Abstract
Objectives. Integrating evidence from demography and epidemiology, we investigated whether the association between maternal achieved status (education) and infant mortality differed by maternal place of origin (nativity) over the life course of Chinese Americans.
Methods. We conducted a population-based cohort study of singleton live births to US-resident Chinese American mothers using National Center for Health Statistics 1995 to 2000 linked live birth and infant death cohort files. We categorized mothers by nativity (US born [n = 15 040] or foreign born [n = 150 620]) and education (≥ 16 years, 13–15 years, or ≤ 12 years), forming 6 life-course trajectories. We performed Cox proportional hazards regressions of infant mortality.
Results. We found significant nativity-by-education interaction via stratified analyses and testing interaction terms (P < .03) and substantial differentials in infant mortality across divergent maternal life-course trajectories. Low education was more detrimental for the US born, with the highest risk among US-born mothers with 12 years or less of education (adjusted hazard ratio = 2.39; 95% confidence interval = 1.33, 4.27).
Conclusions. Maternal nativity and education synergistically affect infant mortality among Chinese Americans, suggesting the importance of searching for potential mechanisms over the maternal life course and targeting identified high-risk groups and potential downward mobility.
The infant mortality rate (IMR), defined as deaths at younger than 1 year of age per 1000 births, is a benchmark of how a nation cares for its future generations as well as a sensitive indicator of the impact of socioeconomic disparities on population health.1–3 Infant mortality remains a major public health concern in the United States because of its persistent high rate relative to that of other developed nations and continuing racial/ethnic and socioeconomic disparities.4,5 To reduce infant death,4,6 recent research has recognized the need for transdisciplinary models and sociocultural considerations.6–10 Clearly, focused explorations within a single racial/ethnic group might advance our understanding of the mechanisms of health inequalities and potentially avoidable inequalities in infant mortality.
Evidence obtained from epidemiology and demography converges to formulate an interactive life-course perspective in which infant survival results from “differential developmental trajectories set forth by early life experiences and cumulative allostatic load over the life course.”11(p13) The differential and cumulative exposures to risk and protective factors, particularly during sensitive periods of development over the maternal life course, shape developmental trajectories and result in disparities in infant survival.11 In contrast with proximate determinants,8,12 early life exposures represent distal exposures in life-course trajectories,13 which helps elucidate mechanisms by which environments and experiences of one generation transmit health assets or hazards to the next.14
Despite the widely cited significant impact of interactions between maternal social factors on infant mortality among non-Hispanic Whites, Hispanics, and African Americans,7,8,12,15–17 empirical investigation of the interaction between distal and proximate factors over the life course was lacking in these reports. One social science study, which investigated the associations of parental social origins (e.g., parental education and father's occupation) and respondent's education with adult well-being, highlighted the respondent's education as achieved status, a proxy for resources, skills, and abilities in the status attainment process, all of which influence health.18 Another seminal study from Aberdeen, Scotland, reported that in the 1950s, “upwardly mobile” mothers, defined as those born into a lower social class (as determined by paternal occupation) but later married into a higher social class (as determined by husband's occupation), tended to be healthier and had lower rates of perinatal mortality than those who married within the lower social class.19 This latter study clearly indicates that the environment into which a mother is born interacts with the conditions present during pregnancy to affect infant survival.11,13,20 Despite interventions to improve maternal life-course development through nurse home visitation,21,22 few studies to date have investigated infant survival over maternal life-course trajectories.19,23
From an interactive life-course perspective, the question arises as to whether infant survival is influenced only by maternal place of origin or interacted upon jointly by achieved status. Maternal higher education is associated with low risk of infant death,4,24 whereas nativity status is distal in the maternal life-course trajectory. Among African Americans, Mexican Americans, and Puerto Ricans, maternal foreign-born or Puerto Rican–born status is generally associated with a lower risk of infant mortality.25–28 Conventional thought suggests that foreign-born or Puerto Rican–born mothers tend to be characterized by better physical and mental health and a host of protective behaviors and culture, whereas US-born status is often associated with loss of cultural protection and erosion of health advantages over time.25–28 Recent research has described immigrant adaptation as a segmented assimilation process by which individuals experience divergent socioeconomic mobility (upward or downward) and reciprocal interactions.2,29–31 Low birthweight (LBW) is another crucial indictor of population health and life-course trajectories,32 and correlates strongly with the risk of infant death.1 To date, the segmented assimilation process has been used only in 1 study to explain interactions between maternal nativity and neighborhood immigrant orientation on LBW in Los Angeles County.32
Paradoxically, foreign-born status has not been favorable for infant mortality in subgroups of Asian Americans and Pacific Islanders,25,26,33,34 who represent the fastest-growing American racial/ethnic group.35,36 They are recently arrived, extremely heterogeneous, and poorly understood in terms of infant survival and child care during acculturation into American society.37 Furthermore, despite increasing recognition of nativity-dependent maternal race/ethnicity effects on infant mortality and nativity-dependent maternal educational effects on LBW among non-Hispanic Whites, African Americans, Mexican Americans, and Central and South Americans,12,17,38,39 similar considerations have been missing from subgroups of Asian Americans and Pacific Islanders.
Chinese Americans are particularly worthy of study of their life course and the potential effects of nativity-by-education interaction on infant mortality. The persistence of parent–child ties and distinctive strategies (split household, small-business family, and dual-wage-earner family) adopted by Chinese American families over 3 different historical periods of the past 100 years testify to their resilience in overcoming political economic constraints.40 Chinese Americans have had unique experiences40 and possible unique life-course trajectories that can inform our “big picture” understanding of sociocultural influence on health.
The unusually low IMRs of Chinese Americans since 1955 compared with other racial/ethnic groups have been puzzling.25,26,41 Possible explanations include reporting errors, extremely low rates of pregnancy among adolescents, maternal higher education, and favorable perinatal health practices, but the life-course perspective has never been considered. Moreover, assuming that the effects of nativity and education were additive, 4 studies reported insignificant nativity differentiation (i.e., adjusted confidence intervals included 1) among the 1985–1987, 1989–1991, and 1995–2000 national birth cohorts as well as the 1992–1997 and 1999–2003 California birth cohorts.25,26,33,34 Little concern has been given to infant survival among Chinese Americans because they have been considered a “model minority,”42 characterized by “hard-work, family solidarity, discipline, respect, and delayed gratification,”43(p39) all of which contribute to their survival and success in the face of extreme hardships and discrimination.43 As a result of legislative actions since 1989 as well as the influx of large numbers of illegal Chinese immigrants in the early 1990s,44,45 changing demographic trends suggest that the findings in earlier cohorts could be unreliable today.33
Furthermore, no investigation of cause-specific infant death among Chinese Americans has taken place since the analysis of the 1983–1984 birth cohorts.46 Because interactions between social factors are relevant to specific causes of infant death,15 special attention should be paid to Chinese Americans, whose behaviors and practices may play a role between distal and proximate determinants over the maternal life course. For example, Chinese cultural norms may influence infant care practices (e.g., sleeping on the back), which in turn affect susceptibility to sudden infant death syndrome (SIDS).46 Higher maternal education has been associated with reduced infant exposure to transportation accidents and injury, which may reflect better maternal driving practices.47 Finally, government policies to ban immigrant entitlements to programs and jobs may directly affect social context and individual susceptibility to illness or death.48
We therefore hypothesized that infant mortality among Chinese Americans occurs within an interactive life-course perspective. Our aim was to discover whether, among Chinese Americans, (1) infant mortality varies by maternal nativity status, (2) the association of maternal education with infant mortality varies by maternal nativity, and (3) cause-specific infant mortality varies by maternal nativity. Concerning the “model minority” image, we compared paternal race, maternal sociodemographic factors, prenatal care utilization, and IMR of foreign-born Chinese Americans with those of non-Hispanic Whites.
METHODS
Because of the scarcity of nationally representative data for Chinese American mothers and infants,37 and following the practices of recent life-course studies using recalls of early-life exposures in questionnaires or surveillance systems,18,49–52 we conducted a population-based cohort study. The National Center for Health Statistics 1995–2000 linked live birth and infant death cohort files provided data on resident live births compiled from birth certificates for all 50 states and the District of Columbia, with high match rates and completeness for infant deaths occurring up to 1 year after the birth.53 After excluding births with missing covariates of interest, we selected all singleton live births to US-resident mothers with a self-reported race classification of Chinese (n = 165 660) and a self-reported nativity status, and classified them as US-born (15 040) and foreign-born (150 620) Chinese Americans. Because the sample sizes varied widely, to perform the appropriate significance tests, we selected from 13 524 770 non-Hispanic Whites a random sample equal in size to the foreign-born Chinese American sample (n = 150 620). Further details are described elsewhere33 and in Table 1.
TABLE 1.
Characteristics of Foreign-Born and US-Born Chinese American Mothers and Non-Hispanic White Mothers With Singleton Live Births: National Center for Health Statistics, 1995–2000
| Non-Hispanic Whites (n = 150 620), % | Chinese Americans, % |
P for Foreign-Born vs US-Born Chinese Americans | P for Foreign-Born Chinese Americans vs Whites | ||
| US Born (n = 15 040) | Foreign Born (n = 150 620) | ||||
| Residence categorya | < .05 | < .05 | |||
| Category I | 11.5 | 33.9 | 42.2 | ||
| Category II | 37.1 | 56.1 | 48.6 | ||
| Category III | 51.4 | 10.0 | 9.2 | ||
| Unmarried | 21.9 | 11.4 | 6.7 | < .05 | < .05 |
| Age, y | < .05 | < .05 | |||
| < 18 | 3.1 | 1.4 | 0.1 | ||
| 18–34 | 82.8 | 67.8 | 74.6 | ||
| ≥ 35 | 14.0 | 30.8 | 25.3 | ||
| Education, y | < .05 | < .05 | |||
| ≤ 12 | 45.6 | 12.9 | 34.9 | ||
| 13–15 | 24.7 | 15.9 | 14.6 | ||
| ≥ 16 | 29.7 | 71.2 | 50.4 | ||
| Having first child | 42.6 | 51.7 | 50.2 | < .05 | < .05 |
| High parity for age | 1.7 | 0.4 | 0.1 | < .05 | < .05 |
| Previous pregnancy loss | 2.7 | 2.5 | 2.3 | NS | < .05 |
| Race of father | < .05 | < .05 | |||
| Chinese | 0.6 | 36.6 | 82.8 | ||
| Non-Hispanic White | 88.2 | 41.9 | 9.5 | ||
| Otherb | 11.2 | 21.5 | 7.7 | ||
| Prenatal care use | < .05 | < .05 | |||
| Intensive | 6.6 | 5.0 | 3.9 | ||
| Adequate | 43.9 | 48.5 | 42.4 | < .05 | < .05 |
| Intermediate | 39.0 | 36.6 | 41.4 | ||
| Inadequate | 5.5 | 4.0 | 6.4 | ||
| None | 0.6 | 0.3 | 0.3 | NS | < .05 |
| Missing | 4.5 | 5.6 | 5.6 | NS | < .05 |
| Initiated during first trimesterc | 87.8 | 92.2 | 87.2 | < .05 | < .05 |
Note. NS = not significant.
Source. Adapted from Li et al.33
Maternal residence was categorized by the population in the place of residence as follows: category I, population of 250 000 or more for both city and county; category II, less than 250 000 for city and 250 000 or more for county; and category III, less than 250 000 for both city and county.
”Other” included births involving unknown or missing data (for non-Hispanic Whites, 8.7%; for US-born Chinese Americans, 3.9%; for foreign-born Chinese Americans, 2.7%).
Births involving missing data for month in which prenatal care began (for non-Hispanic Whites, 1.6%; for US-born Chinese Americans, 2.4%; for foreign-born Chinese Americans, 3.1%) were excluded from percentage calculations.
Measures
We investigated 3 infant mortality measures. Neonatal mortality was defined as infant deaths occurring prior to 28 days of age. Postneonatal mortality was defined as infant deaths occurring at 28 days or more of life. Infant mortality specific to birthweight and gestational age was defined as the number of infant deaths per 1000 live births in that particular subcategory (≥ 2500 g, 1500–2499 g, or 500–1499 g; ≥ 37 or < 37 weeks of gestation). LBW was defined as birthweight less than 2500 grams. Causes of infant deaths for the 1995–1998 and 1999–2000 cohorts were classified according to the International Classification of Diseases, Ninth Revision54 and Tenth Revision55 (ICD-9 and ICD-10), respectively. On the basis of the scheme proposed by Sowards56 and the National Center for Health Statistics Report,57 we grouped and ranked unified categories for leading causes of infant death.
We categorized mothers by 2 nativity groups (foreign and US born) and 3 educational strata (≥ 16, 13–15, and ≤ 12 years of education), thereby forming 6 all-inclusive and mutually exclusive58 life-course trajectories. Because of the small numbers of infant deaths, we combined the lowest 2 of the 4 educational strata used in previous studies.38,39 There were too few infant deaths to study specific causes over the 6 life-course trajectories, but we were able to make comparisons between the 2 nativity groups.
We categorized paternal race status as non-Hispanic White, Chinese, and other.33 We measured parity as high for age, average for age, and low for age, based on a published algorithm.59 The adequacy of prenatal care utilization was defined by the R-GINDEX formula.60
Statistical Analysis
We used the χ2 test for bivariate associations. We employed the PHREG procedure in SAS version 9.13 (SAS Institute, Cary, NC) to perform Cox proportional hazards regression analyses, integrating the strengths of the respective life table and regression techniques.61 We modeled (1) the additive associations of nativity and education with infant mortality, ignoring the nativity-by-education interaction; (2) the association of nativity with infant mortality when stratified by education; (3) the association of education with infant mortality when stratified by nativity; (4) the differentials in mortality among the 6 life-course trajectories and combinations of education by nativity; and (5) nativity–education interaction terms in nonstratified analyses. Covariates included paternal race, marital status, maternal age, parity, maternal residence, and prenatal care utilization.
Previous pregnancy loss did not differ by maternal nativity and was dropped. We selected α = 0.05 as the level of significance. All reported tests of statistical significance were 2 sided, except for a bivariate association between maternal nativity and SIDS because families in China often place sleeping infants on their backs rather than stomachs.46 In this regard, the lower risk of SIDS among the foreign-born Chinese Americans was possibly associated with having a shorter exposure to the Western practice of placing infants on their stomachs in comparison with their US-born counterparts. This association with risk of SIDS was assumed less likely to be affected by the introduction of the “Back to Sleep” campaign in 1994.62
RESULTS
Compared with non-Hispanic Whites and US-born Chinese Americans (Table 1),33 foreign-born Chinese Americans were (1) less likely to reside in a city or county with a population of less than 250 000, be unmarried, be an adolescent mother, have high parity for age, or adequately use prenatal care (P < .01) and (2) more likely to have a Chinese partner (P < .01). Compared with US-born Chinese Americans, foreign-born Chinese Americans were more likely to have low education and begin prenatal care after the first trimester (P < .01).
The IMR of infants born to Chinese American mothers (2.9 of 1000 live births; 3.5 per 1000 for US-born mothers and 2.8 per 1000 for foreign-born mothers) was lower than that of infants born to non-Hispanic White mothers (4.7 per 1000; P < .01). As shown in Table 2, overall, IMR did not vary between infants born to US-born and foreign-born Chinese American mothers by age in days at the time of death, birthweight, or gestational age strata, but it varied by maternal educational strata (P < .05), with US-born Chinese American mothers educated for less than 12 years having the highest risk of infant death among the 6 life-course trajectories (7.8 per 1000 live births; P < .01). In the 1500- to 2499-gram birthweight stratum, the neonatal mortality rate among foreign-born Chinese American mothers was significantly higher than that among their US-born counterparts (P = .04). None of the perinatal outcomes of US-born Chinese Americans were significantly higher than those of non-Hispanic Whites (data available upon request). Among infants weighing more than 2500 grams, those born to foreign-born Chinese American mothers had lower risks of IMR than those born to non-Hispanic White mothers (P < .01). Among infants weighing less than 2500 grams, those born to foreign-born Chinese American mothers also had lower risks of IMR than those born to non-Hispanic White mothers, whereas this differential disappeared in the 2 LBW strata (P = .09 and .75 for 1500–2499 g and 500–1499 g, respectively). There was a similar pattern for birthweight-specific neonatal mortality.
TABLE 2.
Mortality Rates Among Singleton Live Births to Foreign-Born and US-Born Chinese American Mothers and Non-Hispanic White Mothers: National Center for Health Statistics, 1995–2000
| Non-Hispanic Whites (n = 150 620), Mortality Ratea (No./Total) | Chinese American Mortality Ratea (No./Total) |
P for Foreign-Born vs US-Born Chinese Americans | P for Foreign-Born Chinese Americans vs Whites | ||
| Mortality Category | US Born (n = 15 040) | Foreign Born (n = 150 620) | |||
| IMR | 4.7 (714/150 620) | 3.5 (52/15 040) | 2.8 (426/150 620) | .17 | < .01 |
| NMR | 2.9 (438/150 620) | 2.3 (34/15 040) | 1.8 (269/150 620) | .19 | < .01 |
| Post-NMR | 1.8 (276/14 624) | 1.2 (18/15 006) | 1.0 (157/150 351) | .58 | < .01 |
| Birthweight-specific IMRb | |||||
| ≥ 2500 g | 2.2 (316/143 227) | 1.7 (24/14 214) | 1.3 (187/144 743) | .22 | < .01 |
| < 2500 g | 53.7 (395/7362) | 33.7 (27/801) | 40.1 (233/5812) | .38 | < .01 |
| 1500–2499 g | 20.2 (125/6180) | 11.2 (8/714) | 15.9 (81/5079) | .33 | .09 |
| 500–1499 g | 174.4 (189/1084) | 197.5 (16/81) | 168.6 (116/688) | .51 | .75 |
| Birthweight-specific NMRb | |||||
| ≥ 2500 g | 0.8 (119/143 227) | 0.8 (12/14 214) | 0.5 (66/144 743) | .05 | < .01 |
| < 2500 g | 43.1 (317/7362) | 26.2 (21/801) | 34.2 (199/5812) | .23 | < .01 |
| 1500–2499 g | 11.8 (73/6180) | 4.2 (3/714) | 11.6 (59/5079) | .04 | .92 |
| 500–1499 g | 152.2 (165/1084) | 185.2 (15/81) | 152.6 (105/688) | .44 | .98 |
| Gestational age-specific IMRb | |||||
| ≥ 37 wk | 2.3 (313/135 647) | 1.4 (19/13 462) | 1.3 (187/138 631) | .85 | < .01 |
| < 37 wk | 29.4 (358/12 175) | 24.5 (28/1145) | 23.9 (9217/9069) | .91 | .02 |
| Maternal education-specific IMR | |||||
| ≤ 12 y | 6.1 (421/68 610) | 7.8 (15/1935) | 3.4 (179/52 487) | < .01 | < .01 |
| 13–15 y | 4.2 (157/37 182) | 5.4 (13/2388) | 2.8 (61/21 958) | .02 | < .01 |
| ≥ 16 y | 3.0 (136/44 772) | 2.2 (24/10 701) | 2.4 (183/75 853) | .74 | .04 |
Note. IMR = infant mortality rate, NMR = neonatal mortality rate.
Source. Adapted from Li et al.33
Deaths per 1000 live births.
Rates exclude births with missing values (for birthweight strata, 31 among non-Hispanic Whites, 25 among US-born Chinese Americans, and 65 among foreign-born Chinese Americans; for gestational age strata, 2798 among non-Hispanic Whites, 433 among US-born Chinese Americans, and 2920 among foreign-born Chinese Americans).
Table 3 provides the adjusted hazard ratios of 3 mortality risks of Chinese American infants. Section 1 of the table shows that they did not differ by maternal nativity when the nativity-by-education interaction is ignored. Section 2 shows that the associations between nativity and infant and neonatal mortality varied by maternal educational strata. Section 3 shows that the educational gradient in infant mortality was much more pronounced among US-born Chinese Americans (hazard ratio [HR] = 2.11–2.32) than among their foreign-born counterparts (HR = 1.15–1.45). A similar pattern was apparent for postneonatal mortality. Section 4 shows that 3 life-course trajectories for Chinese Americans—US born with 12 years of education or less, foreign born with 12 years of education or less, and US born with 13 to 15 years of education—had significantly higher IMRs than did foreign-born Chinese Americans with 16 years or more of education. US-born Chinese Americans with 12 years of education or less had the highest risk of infant mortality (HR = 2.39; 95% confidence interval [CI] = 1.33, 4.27) and postneonatal mortality (HR = 3.15; 95% CI = 1.42, 6.97).
TABLE 3.
Adjusted Hazard Ratios (AHRs) and 95% Confidence Intervals (CIs) of Infant Mortality Among Singleton Live Births to Foreign-Born and US-Born Chinese American Mothers, With or Without a Nativity–Education Interaction: National Center for Health Statistics, 1995–2000
| Infant Mortality, AHR (95% CI) |
Postneonatal Mortality, AHR (95% CI) |
Neonatal Mortality, AHR (95% CI) |
||||
| Section No. Variable | US Born | Foreign Born | US Born | Foreign Born | US Born | Foreign Born |
| Section 1, nativity | 1.00 | 0.87 (0.64, 1.19) | 1.00 | 0.99 (0.58, 1.69) | 1.00 | 0.82 (0.55, 1.20) |
| Section 2, nativity by education, y | ||||||
| ≤ 12 | 1.00 | 0.61 (0.33, 1.12) | 1.00 | 0.45 (0.19, 1.07) | 1.00 | 0.85 (0.34, 2.12) |
| 13–15 | 1.00 | 0.48* (0.25, 0.94) | 1.00 | 0.70 (0.24, 2.02) | 1.00 | 0.36* (0.16, 0.86) |
| ≥ 16 | 1.00 | 1.24 (0.79, 1.93) | 1.00 | 2.59 (0.92, 7.30) | 1.00 | 0.96 (0.58, 1.59) |
| Section 3, education by nativity, y | ||||||
| ≤ 12 | 2.32* (1.05, 5.14) | 1.45* (1.16, 1.82) | 5.36* (1.30, 22.06) | 1.37 (0.94, 1.99) | 1.47 (0.50, 4.33) | 1.50* (1.14, 1.99) |
| 13–15 | 2.11* (1.05, 4.24) | 1.15 (0.86, 1.54) | 4.06* (1.04, 15.79) | 1.27 (0.80, 2.01) | 1.72 (0.74, 3.98) | 1.09 (0.75, 1.58) |
| ≥ 16 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Section 4, life-course trajectories | ||||||
| Foreign born, ≥ 16 y | 1.00 | 1.00 | 1.00 | |||
| US born, ≥ 16 y | 0.86 | (0.56, 1.33) | 0.39 | (0.14, 1.07) | 1.13 | (0.69, 1.85) |
| Foreign born, 13–15 y | 1.17 | (0.87, 1.57) | 1.25 | (0.79, 1.99) | 1.11 | (0.77, 1.62) |
| Foreign born, ≤ 12 y | 1.50* | (1.20, 1.87) | 1.34 | (0.93, 1.94) | 1.59* | (1.21, 2.10) |
| US born, 13–15 y | 1.97* | (1.11, 3.50) | 1.88 | (0.74, 4.78) | 2.00* | (1.96, 4.16) |
| US born, ≤ 12 y | 2.39* | (1.33, 4.27) | 3.15* | (1.42, 6.97) | 1.70 | (0.70, 4.12) |
Note. Adjusted for marital status, maternal age, parity, paternal race, maternal residence, and prenatal care utilization. Section 1 assumed the additive effects of nativity and education only, and adjusted for maternal education additionally.
P < .05.
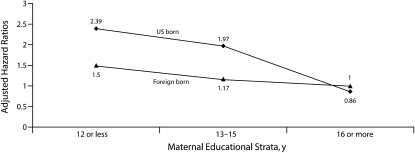
Figure 1 shows substantial nativity differentials in infant mortality in the low educational strata and a dramatic convergence at the high educational strata. When maternal education was dichotomized as 12 years or less or as more than 12 years, the nativity-by-education interactions were further confirmed for infant mortality and postneonatal mortality via significant nativity–education interaction terms (P < .03).
FIGURE 1.
Adjusted hazard ratios of infant mortality predicted by maternal nativity status and educational strata among singleton live births to foreign-born and US-born Chinese American mothers: National Center for Health Statistics, 1995–2000.
Note. The results reflect adjustment for marital status, maternal age, parity, paternal race, maternal residence, and prenatal care utilization.
Cause-specific mortality rates and rankings of causes of death differed by maternal nativity (Table 4). Specifically, the highest-ranking cause of infant death among foreign-born Chinese Americans was congenital malformations, whereas disorders relating to short gestation and unspecified LBW were prominent among US-born Chinese Americans. The numbers of both causes dropped in the postneonatal period. Infants born to US-born Chinese Americans had a higher risk of SIDS in both the infant and postneonatal periods (P = .03 for 1-tailed Fisher exact test). Gender ratios (male:female) for SIDS deaths were 3:2 among non-Hispanic Whites, 3:1 among US-born Chinese Americans, and 2:1 among foreign-born Chinese Americans, with no gender differential in SIDS across maternal nativity status of Chinese Americans (P = .79 for Fisher exact test).
TABLE 4.
Leading Causes of Infant and Postneonatal Death Among Singleton Live Births to Foreign-Born and US-Born Chinese American Mothers and Non-Hispanic White Mothers: National Center for Health Statistics, 1995–2000
| Chinese Americans | ||||||
| Non-Hispanic Whitesa | US Bornb | Foreign Bornc | ||||
| Cause of Death | Rank | No. (Rate)d | Rank | No. (Rate)d | Rank | No. (Rate)d |
| Infant period | ||||||
| All causes | 714 (4.7) | 52 (3.5) | 426 (2.8) | |||
| Congenital malformations | 1 | 186 (1.2) | 3 | 7 (0.5) | 1 | 117 (0.8) |
| Short gestation and unspecified low birthweight | 2 | 162 (1.1) | 1 | 18 (1.2) | 2 | 100 (0.7) |
| Sudden infant death syndrome | 3 | 102 (0.7) | 2 | 8 (0.5) | 4 | 34 (0.2) |
| Infection | 4 | 56 (0.4) | 4 | 4 (0.3) | 3 | 35 (0.2) |
| External reasons | 5 | 26 (0.2) | 1 (0.1) | 5 | 13 (0.1) | |
| Birth asphyxia and respiratory distress of newborn | 6 | 18 (0.1) | 0 | 6 | 7 (0) | |
| Postneonatal period | ||||||
| All causes | 276 (1.8) | 18 (1.2) | 157 (1) | |||
| Sudden infant death syndrome | 1 | 97 (0.6) | 1 | 8 (0.5) | 1.5e | 32 (0.2) |
| Congenital malformations | 2 | 54 (0.4) | 2 | 2 (0.1) | 1.5e | 32 (0.2) |
| Infection | 3 | 29 (0.2) | 1 (0.1) | 3 | 17 (0.1) | |
| External reasons | 4 | 22 (0.1) | 1 (0.1) | 4 | 13 (0.1) | |
| Short gestation and unspecified low birthweight | 5 | 9 (0.1) | 1 (0.1) | 3 (0) | ||
For infant period, n = 150 620; for postneonatal period, n = 150 183.
For infant period, n = 15 040; for postneonatal period, n = 15 006.
For infant period, n = 150 620; for postneonatal period, n = 150 351.
Mortality rate per 1000 live births.
Median rank of the tied data.
DISCUSSION
To our knowledge, the nativity-by-education interaction effect on infant mortality has never been reported previously. Our study found significant nativity-by-education interaction through stratified analyses and the testing of interaction terms. It also found substantial differentials and inequalities in infant mortality across 6 life-course trajectories of Chinese American mothers. Low maternal educational attainment was more detrimental for the infants of US-born Chinese American mothers than for the infants of their foreign-born counterparts, with the infants of US-born mothers with 12 years of education or less being most at risk. The findings for infant mortality were the same pattern as for the postneonatal mortality, which was largely influenced by social and environmental factors.63 Our findings indicate that maternal nativity and education affect infant mortality among Chinese Americans synergistically, and that infant survival might not be influenced only by maternal place of origin but by its interaction with maternal education.
Unlike previous researchers,25,26,33,34 we found that considering the additive associations of maternal nativity and education alone blurs the observed substantial heterogeneity and inequalities of infant mortality among Chinese Americans. We concur with other authors31 that the “model minority” image of Chinese Americans functions to homogenize the group. Our study clearly demonstrates the importance of integrating demography and epidemiology and using an interactive life-course perspective to better understand the determinants of infant mortality.
Interpretations and Implications
Although it is not known how Chinese American mothers’ educational status moderates the effect of maternal place of origin on infant mortality, we propose that intergenerational solidarity and transfer between infants’ mothers and grandparents could provide a means of transmitting the skills needed for routine tasks over their life courses,64 and should be an area of further research. Cross-culturally, it has been reported that intergenerational solidarity and transfer have facilitated the successful adaptation of younger generations of migrant families in 8 affluent countries.65 To understand disparities in LBW among women of Mexican descent, researchers have considered intergenerational transfer of knowledge about diet and stress reduction during pregnancy.66
Differential interactions between people and their environment can influence disparities in infant survival, primarily through intimate (e.g., partner and intergenerational) relationships that exist not only within a family but also extend to anonymous contacts within neighborhoods (e.g., ethnic enclave).8,12,67,68Generally, with different rates of acculturation between immigrant parents and their US-born or US-raised children (e.g., parental pressure for high academic achievement), the cultural gap between a given family and society challenges family relationships and exacerbates diverse circumstances, including intergenerational discrepancies and conflicts, rebellious behavior, withdrawal from school, and alienation from networks.69–71 For immigrants, welfare from the state or other institutions rarely functions adequately; more commonly, the family (nuclear or extended) becomes the sole provider of welfare and information transfer to individuals in need. In this manner, intergenerational solidarity and effective instrumental and moral transfers enable immigrant families in Turkey to cope with the difficulties of acculturation.72 Evidence from China often has characterized relationships between the generations as being marked by filial piety and reciprocity,73,74 with most commentary relating to the duty of the younger generation to support elders.75 This line of research has been limited in the United States, and one recent study described generational differences in Chinese American adolescents’ perceived family closeness and relationship satisfaction with their parents.76 In the case of Chinese American mothers specifically, we propose that support and transfer are bidirectional, with advice from grandparents (regardless of residence) held in high regard, particularly for health behaviors and attitudes that might affect pregnancy and infant survival. Future studies need to determine if dysfunctional intergenerational relations might be associated with higher influence of low education on infant death risk among US-born Chinese American mothers.
Our findings complement 2 explanations of the relationship between immigration and health: the segmented assimilation process29–31 and the healthy selection process,27,28,77 acting alone or in combination. The substantial heterogeneity in infant mortality among Chinese Americans in this study provides new and in-depth evidence regarding reciprocal interactions between the contexts of exit (maternal place of origin) and reception (maternal educational stratum) via segmented assimilation.29–31 In contrast to unidirectional upward mobility of the “model minority,” 6 subgroups of Chinese Americans may experience divergent life-course trajectories through segmented assimilation, creating “ ‘distinctive’ social environments and cultural patterns of adaptation for the group, giving rise to opportunities or constraints for the individual, independent of individual socio-economic and demographic characteristics.”31(p1123)
Maternal education is critical in navigating and negotiating social and institutional environments, and is also important in the system of stratification in infant and child mortality.12,15 Education is generally considered to be a primary means of upward mobility in American families. In our study, the highest risk of infant mortality was among US-born Chinese American mothers with 12 years or less of education, who might experience socioeconomic downward mobility and adaptation into lower segments of society. Conversely, in a study in Aberdeen, Scotland, Illsley found that rates of perinatal mortality were lower among the infants of upwardly mobile mothers.19
The downward mobility in our study may result from women adopting unhealthy lifestyles and accruing limited social capital from family ties and ethnic community resources,31,69 which could be associated with documented mental health problems (e.g., depression, suicide) among Chinese American adolescents and college students.78–80 Downward mobility might explain the highest risk in infant mortality among US-born Chinese American mothers with 12 years or less of education and indicate poor interaction of the individual with her environment.81 At the same time, the positive selection of healthier and more robust immigrants may limit the educational gradient in infant mortality among the foreign born.27,28,77 Importantly, the significantly higher neonatal death risk among infants with birthweights of 1500 to 2499 grams who were born to foreign-born compared with US-born Chinese Americans, and the disappearance of the risk of infant and neonatal death among 2 LBW strata of foreign-born Chinese Americans compared with non-Hispanic Whites, may be associated with disparities in access to quality obstetric and neonatal care82 and require investigation.
Although the health care needs of lower-educated US-born Chinese American mothers require special attention, these needs may be overshadowed by the myth of the “model minority”42,43 or lumped together with the needs of the entire foreign-born group. Meanwhile, both congenital malformations among the infants of foreign-born Chinese American mothers and the SIDS risk among the US-born mothers also require attention. Consistent with the findings of Collins et al. regarding postneonatal mortality among US-born Mexican American mothers,63 a higher risk of SIDS among the infants of US-born Chinese Americans may point to a greater frequency of intentional injury and active neglect.63 In the 1983–1984 birth cohort, the risk of SIDS was greater among the female infants of Chinese Americans46; in the 1995–2000 birth cohort, by contrast, the risk was greater among male infants, but there was no difference between the gender ratios for the infants of US-born and foreign-born mothers. A preference for male babies has long been present in Asian cultures, as has a gender differential in infant mortality in China.83 Our study calls for further investigation of the nativity differential in SIDS and changing gender patterns among Chinese Americans.
Strengths and Limitations
The key strength of our study was that we integrated evidence from demography and epidemiology in an interactive life-course perspective to investigate risk of infant death among a large sample of Chinese Americans. The study also had several limitations. There were too few cases of cause-specific deaths in the subgroups to explore either nativity differentiation or the nativity-by-education interaction. The mothers’ self-recalled early life exposures could be subject to bias,51,52 but the question of maternal nativity status is clear and unambiguous. We were unable to trace repeated deliveries for individual women across the 6 calendar years of this administrative data set. There may have been miscoding or misclassification (e.g., of causes of infant death),84 and comparability of self-reported education between US-born and foreign-born Chinese Americans may not be exact. Maternal country of birth, place of education,85 immigration cohort, length of US residence, parental inherited diseases, and adverse behaviors may further explain the heterogeneity in infant survival in future studies, but they were not completely available in the current data set. Without measurement of the cognitive, material, and psychosocial resources gained through maternal education and accumulated over the life course,86 the observed nativity-by-education interaction effect on infant mortality is explorative rather than confirmative. Finally, our data set lacked plausible constructs, including stable family units, close intergenerational ties, and economic self-sufficiency, all of which are well documented in social sciences40,69 and might shed light on the parental characteristics, family ecology, and neighborhood contexts of Chinese Americans.32,68,87
Conclusions
Our findings indicate that maternal nativity and education synergistically affect infant mortality among Chinese Americans, suggesting the importance of searching for potential mechanisms over the maternal life course and targeting high-risk groups and potential downward mobility to advance research and practice aimed at reducing infant mortality. Compared with rates among non-Hispanic Whites and other immigrant groups,27,63 infant mortality and postneonatal mortality among Chinese Americans were so low that the strategies used by this group to secure infant survival and reduce stress and allostatic load over the maternal life course warrant investigation.11 Inclusion of life-course socioeconomic measures in surveillance systems would help in both monitoring and understanding health inequalities.49 Our study supports the inclusion of life-course socioeconomic measures in the future revision of US birth certificates.88 Incremental advances in life-course research will require primary data collection,27,28 longitudinal data that span a prolonged period,89 and advanced measures of social origin, achieved status, and mediating processes in a broad range of racial/ethnic groups.
Acknowledgments
This study was supported in part by an Isaac E. Capilouto Scholarship from the School of Public Health and the Center for Social Medicine and Sexually Transmitted Diseases, Department of Sociology, University of Alabama at Birmingham, and by The Thompson Foundation.
Preliminary findings from this study were presented at the Third Asia Pacific Congress in Maternal Fetal Medicine, Nanjing, China, August 2007; the 13th Maternal and Child Health Epidemiology Conference, Atlanta, December 2007; and the American Public Health Association Annual Meeting, Philadelphia, November 2009. They were also discussed at the 22nd Society for Pediatric and Perinatal Epidemiologic Research Conference and the 42nd Society for Epidemiologic Research Conference, Anaheim, CA, June 2009.
We gratefully acknowledge comments from anonymous peer referees and editors from Social Science and Medicine and the American Journal of Public Health, and assistance from Greg Alexander, Russell Kirby, Sean-Shong Hwang, William Cockerham, Mark LaGory, Gigliola Baruffi, Min Zhou, Larry Burd, James W. Collins, Richard Scribner, Nancy Landale, Jeffrey Evans, Stella M. Yu, Samantha Rowe, Sioban Harlow, Xinguang Chen, Xiaoming Li, Zhiying You, and Denise Giles.
Human Participant Protection
The National Center for Health Statistics 1995–2000 linked live birth and infant death cohort files, with all personal identifiers removed, were public access files. The present study was reviewed and approved by the institutional review board at the University of North Dakota.
References
- 1.Gortmaker SL, Wise PH. The first injustice: socioeconomic disparities, health services technology, and infant mortality. Annu Rev Sociol. 1997;23:147–170 [DOI] [PubMed] [Google Scholar]
- 2.Finch BK. Early origins of the gradient: the relationship between socioeconomic status and infant mortality in the United States. Demography. 2003;40(4):675–699 [DOI] [PubMed] [Google Scholar]
- 3.Collins JW, Jr, Schulte NF. Infant health: race, risk, and residence. : Kawachi I, Berkman LF, Neighborhoods and Health. New York, NY: Oxford University Press; 2003:223–232 [Google Scholar]
- 4.Hogue CJ, Vasquez C. Toward a strategic approach for reducing disparities in infant mortality. Am J Public Health. 2002;92(4):552–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh GK, Kogan MD. Persistent socioeconomic disparities in infant, neonatal, and postneonatal mortality rates in the United States, 1969–2001. Pediatrics. 2007;119(4):e928–e939 [DOI] [PubMed] [Google Scholar]
- 6.Koontz AM, Buckley KA, Ruderman M. The evolution of fetal and infant mortality review as a public health strategy. Matern Child Health J. 2004;8(4):195–203 [DOI] [PubMed] [Google Scholar]
- 7.Wise PH. The anatomy of a disparity in infant mortality. Annu Rev Public Health. 2003;24:341–362 [DOI] [PubMed] [Google Scholar]
- 8.Mosley WH, Chen LC. An analytical framework for the study of child survival in developing countries. Popul Dev Rev. 1984;10(suppl):25–45 [PMC free article] [PubMed] [Google Scholar]
- 9.Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox: demographic and epidemiologic approaches. Ann N Y Acad Sci. 2001;954:140–174 [DOI] [PubMed] [Google Scholar]
- 10.Scribner R. Paradox as paradigm—the health outcomes of Mexican Americans. Am J Public Health. 1996;86(3):303–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30 [DOI] [PubMed] [Google Scholar]
- 12.Cramer JC. Social factors and infant mortality: identifying high-risk groups and proximate causes. Demography. 1987;24(3):299–322 [PubMed] [Google Scholar]
- 13.Misra DP, Guyer B, Allston A. Integrated perinatal health framework. A multiple determinants model with a life span approach. Am J Prev Med. 2003;25(1):65–75 [DOI] [PubMed] [Google Scholar]
- 14.Emanuel I, Hale CB, Berg CJ. Poor birth outcomes of American black women: an alternative explanation. J Public Health Policy. 1989;10(3):299–308 [PubMed] [Google Scholar]
- 15.Eberstein IW, Nam CB, Hummer RA. Infant mortality by cause of death: main and interaction effects. Demography. 1990;27(3):413–430 [PubMed] [Google Scholar]
- 16.Hummer RA, Eberstein IW, Nam CB. Infant mortality differentials among Hispanic groups in Florida. Soc Forces. 1992;70(4):1055–1075 [Google Scholar]
- 17.Din-Dzietham R, Hertz-Picciotto I. Infant mortality differences between Whites and African Americans: the effect of maternal education. Am J Public Health. 1998;88(4):651–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reynolds JR, Ross CE. Social stratification and health: education's benefit beyond economic status and social origins. Soc Probl. 1998;45(2):221–247 [Google Scholar]
- 19.Illsley R. Social class selection and class differences in relation to stillbirths and infant deaths. BMJ. 1955;2(4955):1520–1524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Emanuel I. Invited commentary: an assessment of maternal intergenerational factors in pregnancy outcome. Am J Epidemiol. 1997;146(10):820–825 [DOI] [PubMed] [Google Scholar]
- 21.Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the life-course development of socially disadvantaged mothers: a randomized trial of nurse home visitation. Am J Public Health. 1988;78(11):1436–1445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olds DL, Kitzman H, Cole R, et al. Effects of nurse home-visiting on maternal life course and child development: age 6 follow-up results of a randomized trial. Pediatrics. 2004;114(6):1550–1559 [DOI] [PubMed] [Google Scholar]
- 23.Sever LE, Emanuel I. Intergenerational factors in the etiology of anencephalus and spina bifida. Dev Med Child Neurol. 1981;23(2):151–154 [DOI] [PubMed] [Google Scholar]
- 24.Pena R, Wall S, Persson LA. The effect of poverty, social inequity, and maternal education on infant mortality in Nicaragua, 1988–1993. Am J Public Health. 2000;90(1):64–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1996;86(6):837–843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hummer RA, Biegler M, Turk PBD, et al. Race/ethnicity, nativity, and infant mortality in the United States. Soc Forces. 1999;77(3):1083–1117 [Google Scholar]
- 27.Landale NS, Oropesa RS, Gorman BK. Migration and infant death: assimilation or selective migration among Puerto Ricans. Am Sociol Rev. 2000;65(6):888–909 [Google Scholar]
- 28.Landale NS, Gorman BK, Oropesa RS. Selective migration and infant mortality among Puerto Ricans. Matern Child Health J. 2006;10(4):351–360 [DOI] [PubMed] [Google Scholar]
- 29.Portes A, Zhou M. The new second generation: segmented assimilation and its variants. Ann Am Acad Pol Soc Sci. 1993;530(1):74–96 [Google Scholar]
- 30.Zhou M. Segmented assimilation: issues, controversies, and recent research on the new second generation. Int Migr Rev. 1997;31(4):975–1008 [PubMed] [Google Scholar]
- 31.Zhou M, Xiong YS. The multifaceted American experiences of the children of Asian immigrants: lessons for segmented assimilation. Ethn Racial Stud. 2005;28(6):1119–1152 [Google Scholar]
- 32.Finch BK, Lim N, Perez W, Do P. Toward a population health model of segmented assimilation: the case of low birth-weight in Los Angeles. Sociol Perspect. 2007;50(3):445–468 [Google Scholar]
- 33.Li Q, Keith L, Kirby RS. Perinatal outcomes of foreign-born and US-born Chinese Americans in the United States, 1995–2000. J Immigr Minor Health. 2010;12(3):282–289 [DOI] [PubMed] [Google Scholar]
- 34.Qin C, Gould JB. Maternal nativity status and birth outcomes in Asian immigrants. J Immigr Minor Health. 2010;12(5):798–805 [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention State-specific trends in US live births to women born outside the 50 states and the District of Columbia—United States, 1990 and 2000. MMWR Morb Mortal Wkly Rep. 2002;51(48):1091–1095 [PubMed] [Google Scholar]
- 36.Kitano H, Daniels R. Asian Americans: Emerging Minorities. Englewood Cliffs, NJ: Prentice Hall; 1995 [Google Scholar]
- 37.Ghosh C. Healthy People 2010 and Asian Americans/Pacific Islanders: defining a baseline of information. Am J Public Health. 2003;93(12):2093–2098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Acevedo-Garcia D, Soobader MJ, Berkman LF. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics. 2005;115(1):e20–e30 [DOI] [PubMed] [Google Scholar]
- 39.Acevedo-Garcia D, Soobader MJ, Berkman LF. Low birthweight among US Hispanic/Latino subgroups: the effect of maternal foreign-born status and education. Soc Sci Med. 2007;65(12):2503–2516 [DOI] [PubMed] [Google Scholar]
- 40.Glenn EN. Split household, small producer and dual wage earner: an analysis of Chinese-American family strategies. J Marriage Fam. 1983;45(1):35–46 [Google Scholar]
- 41.Yu E. The low mortality rates of Chinese infants: some plausible explanatory factors. Soc Sci Med. 1982;16(3):253–265 [DOI] [PubMed] [Google Scholar]
- 42.Lin-Fu JS. Asian and Pacific Island Americans: an overview of demographic characteristics and health care issues. Asian Am Pac Isl J Health. 1993;1(1):20–36 [PubMed] [Google Scholar]
- 43.Zhou M. Intra-group diversity: Asian American population dynamics and challenges of the 21st century. : Ling H, Asian America: Forming New Communities, Expanding Boundaries. Piscataway, NJ: Rutgers University Press; 2009:25–44 [Google Scholar]
- 44.Skeldon R. Migration from China. J Int Aff. 1996;49(2):434–455 [Google Scholar]
- 45.Wong MG. Chinese Americans. : Min PG, Asian Americans: Contemporary Issues and Trends. 2nd ed Thousand Oaks, CA: Pine Forge Press; 2005:110–145 [Google Scholar]
- 46.Wang X, Strobino DM, Guyer B. Differences in cause-specific infant mortality among Chinese, Japanese, and white Americans. Am J Epidemiol. 1992;135(12):1382–1393 [DOI] [PubMed] [Google Scholar]
- 47.Wicklund K, Moss S, Frost F. Effects of maternal education, age, and parity on fatal infant accidents. Am J Public Health. 1984;74(10):1150–1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bollini P, Siem H. No real progress towards equity: health of migrants and ethnic minorities on the eve of the year 2000. Soc Sci Med. 1995;41(6):819–828 [DOI] [PubMed] [Google Scholar]
- 49.Chittleborough CR, Taylor AW, Baum FE, Hiller JE. Monitoring inequities in self-rated health over the life course in population surveillance systems. Am J Public Health. 2009;99(4):680–689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Watt HC, Carson C, Lawlor DA, Patel R, Ebrahim S. Influence of life course socioeconomic position on older women's health behaviors: findings from the British Women's Heart and Health Study. Am J Public Health. 2009;99(2):320–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.James SA, Van Hoewyk J, Belli RF, Strogatz DS, Williams DR, Raghunathan TE. Life-course socioeconomic position and hypertension in African American men: the Pitt County Study. Am J Public Health. 2006;96(5):812–817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang S, Lynch JW, Raghunathan TE, Kauhanen J, Salonen JT, Kaplan GA. Socioeconomic and psychosocial exposures across the life course and binge drinking in adulthood: population-based study. Am J Epidemiol. 2007;165(2):184–193 [DOI] [PubMed] [Google Scholar]
- 53.MacDorman MF, Atkinson JO. Infant mortality statistics from the 1997 period, linked birth/infant death data set. Natl Vital Stat Rep. 1999;47(23). Available at: http://www.cdc.gov/nchs/linked.htm. Accessed June 12, 2008 [PubMed] [Google Scholar]
- 54.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 55.International Classification of Diseases, Tenth Revision. Geneva, Switzerland: World Health Organization; 1992 [Google Scholar]
- 56.Sowards KA. What is the leading cause of infant mortality? A note on the interpretation of official statistics. Am J Public Health. 1999;89(11):1752–1754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Anderson RN, Minino AM, Hoyert DL, Rosenberg HM. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. Natl Vital Stat Rep. 2001;49(2):1–32 [PubMed] [Google Scholar]
- 58.Hallqvist J, Lynch J, Bartley M, Lang T, Blane D. Can we disentangle life course processes of accumulation, critical period and social mobility? An analysis of disadvantaged socio-economic positions and myocardial infarction in the Stockholm Heart Epidemiology Program. Soc Sci Med. 2004;58(8):1555–1562 [DOI] [PubMed] [Google Scholar]
- 59.Alexander GR, Baruffi G, Mor J, Kieffer E. Maternal nativity status and pregnancy outcome among US-born Filipinos. Soc Biol. 1992;39(3–4):278–284 [DOI] [PubMed] [Google Scholar]
- 60.Alexander GR, Cornely DA. Racial disparities in pregnancy outcomes: the role of prenatal care utilization and maternal risk status. Am J Prev Med. 1987;3(5):254–261 [PubMed] [Google Scholar]
- 61.Cox DR. Regression models and life-tables. J R Stat Soc Ser B. 1972;34(2):187–220, with discussion. [Google Scholar]
- 62.The Eunice Kennedy Shriver National Institute of Child Health and Human Development SIDS rate and sleep position, 1988–2003. 2003. Available at: http://www.nichd.nih.gov/sids/upload/SIDS_rate_backsleep_03.pdf. Accessed June 20, 2009
- 63.Collins JW, Jr, Papacek E, Schulte NF, Drolet A. Differing postneonatal mortality rates of Mexican-American infants with United-States-born and Mexico-born mothers in Chicago. Ethn Dis. 2001;11(4):606–613 [PubMed] [Google Scholar]
- 64.Cockerham W. Health lifestyle theory and the convergency of agency and structure. J Health Soc Behav. 2005;46(1):51–67 [DOI] [PubMed] [Google Scholar]
- 65.United Nations Children's Fund (UNICEF) Children in immigrant families in eight affluent countries: their family, national and international context. UNICEF Innocenti Research Centre, Florence, Italy, 2009. Available at: http://www.unicef-irc.org/publications/pdf/ii_immig_families.pdf. Accessed October 23, 2009 [Google Scholar]
- 66.Johnson MA, Marchi KS. Segmented assimilation theory and perinatal health disparities among women of Mexican descent. Soc Sci Med. 2009;69(1):101–109 [DOI] [PubMed] [Google Scholar]
- 67.Peak C, Weeks JR. Does community context influence reproductive outcomes of Mexican origin women in San Diego, California? J Immigr Health. 2002;4(3):125–136 [DOI] [PubMed] [Google Scholar]
- 68.Earls F, Carlson M. The social ecology of child health and well-being. Annu Rev Public Health. 2001;22:143–166 [DOI] [PubMed] [Google Scholar]
- 69.Zhou M. Negotiating culture and ethnicity: intergenerational relations in Chinese immigrant families in the United States. : Mahalingam R, Cultural Psychology of Immigrants. Mahwah, NJ: Lawrence Erlbaum; 2006:315–336 [Google Scholar]
- 70.Zhou M, Bankston CL., III Delinquency and acculturation in the twenty-first century: a decade's change in a Vietnamese American community. : Martinez RJ, Valenzuela AJ, Immigration and Crime: Ethnicity, Race, and Violence. New York, NY: New York University Press; 2006:117–139 [Google Scholar]
- 71.Juang LP, Syed M, Takagi M. Intergenerational discrepancies of parental control among Chinese American families: links to family conflict and adolescent depressive symptoms. J Adolesc. 2007;30(6):965–975 [DOI] [PubMed] [Google Scholar]
- 72.Kalaycıoğlu S, Rittersberger-Tılıç H. Intergenerational solidarity networks of instrumental and cultural transfers in a sample of migrant families in Turkey. Ageing Soc. 2000;20(5):523–542 [Google Scholar]
- 73.Yan Y. The Flow of Gifts: Reciprocity and Social Networks in a Chinese Village. Stanford, CA: Stanford University Press; 1996 [Google Scholar]
- 74.Agree EM, Biddlecom AE, Valente TW. Intergenerational transfers of resources between older persons and extended kin in Taiwan and the Philippines. Popul Stud (Camb). 2005;59(2):181–195 [DOI] [PubMed] [Google Scholar]
- 75.Zimmer Z, Kwong J. Family size and support of older adults in urban and rural China: current effects and future implications. Demography. 2003;40(1):23–44 [DOI] [PubMed] [Google Scholar]
- 76.Willgerodt MA, Thompson EA. The influence of ethnicity and generational status on parent and family relations among Chinese and Filipino adolescents. Public Health Nurs. 2005;22(6):460–471 [DOI] [PubMed] [Google Scholar]
- 77.Rumbaut RG, Weeks JR. Unraveling a public health enigma: why do immigrants experience superior perinatal health outcomes? Res Sociol Health Care. 1996;13B:337–391 [Google Scholar]
- 78.Zhang J, Jin S. Determinants of suicide ideation: a comparison of Chinese and American college students. Adolescence. 1996;31(122):451–467 [PubMed] [Google Scholar]
- 79.Jose PE, Huntsinger CS. Moderation and mediation effects of coping by Chinese American and European American adolescents. J Genet Psychol. 2005;166(1):16–43 [DOI] [PubMed] [Google Scholar]
- 80.Ozer EJ, McDonald KL. Exposure to violence and mental health among Chinese American urban adolescents. J Adolesc Health. 2006;39(1):73–79 [DOI] [PubMed] [Google Scholar]
- 81.Castro FG. Is acculturation really detrimental to health? Am J Public Health. 2007;97(7):1162 [Google Scholar]
- 82.Sanderson M, Sappenfield WM, Jespersen KM, Liu Q, Baker SL. Association between level of delivery hospital and neonatal outcomes among South Carolina Medicaid recipients. Am J Obstet Gynecol. 2000;183(6):1504–1511 [DOI] [PubMed] [Google Scholar]
- 83.Li S, Feldman MW. Sex differential of infant mortality in China: level and trend. Chin J Popul Sci. 1996;8(3):249–267 [PubMed] [Google Scholar]
- 84.Alexander GR, Petersen DJ, Wingate MS, Kirby RS. Research issues in maternal child health. : Kotch JB, Maternal and Child Health: Programs, Problems, Policy in Public Health. 2nd ed Sudbury, MA: Jones and Bartlett Publishers Inc.; 2005:493–534 [Google Scholar]
- 85.Zeng Z, Xie Y. Asian-Americans’ earnings disadvantage reexamined: the role of place of education. Am J Sociol. 2004;109(4):1075–1108 [Google Scholar]
- 86.Lynch J, Kaplan G. Socioeconomic position. : Berkman LF, Kawachi I, Social Epidemiology. New York, NY: Oxford University Press; 2000:13–35 [Google Scholar]
- 87.Jenny AM, Schoendorf KC, Parker JD. The association between community context and mortality among Mexican-American infants. Ethn Dis. 2001;11(4):722–731 [PubMed] [Google Scholar]
- 88.Division of Vital Statistics, National Center for Health Statistics Report of the Panel to Evaluate the US Standard Certificates and Reports. 2000. Available at: http://www.cdc.gov/nchs/data/dvs/panelreport_acc.pdf. Accessed June 28, 2009 [Google Scholar]
- 89.Collins JW, Jr, Wu SY, David RJ. Differing intergenerational birth weights among the descendants of US-born and foreign-born whites and African Americans in Illinois. Am J Epidemiol. 2002;155(3):210–216 [DOI] [PubMed] [Google Scholar]