Health Resources and Services Administration, by the Agency for Healthcare Research and Quality (grants K08 HS16181 and R01 HS018569), and by the Oregon Health and Science University Department of Family Medicine.
Thank you to the Office for Oregon Health Policy and Research, the Oregon Department of Children, Adults, and Families, and the Oregon Department of Medical Assistance Programs. We are grateful for contributions from Janne Boone, Jessica Miller, James Oliver, Rebecca Ramsey, Pooya Naderi, Jeanene Smith, Bruce Goldberg, Ron Taylor, and Jeff Tharpe. A special thank you to Tina Edlund for her survey design expertise. We also acknowledge the parents who completed surveys and the anonymous peer reviewers who shared their insights to improve this article.
Human Participant Protection
This study was approved by the Oregon Health and Science University institutional review board.
References
- 1.Cunningham PJ. SCHIP making progress: increased take-up contributes to coverage gains. Health Aff (Millwood). 2003;22(4):163–172 [DOI] [PubMed] [Google Scholar]
- 2.Cuttler L, Kenney GM. State Children's Health Insurance Program and Pediatrics: background, policy challenges, and role in child health care delivery. Arch Pediatr Adolesc Med. 2007;161(7):630–633 [DOI] [PubMed] [Google Scholar]
- 3.Vistnes JP, Rhoades JA. Changes in Children's Health Insurance Status, 1996–2005: Estimates for the U.S. Civilian Noninstitutionalized Population Under Age 18. Washington, DC: Agency for Healthcare Research and Quality; 2006. Statistical Brief 141 [Google Scholar]
- 4.Vistnes JP, Schone BS. Pathways to coverage: the changing roles of public and private sources. Health Aff (Millwood). 2008;27(1):44–57 [DOI] [PubMed] [Google Scholar]
- 5.DeVoe JE, Dodoo MS, Phillips RL, Green LA. Graham Center one-pager. Who will have health insurance in 2025? Am Fam Physician. 2005;72(10):1989. [PubMed] [Google Scholar]
- 6.Rosenbaum S. Medicaid and national health care reform. N Engl J Med. 2009;361(21):2009–2012 [DOI] [PubMed] [Google Scholar]
- 7.Hudson JL, Selden TM. Children's eligibility and coverage: recent trends and a look ahead. Health Aff (Millwood). 2007;26(5):w618–w629 [DOI] [PubMed] [Google Scholar]
- 8.Horner D, Lazarus W, Morrow B. Express lane eligibility. Future Child. 2003;13(1):224–229 [PubMed] [Google Scholar]
- 9.Dorn S, Kenney GM. Automatically Enrolling Eligible Children and Families Into Medicaid and SCHIP: Opportunities, Obstacles, and Options for Federal Policymakers. New York, NY: Commonwealth Fund; 2006. Publication 931 [Google Scholar]
- 10.Selden TM, Hudson JL. Access to care and utilization among children: estimating the effects of public and private coverage. Med Care. 2006;44(5 Suppl):I-19–I-26 [DOI] [PubMed] [Google Scholar]
- 11.Szilagyi PG, Shone LP, Klein JD, Bajorska A, Dick AW. Improved health care among children with special health care needs after enrollment into the State Children's Health Insurance Program. Ambul Pediatr. 2007;7(1):10–17 [DOI] [PubMed] [Google Scholar]
- 12.Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338(8):513–519 [DOI] [PubMed] [Google Scholar]
- 13.Newacheck PW, Hughes DC, Stoddard JJ. Children's access to primary care: differences by race, income, and insurance status. Pediatrics. 1996;97(1):26–32 [PubMed] [Google Scholar]
- 14.Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005;353(4):382–391 [DOI] [PubMed] [Google Scholar]
- 15.Hadley J. Sicker and poorer—the consequences of being uninsured: a review of the research on the relationship between health insurance, medical care use, health, work, and income. Med Care Res Rev. 2003;60(2 Suppl):3S–75S [DOI] [PubMed] [Google Scholar]
- 16.Kogan MD, Alexander GR, Teitelbaum MA, Jack BW, Kotelchuck M, Pappas G. The effect of gaps in health insurance on continuity of a regular source of care among preschool-aged children in the United States. JAMA. 1995;274(18):1429–1435 [PubMed] [Google Scholar]
- 17.Stevens GD, Seid M, Halfon N. Enrolling vulnerable, uninsured but eligible children in public health insurance: association with health status and primary care access. Pediatrics. 2006;117(4):e751–e759 [DOI] [PubMed] [Google Scholar]
- 18.DeVoe JE, Graham A, Krois L, Smith J, Fairbrother GL. “Mind the gap” in children's health insurance coverage: does the length of a child's coverage gap matter? Ambul Pediatr. 2008;8(2):129–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cummings JR, Lavarreda SA, Rice T, Brown E. The effects of varying periods of uninsurance on children's access to health care. Pediatrics. 2009;123(3):e411–e418 [DOI] [PubMed] [Google Scholar]
- 20.Sommers AS, Dubay L, Blumberg LJ, Blavin FE, Czajka JL. Dynamics in Medicaid and SCHIP eligibility among children in SCHIP's early years: implications for reauthorization. Health Aff (Millwood). 2007;26(5):w598–w607 [DOI] [PubMed] [Google Scholar]
- 21.Sommers BD. Why millions of children eligible for Medicaid and SCHIP are uninsured: poor retention versus poor take-up. Health Aff (Millwood). 2007;26(5):w560–w567 [DOI] [PubMed] [Google Scholar]
- 22.Ross DC, Hill IT. Enrolling eligible children and keeping them enrolled. Future Child. 2003;13(1):81–97 [PubMed] [Google Scholar]
- 23.Wright BJ, Carlson MJ, Edlund T, DeVoe J, Gallia C, Smith J. The impact of increased cost sharing on Medicaid enrollees. Health Aff (Millwood). 2005;24(4):1106–1116 [DOI] [PubMed] [Google Scholar]
- 24.Westat Annual Report of the National CAHPS Benchmarking Database 2000. Rockville, MD: Agency for Healthcare Research and Quality; 2003 [Google Scholar]
- 25.Elliot D. Weighting for Non-Response: A Survey Researcher's Guide. London, UK: Office of Population Censuses and Surveys, Social Survey Division; 1991 [Google Scholar]
- 26.Kalton G, Kasprzyk D. The treatment of missing survey data. Surv Methodol. 1986;12(1):1–16 [Google Scholar]
- 27.Agency for Healthcare Research and Quality Medical Expenditure Panel Survey. Available at: http://www.meps.ahrq.gov/mepsweb. Accessed February 23, 2010
- 28.Community Tracking Study: Household Survey Instrument 2000–01. (Round Three). Washington, DC: Center for Studying Health System Change; 2004. Technical Publication 54 [Google Scholar]
- 29.CAHPS 2.0 Survey and Reporting Kit. Silver Spring, MD: Agency for Healthcare Research and Quality; 2002 [Google Scholar]
- 30.National Center for Health Statistics National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis.htm. Accessed August 20, 2007
- 31.Selden TM, Hudson JL, Banthin JS. Tracking changes in eligibility and coverage among children, 1996–2002. Health Aff (Millwood). 2004;23(5):39–50 [DOI] [PubMed] [Google Scholar]
- 32.Aiken KD, Freed GL, Davis MM. When insurance status is not static: insurance transitions of low-income children and implications for health and health care. Ambul Pediatr. 2004;4(3):237–243 [DOI] [PubMed] [Google Scholar]
- 33.Fairbrother GL, Emerson HP, Partridge L. How stable is Medicaid coverage for children? Health Aff (Millwood). 2007;26(2):520–528 [DOI] [PubMed] [Google Scholar]
- 34.Holahan J, Dubay L, Kenney GM. Which children are still uninsured and why. Future Child. 2003;13(1):55–79 [PubMed] [Google Scholar]
- 35.Fairbrother G, Dutton MJ, Bachrach D, Newell K-A, Boozang P, Cooper R. Costs of enrolling children in Medicaid and SCHIP. Health Aff (Millwood). 2004;23(1):237–243 [DOI] [PubMed] [Google Scholar]
- 36.Sommers BD. From Medicaid to uninsured: drop-out among children in public insurance programs. Health Serv Res. 2005;40(1):59–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaiser Commission on Medicaid and the Uninsured State Children's Health Insurance Program (CHIP): reauthorization history. Available at: http://www.kff.org/medicaid/upload/7743-02.pdf. Accessed February 23, 2009
- 38.Kaiser Commission on Medicaid and the Uninsured Children's Health Insurance Program Reauthorization Act of 2009 (CHIPRA). Available at: http://www.kff.org/medicaid/upload/7863.pdf. Accessed February 28, 2009
- 39.Iglehart JK. Medicaid expansion offers solutions, challenges. Health Aff (Millwood). 2010;29(2):230–232 [DOI] [PubMed] [Google Scholar]
- 40.Health policy brief: enrolling more kids in Medicaid and CHIP. Health Affairs. January 27, 2011. Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=39. Accessed February 7, 2011
- 41.Sommers BD, Rosenbaum S. Issues in health reform: how changes in eligibility may move millions back and forth between Medicaid and insurance exchanges. Health Aff (Millwood). 2011;30(2):228–236 [DOI] [PubMed] [Google Scholar]
- 42.Kaiser Commission on Medicaid and the Uninsured. Medicaid Performance Bonus. Available at: http://www.kff.org/medicaid/upload/7884.pdf. Accessed February 28, 2009
- 43.Kaiser Commission on Medicaid and the Uninsured. Building an express lane eligibility initiative: a roadmap of key decisions for states. Available at: http://www.kff.org/medicaid/upload/8043.pdf. Accessed February 28, 2010
- 44.Simpson LA, Fairbrother G. How health policy influences quality of care in pediatrics. Pediatr Clin North Am. 2009;56(4):1009–1021 [DOI] [PubMed] [Google Scholar]