Abstract
Climate change presents the biggest threat to human health in the 21st century. However, many public health leaders feel ill equipped to face the challenges of climate change and have been unable to make climate change a priority in service development. I explore how to achieve a regionally responsive whole-of-systems approach to climate change in the key operational areas of a health service: service governance and culture, service delivery, workforce development, asset management, and financing. The relative neglect of implementation science means that policymakers need to be proactive about sourcing and developing models and processes to make health services ready for climate change. Health research funding agencies should urgently prioritize applied, regionally responsive health services research for a future of climate change.
Climate change has emerged as the biggest global health threat of the 21st century. That finding was published in a watershed 2009 article in The Lancet,1 a study that analyzed the global health implications of the summary work of the Intergovernmental Panel on Climate Change.2,3 The Lancet piece1 is supported by more than 10 000 articles on the health effects of climate change published in other leading journals, such as BMJ, Nature, and JAMA.4–6 Over the last 10 years a raft of books7–10 on the subject have also been published, offering detailed discussions of the public health implications of climate change. The health effects of climate change are also the subject of ongoing work for the Global Environmental Change and Human Health project.11
Many people are now familiar with the attribution of extreme weather events to climate change and the direct health effects of these events: death, injuries, and problems with water and food security caused by heat waves, droughts, flooding rains, and cyclones.12,13 Less familiar—but increasingly well documented in the literature—are the indirect health effects of climate change. These include changes in the distribution of insect-borne diseases, such as Ross River virus14; increases in conditions linked to changes in the distribution and seasonality of plant allergens, such as asthma15; and mental health issues linked to extended drought.16 Climate change research has also frequently identified vulnerable groups who may be differently affected by climate change, often within socioeconomically disadvantaged populations, such as older citizens or indigenous peoples.17
However, many key issues involved with translating the climate change literature into health services and workforce development have been neglected. Even relatively affluent nations lack policy frameworks and regional-level evidence that can equip health policymakers to make the translation from big-picture climate change issues to on-the-ground regional service development. The United States has contributed the vast bulk of climate change research, together with other developed countries such as the United Kingdom, Canada, and Australia. However, most public health leaders in the United States feel unprepared for climate change and ill equipped to make the necessary service adaptations,18 despite the recent rapid proliferation of national service-oriented policy guidelines, such as the US Centers for Disease Control and Prevention's CDC Policy on Climate Change and Public Health19 and the UK Department of Health's The Health Impact of Climate Change: Promoting Sustainable Communities.20 Australia has prioritized investment in research that can inform national planning for climate change, and the government has a human health and climate change National Adaptation Research Plan,21 but little is known about changing regional health needs and the related changes to local health care infrastructure that will likely be needed.21,22
BARRIERS TO TRANSLATING RESEARCH INTO SERVICE DEVELOPMENT
The knowledge translation literature—from the 1995 publication of Rogers’ diffusion theory23,24 to more recent work by Nutley et al25—suggests that there are many complex reasons for the poor translation of the climate change research into regional health service development. As seminal policy analysts such as Tesh,26 Stone,27 and Majone28 have argued, policymaking occurs in a context of conflicting values, warring interest groups, and strategic political considerations. Recent work at the “science in society” end of climate change research—notably Dessler and Parson's book The Science and Politics of Climate Change29 and Hulme's Why We Disagree About Climate Change30—pointed to the complexities (and crude realities) of climate change policy debates in which the values of scientific objectivity collide with narrow economic interests.
However, the barriers to translating climate change research into service development stem not only from politics, economics, and values. Studies of research translation also have suggested that such barriers can be related to the quality and relevance of evidence (i.e., the failure of research to engage with the evidence needs of local policymaking contexts).31,32 Dessler and Parson pointed out that climate change science has had much less to say about regional-level impacts (i.e., complex interactions between local climate effects, human systems and activity, and local ecologies).29 Climate change and health research generally has been defined by epidemiological, quantitative methodologies that have been used within a paradigm relating climate change causes to health effects. In such a paradigm, deciphering implications for more localized policy and service development is difficult. Epidemiology has not yet developed a satisfactory approach to evaluating what it calls “neighborhood effects” since the problem was first elaborated in Susser's foundational work, Causal Thinking in the Health Sciences, which explored the wider environmental or ecological contexts of health.29,33–35
Methodological issues aside, studies of research translation also suggest that barriers to research uptake may be related to real but unacknowledged differences between what policymakers need and what climate change researchers think they need.32 The shape of climate change research has also been defined by perceptions within the scientific community and leading journals about which priorities are most pressing and how they should be communicated. For example, many recent articles in The Lancet attend to the pressing need to sell the public health benefits of mitigation36–40 and address broad population health policy issues,41,42 rather than the more qualitative operational questions of how health services themselves will need to be developed. In the context of a perceived global emergency, scholarly research demonstrating the health costs of climate change has been more concerned with persuading global communities to unite to address the global causes of climate change but has not necessarily offered local communities ways of coming together to minimize the local health consequences.
Without intervention, the research market is unlikely to correct this evidence gap or the related situation of policymakers being unsure of how to respond to climate change in their specific regions. Within the health sciences, health service research remains a marginalized area of inquiry. By far the largest contributor to health research is the United States, which has doubled its biomedical health research expenditure since the middle of the 1990s, although only a minute amount of this research (1.5% in 2002) focused on health services.43 Climate change consulting is now one of the fastest-growing subsectors of the lucrative eco-business sector, but the attention there has been focused on carbon-emissions advice rather than training policymakers and other professionals in the public sector.44 Scrutiny of the undergraduate and graduate offerings at universities in the developed world suggests that ecological topics are included in some public policy courses; for example, the Master of Public Health program at Harvard University has core requirements in environmental health sciences, and the Masters in Climate Change at the Australian National University has a strong applied-policy orientation. Yet the work of educating and training health policymakers remains largely undone.
THE ROLE OF HEALTH SERVICES AND HEALTH SERVICES RESEARCH
The lack of service-oriented research to drive regional health service development for climate change has implications that are potentially very serious. An inability on the part of services and systems to meet health needs brought about by climate change will lead to increased injuries, impaired quality of life, and loss of life. In 2002, the World Health Organization45 estimated that climate change was responsible for around 154 000 deaths worldwide, and not just in vulnerable populations in the developing world. For example, an estimated 6% of cases of malaria in middle-income countries and 7% of dengue fever cases in industrialized countries can be attributed to climate change.45 Without regionally responsive research on how local conditions are shaping the rising health burden of climate change in particular regions, public health leaders in the 21st century cannot minimize the direct and indirect health effects of climate change.
The health effects of climate change are not simply caused by climate change as such; they are a result of the ways in which local conditions—including a lack of health services—interact with global forces to produce these health effects. Accounts of the health effects of climate-influenced disasters suggest that a lack of adequate responses and services in the disaster setting is often a necessary (but not sufficient) cause of the health consequences of such events, particularly for vulnerable groups. For example, many low-income people were trapped during Hurricane Katrina because the hurricane occurred at the end of a pay period, and they could not afford the bus fare out of New Orleans.1,46 A lack of adequate gender-sensitive trauma services to deal with the disaster-related rape of economically disadvantaged women after Hurricane Katrina also contributed to the heavy indirect health burden of this disaster.47 A year after the hurricane, many hospitals in the New Orleans area were still closed, contributing to a wide range of long-term health care problems, particularly for the poor and uninsured.48
In appropriate services can also contribute to the health burden from climate change. For example, research conducted in the aid-dependent island microstate of Niue offers evidence that development of services without adequate community consultation can actually impair the capacity of indigenous communities to adapt to climate change by undermining their traditional governance mechanisms, ultimately making them more climate-vulnerable.49
Without regionally responsive service-oriented research, many of the health risks of climate change might even be overstated for particular regions. This overstatement can be seen in the case of malaria, which recent research has shown not to be increasing, contrary to what might be intuitively expected as a result of global warming. Part of the explanation has to do with the effectiveness of public health measures such as medications, insecticides, and bed nets. Epidemiological models that have not taken local service delivery factors into account are now thought to have produced faulty predictions, particularly for well-resourced developed countries. Thus, in a world affected by human activity, malaria and other vector-borne diseases may be consequences of climate change, but not in any simple or direct manner.50–52
I intend here to address the emerging challenge of how to understand and prioritize regional health service development for climate change. I build on the work of researchers who have attempted to translate the scientific climate change literature into public policy responses53 as part of a focus on adapting to climate change, not just mitigating it. Adaptation is defined here as responses by health services that are aimed at reducing the rising health burden of climate change. Mitigation is defined as responses by health services aimed at reducing greenhouse gas emissions—a cause of climate change—to slow global warming. Regional policy in this context refers to public health actions for climate change adaptation and mitigation at the community, municipality, state, and provincial levels. A health service is a multidimensional entity comprising many different interacting elements that may have human and cultural dimensions as well as technological, spatial, and material dimensions.54
THE WHOLE-OF-SYSTEMS POLICY RESPONSE TO CLIMATE CHANGE
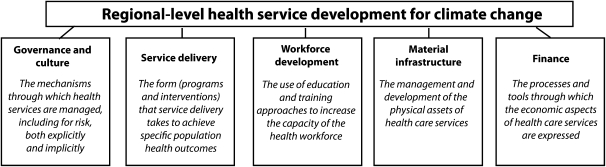
For health service development in a context of climate change, I propose a model that comprises 5 areas or domains of health services: governance and culture, service delivery, workforce development, material infrastructure, and finance. Figure 1 offers definitions of each of these 5 key domains, which together constitute the whole-of-systems approach to climate change.
FIGURE 1.
Definition of a whole-of-systems approach to developing health services for climate change.
Of course, our definitions of the scope of health services reflect our values. Evans and Stoddart reminded us of this fact, recalling a long tradition of research into the socioeconomic determinants of health, to argue that the boundaries of health are not politically neutral.55 The whole-of-systems approach describes health system responses in terms that involve a wide range of health and community services that could feasibly be part of whole-of-government or even whole-of-community responses to climate change. This approach includes strategic, political, and economic responses, not just narrow health interventions. Without such whole-of-system approaches to delivering services for climate change, it is difficult to see how health services can bring about key outcomes for climate-vulnerable populations.
A strength of the whole-of-systems approach is that it highlights a wide range of interactive factors and pathways that need to be considered. Yet how should priorities for specific policymaking contexts be developed? This development will likely require the involvement of policymakers who understand both the big-picture possibilities of health service adaptation and the details of feasible regional priorities that have local community support. Accordingly, I first identify a wide range of likely necessary responses to climate change under each of the 5 service-development areas. Then I extrapolate from those broad understandings to describe the practical steps that might be involved in identifying regional policy priorities. The challenge of anticipatory climate change policy is to identify what needs to be added to existing public health policies and priorities.
Governance and Culture
The climate change literature suggests that the governance and culture of health services will need to adapt to meet the demands of climate change. Health policymakers will need to understand the possibilities of adaptation (and mitigation) through governance that uses a variety of mechanisms—legislative, technical, educational, advisory, cultural, and behavioral. For example, in regards to climate-sensitive waterborne diseases, governance will need to be exercised in the following ways:
legislative and regulatory development to ensure appropriate water quality, using such instruments as the United Nations’ Protocol of Water and Health56;
the management of information systems, such as computerized early-warning systems for epidemics of waterborne diseases;
educational and advisory systems such as policy and practice networks for disseminating clinical guidelines for the management of waterborne diseases; and
community health and social service agencies that can encourage people to adopt safe behaviors for storage, handling, and consumption of water.57
In particular, policymakers will want to consider adapting approaches to managing risk and uncertainty to meet the regional challenges of climate change.5,13 Risk management is an interdisciplinary skill, and risk assessment forms a sprawling body of applied and scholarly literature. Much of the decision support for policymakers in the area of risk management has focused on identifying ways to minimize and control existing and possible risks, such as developing better understandings of risk. The risk management literature also offers ways to conceptualize and map uncertainty as part of the growing science of decision-support modeling, which involves elucidating the nature, level, and sources of uncertainty.58
Clearly, a key task of developing climate change–ready service governance and culture is to assess and develop effective mechanisms for managing risks and uncertainties associated with climate change. This task is central in emerging applied research by health agencies around the world (i.e., the 2008 Health Canada report Human Health in a Changing Climate: A Canadian Assessment of Vulnerabilities and Adaptive Capacity).59 Risk management for climate change can be developed using existing national and international standards for risk management as a point of departure, such as BS 6079-3:2000,60 ISO 31000:2009,61 and Enterprise Risk Management—Integrated Framework.22,62 Health impact assessments have been used to assess and manage the community health risks of an intended action that has environmental implications, such as road construction.63–65 Researchers have recently recognized that health impact assessments can be used in assessments of the regional-level health impacts and risks of climate change, and some have called for their further development for this purpose.66 The World Health Organization has not yet released a model for this application, but there are some important early examples of this kind of applied research, including a major scoping health impact assessment for the state of Victoria in Australia to identify climate-vulnerable populations and related health service issues.67
The management and use of research to respond to regional-level climate change will thus be a particular challenge for policymakers in a context of climate change. For example, it will become increasingly critical to be able to translate applied research from international collaborative agencies such as the World Health Organization and the United Nations, as well as scholarly literature, into well-developed regional-forecasting research infrastructures. Research infrastructure will need to be managed to ensure that it has a strong translational orientation to facilitate futures-oriented policy development with a regional focus. Governance for climate change will also involve establishing effective feedback loops for policy, to ensure timely delivery of information about whether climate change policy is working.
A key task of governance for climate change is to develop effective plans. The United Nations Framework Convention on Climate Change has found that even developed countries lack adequate planning for extreme events. For example, one third of cities in the United States that are vulnerable to heat events have been found to lack any written heat-event plans.57 Such plans will most likely need to encompass multiple goals for both mitigation and adaptation. This approach is modeled in such documents as the recent Heat Health Action Plans from the World Health Organization, which focuses on prevention through a variety of adaptation mechanisms, including regulatory mechanisms for building infrastructure; educational and advisory governance mechanisms, such as meteorological early-warning systems and clinical guidelines for health practitioners; and population health interventions for behavioral adaptations, such as recognizing the signs of heat stress.68 Accordingly, plans for managing the health effects of climate change will ideally integrate different kinds of adaptation mechanisms to model regionally responsive whole-of-community approaches.
An example of the critical importance of well-developed regional planning for climate change is the bushfires tragedy that took place in Victoria, Australia, in which 173 people perished in 12 fires on February 7, 2009. The record-breaking heat-wave conditions on that day—in the city of Melbourne the temperature reached 46.4°C—followed a period of extended drought with near-record low amounts of rainfall. The behavior of the fires was unprecedented:
[flames] leapt 100 m into the air, generating heat so intense that aluminum road signs melted. The plume of the fires created a convection effect that generated winds so strong that trees appeared to have been screwed from the ground.69(p12)
The August 2009 interim report of the Victorian Bushfires Royal Commission69 raises concerns about how well local, state, and national government agencies had integrated evidence-based risk management, including early-warning systems, to ensure that people were willing and able to act upon those warnings. For example, 80% of calls to the Victorian Bushfire Information Service on February 7 went unanswered.69
For other countries, such findings, coming from a wealthy nation that has long experience of bushfires, should be a sobering warning. Beyond Australia, wildfires feature in the work of futures-oriented organizations set up by proactive regional governments, such as the California Climate Change Research Center.70 However, in many regions in the United States and other countries where catastrophic wildfires present a major threat, little evidence exists that lessons from scholarly and applied research are being translated into comprehensive regional planning.
At the time of this writing, Australia was dealing with further climate-influenced loss of life and livelihoods as a result of catastrophic flooding caused by heavy rainfall. An area the size of France and Germany combined has been affected by flood waters moving in sheets tens of kilometers wide. Thirty-five people have died, tens of thousands of homes have been damaged, and billions of dollars of damage have been done to community infrastructure, agriculture, and mining. Indirect effects on food security and mental health will be major. At the domestic level, the Australian floods of 2010 to 2011 have highlighted the importance of regional-level planning and risk management, particularly through local government agencies. Internationally, these floods also point to the critical importance of sharing lessons about such regional-level governance approaches.
Service Delivery
Many complexities are involved in developing programs and interventions for a world whose climate is changing, mostly relating to managing uncertainty. For example, a number of diseases not previously thought to be climate sensitive, such as chicken pox, have now been identified as climate sensitive.71 In addition, climate change will interact with many other factors in unpredictable ways as ecosystems fail and are reshaped by climate change.5,6,9,13,72 For these reasons, policymakers who rely on static assumptions about diseases, their causes, and implications for health service delivery cannot scope out a definitive set of climate-relevant service-delivery issues.
However, service-delivery issues for target areas can be modeled by extrapolating from maps of the direct and indirect consequences of climate change developed using the risk management tools and processes referred to in the Governance and Culture section. Regional risk profiles will need to be established to assess the likely nature of immediate events, such as extreme weather events, as well as long-term health effects stemming from changes in air quality and ozone depletion. The capacity of services to meet shifts in the nature and distribution of infectious diseases such as cholera,13 as well as animal and vector-borne diseases such as malaria,73 will be central to such risk profiles. These profiles will ideally emphasize adapting existing interventions and services so that climate change considerations can be integrated into the health care system in cost-effective ways.
A critical concept in adapting service delivery to climate change is the concept of climate-vulnerable populations.6 Policymakers will need nuanced information about how climate change is differently affecting indigenous populations, older citizens, children, people living with disabilities, and other groups. The adaptive capacity of such groups can be assessed as part of a participatory approach to policy decision-making that involves members of those groups in the development of service responses to climate change.59 To achieve this participative approach, Minkler and Wallerstein offered key regional-level, community needs–mapping tools for vulnerable populations in their edited collection Community Based Participatory Research for Health.74 Policymakers can adapt action research approaches, such as participatory appraisal of needs and development of action,75–77 to involve vulnerable groups in planning and intervention development at the more localized level (not just risk assessment).
Another tool for pre-emptive policy action involving the community is Q-methodology,78 a multistep, mixed qualitative–quantitative approach for identifying and mapping community values and views on a particular policy option. Q-methodology can be adapted for community consultations that help identify and map key climate-vulnerable groups, their needs, and their views on appropriate interventions. Solutions will also need to include public health education programs that can help build the adaptive capacity of local communities, particularly for vulnerable populations.
Such participative approaches are already being used to develop climate-ready services for Canada's northern aboriginal populations.79 Loss of access to food resources and accidents because of ice thinning are affecting these populations, who use sea ice to access wildlife resources and travel between communities during winter months.79 Although indigenous people too often must deal with unequal health outcomes and inequitable access to health care services, early Canadian research79 suggests they also have considerable potential to adapt to climate change. Their observations of changes in their natural environment can also greatly enhance scientific research into the regional effects of climate change.
Workforce Development
The importance of workforce development for climate change is increasingly being understood. For example, climate change has featured in the Global Health Workforce Alliance's efforts to build policy frameworks for workforce development.80 Sentinel organizations such as the World Medical Association are making public statements about the need for better education and training for doctors facing the challenges of climate change.81 Some countries are now reexamining health and allied health workforce policy and planning with consideration of climate change or are reworking climate change planning to include health workforce development. For example, Australia's national adaptation research plan for climate change and human health emphasizes workforce development for climate change as a critical priority.21
At least 3 elements of workforce development are necessary to ensure an effective response to climate change:
undergraduate through postgraduate training in health and allied health professional courses,
professional development of the existing health and allied health workforce, and
professional development of public health policymakers and their staff.
In relation to undergraduate and postgraduate education and training, there are working models for how to integrate ecological considerations, including climate change, into the curriculum.82,83 An emerging body of literature exists, exploring how to include climate change in education and training systems, such as through accreditation mechanisms.84 With regard to professional development of existing health practitioners, health professional groups are increasingly offering guidance concerning key directions,85 and short courses are offered by national professional associations such as the UK Royal College of Physicians. Existing systems and learning models must be adapted and extended, rather than reinvented.86 Yet climate change remains largely not integrated into undergraduate, postgraduate, and continuing professional development for health professionals.
The evidence for professional development of public health policymakers and their staff in government agencies is equally scarce. Available public health training opportunities for climate change tend to focus on a discrete disease area. For example, the US Institute of Medicine of the National Academies has organized public workshops on the possible infectious disease impacts of global climate change.87 Such learning opportunities tend not to address the whole-of-service operational development challenges that regional policymakers face.
The blind spot in workforce development for climate change is thus the whole-of-systems focus for regional contexts. What can regional policymakers do to make education and training more responsive to regional climate change issues? Education and training are often shaped by standardized national and international content. However, the importance of policymakers collaborating with workforce organizations in their own regions should not be understated. Considerable scope exists for individual medical, nursing, and allied health professional schools to include climate change in their interpretations of national curricula and standards. For instance, they could implement problem-based learning through the use of case-based scenarios.86,88 Policymakers can also recruit consultancy services to deliver local training packages developed using the results of regional risk assessment exercises. They can further share their health risk assessment findings with national agencies setting standards and developing curricula for the health professions. They can also support design of materials that help develop the carbon literacy and numeracy (i.e., knowledge about carbon emissions) of patients.
Material Infrastructure
In many regions, health care infrastructure—the built environment of health services—has not been designed to withstand extreme weather events or to contribute to the mitigation of climate change. Yet in a context in which many health services are publicly funded to serve the common good, an argument could be made that health services providers have a particular responsibility to be proactive in mitigating climate change.
In line with the United Nations Framework Convention on Climate Change, development of health care infrastructure should take both mitigation and adaptation responses into account.22,57 For example, mitigation efforts can draw on the Council of the European Union's Emissions Trading System and Energy Performance of Buildings Directive in amended form89 as part of ensuring that health systems meet their best-practice mitigation obligations.
The most comprehensive national model of mitigation for health care services is the UK National Health Service (NHS) carbon-reduction strategy for England, Saving Carbon, Improving Health, published in 2009.90 This model is supported by detailed carbon footprinting analyses,91 and it suggests the political complexity of carbon reduction in the health care sector, which is susceptible to policy shifts by changing governments. For example, procurement of supplies contributes to 60% of emissions from the health care sector, and emissions from procurement of pharmaceuticals account for around one fifth of emissions for the NHS in England (comparable with carbon emissions from travel or building energy use). However, carbon-reduction strategies are relatively poorly developed for pharmaceutical procurement.91 There are also some accessible working models for health service mitigation, such as green hospitals92 and green clinics for family practices.93 However, as yet no sound evidence base exists for the comparative effectiveness of different mitigation models for health services.
Better health infrastructure planning must be developed to deal with such events as heat waves, water-supply problems, and flooding. These challenges may involve such problems as a lack of power supply to affected areas. An important facilities research article by Carthey et al.22 suggested that meeting the challenges of climate change will involve review and development of relevant infrastructure guidelines such as building codes, as well as guidelines for architectural designs and land-use planning. Addressing climate change will also involve review and development of procedures for maintenance of building equipment, such as air conditioning, and building infrastructure, such as roofs and downspouts. Climate change will also pose challenges for environmental management of areas adjacent to health facilities, development and management of transport and road facilities, and planning for better use of other public spaces in case of such public health emergencies as flooding.22
Here, as elsewhere, generic knowledge about how to respond to the infrastructure challenges of climate change has to be supplemented with detailed information about the needs climate change will cause in a particular region. As Carthey et al. pointed out, temperature modeling is currently accurate to 300 × 300 kilometer grids and is not oriented to risk assessments for a particular major critical hospital facility in a built-up urban area.22 They advocate using tools such as the Australian risk and opportunity management system94 as a basis for developing a participative, regional focus in risk-management and solutions-finding exercises.22
The most important step in preparing health care infrastructure for climate change lies in ensuring that asset-management staff are properly trained and aware of the implications of climate change for facilities management in the future. For example, they will need to understand adaptation technologies for water supplies57 in contexts in which local communities may face severe water restrictions. Development of asset-management skills for climate change will require more than extrapolation from existing models and knowledge. As the United Nations Framework Convention on Climate Change has outlined, hazard mapping and infrastructure development will need to emphasize vulnerability-based assessments rather than previous experience, including the use of data from probabilistic computer modeling.57
Finance
A growing body of literature can inform regional policy considerations having to do with financing health care in a context of climate change. Existing approaches to policy decision support that rely on cost-effective modeling95 can be adapted to account for the opportunity cost or true cost of a mitigation or adaptation option, taking into account the cost of forgoing another mitigation or adaptation option. The financial performance of regional health care services in terms of carbon offsetting will be important policy information, requiring new applications of traditional financial reporting methods for health care services. Policymakers will need to develop comparative systems analyses,96 including analyses gauging financial performance, to support decisions about the value of mitigation and adaptation interventions. A complex range of information, both quantitative and qualitative, will be important in ensuring that, for example, adaptation strategies for vulnerable populations are considered in terms of their economic value.
A key priority is the development of business plans and business models for the health care sector that account for mitigation and adaptation situations. The financial analysis literature for climate change indicates the importance of planning for and monitoring likely climate-sensitive shifts in health care demand in both the public and private sectors.97 Such policy decision support can be informed by adapting existing approaches to market share analysis of health services,98 an important new frontier of health policy research. Available models for producing adaptive improvements in the financial performance of hospitals96 can also inform approaches to ensuring that the health care services of the future are sustainable both ecologically and economically.
Such business plans and models can translate the recommendations of the Stern report on the economics of climate change99 into multilevel regional approaches to health care financing in a world of climate change, such as regulation, including regional procurement policies oriented toward carbon reduction; policies that support innovative, regionally responsive financing approaches; financial incentives leading to better regional use of low-carbon technologies; removal of regional-level financial barriers to energy efficiency; and regional-level education and information about financial aspects of climate change.
Signs indicate that the health sector is moving in this direction in at least some countries. For example, the Sustainable Development Unit of the NHS is now developing a systematic approach to mitigation, underpinned by legislation and policy.90 The unit has produced guidelines100 for NHS commissioners that advocate a whole-systems, evidence-based approach to operating the NHS. These guidelines include procurement procedures that calculate emissions using top-down input-output analytical methodology, approaches to energy consumption in which emissions can be calculated from data provided by staff at NHS facilities, and calculation of travel-related emissions on the basis of travel surveys and business mileage.100 The resources produced for health commissioners include a series of marginal abatement cost curves that model the carbon and financial savings from various carbon-reduction measures and provide ideas about how money can be saved and sustainability improved.101 The NHS Sustainable Development Unit emphasizes the emerging nature of such metrics for sustainability and the importance of regional policymakers taking a proactive approach to developing them further for their own purposes.100 Such approaches should include consideration of the future costs of inaction for specific regional communities, in accordance with the Stern report.99
The mitigation experiences of the health care sector to date suggest that the costs of implementing carbon-reduction strategies can be offset by recurrent savings. For example, at Westmead Hospital in New South Wales in Australia, a lighting upgrade that cost approximately $2 million has saved approximately $300 000 each year, leading to an anticipated net financial benefit after 7 years. Such accounts suggest that a 25% reduction in energy consumption is readily achievable, with lighting upgrades delivering a swift 10% reduction.102
Strategies for Development of 5 Key Health Care Service Areas for Climate Change
| Governance and culture | Plan for use of different mechanisms for adaptation—legislative, technical, educational and advisory, cultural, and behavioral. |
| Service delivery | Map direct and indirect health effects using risk management tools; involve climate-vulnerable populations in developing service responses. |
| Workforce development | Develop undergraduate, postgraduate, and professional development systems, including those oriented toward health agency leadership. |
| Material infrastructure | Educate and train asset management staff to use generic and regional information as part of implementing risk management tools. |
| Finance | Adapt economic decision-support approaches and develop business plans and models for mitigation and adaptation. |
Practical Steps to Identify Specific Regional Policy Priorities for the Development of Health Care Services for Climate Change
| 1. Method identification |
| • Identify possibly useful risk management tools (considering standard risk-management tools and health impact assessment tools), guidelines, and models. |
| • Collect information helpful in assessing how well these risk-management tools, guidelines, and models fit the needs of the local context. |
| • Establish a stakeholder reference group of multidisciplinary experts, from service providers to climate change scientists, to ensure regional knowledge translation and implementation. |
| 2. Method modification |
| • Modify risk-management tool to include scope for collecting data on regional-level health risks and possible service developments under the 5 service development domains. |
| • Use both quantitative and qualitative data-collection methods, supplementing quantitative data with observational case studies and interviews with local experts. |
| • Use community consultation methods to ensure a focus on the needs of climate-vulnerable groups, such as children and older citizens as well as the socioeconomically disadvantaged. |
| • Include scope to collect data on the wider pragmatic determinants of policy, such as strategic and economic considerations relevant to service development options. |
| • Work with stakeholder groups to collect trial data and refine data-collection methods. |
| 3. Data collection |
| • Implement tool through stakeholder reference group. |
| • Involve a wide range of health and allied health services in data collection. |
| • Include policymakers and others who can offer accounts of sociopolitical and economic barriers to implementation of any service adaptation options, as well as strategies for overcoming these barriers. |
| • Collect a wide range of supplementary comparative information, such as known benefits and costs of different adaptation (and mitigation) responses in other systems (in other countries and in the same region). |
| 4. Development of data analyses |
| • Analyze data to identify priority areas of risk and adaptation (as well as mitigation) under each of the 5 service development areas. |
| • Use epidemiological and narrative analyses to obtain information-rich findings about the local context. |
| • Invite the stakeholder reference group to review data analyses and provide information on likely lag times of any effects as well as bias introduced by participant populations. |
| • Audit regional findings obtained in this way against local health plans and developments to determine which priorities need to be added to existing public health policies. |
| • Analyze best-practice implications of regional findings in the light of existing guidelines and models for achieving adaptation and mitigation, to help decide what is best practice for this region. |
| 5. Development of service priorities |
| • Develop a user-friendly, written regional impact statement with policy priorities, working with the stakeholder reference group to include: risks for identified groups; likelihood of specific negative (and positive) health outcomes; key health service adaptation and mitigation options for managing each risk, given under the 5 service development domains; cost-benefit analyses of each adaptation and mitigation option, including the costs of inaction; and strategic and political considerations important to the implementation success of the priority adaptation options. |
REGIONAL-LEVEL IMPLEMENTATION
The first box on the previous page summarizes the main strategies for each of the 5 key dimensions of health care service development. Clearly, policymakers will need to tailor policy to suit specific regional needs for adaptation and mitigation. How should the strategies in the box be translated into specific policy priorities for a particular region? The second box on the previous page summarizes the practical steps that policymakers could take to identify specific regional priorities for anticipatory health policy for climate change. It includes an emphasis on the sociopolitical contexts in which regional policymaking occurs, and it emphasizes facilitating knowledge transfer in a context in which many of the main lessons of extreme events have not been well-translated into regional-level responses.
In a context in which many health care systems are internally fragmented and are poorly integrated with sectors and agencies beyond health care, what institutional mechanisms are available to take these steps? The answer will depend on the local context. The prerequisite for filling this role is the capacity to design and implement highly participatory action research, in order to create a 2-way street for knowledge transfer between local and global contexts. Some regional health authorities and regional universities may be able to lead such action research projects, but new mechanisms for achieving regional-level health responses to climate change should not be neglected. In some countries, such as the United Kingdom and Australia, local governments are emerging as regional health leaders for climate change. For example, the Australian government's Climate Change Adaptation Actions for Local Government103 includes development of health services as a key way in which local governments can help their communities adapt to climate change. Regional health risk assessment for climate change is beginning to be included in the work of some local governments as part of the Australian government's Local Adaptation Pathways Program.103 Health policymakers and climate change researchers may be more effective working through such local community agencies.
CONCLUSIONS
The urgent task of ensuring adequate health care responses to climate change involves much more than giving regional policymakers access to the main findings of climate change research. Much of the climate change literature does not offer an evidence base for managing the specific challenges of regional service development that policymakers now face. The climate change literature tells policymakers about big-picture health consequences but does not offer nuanced information about likely regional health service needs. Nor will national guidelines offer the kind of nuanced, contextually rich information essential to regional service development for a world in which the climate is changing.
The implementation science of making health care services climate ready is only beginning to emerge as a discrete area of research endeavor. Accordingly, policymakers will need to develop and adapt approaches that can help make services climate ready, including those that address regional research infrastructure. However, the most urgent task for policymakers may be to insist that elite health research funding agencies urgently prioritize regionally specific applied research for climate-responsive policy and services development. Approaches that unite local communities to find local solutions are needed now.
Acknowledgments
This work was funded by the University Department of Rural Health, University of Tasmania, under an operating grant from the Department of Health and Ageing.
The author would like to thank the many international and Australian researchers, as well as local Tasmanian policymakers, students, and health practitioners, who have supported her work in regional development for climate change. Particular thanks are owed to Associate Professor Elaine Stratford, Head of the School of Geography and Environmental Studies at the University of Tasmania. Thanks are also owed to the author's three reviewers at the American Journal of Public Health for their exacting and useful feedback.
Human Participant Protection
No protocol approval was required because no human research participants were involved.
References
- 1.Costello A, Allen A, Ball S, et al. Managing the health effects of climate change. Lancet. 2009;373(9676):1693–1733 [DOI] [PubMed] [Google Scholar]
- 2.Intergovernmental Panel on Climate Change Summary for policymakers. : Solomon S, Qin D, Manning M, et al., Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK: Cambridge University Press; 2007 [Google Scholar]
- 3.MacCracken M. Prospects for future climate change and the reasons for early action. J Air Waste Manag Assoc. 2008;58(6):735–786 [DOI] [PubMed] [Google Scholar]
- 4.Haines A, Patz JA. Health effects of climate change. JAMA. 2004;291(1):99–103 [DOI] [PubMed] [Google Scholar]
- 5.Patz JA, Campbell-Lendrum D, Holloway T, Foley JA. Impact of regional climate change on human health. Nature. 2005;438(7066):310–317 [DOI] [PubMed] [Google Scholar]
- 6.McMichael AJ, Friel S, Nyong A, Corvalan C. Global environmental change and health: impacts, inequalities, and the health sector. BMJ. 2008;336(7637):191–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menne B, Ebi K. Climate Change Adaptation Strategies for Human Health. Heidelberg, Germany: World Health Organization; 2006 [Google Scholar]
- 8.Ebi K, Smith J, Burton I, eds. Integration of Public Health With Adaptation to Climate Change: Lessons Learned and New Directions. London, UK: Taylor & Francis; 2005 [Google Scholar]
- 9.McMichael A, Campbell-Lendrum D, Corvalan C, et al. Climate Change and Human Health: Risks and Responses. Geneva, Switzerland: World Health Organization; 2003 [Google Scholar]
- 10.Martens P, McMichael A. Environmental Change, Climate and Health: Issues and Research Methods. Cambridge, UK: Cambridge University Press; 2002 [Google Scholar]
- 11.Earth System Science Partnership Global environmental change and human health (GECHH). Available at: http://www.essp.org/index.php?id=13. Accessed May 21, 2010
- 12.Diaz JH. The influence of global warming on natural disasters and their public health outcomes. Am J Disaster Med. 2007;2(1):33–42 [PubMed] [Google Scholar]
- 13.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367(9513):859–869 [DOI] [PubMed] [Google Scholar]
- 14.Woodruff RE, Guest CS, Garner MG, Becker N, Lindsay M. Early warning of Ross River virus epidemics: combining surveillance data on climate and mosquitoes. Epidemiology. 2006;17(5):569–575 [DOI] [PubMed] [Google Scholar]
- 15.Beggs PJ. Impacts of climate change on aeroallergens: past and future. Clin Exp Allergy. 2004;34(10):1507–1513 [DOI] [PubMed] [Google Scholar]
- 16.Morrissey SA, Reser JP. Natural disasters, climate change and mental health considerations for rural Australia. Aust J Rural Health. 2007;15(2):120–125 [DOI] [PubMed] [Google Scholar]
- 17.Woodward A, Scheraga J. Looking to the future: challenges for scientists studying climate change and health. : McMichael A, Campbell-Lendrum D, Corvalan C, et al., Climate Change and Human Health: Risks and Responses. Geneva, Switzerland: World Health Organization; 2003:61–78 [Google Scholar]
- 18.Balbus J, Ebi K, Finzer L, et al. Are We Ready?: Preparing for the Public Health Challenges of Climate Change. New York, NY: Environmental Defense Fund; 2008 [Google Scholar]
- 19.Centers for Disease Control and Prevention Climate change and public health. CDC policy. Available at: http://www.cdc.gov/ClimateChange/policy.htm. Accessed October 5, 2009
- 20.UK Department of Health The health impact of climate change: promoting sustainable communities—guidance document. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/DH_082690. Accessed October 13, 2009
- 21.McMichael A, Weaver H, Berry H, et al. National Adaptation Research Plan: Human Health. Canberra, Australia: National Climate Change Adaptation Research Facility; 2008 [Google Scholar]
- 22.Carthey J, Chandra V, Loosemore M. Adapting Australian health facilities to cope with climate-related extreme weather events. J Facil Manage. 2009;7(1):36–51 [Google Scholar]
- 23.Dobbins M, Ciliska D, Cockerill R, Barnsley J, DiCenso A. A framework for the dissemination and utilization of research for health-care policy and practice. Online J Knowl Synth Nurs. 2002;9:7. [PubMed] [Google Scholar]
- 24.Rogers E. Diffusion of Innovations. New York, NY: Free Press; 1995 [Google Scholar]
- 25.Nutley S, Walter I, Davies H. Using Evidence: How Research Can Inform Public Services. Bristol, UK: Policy Press; 2007 [Google Scholar]
- 26.Tesh S. Hidden Arguments: Political Ideology Disease Prevention Policy. New Brunswick, NJ: Rutgers University Press; 1988 [Google Scholar]
- 27.Stone D. Policy Paradox: The Art of Political Decision-Making. 2nd ed. New York, NY: W.W. Norton; 2002 [Google Scholar]
- 28.Majone G. Evidence, Argument & Persuasion in the Policy Process. New Haven, CT: Yale University Press; 1989 [Google Scholar]
- 29.Dessler A, Parson E. The Science and Politics of Climate Change: A Guide to the Debate. 2nd ed. Cambridge, UK: Cambridge University Press; 2010 [Google Scholar]
- 30.Hulme M. Why We Disagree About Climate Change. Cambridge, UK: Cambridge University Press; 2009 [Google Scholar]
- 31.Black N. Evidence-based policy: proceed with care. BMJ. 2001;323(7307):275–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bell E. Research for Health Policy. Oxford, UK: Oxford University Press; 2010 [Google Scholar]
- 33.Susser M. Causal Thinking in the Health Sciences: Concepts and Strategies of Epidemiology. New York, NY: Oxford University Press; 1973 [Google Scholar]
- 34.Kaufman JS, Poole C. Looking back on “Causal Thinking in the Health Sciences.” Annu Rev Public Health. 2000;21:101–119 [DOI] [PubMed] [Google Scholar]
- 35.Bell E. Great 21st century debates about the usefulness of research: can they help rural research? Rural Soc. 2008;18(1):3–16 [Google Scholar]
- 36.Haines A, McMichael A, Smith K, Roberts I, Woodcock J, Markandya A. Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. Lancet. 2009;374(9707):2104–2114 [DOI] [PubMed] [Google Scholar]
- 37.Markandya A, Armstrong B, Hales S, Chiabai A, Criqui P, Mima S. Public health benefits of strategies to reduce greenhouse-gas emissions: low-carbon electricity generation. Lancet. 2009;374(9706):2006–2015 [DOI] [PubMed] [Google Scholar]
- 38.Friel S, Dangour A, Garnett T, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: food and agriculture. Lancet. 2009;374(9706):2016–2025 [DOI] [PubMed] [Google Scholar]
- 39.Wilkinson P, Smith K, Davies M, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: household energy. Lancet. 2009;374(9705):1917–1929 [DOI] [PubMed] [Google Scholar]
- 40.Woodcock J, Edwards P, Tonne C, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: urban land transport. Lancet. 2009;374(9705):1930–1943 [DOI] [PubMed] [Google Scholar]
- 41.Hajat S, O'Connor M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet. 2010;375(9717):856–863 [DOI] [PubMed] [Google Scholar]
- 42.Semenza JC, Menne B. Climate change and infectious diseases in Europe. Lancet Infect Dis. 2009;9(6):365–375 [DOI] [PubMed] [Google Scholar]
- 43.Moses H, Dorsey E, Matheson D, Thier S. Financial anatomy of biomedical research. JAMA. 2005;294(11):1333–1342 [DOI] [PubMed] [Google Scholar]
- 44.Carr D, ed. Consultancy Market Guide for 2009. 16th ed London, UK: Haymarket Business Media; 2009 [Google Scholar]
- 45.World Health Organization The World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva, Switzerland: World Health Organization; 2002 [Google Scholar]
- 46.Haney T, Elliott J, Fussell E. Families and hurricane response: evacuation, separation, and the emotional toll of hurricane Katrina. In: Brunsma D, Overfelt D, Picou J, eds. The Sociology of Katrina: Perspectives on a Modern Catastrophe. Lanham, MA: Rowman & Littlefield; 2007:8 [Google Scholar]
- 47.Richter R, Flowers T. Gendered dimensions of disaster care: critical distinctions in female psychosocial needs, triage, pain assessment, and care. Am J Disaster Med. 2008;3(1):31–37 [PubMed] [Google Scholar]
- 48.Rudowitz R, Rowland D, Shartzer A. Health care in New Orleans before and after Hurricane Katrina. Health Aff. 2006;25(5):w393–w406 [DOI] [PubMed] [Google Scholar]
- 49.Barnett J. The effect of aid on capacity to adapt to climate change: insights from Niue. Polit Sci. 2008;60(1):31–45 [Google Scholar]
- 50.Ledford H. Malaria may not rise as world warms. Nature. 2010;465(7296):280–281 [DOI] [PubMed] [Google Scholar]
- 51.Chaves LF, Koenraadt CJ. Climate change and highland malaria: fresh air for a hot debate. Q Rev Biol. 2010;85(1):27–55 [DOI] [PubMed] [Google Scholar]
- 52.Gething PW, Smith DL, Patil AP, Tatem AJ, Snow RW, Hay SI. Climate change and the global malaria recession. Nature. 2010;465(7296):342–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Frumkin H, Hess J, Luber G, Malilay J, McGeehin M. Climate change: the public health response. Am J Public Health. 2008;98(3):435–445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bell E. Time, space, and body in adolescent residential services: re-imagining service design research. Addict Res Theory. 2007;15(1):97–111 [Google Scholar]
- 55.Evans RG, Stoddart GL. Consuming research, producing policy? Am J Public Health. 2003;93(3):371–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.United Nations Economic Commission for Europe Convention on the protection and use of transboundary watercourses and international lakes: protocol on water and health. Available at: http://www.unece.org/env/water/text/text_protocol.htm. Accessed September 9, 2009
- 57.United Nations Framework Convention on Climate Change Technologies for Adaptation to Climate Change. Bonn, Germany: Climate Change Secretariat; 2006 [Google Scholar]
- 58.Walker W, Harremoes P, Rotmans J, et al. Defining uncertainty: a conceptual basis for uncertainty management in model-based decision support. Integrated Assess. 2003;4(1):5–17 [Google Scholar]
- 59.Séguin J, ed. Human Health in a Changing Climate: A Canadian Assessment of Vulnerabilities and Adaptive Capacity. Ottawa, Canada: Health Canada; 2008 [Google Scholar]
- 60.British Standards Institution Project Management: Guide to the Management of Business Related Project Risk. BS 6079-3:2000. London, UK: British Standards Insititution; 2000 [Google Scholar]
- 61.International Organization for Standardization Risk Management: Principles and Guidelines. ISO 31000:2009. Geneva, Switzerland: International Organization for Standardization; 2009 [Google Scholar]
- 62.Committee of Sponsoring Organizations of the Treadway Commission Enterprise Risk Management—Integrated Framework. Sarasota, FL: Committee of Sponsoring Organizations of the Treadway Commission; 2004 [Google Scholar]
- 63.European Centre for Health Policy Health impact assessment: main concepts and suggested approach. Gothenburg consensus paper. Brussels, Belgium: European Centre for Health Policy, World Health Organization Regional Office for Europe; 1999 [Google Scholar]
- 64.Mindell JS, Boltong A, Forde I. A review of health impact assessment frameworks. Public Health. 2008;122(11):1177–1187 [DOI] [PubMed] [Google Scholar]
- 65.Cole BL, Fielding JE. Health impact assessment: a tool to help policy makers understand health beyond health care. Annu Rev Public Health. 2007;28:393–412 [DOI] [PubMed] [Google Scholar]
- 66.Patz J, Campbell-Lendrum D, Gibbs H, Woodruff R. Health impact assessment of global climate change: expanding on comparative risk assessment approaches for policy-making. Annu Rev Public Health. 2008;29:27–39 [DOI] [PubMed] [Google Scholar]
- 67.Turk R, Battle C, Hanna E, Spickett J, Raso B. The Scoping of Climate Change Impacts on Population Health and Vulnerabilities—Benchmarking. Melbourne, Australia: Department of Health; 2010 [Google Scholar]
- 68.Matthies F, Bickler G, Cardenosa Marin N, Hales S, eds. Heat Health Action Plans: A Guidance Document. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2009 [Google Scholar]
- 69.Teague B, McLeod R, Pascoe S. 2009 Victorian Bushfires Royal Commission: Interim Report. Melbourne, Australia: State Government of Victoria; 2009 [Google Scholar]
- 70.Dreschler D. Climate change and public health in California. Available at: http://www.energy.ca.gov/2009publications/CEC-500-2009-034/CEC-500-2009-034-F.PDF. Accessed May 25, 2010
- 71.Bultó PL, Rodríguez A, Valencia A, Vega N, Gonzalez M, Carrera A. Assessment of human health vulnerability to climate variability and change in Cuba. Environ Health Perspect. 2006;114(12):1942–1949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Patz JA, Olson SH. Climate change and health: global to local influences on disease risk. Ann Trop Med Parasitol. 2006;100(5–6):535–549 [DOI] [PubMed] [Google Scholar]
- 73.Patz JA, Kovats R. Hotspots in climate change and human health. BMJ. 2002;325(7372):1094–1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Minkler M, Wallerstein N, eds. Community Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003 [Google Scholar]
- 75.White L. The role of systems research and operational research in community involvement: a case study of a health action zone. Syst Res Behav Sci. 2003;20(2):133–145 [Google Scholar]
- 76.Taket A, White L. Experience in the practice of one tradition of multimethodology. Syst Pract Action Res. 1998;11(2):153–168 [Google Scholar]
- 77.White L, Taket A. Beyond appraisal: participatory appraisal of needs and the development of action (PANDA). Omega. 1997;25(5):523–535 [Google Scholar]
- 78.Ellis G, Barry J, Robinson C. Many ways to say “no,” different ways to say “yes”: applying Q-methodology to understand public acceptance of wind farm proposals. J Environ Plann Manage. 2007;50(4):517–551 [Google Scholar]
- 79.Furgal C, Seguin J. Climate change, health, and vulnerability in Canadian northern Aboriginal communities. Environ Health Perspect. 2006;114(12):1964–1970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Health Workforce Advocacy Initiative Guiding principles for national health workforce strategies. Available at: http://www.healthworkforce.info/advocacy/HWAI_Principles.pdf. Accessed October 6, 2009
- 81.World Medical Association WMA declaration of Delhi on health and climate change. Available at: http://www.wma.net/en/30publications/10policies/c5/index.html. Accessed January 5, 2010
- 82.Green EI, Blashki G, Berry H, Harley D, Horton G, Hall G. Preparing Australian medical students for climate change. Aust Fam Physician. 2009;38(9):726–729 [PubMed] [Google Scholar]
- 83.Wilcox B, Kasuya R. Integrating ecohealth into a medical school curriculum: a vision of the future at the University of Hawaii John A. Burns School of Medicine. EcoHealth. 2004;1(suppl 1):S34–S42 [Google Scholar]
- 84.Bell E. Climate change: is Australian rural and remote medical education ready for the age of consequences? Paper presented at: 10th National Rural Health Alliance Conference; May 17–20, 2009; Cairns, Australia. [Google Scholar]
- 85.British Medical Association BMA response to the European commission green paper on the European workforce for health. Available at: http://ec.europa.eu/health/ph_systems/docs/medical_en.pdf. Accessed October 5, 2009
- 86.Bell E. Climate change: what competencies and which medical education and training approaches? BMC Med Educ. 2010;10:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Board on Global Health Global climate change and extreme weather events: understanding the contributions to infectious disease emergence: workshop summary. Available at: http://www.ncbi.nlm.nih.gov/books/NBK45747/pdf/TOC.pdf. Accessed January 25, 2011 [PubMed]
- 88.Rapport DJ, Howard J, Lannigan R, McCauley W. Linking health and ecology in the medical curriculum. Environ Int. 2003;29(2–3):353–358 [DOI] [PubMed] [Google Scholar]
- 89.Council adopts position at first reading on the energy performance of buildings directive [press release]. Brussels, Belgium: Council of the European Union; April 15, 2010 [Google Scholar]
- 90.Sustainable Development Unit Saving Carbon, Improving Health: NHS Carbon Reduction Strategy for England. Cambridge, UK: National Health Service; 2009 [Google Scholar]
- 91.Sustainable Development Unit NHS England carbon emissions carbon footprinting report. Available at: http://www.sd-commission.org.uk/publications/downloads/NHS_Carbon_Emissions_modelling1.pdf. Accessed July 12, 2010
- 92.McGain F, Blashki G, Moon K, Armstrong F. Mandating sustainability in Australian hospitals. Med J Aust. 2009;190(12):719–720 [DOI] [PubMed] [Google Scholar]
- 93.Fogarty A, Blashki G, Morrell E, Horton G. The GreenClinic pilot—educational intervention for environmentally sustainable general practice. Aust Fam Physician. 2008;37(8):681–683 [PubMed] [Google Scholar]
- 94.Loosemore M. Risk and opportunity managment systems (ROMS): a new approach to managing risk using multimedia technology—incorporating stakeholder perceptions of risk into corporate risk management strategies. Available at: http://www.risk-opportunity.com/pdfs/ROMS%20Paper.pdf. Accessed May 26, 2010
- 95.Mauskopf JA, Paul J, Grant D, Stergachis A. The role of cost-consequence analysis in healthcare decision-making. Pharmacoeconomics. 1998;13(3):277–288 [DOI] [PubMed] [Google Scholar]
- 96.Beynon M, Kitchener M. Ranking the “balance” of state long-term care systems: a comparative exposition of the SMARTER and CaRBS techniques. Health Care Manage Sci. 2005;8(2):157–166 [DOI] [PubMed] [Google Scholar]
- 97.Bosello F, Roson R, Tol R. Economy-wide estimates of the implications of climate change: human health. Ecol Econ. 2006;58(3):579–591 [Google Scholar]
- 98.Wells R, Banaszak-Holl J. A critical review of recent US market level health care strategy literature. Soc Sci Med. 2000;51(5):639–656 [DOI] [PubMed] [Google Scholar]
- 99.Stern N. The Stern Review: The Economics of Climate Change. London, UK: Cabinet Office, HM Treasury; 2006 [Google Scholar]
- 100.Sustainable Development Unit Commissioning for sustainability. Available at: http://www.sdu.nhs.uk/publications-resources/8/Commissioning-for-Sustainability. Accessed May 25, 2010
- 101.AEA Technology NHS England marginal abatement cost curve. Cambridge, UK: NHS Sustainable Development Unit; 2010. Available at: http://www.sdu.nhs.uk/documents/MACC_Final_SDU_and_AEA.pdf. Published January 2010. Accessed January 25, 2011 [Google Scholar]
- 102.Pencheon D, Rissel C, Hadfield G, Madden L. Health sector leadership in mitigating climate change: experience from the UK and NSW. N S W Public Health Bull. 2009;20(11–12):173–176 [DOI] [PubMed] [Google Scholar]
- 103.Department of Climate Change Climate Change Adaptation Actions for Local Government. Canberra, Australia: Department of Climate Change; 2009 [Google Scholar]