Abstract
Objectives. We examined the health-related quality of life of residents in mountaintop mining counties of Appalachia using the 2006 national Behavioral Risk Factor Surveillance System.
Methods. Dependent variables included self-rated health; the number of poor physical, poor mental, and activity limitation days (in the past 30 days); and the Healthy Days Index. Independent variables included metropolitan status, primary care physician supply, and Behavioral Risk Factor Surveillance System behavioral and demographic variables. We compared dependent variables across 3 categories: mountaintop mining (yes or no), other coal mining (yes or no), and a referent nonmining group. We used SUDAAN MULTILOG and multiple linear regression models with post hoc least squares means to test mountaintop mining effects after adjusting for covariates.
Results. Residents of mountaintop mining counties reported significantly more days of poor physical, mental, and activity limitation and poorer self-rated health (P < .01) compared with the other county groupings. Results were generally consistent in separate analyses by gender and age.
Conclusions. Mountaintop mining areas are associated with the greatest reductions in health-related quality of life even when compared with counties with other forms of coal mining.
Measures of health-related quality of life (HRQOL) continue to be among the most crucial tools for measuring population health1 and are emerging as both outcome and predictor measures in clinical practice.2 However, their integration into larger public health practice has been limited, particularly as valid county-level outcome indicators of health3 in association with geographic environmental quality measures (e.g., air and water quality and coal mining).4 Such multilevel analyses could serve as a useful resource for assessing community health and subsequently contributing to improved decision-making.
Appalachian populations are known to suffer disproportionately higher morbidity and mortality compared with the nation as a whole.5–8 More importantly, research has found exacerbated Appalachian health disparities as a function of coal production9–13 even after controlling for covariates such as smoking, education, poverty, race, health insurance, and access to physicians. In addition, persons in central Appalachia, where coal mining is heaviest, are at greater risk for major depression and severe psychological distress compared with other areas of Appalachia or the nation.14
Because most coal mining public health research to date has relied on county-level data with limited covariates, we15 sought to address this gap by analyzing individual-level HRQOL outcomes using Behavioral Risk Factor Surveillance System (BRFSS) data with more extensive covariates. This research has determined that residents of Appalachian coal mining counties reported poorer self-rated health and HRQOL compared with residents in counties without coal mining inside and outside Appalachia. The effects were consistent for men and women and by age group even after adjusting for smoking status, alcohol use, educational attainment, marital status, race/ethnicity, body mass index (BMI; defined as weight in kilograms divided by height in meters squared), income, metropolitan residence status, and access to physicians.15 However, these studies did not differentiate between the practice of mountaintop mining (MTM) and other forms of mining.
We expanded on previous research by exploring the specific effects of MTM on HRQOL outcomes. MTM is a form of surface mining that occurs in central Appalachia. Relative to other forms of surface mining and underground mining, MTM results in large-scale impairment in surface and ground water and in local air quality and subsequently, perhaps, human health.16–20 We performed this study in 4 central Appalachian states (Kentucky, Tennessee, Virginia, and West Virginia) where MTM permits are active to determine whether residence in 1 of 3 geographic areas (MTM county, other coal mining county, and nonmining county) was related to reduced HRQOL before and after adjustment for covariates. We hypothesized that residents of counties in MTM areas in central Appalachia would report significantly reduced HRQOL and self-rated health when compared with residents of counties outside the central Appalachian MTM zone and referent nonmining counties.
METHODS
The study design is a retrospective analysis of 2006 BRFSS data on HRQOL in relation to individual- and county-level risks. Data for the current study were limited to the 4 central Appalachian states where MTM occurs. The BRFSS is a telephone-based, random, stratified survey established in 1984 to gather information on health risk behaviors, preventive health practices, and health care access primarily related to chronic disease and injury and is weighted to reflect the population of the United States.21
The 2006 BRFSS data were collected in all 50 states, the District of Columbia, Puerto Rico, and the US Virgin Islands with a median response rate of 51%.22 Because nonresponse is an indicator of potential bias, comparisons between respondents and nonrespondents on key demographics was necessary. In 2006, 60% of BRFSS respondents were women (vs 51% nationally); 80% were White non-Hispanic (vs 75%); and 6% were aged 18 to 24 years (vs 14%), 13% were aged 25 to 34 years (vs 17%), 18% were aged 35 to 44 years (vs 19%), 22% were aged 45 to 54 years (vs 19%), 18% were aged 55 to 64 years (vs 14%), and 21% were aged 65 years or older (vs 17%). The combined large sample size and overall demographic differences suggest that despite the low response rate, little nonresponse bias was experienced in 2006.
Data
The dependent variables were the Centers for Disease Control and Prevention's 4 core HRQOL items placed in the BRFSS: self-rated health, the number of poor physical and mental health days, and the number of activity limitation days (during the past 30 days).23 Item 1 focuses on self-perceived health: “In general, how would you rate your health?” Items 2 and 3 relate to recent physical and mental health symptoms and are considered mutually exclusive and are worded as such: “Now thinking about your physical (or mental) health, for how many days during the past 30 days was your physical (or mental) health not good?” Item 4 is conceptualized as a global measure of disability that explicitly incorporates both physical and mental health: “During the past 30 days, on how many days did poor physical or mental health keep you from doing your usual activities?”
Construct validity23,24 and test–retest reliability25,26 of the core HRQOL scale have been established. In addition, a Healthy Days Index was calculated by adding the number of poor physical and mental health days (unhealthy days) a respondent experienced during the past 30 days and subtracting that number from 30, with a logical maximum of 30 days. Response options to the self-rated health item were excellent, very good, good, fair, and poor. For the days questions, respondents were prompted to report an exact figure (range 0–30 days).
We took independent variables from the 2006 BRFSS survey, the county-level supplementary file provided by the Centers for Disease Control and Prevention for the 2006 survey, and Energy Information Administration data.27 Variables taken from the BRFSS were smoking, BMI, alcohol consumption, age, gender, race/ethnicity, marital status, income, education, and metropolitan residence status.
More specifically, we coded smoking as a 3-level variable: current smoker, former smoker, or not a lifetime smoker. We coded body mass index as a 3-level variable: neither overweight nor obese (BMI < 25 kg/m2), overweight (BMI = 25–<30 kg/m2), or obese (BMI ≥30 kg/m2). We coded alcohol consumption as any consumption (yes or no) in the previous 30 days. We coded age in number of years. We coded race/ethnicity as a series of dichotomous variables specifying African American, Native American, non-White Hispanic, Asian American, or White non-Hispanic. We coded marital status as a dummy variable specifying married or cohabitating versus any other status.
We coded income as an 8-level variable for annual household income: less than $10 000, $10 000 to less than $15 000, $15 000 to less than $20 000, $20 000 to less than $25 000, $25 000 to less than $35 000, $35 000 to less than $50 000, $50 000 to less than $75 000, and $75 000 or more. We coded education into 2 dummy variables specifying high school or college graduation, with less than high school used as the referent. We coded metropolitan status as a 5-level variable: (1) in the center city of a metropolitan statistical area (MSA), (2) outside the center city of an MSA but inside the county containing the center city, (3) inside a suburban county of the MSA, (4) in an MSA that has no center city, and (5) not in an MSA. The final variable we included from the BRFSS was the county-level 2005 number of office-based general practice physicians per 100 000 persons.
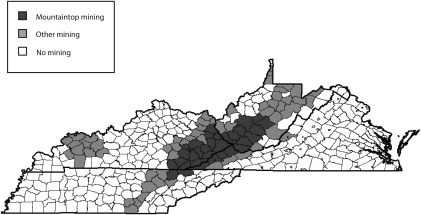
The Energy Information Administration was the source for identifying coal mining counties, which includes data for tons of coal at the county-level mined using both underground and surface techniques. For the current study, we identified a coal mining county as one with any amount of coal mining having occurred from 1994 to 2006. In practice, most counties with mining in 1 year have mining most or all years. We classified each coal mining county according to whether it was in the MTM surface mining area (yes or no). We based the MTM classification on a map of MTM areas in central Appalachia28 overlaid with coal production data from the Energy Information Administration to confirm surface mining activity. Figure 1 shows a county map of the 4-state region with the 3 mining groups identified.
FIGURE 1.
Coal mining areas in Central Appalachian states: 1994–2006.
Of the 1148 counties in the national 2006 BRFSS, 120 (10.4%) were located within the 4-state region. The 120 counties represent 29.7% of the total 404 counties in the 4 states. These counties included 19 of 32 (59.0%) MTM counties in the region, 23 of 58 (40.0%) other coal mining counties, and 78 of 321 (24.0%) nonmining counties.
Data Analysis
We made descriptive summaries of the variables followed by inferential analyses to examine HRQOL in coal mining areas. Because of the complex sampling design of the BRFSS, we analyzed models using SUDAAN version 10.0.1 (RTI International, Research Triangle Park, NC) Proc MULTILOG for the ordinal measure of self-rated health and Proc REGRESS for the continuous HRQOL days measures. For the MULTILOG models, we dichotomized self-rated health into fair or poor health and compared this with the referent excellent or very good or good health rating. Odds ratios (ORs) were found for the MULTILOG models, and regression coefficients for the regress models. We estimated all models both before and after controlling for covariates. We used the nonmining counties as the referent in comparison with the 2 mining (MTM and non-MTM) groups. We examined post hoc least squares means in the regress models.
For the continuous variables, we calculated effect size from the post hoc comparisons to determine the overall magnitude of the comparisons using the f effect size index for multiple means. Effect size values provide an indication of the magnitude of observed differences and in a practical sense show the size of differences between means. Effect sizes of 0.10, 0.25, and 0.40 indicate small, medium, and large effects, respectively, using the f calculation for multiple means.29 We used counties without mining in each of the 4 states as the referent group for the categorical county grouping variable.
RESULTS
The final BRFSS sample size for the 4 states was 10 234. Table 1 provides a summary of the demographic categorical and continuous covariate study variables overall and by the 3 county groups.
TABLE 1.
Demographic Categorical and Continuous Variables (Covariates) by County Group: Behavioral Risk Factor Surveillance System; Kentucky, Tennessee, Virginia, and West Virginia, 2006
| Characteristics | No Coal Mining | Other Coal Mining | Mountaintop Coal Mining | Total |
| Categorical variables, no. (%) | ||||
| No. counties | 78 (65.0) | 23 (19.2) | 19 (15.8) | 120 |
| Sample size | 7162 (70.0) | 1614 (15.8) | 1458 (14.2) | 10 234 |
| Women | 4440 (62.0) | 976 (60.5) | 891 (61.1) | 6307 |
| Smoking status | ||||
| Current | 1579 (22.0) | 392 (24.3) | 393 (27.0) | 2364 |
| Former | 1947 (27.1) | 457 (28.3) | 400 (27.4) | 2804 |
| Nonsmoker | 3636 (50.8) | 765 (47.4) | 665 (45.6) | 5066 |
| Alcohol use (past 30 d) | 4257 (59.4) | 1120 (69.4) | 1126 (77.2) | 6503 |
| High school education | 3974 (55.5) | 995 (61.6) | 855 (58.6) | 5824 |
| College education | 2456 (34.3) | 387 (24.0) | 296 (20.3) | 3139 |
| Married | 4096 (57.2) | 983 (60.9) | 819 (56.2) | 5898 |
| Race/ethnicity | ||||
| African American | 820 (11.5) | 26 (1.6) | 34 (2.3) | 880 |
| Asian American | 125 (1.8) | 14 (0.1) | 15 (1.0) | 154 |
| Native American | 252 (3.5) | 36 (2.2) | 50 (3.4) | 338 |
| Hispanic | 129 (1.8) | 13 (0.1) | 16 (1.1) | 158 |
| Overweighta | 2698 (37.7) | 588 (36.4) | 512 (35.1) | 3798 |
| Obeseb | 1959 (27.4) | 524 (32.5) | 499 (34.2) | 2982 |
| Continuous variables, mean (SD) | ||||
| Income categoryc | 5.6 (2.1) | 5.1 (2.2) | 4.6 (2.3) | 5.4 (2.2) |
| Age, y | 51.4 (16.0) | 52.8 (15.9) | 51.9 (15.8) | 51.7 (16.0) |
| Metropolitan status categoryd | 2.3 (1.5) | 3.3 (1.7) | 4.0 (1.6) | 2.7 (1.7) |
| Physicians per 1000 population | 29.8 (11.9) | 30.2 (15.8) | 27.2 (9.1) | 29.5 (12.3) |
Note. Percentages may not add to 100% because of rounding.
Body mass index (BMI; defined as weight in kilograms divided by height in meters squared) = 25–<30 kg/m2.
BMI ≥30 kg/m2.
Coded as an 8-level variable for annual household income: less than $10 000, $10 000 to less than $15 000, $15 000 to less than $20 000, $20 000 to less than $25 000, $25 000 to less than $35 000, $35 000 to less than $50 000, $50 000 to less than $75 000, and $75 000 or more.
Coded as a 5-level variable: (1) in the center city of a metropolitan statistical area (MSA), (2) outside the center city of an MSA but inside the county containing the center city, (3) inside a suburban county of the MSA, (4) in an MSA that has no center city; and (5) not in an MSA.
MULTILOG Regression Results
Both unadjusted and adjusted comparisons for the self-rated health variable suggest all coal mining counties have significantly reduced self-rated health. Before we added covariates to the model, residents in other mining counties had 1.30 greater odds of reporting fair or poor self-rated health (95% confidence interval [CI] = 1.15, 1.48; P ≤ .001) compared with referent non–coal mining counties while residents of MTM counties had 2.20 greater odds (95% CI = 1.95, 2.49; P ≤ .001). When we added the covariates to the model, the effects persisted only in the MTM counties (OR = 1.31; 95% CI = 1.13, 1.52; P ≤ .001) compared with residents in other mining counties (OR = 0.89; 95% CI = 0.76, 1.03).
Multiple Linear Regression Results
Tables 2 and 3 provide unadjusted and adjusted mean comparisons for the HRQOL dependent variables. Similar to the MULTILOG models, both surface and other coal mining counties have significantly reduced health ratings on all the variables before we added covariates to the model, but MTM counties reported greater HRQOL impairment (Table 2). Effect sizes for these differences range from 0.15 to 0.42, indicating modest to large effects. Specifically, the effect size was 0.15 for poor physical health days (F [1, 10 231] = 100.00; P ≤ .001), 0.21 for poor mental health days (F [3, 10 231] = 76.42; P ≤ .001), 0.18 for activity limitation days (F [1, 10 231] = 77.96; P ≤ .001), and 0.42 for the Healthy Days Index (poor physical and mental health days combined, F [1, 10 231] = 126.99; P ≤ .001).
TABLE 2.
Health Related Quality of Life by Mining Group: Behavioral Risk Factor Surveillance System; Kentucky, Tennessee, Virginia, and West Virginia; 2006
| Mountaintop Coal Mining |
Other Coal Mining |
No Coal Mining |
||||
| Variables | Unadjusted Mean (SE) | Adjusted Mean (SE) | Unadjusted Mean (SE) | Adjusted Mean (SE) | Unadjusted Mean (SE) | Adjusted Mean (SE) |
| Poor physical health (past 30 d) | 7.76 (0.30)*** | 6.06 (0.28)*** | 5.99 (0.25)*** | 4.92 (0.23) | 4.63 (0.10) | 4.91 (0.10) |
| Poor mental health (past 30 d) | 6.32 (0.27)*** | 5.12 (0.27)*** | 4.86 (0.23)*** | 4.21 (0.22) | 3.80 (0.09) | 4.00 (0.09) |
| Activity limitation (past 30 d) | 5.34 (0.26)*** | 3.97 (0.25)** | 3.73 (0.20)** | 2.89 (0.19)* | 2.95 (0.08) | 3.18 (0.08) |
| Healthy Days Index | 11.11 (0.34)*** | 9.08 (0.32)*** | 8.97 (0.30)*** | 7.79 (0.28) | 7.08 (0.12) | 7.42 (0.11) |
Note. Nonmining counties served as the referent group. A Healthy Days Index was calculated by adding the number of poor physical and mental health days (unhealthy days) a respondent experienced during the past 30 days and subtracting that number from 30, with a logical maximum of 30 days.
*P < .05; **P < .01; ***P ≤ .001.
TABLE 3.
Health Related Quality of Life by County Group, Stratified by Gender and by Age Group: Behavioral Risk Factor Surveillance System; Kentucky, Tennessee, Virginia, and West Virginia; 2006
| Mountaintop Coal Mining, Mean (SE) | Other Coal Mining, Mean (SE) | No Coal Mining, Mean (SE) | |
| Women | |||
| Poor physical health (past 30 d) | 6.24** (0.37) | 4.99 (0.30) | 5.31 (0.13) |
| Poor mental health (past 30 d) | 5.78* (0.37) | 4.75 (0.31) | 4.65 (0.12) |
| Activity limitation (past 30 d) | 3.99 (0.32) | 3.03** (0.26) | 3.44 (0.11) |
| Healthy Days Index | 9.65*** (0.43) | 8.33 (0.37) | 8.35 (0.15) |
| Men | |||
| Poor physical health (past 30 d) | 5.77* (0.43) | 4.91 (0.37) | 4.28 (0.15) |
| Poor mental health (past 30 d) | 4.05* (0.12) | 3.45 (0.30) | 2.96 (0.13) |
| Activity limitation (past 30 d) | 3.89* (0.39) | 2.72 (0.29) | 2.77 (0.13) |
| Healthy Days Index | 8.11*** (0.17) | 6.97 (0.41) | 5.94 (0.17) |
| Age < 50 y | |||
| Poor physical health (past 30 d) | 4.35** (0.36) | 2.99** (0.28) | 3.45 (0.12) |
| Poor mental health (past 30 d) | 5.46** (0.41) | 4.54 (0.34) | 4.51 (0.13) |
| Activity limitation (past 30 d) | 3.18** (0.32) | 2.06** (0.24) | 2.45 (0.10) |
| Healthy Days Index | 8.04** (0.46) | 6.52 (0.39) | 6.79 (0.15) |
| Age ≥ 50 y | |||
| Poor physical health (past 30 d) | 7.43* (0.42) | 6.53 (0.34) | 6.13 (0.15) |
| Poor mental health (past 30 d) | 4.74* (0.36) | 3.94 (0.28) | 3.59 (0.12) |
| Activity limitation (past 30 d) | 4.52 (0.35) | 3.57 (0.28) | 3.80 (0.12) |
| Healthy Days Index | 9.83*** (0.46) | 8.77 (0.38) | 7.96 (0.16) |
Note. Nonmining counties served as the referent group. A Healthy Days Index was calculated by adding the number of poor physical and mental health days (unhealthy days) a respondent experienced during the past 30 days and subtracting that number from 30, with a logical maximum of 30 days.
*P < .05; **P < .01; ***P ≤ .001.
When we added the covariates to the model, the effects of coal mining on HRQOL persisted in the MTM counties (Table 2). In addition, HRQOL impairment in other coal mining counties begin to appear more similar in HRQOL to the referent nonmining counties, which is consistent with a body of literature documenting health disparities among the Appalachian population that result from the covariates included, such as income and smoking.11,12 However, the effect sizes for these differences are not as strong, ranging in strength from 0.03 to 0.06 despite retaining their statistical significance (F [1, 10 231] = 13.92; P < .001, physical health days; F [1, 10 231] = 14.60; P < .001, mental health days; F [1, 10 231] = 8.54; P < .01, activity limitation days; and F [1, 10 231] = 22.19; P ≤ .001 Healthy Days Index).
When we repeated the models with covariates separately for men and women, we found similar findings for each gender, particularly for men and women in MTM counties for the Healthy Days Index (Table 3). In addition, when we repeated the models once again by age group (younger than 50 years or 50 years or older), the effects remained and increased with age in the MTM counties for the Healthy Days Index (Table 3). Although not shown in the table, significant similar trends were noted for greater odds of reporting fair or poor self-rated health for both genders and the 50 years old or older group in each of the mining county groups; however, the greatest odds were among residents in the MTM counties (OR = 2.04–2.50; P ≤ .001).
DISCUSSION
We further expand the literature base on the effects of coal mining on self-rated health and HRQOL15 by isolating mountaintop mining (MTM) activities and comparing them with other coal mining and nonmining areas in 4 central Appalachian states. In this individual-level health behavioral analysis using BRFSS data, self-rated health and HRQOL were significantly reduced among residents of MTM counties in the unadjusted and adjusted models. When analyzed by gender and age group, although the effects were slightly stronger for men, effects were present for women as well, and trends were similar for the MTM counties. These findings suggest the unique contributions MTM activity makes to negative health ratings among residents in counties with MTM activity compared with residents in the other county groupings and further add to a developing environmental health disparities literature base pertaining specifically to coal extraction and processing in Appalachia.10–13,15
Interestingly, in some cases, women residents in the other mining county grouping reported statistically improved HRQOL in the adjusted models. This effect was only seen in women younger than 50 years and was limited primarily by the activity limitation days measure, which used a more severe health standard than did the other questions (e.g., work loss days, bed disability days) and has been found to be a useful indicator of disability30,31 even at the county level.32 This finding is difficult to explain, but it may be that these environments, after controlling for critical variables such as income and education, characterize the finer qualities of primarily rural settings relative to the referent group. In addition, our analysis did not control for other potentially confounding variables, such as the higher rates at which women enroll in continuing education and community colleges.33 Still further, this finding may be spurious, given that women consistently report significantly reduced HRQOL, including activity limitation, compared with men in other population-based studies.34,35
Self-rated health spans past and present physical, behavioral, emotional, and cognitive aspects of health and includes cognitive aspects in the future (i.e., people may forecast a health trajectory into the future on the basis of past and present information).36 In addition, a robust body of literature has linked self-rated health to mortality.37–45 Because of this link, the Centers for Disease Control and Prevention and the World Health Organization23,46 recommend self-rated health as a measure of population health. Therefore, the increased ORs of reporting fair or poor self-rated health among MTM county residents in the adjusted models suggest a significant elevated mortality risk in these populations.
Noting inconsistencies among self-rated health among 4 large nationally representative surveys, particularly among the category of fair or poor self-rated health,47 some have questioned the use of this indicator to track population health. However, the consistent findings among the HRQOL items in this study that mirror the results found with the self-rated items suggest that the effects among residents in the MTM counties are not spurious or data artifacts. The effect sizes for the HRQOL items are small in the adjusted models, as expected, because they query respondents’ health of only the past 30 days. Yet results of the Healthy Days Index adjusted findings (Table 2) still suggest, on average, approximately 1.5 days worse reported HRQOL among residents of MTM counties compared with residents in the other coal mining counties and residents in the referent nonmining counties each month. Thus, MTM county residents experience, on average, 18 more unhealthy days per year than do the other populations. Across an average American lifetime of 78 years, that is approximately 1404 days, or almost 4 years, of additional HRQOL impairment directly associated with residence in an MTM county. To gain insight into the magnitude of these findings, when MTM and other coal mining counties were not separated in a previous study,15 there were 462 reduced HRQOL days across an average American life.
Limitations
Our study has several limitations. First, county of residence does not necessarily indicate exposure in this ecological design study. Coal mining activity may be distributed more heavily in some parts of a county than in others, and mining effects may cross county lines to affect nonmining counties. Similarly, forms of surface mining occur in the non-MTM counties, and other industry activities—such as coal preparation and transportation—that also pose environmental risks take place in both MTM and other mining areas. This fact may partially explain some of the observed small effect sizes. If only residents of communities where coal mining activity directly occurred were surveyed, the effect sizes and reduced HRQOL could be larger than are those reported in this study.
Second, only 52 counties that were located within Appalachia and where coal mining was present were available for analysis. Third, multiple statistical tests raise the possibility of a type I error, although most Appalachian mining effects were significant at P < .01 or better. Fourth, additional unmeasured confounds such as psychological stress and economic uncertainties among residents and workers in mining areas may influence HRQOL in both MTM and non-MTM environments. Fifth, the study does not include direct environmental measures of air and water quality; information, such as that from the Environmental Protection Agency's (EPA) national ambient air quality standards, exists for only a limited set of primarily urban counties. Likewise, water quality data are available nationwide only for public water systems and not for private wells and for public systems only when an established EPA standard has been exceeded. Future research will need to obtain specific environmental and health measures of these communities to fully assess the impact of coal mining on human health.
Conclusions
Results indicate that previously documented HRQOL disparities in Appalachia's coal mining areas are concentrated in MTM zones in the central part of the region. These disparities partly reflect the chronic socioeconomic weaknesses inherent in coal-dependent economies and highlight the need for efforts at economic diversification in these areas. However, significant disparities persist after control for these risks and suggest that the environmental impacts of MTM may also play a role in the health problems of the area's population. In April 2010, the EPA issued new guidance regulating MTM that recognized the environmental and community health costs imposed by this practice48; the guidance was intended to make new MTM permits much more difficult to obtain. Several weeks after this ruling, the first MTM permit application to come before the EPA was nevertheless approved, leading to concerns from environmental communities that the rules would not be interpreted or enforced as intended.49 Our results contribute to the evidence base in support of the April EPA decision.
Human Participant Protection
This study was a secondary analysis of anonymous, publically available data, and institutional review board approval was not required.
References
- 1.Thacker SB, Stroup DF, Carande-Kulis V, Marks JS, Roy K, Gerberding JL. Measuring the public's health. Public Health Rep. 2006;121(1):14–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nguyen LL, Henry AJ. Health-related quality of life: a measure of process and outcome. Vasc Med. 2010;15(3):233–234 [DOI] [PubMed] [Google Scholar]
- 3.Jia H, Moriarty DG, Kanarek N. County-level social environment determinants of health-related quality of life among US adults: a multilevel analysis. J Community Health. 2009;34(5):430–439 [DOI] [PubMed] [Google Scholar]
- 4.Thacker SB, Stroup DF, Parrish RG, Anderson HA. Surveillance in environmental public health: issues, systems, and sources. Am J Public Health. 1996;86(5):633–638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wingo PA, Tucker TC, Jamison PM, et al. Cancer in Appalachia, 2001–2003. Cancer. 2008;112(1):181–192 [DOI] [PubMed] [Google Scholar]
- 6.Caudill H. Night Comes to the Cumberlands: A Biography of a Depressed Area. Ashland, KY: Jesse Stuart Foundation; 2001 [Google Scholar]
- 7.Centers for Disease Control and Prevention Cancer death rates—Appalachia, 1994–1998. MMWR Morb Mortal Wkly Rep. 2002;51(24):527–529 [PubMed] [Google Scholar]
- 8.Halverson JA, Ma L, Harner EJ. An Analysis of Disparities in Health Status and Access to Health Care in the Appalachian Region. Washington, DC: Appalachian Regional Commission; 2004 [Google Scholar]
- 9.Hendryx M. Mortality rates in Appalachian coal mining counties: 24 years behind the nation. Environmental Justice. 2008;1(1):5–11 [Google Scholar]
- 10.Hendryx M. Mortality from heart, respiratory, and kidney disease in coal mining areas of Appalachia. Int Arch Occup Environ Health. 2009;82(2):243–249 [DOI] [PubMed] [Google Scholar]
- 11.Hendryx M, O'Donnell K, Horn K. Lung cancer mortality is elevated in coal mining areas of Appalachia. Lung Cancer. 2008;62(1):1–7 [DOI] [PubMed] [Google Scholar]
- 12.Hendryx M, Ahern M. Relations between health indicators and residential proximity to coal mining in West Virginia. Am J Public Health. 2008;98(4):669–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hendryx M, Zullig KJ. Higher coronary heart disease and heart attack morbidity in Appalachian coal mining regions. Prev Med. 2009;49(5):355–359 [DOI] [PubMed] [Google Scholar]
- 14.Zhang Z, Infante A, Meit M, English N, Dunn M, Bowers K. An Analysis of Mental Health and Substance Abuse Disparities & Access to Treatment Services in the Appalachian Region. Final Report. Washington, DC: Appalachian Regional Commission; 2008 [Google Scholar]
- 15.Zullig KJ, Hendryx M. A comparative analysis of health-related quality of life (HRQOL) for residents of U.S. counties with and without coal mining. Public Health Rep. 2010;125(4):548–555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palmer MA, Bernhardt ES, Schlesinger WH, et al. Science and regulation. Mountaintop mining consequences. Science. 2010;327(5962):148–149 [DOI] [PubMed] [Google Scholar]
- 17.Ghose MK. Generation and quantification of hazardous dusts from coal mining in the Indian context. Environ Monit Assess. 2007;130(1–3):35–45 [DOI] [PubMed] [Google Scholar]
- 18.McAuley SD, Kozar MD. Ground-Water Quality in Unmined Areas and Near Reclaimed Surface Coal Mines in the Northern and Central Appalachian Coal Regions, Pennsylvania and West Virginia. Reston, VA: US Department of the Interior, US Geological Survey; 2006 [Google Scholar]
- 19.Hitt NP, Hendryx M. Ecological integrity of streams related to human cancer mortality rates. EcoHealth. 2010;7(1):91–104 [DOI] [PubMed] [Google Scholar]
- 20.US Department of Labor, Mining Safety and Health Administration Effects of Blasting on Air Quality. Arlington, VA; 2010 [Google Scholar]
- 21.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System Operational and User's Guide, Version 3.0, December 12, 2006. Available at: ftp://ftp.cdc.gov/pub/Data/Brfss/userguide.pdf. Accessed March 23, 2009
- 22.Centers for Disease Control and Prevention BRFSS: 2006 Behavioral Risk Factor Surveillance System Summary Data. Available at: ftp://ftp.cdc.gov/pub/Data/Brfss/2006SummaryDataQualityReport.pdf. Accessed March 23, 2009
- 23.Hennessy CA, Moriarty DG, Zack MM, Scherr PA, Brackbill R. Measuring health-related quality of life for public health surveillance. Public Health Rep. 1994;109(5):665–672 [PMC free article] [PubMed] [Google Scholar]
- 24.Newschaffer CJ. Validation of the BRFSS HRQOL Measures in a Statewide Sample: Final Report. Atlanta, GA: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 1998 [Google Scholar]
- 25.Andresen EM, Catlin TK, Wyrich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57(5):339–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nanda U, Andresen EM. Performance measures of health-related quality of life and function among disabled adults [abstract]. Qual Life Res. 1998;7(7):644 [Google Scholar]
- 27.Freme F. Coal Industry Annuals and Annual Coal Reports 1994–2006. Available at: http://www.eia.doe.gov/cneaf/coal/page/acr/backissues.html. Accessed May 19, 2008
- 28.Skytruth Mountaintop removal mining, Part 1: Measuring the extent of mountaintop removal in Appalachia; 2009. Available at: http://blog.skytruth.org/2009/12/measuring-mountaintop-removal-mining-in.html. Accessed April, 21, 2010
- 29.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988 [Google Scholar]
- 30.Verbrugge LM, Merrill SS, Liu X. Measuring disability with parsimony. Disabil Rehabil. 1999;21(5–6):295–306 [DOI] [PubMed] [Google Scholar]
- 31.Clark MS, Bond MJ, Prior KN, Cotton AC. Measuring disability with parsimony: evidence for the utility of a single item. Disabil Rehabil. 2004;26(5):272–279 [DOI] [PubMed] [Google Scholar]
- 32.Jia H, Muening P, Boraski E. Comparison of small-area analysis techniques for estimating county-level outcomes. Am J Prev Med. 2004;26(5):453–460 [DOI] [PubMed] [Google Scholar]
- 33.Cohen AM, Brawer FB. Students: Diverse Backgrounds, Purposes, and Outcomes. The American Community College. San Francisco, CA: John Wiley; 2003:45–46 [Google Scholar]
- 34.Ford ES, Mokdad AH, Li C, et al. Gender differences in coronary heart disease and health-related quality of life: findings from 10 states from the 2004 Behavioral Risk Factor Surveillance System. J Womens Health (Larchmt). 2008;17(5):757–768 [DOI] [PubMed] [Google Scholar]
- 35.Zack MM, Moriarty DG, Stroup DF, Ford ES, Mokdad AH. Worsening trends in adult health-related quality of life and self-rated health—United States, 1993–2001. Public Health Rep. 2004;119(5):493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sehulster JR. Health and self: paths for exploring cognitive aspects underlying self-report of health status. : Schechter S, Proceedings of the 1993 NCHS Conference on the Cognitive Aspects of Self-Reported Health Status. Hyattsville, MD: US Department of Health and Human Services; 1994: 89–105 Working Paper, No. 10 [Google Scholar]
- 37.Ballis DS, Segall A, Chipperfield JG. Two views of self-rated general health status. Soc Sci Med. 2003;56(2):203–217 [DOI] [PubMed] [Google Scholar]
- 38.Benjamins MR, Hummer RA, Eberstein IW, Nam CB. Self-reported health and adult mortality risk: an analysis of cause-specific mortality. Soc Sci Med. 2004;59(6):1297–1306 [DOI] [PubMed] [Google Scholar]
- 39.Farkas J, Nabb S, Zaletel-Kragelj L, Cleland JG, Lainscak M. Self-rated health and mortality in patients with chronic heart failure. Eur J Heart Fail. 2009;11(5):518–524 [DOI] [PubMed] [Google Scholar]
- 40.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37 [PubMed] [Google Scholar]
- 41.Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982;72(8):800–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kaplan GA, Camacho T. Perceived health and mortality: a nine-year follow-up of the human population laboratory cohort. Am J Epidemiol. 1983;117(3):292–304 [DOI] [PubMed] [Google Scholar]
- 43.Idler EL, Kasi SV, Lemke JH. Self-evaluated health and mortality among the elderly in New Haven, Connecticut, and Iowa and Washington Counties, Iowa, 1982–1986. Am J Epidemiol. 1990;131(1):91–103 [DOI] [PubMed] [Google Scholar]
- 44.Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am J Public Health. 1990;80(4):446–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152(9):874–883 [DOI] [PubMed] [Google Scholar]
- 46.de Bruin A, Picavet JSJ, HHHealth Interview Surveys: Towards International Harmonization of Methods and Instruments. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 1996. WHO Regional Publications, European Series, No. 58 [PubMed] [Google Scholar]
- 47.Salomon JA, Nordhagen S, Oza S, Murray CJL. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol. 2009;170(3):343–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.US Environmental Protection Agency EPA Issues Comprehensive Guidance to Protect Appalachian Communities From Harmful Environmental Impacts of Mountaintop Mining. Available at: http://yosemite.epa.gov/opa/admpress.nsf/e77fdd4f5afd88a3852576b3005a604f/4145c96189a17239852576f8005867bd!OpenDocument. Accessed June, 10, 2010
- 49.Ward K. EPA gives tentative OK to Logan mine permit. Charleston Gazette. June 29, 2010 [Google Scholar]