Abstract
Objectives. We examined racial disparities in rehospitalization rates among a cohort of non-Hispanic White and Black Medicare beneficiaries admitted to skilled nursing facilities for postacute care.
Methods. We analyzed the 2008 national Nursing Home Minimum Data Set, augmented with other databases. We used multivariable logistic regression to estimate overall racial disparities in rehospitalization rates within 30 days and 90 days of nursing facility admission and the extent to which the disparities were explained by patient, facility, market, and state factors. Stratified analyses identified persistent disparities within patient subgroups, facility types, and states.
Results. The 30-day rehospitalization rates were 14.3% for White patients (n = 865 993) and 18.6% for Black patients (n = 94 651); the 90-day rehospitalization rates were 22.1% and 29.5%, respectively. Both patient and admitting facility characteristics accounted for a considerable portion of overall racial disparities, but disparities persisted after multivariable adjustments overall and in patient subgroups.
Conclusions. We found persistent racial disparities in rehospitalization among the nation's skilled nursing facility patients receiving postacute care. Targeted efforts are needed to remove these disparities.
Medicare beneficiaries admitted to skilled nursing facilities typically have undergone a recent episode of acute care in a short-term general hospital. Medicare covers their postacute services during nursing facility stays of up to 100 days, with the purpose of rehabilitation or functional recovery. Patients in these facilities have an average age of 80 years, more than one third are cognitively impaired, and approximately one half have difficulties in activities of daily living and 5 or more comorbidities.1
Transfer of these vulnerable patients back to hospitals is common,2–4 yet often considered inappropriate or potentially preventable.3,5,6 Broad consensus exists that rehospitalizations of skilled nursing facility patients disrupt service routines and patient–caregiver relationships,7 place them at risk for medical errors and iatrogenic problems,5,7 lead to greater functional and cognitive impairment,7,8 and are associated with elevated Medicare costs.6 In its recent report to Congress, the Medicare Payment Advisory Commission recommended reforms in Medicare payment rules to create financial incentives to reduce rehospitalization rates.9
Minority nursing home patients tend to receive less adequate care than do non-Hispanic Whites in the management of common chronic conditions,10–12 such as diabetes; in immunizations against influenza and pneumonia13; and in prevention and treatment of pressure ulcers.14,15 Racial minorities have also been found to be disproportionately served in nursing facilities with high concentrations of minority or Medicaid patients, poor resources, and inferior quality of care.16–19 Studies on long-term, custodial care nursing home residents found associations between minority race and higher hospitalization rates.20–23 In an analysis of long-term residents of urban nursing facilities, Gruneir et al.20 reported that 19% of White and 24% of Black residents were hospitalized and that residents in facilities with higher percentages of Blacks had a higher risk of hospitalization. No previous research, however, examined the extent of similar racial disparities among postacute skilled nursing facility residents.
We characterized racial disparities in rehospitalization rates among a national cohort of postacute care Medicare patients admitted to skilled nursing facilities. We assessed (1) whether Black patients were more likely than were White patients to be transferred back to an acute care hospital within 30 days and 90 days of nursing facility admission and (2) whether such racial disparities persisted in subgroups of patients defined by key patient characteristics, facility types, or states, in light of the varied risks of rehospitalization of nursing facility patients associated with individual demographic and health status,3,4 facility practice patterns,5–7 and state policies.2,24
METHODS
Our primary source of data was the 2008 Nursing Home Minimum Data Set (MDS), from which we created a retrospective cohort of national Medicare admissions to all federally certified skilled nursing facilities between January 1 and September 30, 2008. More than 90% of nursing facilities in the United States are federally certified.25 The MDS contained more than 350 assessment items for patient demographics; socioeconomic status; physical, cognitive, and mental health status; disease diagnoses; and routine treatments received. Assessments were performed by nursing staff at admission, at predetermined intervals following admission, and whenever patients incurred a significant change of health status. MDS assessments are considered to be accurate and valid,26,27 making the database a useful tool for a broad array of purposes, such as outcome tracking, quality-of-care evaluations, and setting regulatory and payment standards.28
We included in our cohort all MDS admission assessments during the study period that were administratively designated as Medicare prospective payment system assessments. We then linked this admission cohort to MDS discharge-tracking records by unique encrypted patient identifiers to determine the discharge status of patients within 30 days and 90 days of admission (such as discharge to an acute care hospital). The initial cohort represented 1 106 619 admissions. Patients were excluded if they had a do-not-hospitalize order at admission (n = 16 975) or died within 90 days of admission (n = 65 873, among whom 30 172 died within 30 days of admission). The final sample retained only non-Hispanic White and Black patients and excluded the 63 127 patients of other race/ethnicity (∼6% of all admissions).
We linked this patient sample to 2 external data files: the 2008 Online Survey, Certification, and Reporting file, a facility-level database maintained by the Centers for Medicare and Medicaid, which provided facility covariates, and the 2008 Area Resource File, obtained from the Health Resources and Services Administration, which contained characteristics of nursing home markets. We defined the market as the county where each facility was located.17 The final analytic sample comprised 960 644 admissions of White and Black Medicare beneficiaries to 14 798 skilled nursing facilities.
Variables
The 2 outcomes of interest were whether a patient had at least 1 discharge to an acute care hospital within 30 days and within 90 days of admission to the skilled nursing facility. The key independent variable was patient race (Black vs White). We selected patient covariates that might affect the risk of rehospitalization by considering findings of previous studies3,4,24,29 and clinical factors. These covariates were age (categorized as < 65 years, 65–74 years, 75–84 years, and ≥ 85 years), gender, education (< high school diploma, high school diploma, some college or technical school, and ≥ bachelor's degree), primary language (English vs non-English), marital status (married or not married [i.e., never married, widowed, separated, or divorced]), whether the patient was admitted to the skilled nursing facility directly from a hospital, whether the patient had a do-not-resuscitate order at admission, the number of activities of daily living (ADLs) that each patient could perform at admission, whether the patient had cognitive impairment, and a set of binary variables (1 or 0) indicating the presence (at admission) of diabetes, other endocrine disease, cardiovascular disease, musculoskeletal disease, dementia, neurologic disease other than dementia, anxiety disorder, depression, schizophrenia, bipolar disorder, pulmonary disease, sensory disease, and other diseases.
ADLs were bed mobility, transfer, dressing, eating, toilet use, personal hygiene, and bathing. We coded each ADL component into 5 categories, from 0 (independence) to 4 (total dependence), resulting in a total range of the aggregate ADL score of 0 to 28. We defined patients as cognitively impaired if they had impaired short-term memory and were dependent in daily decision-making.
Facility covariates were hospital affiliation status (hospital-based vs freestanding), profit status (for-profit, nonprofit, or government), chain affiliation (yes or no), total number of beds, percentage of Black patient admissions, and percentage of Medicaid residents among total current residents. One county-level covariate was a measure of market competition based on the Herfindahl-Hirschman Index,30 calculated as the sum of squared shares of nursing home beds for all nursing homes in the county. Market competitiveness ranged between 0 (least competition) and 1 (highest competition). Other county demand and supply variables were per capita income, percentage of population 65 years old or older, number of persons 65 years old or older per nursing home bed, number of hospital beds per 1000 population, and a designation of rural versus urban area as defined by the US Census Bureau and the Office of Management and Budget in 2008.31
Statistical Analyses
We performed bivariate analyses to determine racial differences in rehospitalization rates and in patient, facility, and county characteristics. We compared differences in means with the t test and differences in proportions with the χ2 test.
In multivariable analyses, we estimated 2 sets of logistic regression models to determine the association of Black race with the likelihoods of 30-day and 90-day rehospitalization. The dependent variable in each model was binary: the value was 1 if the patient was rehospitalized and 0 otherwise. Analyses first estimated the overall (or unadjusted) racial effect by including only race in a base model and then sequentially added to the base model patient covariates (model 1), facility characteristics (model 2), county covariates (model 3), and state dummies (model 4), to determine the extent to which the overall racial disparities in risk of rehospitalization were mediated or explained by these covariates. All models adjusted for the potential clustering of patients admitted to the same facility, through the Huber–White heteroskedasticity estimates of covariates.32
To determine whether racial disparities varied within subgroups of patients, we estimated additional sets of models, which were stratified by (1) key patient characteristics (age categories, gender, education levels, marital status, difficulties with ADLs, and cognitive impairment status) and (2) key facility attributes (hospital affiliation status, percentage of Medicaid residents [for freestanding facilities], profit status, chain affiliation, number of beds, and percentage of postacute admissions of Black patients). Because previous research showed state variations in skilled nursing facility rehospitalization rates,2,24 we also estimated models stratified by state to test racial disparities within each state.
Stratified models adjusted for all patient, facility, and county covariates and state dummies, except for the variable used for stratification. We predicted the 30-day (or 90-day) rehospitalization rates for Black and White patients within stratum for each model, and we defined racial disparity as the difference in predicted rate between Black and White patients. We performed all analyses in SAS version 9.2 (SAS Institute Inc, Cary, NC).
RESULTS
Table 1 presents descriptive statistics of White (n = 865 993) and Black (n = 94 651) skilled nursing facility patients admitted between January and September 2008. Compared with White patients, Black patients tended to be younger (75 vs 80 years on average) and less likely to have a bachelor's degree or more education (7% vs 12%), to be married (23% vs 32%), or to have a do-not-resuscitate order (10% vs 31%) than were White patients. Diagnosis patterns at admission also varied considerably between racial groups. Furthermore, Black patients were more likely to be admitted to for-profit facilities (78% vs 72%), to facilities with higher concentrations of Black patients (37% vs 7%) and to facilities with higher percentages of long-term care residents receiving Medicaid benefits (59% vs 50%) than were White patients.
TABLE 1.
Skilled Nursing Facility Patient Characteristics by Race: Nursing Home Minimum Data Set, United States, January–September 2008
| Total (n = 960 644), % or Mean (SD) | White (n = 865 993), % or Mean (SD) | Black* (n = 94 651), % or Mean (SD) | |
| Discharge to hospital | |||
| Within 30 d of admission | 14.7 | 14.3 | 18.6 |
| Within 90 d of admission | 22.8 | 22.1 | 29.5 |
| Patient characteristics at admission | |||
| Age, y | 76.7 (11.0) | 80.2 (10.6) | 74.5 (12.9) |
| Men | 34.6 | 34.1 | 39.4 |
| Education | |||
| < High school diploma | 22.9 | 21.3 | 36.9 |
| High school diploma | 44.9 | 45.6 | 38.9 |
| Some college/technical school | 18.1 | 18.6 | 13.9 |
| ≥ Bachelor's degree | 11.9 | 12.4 | 6.9 |
| Missing | 2.2 | 2.1 | 3.4 |
| English as primary language | 98.5 | 98.5 | 98.7 |
| Married | 31.4 | 32.2 | 23.2 |
| Admitted from hospital | 90.8 | 90.8 | 91.0 |
| Had do-not-resuscitate order | 29.1 | 31.1 | 10.4 |
| Activities of daily living at admissiona | 16.7 (5.3) | 16.6 (5.2) | 17.6 (6.2) |
| Cognitive impairment | 40.6 | 40.1 | 45.4 |
| Disease diagnosis at admission | |||
| Diabetes | 33.0 | 31.3 | 47.8 |
| Other endocrine disease | 20.2 | 21.4 | 9.7 |
| Cardiovascular disease | 86.3 | 86.0 | 89.0 |
| Musculoskeletal disease | 45.7 | 46.9 | 34.7 |
| Dementia | 24.2 | 24.0 | 26.1 |
| Neurologic disease other than dementia | 25.0 | 24.0 | 33.8 |
| Anxiety disorder | 14.5 | 15.3 | 7.2 |
| Depression | 30.3 | 31.4 | 19.6 |
| Bipolar disorder | 1.8 | 1.9 | 1.5 |
| Schizophrenia | 1.4 | 1.2 | 2.9 |
| Pulmonary disease | 24.3 | 24.8 | 19.7 |
| Sensory disease | 11.0 | 11.2 | 9.7 |
| Other | 59.5 | 59.6 | 58.7 |
| Facility characteristics | |||
| Hospital-based | 7.5 | 7.4 | 8.4 |
| Profit status | |||
| For-profit | 72.8 | 72.1 | 78.2 |
| Nonprofit | 27.3 | 27.9 | 21.8 |
| Government | 3.2 | 3.2 | 2.5 |
| Chain affiliated | 57.9 | 57.6 | 60.6 |
| Beds, no. | 133.8 (77.4) | 130.9 (75.5) | 151.2 (91.4) |
| Admissions of Black patients for postacute care, % | 9.9 (16.3) | 6.9 (11.2) | 37.0 (27.4) |
| Medicaid residents, % | 50.5 (24.2) | 49.6 (24.0) | 58.9 (24.5) |
| County characteristics | |||
| Competitionb | 0.8 (0.2) | 0.8 (0.2) | 0.9 (0.1) |
| Per capita income, $1000 | 37.0 (10.7) | 36.9 (10.6) | 37.9 (11.6) |
| Persons aged ≥ 65 y, % | 13.5 (3.7) | 13.6 (3.8) | 12.4 (3.0) |
| Persons aged ≥ 65 y/nursing home bed | 25.4 (12.3) | 25.5 (12.5) | 24.7 (10.0) |
| Hospital beds/1000 population | 3.5 (2.5) | 3.4 (2.4) | 4.1 (2.9) |
| Rural | 18.3 | 19.1 | 11.6 |
Seven types of activities of daily living were coded 0 (independence) to 4 (total dependence) for a score of 0 to 28.
According to Herfindahl-Hirschman Index, calculated as the sum of squared shares of nursing home beds for all nursing homes in the county. Market competitiveness scores ranged from 0 (least competition) to 1 (highest competition).
*P < .001 for all comparisons between White and Black patients derived from χ2 test (categorical variables) or t test (continuous variables), except comparison for whether patients were admitted from a hospital (P = .022).
The unadjusted rates of rehospitalization were 14.3% for White patients and 18.6% for Black patients within 30 days of skilled nursing facility admission and 22.1% and 29.5%, respectively, within 90 days of admission (Table 1). These differential rates indicated an overall 40% increased odds of 30-day rehospitalization (Table 2; in the base model, odds ratio [OR] = 1.37; 95% confidence interval [CI] = 1.35, 1.40; P < .001) and an overall 50% increased odds of 90-day rehospitalization (OR = 1.48; 95% CI 1.46, 1.50; P < .001) associated with Black race.
TABLE 2.
Racial Disparities in Rehospitalization After Admission to a Skilled Nursing Facility: Nursing Home Minimum Data Set, United States, January–September 2008
| Rehospitalization |
||
| Effect of Race (Black vs White) | Within 30 Days, OR (95% CI) | Within 90 Days, OR (95% CI) |
| Base modela no covariates | 1.37* (1.35, 1.40) | 1.48* (1.46, 1.50) |
| Model 1b | 1.18* (1.16, 1.20) | 1.25* (1.23, 1.27) |
| Model 2c | 1.06* (1.04, 1.08) | 1.09* (1.06, 1.11) |
| Model 3d | 1.06* (1.04, 1.09) | 1.09* (1.07, 1.11) |
| Model 4e | 1.06* (1.04, 1.09) | 1.09* (1.07, 1.11) |
Note. CI = confidence interval; OR = odds ratio.
No covariates.
Patient covariates.
Patient and facility covariates.
Patient, facility, and county covariates.
Patient, facility, and county covariates, plus state dummies.
*P < .001.
The overall racial disparity attenuated after sequential adjustment for patient and nursing home covariates (Table 2). ORs were reduced to 1.18 for 30-day rehospitalization and 1.25 for 90-day rehospitalization when we adjusted for patient covariates (model 1), and to 1.06 for 30-day rehospitalization and 1.09 for 90-day rehospitalization when we adjusted for both patient and facility covariates (model 2). The ORs for Black rehospitalization were not further reduced and remained statistically significant (P < .001) when we also controlled for county and state covariates, suggesting that persistent racial effects on rehospitalization were independent of the patient, facility, county, and state factors considered in the analyses.
Table 3 presents the predicted hospital admission rates for Black and White patients according to stratified models. For both White and Black patients, younger age, male gender, lower education attainment, and higher physical or cognitive impairment tended to be associated with increased rehospitalization rates. In addition, patients admitted to freestanding (rather than hospital-based) facilities, to facilities with higher concentrations of Medicaid or Black patients, and to larger or for-profit facilities had elevated rehospitalization rates. These results were generally consistent with those of previous studies.3,4,24,29,30
TABLE 3.
Predicted Rehospitalization Rates After Admission to a Skilled Nursing Facility Among Black and White Patients, Overall and Stratified by Key Patient and Facility Characteristics: Nursing Home Minimum Data Set, United States, January–September 2008
| 30-Day Rehospitalization Rate |
90-Day Rehospitalization Rate |
|||||
| Stratification Variables | White, % | Black, % | Disparity,a % (95% CI) | White, % | Black, % | Disparity,a % (95% CI) |
| No stratification | 14.3 | 18.6 | 4.3 (4.3, 4.4) | 22.1 | 29.5 | 7.5 (7.4, 7.6) |
| Patient characteristics | ||||||
| Age, y | ||||||
| < 65 | 14.9 | 19.1 | 4.3 (4.1, 4.4) | 23.0 | 29.5 | 6.5 (6.2, 6.8) |
| 65–74 | 14.6 | 19.0 | 4.4 (4.2, 4.5) | 22.0 | 29.3 | 7.3 (7.1, 7.5) |
| 75–84 | 14.3 | 18.2 | 3.9 (3.7, 4.0) | 21.8 | 29.0 | 7.2 (7.0, 7.4) |
| ≥ 85 | 14.0 | 18.4 | 4.4 (4.3, 4.5) | 22.2 | 30.6 | 8.5 (8.3, 8.6) |
| Gender | ||||||
| Women | 12.9 | 17.5 | 4.6 (4.5, 4.7) | 20.2 | 27.9 | 7.7 (7.5, 7.8) |
| Men | 16.9 | 20.3 | 3.4 (3.3, 3.6) | 25.6 | 32.0 | 6.5 (6.3, 6.6) |
| Education | ||||||
| < High school diploma | 15.0 | 18.5 | 3.6 (3.5, 3.7) | 24.0 | 30.0 | 6.0 (5.8, 6.2) |
| High school diploma | 14.4 | 18.8 | 4.3 (4.2, 4.5) | 22.2 | 29.6 | 7.4 (7.2, 7.5) |
| Some college/technical school | 13.3 | 17.6 | 4.3 (4.2, 4.5) | 20.4 | 27.5 | 7.2 (6.9, 7.4) |
| ≥ Bachelor's degree | 13.1 | 16.6 | 3.4 (3.2, 3.7) | 20.0 | 26.0 | 6.0 (5.6, 6.4) |
| Marital status | ||||||
| Married | 15.4 | 19.4 | 4.0 (3.8, 4.1) | 22.9 | 29.7 | 6.9 (6.6, 7.1) |
| Not married | 13.7 | 18.3 | 4.6 (4.6, 4.7) | 21.7 | 29.5 | 7.8 (7.7, 7.9) |
| Activities of daily living status at admissionb | ||||||
| 0–7 | 8.4 | 11.6 | 3.2 (3.0, 3.3) | 12.8 | 17.9 | 5.1 (4.9, 5.4) |
| 8–14 | 10.3 | 12.5 | 2.3 (2.2, 2.3) | 15.4 | 19.2 | 3.8 (3.7, 4.0) |
| 15–21 | 14.6 | 17.3 | 2.7 (2.7, 2.8) | 22.7 | 27.6 | 4.9 (4.8, 5.0) |
| 22–28 | 23.3 | 28.2 | 4.9 (4.7, 5.0) | 36.5 | 45.2 | 8.7 (8.5, 8.9) |
| Cognitive impairment | ||||||
| No | 13.0 | 16.5 | 3.4 (3.4, 3.5) | 19.5 | 25.3 | 5.8 (5.7, 5.9) |
| Yes | 16.1 | 21.2 | 5.1 (4.9, 5.2) | 25.9 | 34.6 | 8.7 (8.6, 8.9) |
| Facility characteristics | ||||||
| Hospital-based | 8.6 | 10.3 | 1.7 (1.5, 1.8) | 11.6 | 14.6 | 3.0 (2.8, 3.3) |
| Freestanding, % of Medicaid residents | ||||||
| < 25 | 12.7 | 16.4 | 3.7 (3.4, 3.9) | 18.5 | 24.0 | 5.5 (5.1, 5.8) |
| 25–49 | 13.8 | 17.0 | 3.1 (3.0, 3.3) | 20.9 | 25.7 | 4.8 (4.6, 5.0) |
| 50–74 | 15.2 | 19.1 | 3.9 (3.8, 4.0) | 24.1 | 30.7 | 6.6 (6.4, 6.7) |
| ≥ 75 | 16.4 | 21.6 | 5.1 (5.0, 5.3) | 26.9 | 35.3 | 8.4 (8.2, 8.7) |
| Profit status | ||||||
| For-profit | 15.0 | 19.7 | 4.7 (4.6, 4.8) | 23.5 | 31.4 | 7.9 (7.8, 8.0) |
| Nonprofit | 12.6 | 15.1 | 2.5 (2.4, 2.7) | 18.8 | 23.5 | 4.8 (4.6, 5.0) |
| Government | 12.5 | 15.4 | 3.0 (2.5, 3.4) | 19.8 | 24.5 | 4.7 (4.0, 5.4) |
| Chain affiliation | ||||||
| Yes | 14.6 | 18.8 | 4.2 (4.1, 4.3) | 22.7 | 29.8 | 7.1 (6.9, 7.2) |
| No | 13.7 | 18.3 | 4.5 (4.4, 4.6) | 21.1 | 29.1 | 8.0 (7.8, 8.1) |
| Beds, no. | ||||||
| < 50 | 9.5 | 9.5 | −0.1 (-0.2, 0.1) | 13.2 | 12.7 | −0.6 (−0.8, −0.3) |
| 50–99 | 14.1 | 18.4 | 4.3 (4.1, 4.4) | 22.0 | 29.8 | 7.8 (7.6, 8.0) |
| 100–149 | 14.9 | 19.0 | 4.1 (4.0, 4.2) | 23.1 | 30.1 | 7.0 (6.9, 7.2) |
| ≥ 150 | 14.9 | 19.8 | 4.9 (4.7, 5.0) | 23.3 | 31.6 | 8.3 (8.1, 8.5) |
| Admissions of Black patients for postacute care, % | ||||||
| < 5 | 14.2 | 16.1 | 2.0 (1.8, 2.2) | 21.6 | 24.8 | 3.2 (2.9, 3.5) |
| 5–14 | 14.9 | 16.7 | 1.8 (1.7, 1.9) | 23.2 | 26.4 | 3.3 (3.1, 3.5) |
| 15–29 | 15.4 | 18.1 | 2.6 (2.5, 2.8) | 24.4 | 28.3 | 3.9 (3.7, 4.2) |
| ≥ 30 | 17.0 | 19.9 | 2.9 (2.7, 3.0) | 27.1 | 31.9 | 4.9 (4.7, 5.1) |
Note. CI = confidence interval. Predicted rates were based on logistic regression models that controlled for patient, facility, county, and state covariates except for the variable used for stratification.
Black−White.
Seven types of activities of daily living were coded 0 (independence) to 4 (total dependence) for a score of 0 to 28.
Despite these patient and facility variations in risk of rehospitalization, Black patients had higher hospital admission rates than did White patients in almost all stratified analyses. This racial disparity was particularly pronounced within several subgroups, such as patients with the most difficulties in ADLs (racial difference = 4.9% for 30-day rehospitalization and 8.7% for 90-day rehospitalization) or with cognitive impairment (racial difference = 5.1% and 8.7%, respectively). The disparity was also more evident in freestanding facilities, facilities caring for more Medicaid residents, for-profit facilities, and facilities with more beds.
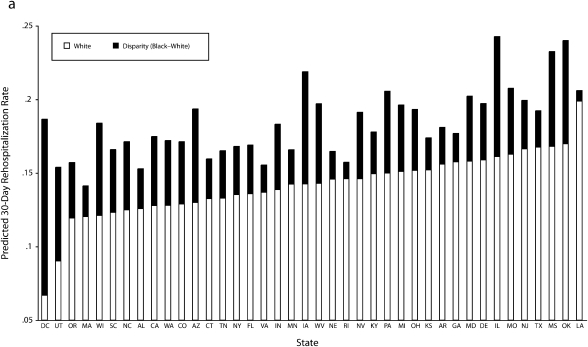
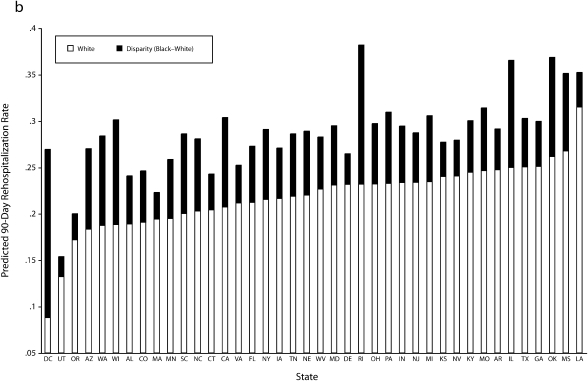
The final stratified analyses by state found substantial interstate variation in rehospitalization rates (Figure 1). For White patients, the rate ranged from 7% in Washington, DC, to 20% in Louisiana within 30 days of admission, and from 9% in Washington, DC, to 31% in Louisiana within 90 days of admission. Rates for Black patients also differed by state but were higher than for Whites in all the states we examined, and the racial disparities we observed were greater in some areas (such as Washington, DC, and Illinois) than in others.
FIGURE 1.
Rehospitalization rates for Black and White skilled nursing facility patients by state at (a) 30 and (b) 90 days: Nursing Home Minimum Data Set, United States, January–September 2008.
Note. States are sorted by rate for White patients, which is the bottom part of the histogram; the top part of each histogram highlights disparity for Black patients. States (Alaska, Hawaii, Idaho, Maine, Montana, North Dakota, New Hampshire, New Mexico, South Dakota, Vermont, and Wyoming) with fewer than 50 Black admissions were not included in the stratified analyses.
DISCUSSION
Our analyses revealed that among a cohort of White and Black Medicare patients admitted to US skilled nursing facilities in 2008, Black patients had a 40% higher risk of being rehospitalized within 30 days of admission and a 50% increased risk of being rehospitalized within 90 days of admission. Variations in patient characteristics (demographic, socioeconomic, and clinical) and the type of admitting facilities may explain a considerable portion of this racial disparity, but the disparity persisted after adjustment for these and other factors and persisted within subgroups of patient and facility types. Finally, despite substantial interstate differences in predicted rehospitalization rates, Black patients tended to have higher rates than did Whites in all states and the District of Columbia.
Although racial disparities in hospitalization of long-term care nursing home residents have been suggested in previous research,20–23 ours is the first study, to our knowledge, that comprehensively evaluated racial disparities in skilled nursing facility rehospitalizations. At the micro level, the decision to send a nursing facility patient to a hospital may be affected by a variety of factors, which include the acuity and severity of disease, family and patient preferences, and facility-related factors such as practice routines or ability to respond to emergency situations.4,33–35 The persistent racial disparities in the likelihood of hospital readmission may be a manifestation of the underlying differences in these varied factors between racial groups.
The existing literature suggests substantial racial segregation in nursing home care: racial minority patients tend to reside in facilities that have higher percentages of minority residents, are disadvantaged financially (e.g., are heavily reliant on Medicaid reimbursement), and provide poorer-quality care.16–19 Our descriptive analyses confirmed these findings for skilled nursing facility admissions (Table 1). Previous research also established that improved staffing levels of physician assistants and geriatric nurse practitioners in skilled nursing facilities, as well as on-site availability of technological resources such as intravenous therapy or x-rays, effectively reduce their rehospitalization rates.33–35 Therefore, the resource-poor facilities that house the majority of Black patients may be more likely to send their patients out to hospitals because they are less able to provide on-site access to medical staff and technological resources in emergencies, which may contribute to the racial disparities we observed.
Our stratified analyses (Table 3) found that facilities that had more Medicaid beneficiaries or more Black patients admitted or were profit driven (and therefore had less incentive to invest in clinical care30) also had higher rehospitalization rates for both White and Black patients. In addition, compared with freestanding facilities, hospital-based skilled nursing facilities may be better staffed by professional nurses36 and have enhanced access to varied clinical resources and thus may experience lower rehospitalization rates.3,29 These results provide further evidence that the practice patterns in resource-poor facilities, which serve a disproportionately high number of Black patients, contribute to the racial disparity in hospital readmission rate.
Even within similar types of facilities, however, Black patients had a consistently higher risk of hospital admission than did White patients, and such racial disparities were greater in resource-poor facilities. This risk of hospital admission might be explained by the fact that even in facilities with relatively similar practices, Black patients tend to desire more aggressive and life-sustaining medical treatments than do White patients,23,37 which may stem from distrust of the medical care system among minority patients and their desire not to lose access to the health care system. Another possible reason is that compared with White patients, minority patients (and their families) tend to have poorer communication with physicians and other nursing home staff,38 which may impede provider response to patients' altered health conditions, complicate diagnosis and treatment, and thus exacerbate the risk of hospital admission. Taken together, patient and facility factors may explain much of the racial disparity, as suggested by the analyses shown in Table 2.
Although we are unsure why states varied substantially in rehospitalization rates, recent studies suggest that systematic differences in state or local practice norms2 and in state nursing home regulations24 play a role. Our study contributes to the literature by showing that in addition to the overall variation in state rehospitalization rates, Black nursing facility patients in all states and the District of Columbia experienced more frequent hospital admissions than did White patients, and the magnitude of this racial disparity was more pronounced in some areas.
Policies aimed at reducing rehospitalization of elderly people and the associated Medicare expenditures have been proposed. The Medicare bundled payment for an episode of care across settings (such as hospitals, postacute care facilities, and physician offices)9 is designed to provide financial incentives for better across-setting care coordination and to reduce excessive rehospitalizations and other inefficient uses of resources. In addition, the ongoing Centers for Medicare and Medicaid demonstration of pay for performance is designed to determine the impact of performance-based reimbursements on nursing home quality and Medicare expenditures.39 One of the targeted areas of performance is reduction of inappropriate hospitalizations, and its resulting Medicare savings would be used to financially reward facilities with the best performance.
Our findings suggest that reducing racial disparities in nursing home quality should be another important policy goal in addition to these well-designed initiatives for global quality improvement. Individual facilities, especially those serving mostly minority patients, may lack necessary resources or expertise to improve care quality and have to rely to a greater extent on resource-rich settings, such as hospitals, to serve their patients. As a result, performance-based approaches to quality improvement may unfairly penalize these facilities. Interventions targeting these facilities and their minority patients would be another cost-effective way to reduce rehospitalization and its associated racial disparities.
Limitations
We focused on hospital admissions as an important performance indicator for skilled nursing facilities. In light of the multidimensional nature of nursing home care,40 the issue of racial disparities may not be generalizable to other performance areas. We focused only on non-Hispanic Whites and Blacks in nursing facilities; we excluded patients of other races/ethnicities because of small sample sizes, which prevented accurate comparisons, especially in stratified analyses.
Finally, although we performed detailed multivariable and stratified analyses, we had no way to control for other patient and facility variables, such as patient preferences (although our analyses excluded those with a do-not-hospitalize order and controlled for whether a do-not-resuscitate order was present at admission) and facility practice patterns. Understanding the role of these and other factors in racial disparities in skilled nursing facility rehospitalization will be important in addressing this issue, although it will require in-depth investigation beyond the scope of our study.
Conclusions
Among a national cohort of White and Black patients admitted to skilled nursing facilities, we found that Black race was associated with a 40% increased risk of rehospitalization within 30 days of admission and a 50% increased risk of rehospitalization within 90 days of admission. This racial disparity was largely explained by patient characteristics and facility types, but it persisted after we controlled for these factors in both the overall cohort and subgroups of patients. In the context of current efforts to reduce the overall rehospitalization rate in this vulnerable population, our findings suggest that targeted interventions to address racial disparities could play an important role.
Acknowledgments
This study was funded by the National Institute on Aging (NIA; grant R01AG032264).
Note. The views expressed in this article are those of the authors and do not necessarily represent the views of the NIA or the Department of Veterans Affairs.
Human Participant Protection
This study was approved by the institutional review boards of the University of Iowa and the University of California, Irvine.
References
- 1.Liu K, Garrett B, Wissoker DA, et al. Options for improving Medicare payment for skilled nursing facilities. Urban Institute; 2007. Available at: http://www.urban.org/url.cfm?ID = 411526. Accessed January 25, 2011 [Google Scholar]
- 2.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood). 2010;29(1):57–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donelan-McCall N, Eilertsen TB, Fish R, Kramer A. Small Patient Population and Low Frequency Event Effects on the Stability of SNF Quality Measures. Washington, DC: Medicare Payment Advisory Commision; 2006 [Google Scholar]
- 4.Hutt E, Ecord M, Eilertsen TB, Frederickson E, Kramer AM. Precipitants of emergency room visits and acute hospitalization in short-stay Medicare nursing home residents. J Am Geriatr Soc. 2002;50(2):223–229 [DOI] [PubMed] [Google Scholar]
- 5.Saliba D, Kington R, Buchanan J, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc. 2000;48(2):154–163 [DOI] [PubMed] [Google Scholar]
- 6.Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs [see editorial comments by Drs. Jean F. Wyman and William R. Hazzard, pp 760–761] J Am Geriatr Soc. 2010;58(4):627–635 [DOI] [PubMed] [Google Scholar]
- 7.Ouslander JG, Weinberg AD, Phillips V. Inappropriate hospitalization of nursing facility residents: a symptom of a sick system of care for frail older people. J Am Geriatr Soc. 2000;48(2):230–231 [DOI] [PubMed] [Google Scholar]
- 8.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451–458 [DOI] [PubMed] [Google Scholar]
- 9.Report to the Congress: Medicare Payment Policy. Washington DC: Medicare Payment Advisory Commission; 2008. [Google Scholar]
- 10.Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. JAMA. 1998;279(23):1877–1882 [DOI] [PubMed] [Google Scholar]
- 11.Christian JB, Lapane KL, Toppa RS. Racial disparities in receipt of secondary stroke prevention agents among US nursing home residents. Stroke. 2003;34(11):2693–2697 [DOI] [PubMed] [Google Scholar]
- 12.Allsworth JE, Toppa R, Palin NC, Lapane KL. Racial and ethnic disparities in the pharmacologic management of diabetes mellitus among long-term care facility residents. Ethn Dis. 2005;15(2):205–212 [PubMed] [Google Scholar]
- 13.Li Y, Mukamel DB. Racial disparities in receipt of influenza and pneumococcus vaccinations among US nursing-home residents. Am J Public Health. 2010;100(Suppl 1):S256–S262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baumgarten M, Margolis D, van Doorn C, et al. Black/White differences in pressure ulcer incidence in nursing home residents. J Am Geriatr Soc. 2004;52(8):1293–1298 [DOI] [PubMed] [Google Scholar]
- 15.Cai S, Mukamel DB, Temkin-Greener H. Pressure ulcer prevalence among Black and White nursing home residents in New York state: evidence of racial disparity? Med Care. 2010;48(3):233–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff (Millwood). 2007;26(5):1448–1458 [DOI] [PubMed] [Google Scholar]
- 17.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angelelli J, Grabowski DC, Mor V. Effect of educational level and minority status on nursing home choice after hospital discharge. Am J Public Health. 2006;96(7):1249–1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grabowski DC. The admission of Blacks to high-deficiency nursing homes. Med Care. 2004;42(5):456–464 [DOI] [PubMed] [Google Scholar]
- 20.Gruneir A, Miller SC, Feng Z, Intrator O, Mor V. Relationship between state Medicaid policies, nursing home racial composition, and the risk of hospitalization for Black and White residents. Health Serv Res. 2008;43(3):869–881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Becker MA, Boaz TL, Andel R, Gum AM, Papadopoulos AS. Predictors of preventable nursing home hospitalizations: the role of mental disorders and dementia. Am J Geriatr Psychiatry. 2010;18(6):475–482 [DOI] [PubMed] [Google Scholar]
- 22.Becker M, Andel R, Boaz T, Howell T. The association of individual and facility characteristics with psychiatric hospitalization among nursing home residents. Int J Geriatr Psychiatry. 2009;24(3):261–268 [DOI] [PubMed] [Google Scholar]
- 23.Mor V, Papandonatos G, Miller SC. End-of-life hospitalization for African American and non-Latino White nursing home residents: variation by race and a facility's racial composition. J Palliat Med. 2005;8(1):58–68 [DOI] [PubMed] [Google Scholar]
- 24.Grabowski DC, Feng Z, Intrator O, Mor V. Medicaid bed-hold policy and Medicare skilled nursing facility rehospitalizations. Health Serv Res. 2010;45(6 Pt 2):1963–1980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat 13. 2009;(167):1–155 [PubMed] [Google Scholar]
- 26.Mor V, Angelelli J, Jones R, Roy J, Moore T, Morris J. Inter-rater reliability of nursing home quality indicators in the U.S. BMC Health Serv Res. 2003;3(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawton MP, Casten R, Parmelee PA, Van Haitsma K, Corn J, Kleban MH. Psychometric characteristics of the minimum data set II: validity. J Am Geriatr Soc. 1998;46(6):736–744 [DOI] [PubMed] [Google Scholar]
- 28.Mor V. A comprehensive clinical assessment tool to inform policy and practice: applications of the minimum data set. Med Care. 2004;42(4 Suppl):III50–III59 [DOI] [PubMed] [Google Scholar]
- 29.Stearns SC, Dalton K, Holmes GM, Seagrave SM. Using propensity stratification to compare patient outcomes in hospital-based versus freestanding skilled-nursing facilities. Med Care Res Rev. 2006;63(5):599–622 [DOI] [PubMed] [Google Scholar]
- 30.Grabowski DC, Hirth RA. Competitive spillovers across non-profit and for-profit nursing homes. J Health Econ. 2003;22(1):1–22 [DOI] [PubMed] [Google Scholar]
- 31.US Census Bureau Metropolitan and micropolitan statistical areas. Available at: http://www.census.gov/population/www/metroareas/metroarea.html. Accessed January 25, 2011
- 32.White HA. heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48(4):817–838 [Google Scholar]
- 33.Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev. 2008;65(1):3–39 [DOI] [PubMed] [Google Scholar]
- 34.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52(10):1730–1736 [DOI] [PubMed] [Google Scholar]
- 35.Buchanan JL, Murkofsky RL, O'Malley AJ, et al. Nursing home capabilities and decisions to hospitalize: a survey of medical directors and directors of nursing. J Am Geriatr Soc. 2006;54(3):458–465 [DOI] [PubMed] [Google Scholar]
- 36.Liu K, Black KJ. Hospital-based and freestanding skilled nursing facilities: any cause for differential Medicare payments? Inquiry. 2003;40(1):94–104 [DOI] [PubMed] [Google Scholar]
- 37.O'Brien LA, Grisso JA, Maislin G, et al. Nursing home residents’ preferences for life-sustaining treatments. JAMA. 1995;274(22):1775–1779 [PubMed] [Google Scholar]
- 38.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient–physician relationship. JAMA. 1999;282(6):583–589 [DOI] [PubMed] [Google Scholar]
- 39.Quality Monitoring for Medicare Global Payment Demonstrations: Nursing Home Quality-Based Purchasing Demonstration. Boston, MA: Abt Associates Inc; 2006 [Google Scholar]
- 40.Mukamel DB, Glance LG, Li Y, et al. Does risk adjustment of the CMS quality measures for nursing homes matter? Med Care. 2008;46(5):532–541 [DOI] [PMC free article] [PubMed] [Google Scholar]