Abstract
Objectives. We evaluated the relationship between having an intellectual or developmental disability (IDD) and the timing of the first dental visit for children who were newly enrolled in Medicaid in Iowa.
Methods. We identified children aged 3 to 8 years with and without IDD who were newly enrolled in the Iowa Medicaid program in 2005 (N = 5391). We gathered data on presence of IDD, health status, age at baseline, gender, length of Medicaid enrollment, medical care visits, household Medicaid enrollment, urbanization, residence in a federally designated Health Professional Shortage Area (HPSA), and time of first dental visit through 2007.
Results. About 32% of children had a first dental visit within 6 months of enrollment; this proportion increased to 49%, 64%, and 74% by years 1, 2, and 3, respectively. In the unadjusted models, there was no significant difference between children with and without IDD in time to first dental visit (P = .22). After adjusting for model covariates, however, children with IDD were 31% more likely to have a delayed first dental visit (P = .04).
Conclusions. Newly Medicaid-enrolled children aged 3 to 8 years with IDD in Iowa were significantly more likely to have a later first dental visit. Future interventions should focus on ensuring timely access to first dental visits for all Medicaid-enrolled children, with an emphasis on those with IDD.
The Institute of Medicine's 2001 publication Crossing the Quality Chasm stresses that receiving health care services at the appropriate time is an important measure of health care quality.1 Although this report does not explicitly discuss dental care, it is widely accepted that the timing of dental visits is important in preventing the onset and progression of dental caries, the most common chronic childhood disease in the United States.2,3 Ensuring that children have earlier first dental visits—ideally by age 12 months, as recommended by the American Academy of Pediatric Dentistry4—optimizes the benefits associated with the establishment of a dental home, including the provision of caries risk assessments,5 anticipatory guidance,6–9 oral hygiene instruction,10,11 dietary counseling,12,13 and health education.14,15 Earlier first dental visits also allow dentists to provide children at increased risk for caries with appropriate preventive dental care, such as pit and fissure sealants and topical fluoride treatments.16–20
Previous research suggests that children with an intellectual or developmental disability (IDD) are at increased risk for dental caries. For instance, many children with IDD take prescription medications that result in xerostomia and reduced salivary buffering capacity.21 In addition, children with IDD often have behavioral comorbidities that make it difficult for caregivers to provide regular oral hygiene.22 From a provider perspective, dentists may be less willing to see children with IDD if they have inadequate training23,24 or offices that are ill-equipped to treat patients with IDD.25 Also, some dentists resist seeing children enrolled in public health insurance programs, such as Medicaid, because of insufficient reimbursement,26,27 additional administrative burdens,28 and patient behaviors such as frequent late cancellations or no-shows.29
It is reasonable to believe that these factors would combine to create access problems for children with IDD, but published studies have so far failed to identify significant differences in children's dental utilization on the basis of whether they have IDD. In a study based on data from the 1997 National Health Interview Survey, Schultz et al. reported that for children aged 2 to 17 years, those with a developmental disability were just as likely as those without a developmental disability to have seen a dentist in the previous 6 months (53% and 51%, respectively).30 A 2001 study reported that 82.5% of caregivers of children in the Iowa Supplemental Security Income program had no problems finding dental care for their child.31 In a more recent study, Chi et al. found no significant difference in the likelihood of preventive dental care utilization for Medicaid-enrolled children with and without IDD (P = .14) after adjusting for model covariates.32 Collectively, these findings suggest that children with IDD do not have worse access to dental services than do those with IDD.
However, these studies have 3 major limitations: (1) the lack of adjustment for overall health status, which assumes homogeneity in access to dental care for all children30–32; (2) a cross-sectional measure of utilization during a single calendar year, which fails to account for utilization over longer time periods30–32; and (3) no control group.31 No published study to date has investigated the relationship between IDD status and access to first dental visits for Medicaid-enrolled children while accounting for these limitations.
We used survival analytic techniques33 to compare the time to first dental visit for newly Medicaid-enrolled children with and without IDD and to identify the factors related to earlier first dental visit after enrollment in Medicaid. On the basis of the premise that Medicaid-enrolled children with IDD face more barriers to dental care access than children without IDD, we hypothesized that children with IDD would have a later first dental visit than would children without IDD. This research was a continuation of efforts to identify potential explanations for why publicly insured children have difficulties accessing dental care, and we intended our findings to form the basis for future clinical interventions and policies aimed at reducing pediatric oral health disparities for the most vulnerable child subgroup: those who have an IDD.
METHODS
Under an agreement with the Iowa Department of Human Services, we obtained Iowa Medicaid enrollment, medical claims, and dental claims files for calendar years 2005, 2006, and 2007. The Medicaid enrollment files included the patient's unique identification number (used to link the files), gender, age, county of residence, and zip code at baseline. We defined “baseline” as the month in 2005 in which the patient was first enrolled in Medicaid. We used the medical claims and enrollment files to determine the patient's IDD status. The dental claims files listed all dental services received by the patient. All recipient-level data were deidentified to ensure patient confidentiality.
We limited our analysis to newly enrolled children aged 3 to 8 years. To be considered newly enrolled, the child could not have been enrolled in the Medicaid program in the 12 months prior to baseline. We restricted the analyses to children aged 3 to 8 years because of the teeth expected to be present clinically in that age group, with most exhibiting primary (all baby teeth) or early mixed dentitions (mostly baby teeth along with newly erupted permanent incisors and first molars). We excluded children aged younger than 3 years because these enrollees tend to exhibit very low dental utilization and face different barriers to access related to their young age.34 These criteria resulted in a final cohort of 5391 children aged 3 to 8 years who were newly Medicaid-enrolled in 2005.
Measures
An oral health disparities model presented by Patrick et al.35 formed the conceptual framework for this study. We evaluated ascribed, proximal, immediate, intermediate, and distal factors as potential determinants of the time to first dental visit, with an emphasis on IDD status (yes/no) as the primary variable of interest. Our IDD identification methods consisted of a combination of categorical criteria (e.g., medical diagnosis) and other criteria (e.g., enrollment in programs designed specifically for children with IDD) described previously.32 We assembled a team of medical and dental child development specialists from the University of Iowa to develop these identification methods. The main criterion was evidence of a nonacquired cognitive deficit with a developmental etiology. The outcome variable was the time to first dental visit assessed over a maximum of 3 calendar years (2005, 2006, and 2007), measured as the month in which the child received his or her first dental service and on the basis of Current Dental Terminology code.36
In addition, we used Clinical Risk Grouping methods37 to assign each child to 1 of 9 hierarchical core health status groups: (1) healthy, (2) acute condition, (3) single minor chronic condition, (4) minor chronic in multiple systems, (5) single dominant or moderate chronic condition, (6) significant chronic disease in multiple systems, (7) dominant chronic in 3 or more systems, (8) dominant and metastatic malignancies, and (9) catastrophic condition. The group to which a child was assigned served as a proxy for the child's overall health status. Because of unequal distributions of children across the 9 groups, we created a 4-level categorical variable for the regression analyses (group 1, group 2, groups 3–4, and groups 5–9).
For each child, we gathered data on age at baseline, gender, and the total number of months the child was enrolled in Medicaid from baseline to the end of the study period (December 2007). We assessed whether the child had any primary medical care visits in 2005. We also created the following dichotomous variables measured at baseline: evidence of at least 1 other child from the same household enrolled in Medicaid, evidence of any Medicaid-enrolled adults in the child's household, and residence in a federally designated dental Health Professional Shortage Area (HPSA). A binary variable measured whether the child resided in a federally designed dental Health Professional Shortage Area (HPSA) and a 4-level variable measured the degree of urbanization of the county in which the child lived (on the basis of the US Department of Agriculture's Rural–Urban Continuum Codes38): metropolitan, urban adjacent to metropolitan, urban nonadjacent to metropolitan, and rural.
Analyses
After generating descriptive data for children with and without IDD, we used the log-rank test and Kaplan-Meier survival curves to compare the rates of first dental visits among the levels for the main independent variable and model covariates (unadjusted for other covariates). For the purposes of the survival analyses, data were censored when the child lost Medicaid eligibility or failed to have a visit by the end of the study period. We performed regression analyses using Cox regression methods. The proportional hazards assumption was tested with time-dependent covariates [covariate*log(time)]. Any violation of this assumption was handled by adding the log(time) by covariate interaction to the Cox regression model. We did not use a variable selection method because construction of the final regression model was based on an a priori conceptual model. The number of months of Medicaid enrollment was not included in the final model because enrollment could extend beyond the time at which the first dental visit took place, which would introduce conceptual problems related to temporality. All data were analyzed using the PROC LIFETEST and PROC TPHREG statements in SAS version 9.1 for Windows (SAS Institute, Cary, NC).39
RESULTS
About 1.8% of children aged 3 to 8 years in the Iowa Medicaid program in 2005 were identified as having IDD (Table 1). Children with IDD were enrolled in Medicaid for longer than were those without: more than 90% of children with IDD were enrolled for at least 25 months. The age distributions for both groups were similar, and about 94.8% of children with IDD had a primary medical care visit, whereas only 80.4% of children without IDD did. Larger proportions of children without IDD had another child or adult from the same household also enrolled in Medicaid and lived in a dental HPSA.
TABLE 1.
Newly Medicaid-Enrolled Children Aged 3–8 Years: Iowa, 2005
| Variable | Children With an IDD (n = 96), No. (%) or Mean ±SD | Children Without an IDD (n = 5295), No. (%) or Mean ±SD | Total Study Population (N = 5391), No. (%) or Mean ±SD |
| Ascribed factors | |||
| Clinical Risk Group | |||
| Healthy | 40 (41.7) | 4304 (81.3) | 4344 (80.6) |
| Acute condition | 7 (7.3) | 427 (8.1) | 434 (8.1) |
| Single minor chronic condition | 7 (7.3) | 220 (4.2) | 227 (4.2) |
| Minor chronic in multiple systems | 0 (0.0) | 2 (< 0.1) | 2 (< 0.1) |
| Single dominant or moderate chronic condition | 27 (28.1) | 289 (5.5) | 316 (5.9) |
| Significant chronic disease in multiple systems | 12 (12.5) | 47 (0.9) | 59 (1.1) |
| Dominant chronic in 3 or more systems | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Dominant and metastatic malignancies | 0 (0.0) | 3 (0.1) | 3 (0.1) |
| Catastrophic condition | 3 (3.1) | 3 (0.1) | 6 (0.1) |
| Age, y | |||
| Mean ±SD | 5.3 ±1.7 | 5.2 ±1.7 | 5.2 ±1.7 |
| 3 | 20 (20.8) | 1056 (19.9) | 1076 (20.0) |
| 4 | 17 (17.7) | 1032 (19.5) | 1049 (19.5) |
| 5 | 16 (16.7) | 938 (17.7) | 854 (17.7) |
| 6 | 18 (18.8) | 803 (15.2) | 821 (15.2) |
| 7 | 11 (11.5) | 755 (14.3) | 766 (14.2) |
| 8 | 14 (14.6) | 711 (13.4) | 725 (13.4) |
| Gender | |||
| Female | 31 (32.3) | 2612 (49.3) | 2643 (49.0) |
| Male | 65 (67.7) | 2683 (50.7) | 2748 (51.0) |
| Total length of Medicaid enrollment, mo | |||
| Mean ±SD | 41.3 ±8.2 | 30.0 ±13.5 | 30.2 ±13.5 |
| 6 | 0 (0.0) | 99 (1.9) | 99 (1.8) |
| 7–12 | 1 (1.0) | 902 (17.0) | 903 (16.8) |
| 13–24 | 7 (7.3) | 1008 (19.0) | 1015 (18.8) |
| 25–36 | 88 (91.7) | 3286 (62.1) | 3374 (62.6) |
| Proximal factor | |||
| Any primary medical care visits by child in 2005 (yes) | 91 (94.8) | 4259 (80.4) | 4350 (80.7) |
| Immediate factors | |||
| At least one Medicaid-enrolled child in the household (yes) | 37 (38.5) | 4241 (80.1) | 4278 (79.4) |
| At least one Medicaid-enrolled adult in the household (yes) | 21 (21.9) | 2889 (54.6) | 2910 (54.0) |
| Intermediate factors | |||
| Degree of rurality of child's county of residence | |||
| Metropolitan | 67 (69.8) | 2950 (55.7) | 3017 (56.0) |
| Urban adjacent to metropolitan | 13 (13.5) | 1041 (19.7) | 1054 (19.6) |
| Urban nonadjacent to metropolitan | 13 (13.5) | 995 (18.8) | 1008 (18.7) |
| Rural | 3 (3.1) | 309 (5.8) | 312 (5.8) |
| Distal factor | |||
| Resides in a dental HPSA (yes) | 51 (53.1) | 3385 (63.9) | 3436 (63.7) |
Note. HPSA = Health Professional Shortage Area; IDD = intellectual or developmental disability.
Dental Utilization
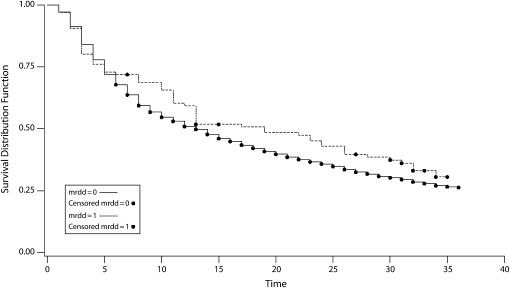
Table 2 displays the cumulative proportions of children with a first dental visit at specified time intervals unadjusted for covariates but adjusted for censoring. About 32% had a first dental visit within 6 months of enrollment; this proportion increased to 49%, 64%, and 74% by years 1, 2, and 3, respectively. After 6 months, the proportion of children without a dental visit remained higher for children with IDD than for those without IDD (Figure 1), although these differences did not reach statistical significance (P = .22). Among all children who had their first dental visit within 6 months of enrollment, those with no primary medical care visit were the smallest group (22%); the corresponding rate was about 35% for those with a primary medical care visit.
TABLE 2.
Cumulative Proportions of Children Aged 3–8 Years With a First Dental Visit at Specified Time Intervals, After Medicaid Enrollment in 2005: Iowa, 2005–2007
| First Dental Visitaa |
||||||
| Variable | No. (%) | 6 Months | 1 Years | 2 Years | 3 Years | Pb |
| All children | 5391 (100) | 0.32 | 0.49 | 0.64 | 0.74 | … |
| Identified with an IDD | ||||||
| Yes | 96 (1.8) | 0.28 | 0.41 | 0.57 | 0.69 | .22 |
| No | 5295 (98.2) | 0.32 | 0.49 | 0.64 | 0.74 | … |
| Clinical Risk Group | ||||||
| Healthy | 4344 (80.6) | 0.31 | 0.48 | 0.63 | 0.73 | .01 |
| Acute condition | 434 (8.1) | 0.38 | 0.53 | 0.69 | 0.77 | … |
| Single minor chronic condition | 227 (4.2) | 0.35 | 0.53 | 0.70 | 0.79 | … |
| Minor chronic in multiple systems | 2 (< 0.1) | 0.00 | 0.00 | 1.00 | 1.00 | … |
| Single dominant or moderate chronic condition | 316 (5.9) | 0.34 | 0.52 | 0.70 | 0.78 | |
| Significant chronic disease in multiple systems | 59 (1.1) | 0.36 | 0.49 | 0.58 | 0.65 | … |
| Dominant chronic in 3 or more systems | 0 (0.0) | … | … | … | … | |
| Dominant and metastatic malignancies | 3 (0.1) | 0.33 | 0.33 | 0.33 | 0.33 | … |
| Catastrophic condition | 6 (0.1) | 0.33 | 0.67 | 0.67 | 0.67 | … |
| Age, y | ||||||
| 3–5 | 3079 (57.1) | 0.31 | 0.48 | 0.64 | 0.73 | .13 |
| 6–8 | 2312 (42.9) | 0.34 | 0.50 | 0.65 | 0.74 | … |
| Gender | ||||||
| Boy | 2748 (51.0) | 0.31 | 0.47 | 0.63 | 0.74 | .13 |
| Girl | 2643 (49.0) | 0.33 | 0.51 | 0.65 | 0.74 | … |
| Total length of Medicaid enrollment, mo | ||||||
| 1–6 | 99 (1.8) | 0.26 | … | … | … | …c |
| 7–12 | 903 (16.8) | 0.35 | 0.44 | … | … | … |
| 13–24 | 1015 (18.8) | 0.29 | 0.48 | 0.64 | … | … |
| 25–36 | 3374 (62.6) | 0.32 | 0.50 | 0.65 | 0.74 | … |
| Proximal factors | ||||||
| Any primary medical care visits by child in 2005 | ||||||
| Yes | 4350 (80.7) | 0.35 | 0.52 | 0.67 | 0.77 | .001 |
| No | 1041 (19.3) | 0.22 | 0.37 | 0.53 | 0.70 | … |
| At least one Medicaid-enrolled child in the household | ||||||
| Yes | 4278 (79.4) | 0.32 | 0.49 | 0.65 | 0.74 | .51 |
| No | 1113 (20.6) | 0.32 | 0.48 | 0.62 | 0.74 | … |
| Immediate factor | ||||||
| At least one Medicaid-enrolled adult in the household | ||||||
| Yes | 2910 (54.0) | 0.30 | 0.47 | 0.63 | 0.74 | .02 |
| No | 2481 (46.0) | 0.34 | 0.51 | 0.65 | 0.74 | … |
| Intermediate factor | ||||||
| Degree of rurality of child's county of residence | ||||||
| Metropolitan | 3017 (56.0) | 0.34 | 0.51 | 0.66 | 0.76 | .001 |
| Urban adjacent to metropolitan | 1054 (19.6) | 0.28 | 0.45 | 0.61 | 0.73 | … |
| Urban nonadjacent to metropolitan | 1008 (18.7) | 0.31 | 0.46 | 0.62 | 0.69 | … |
| Rural | 312 (5.8) | 0.33 | 0.50 | 0.62 | 0.69 | … |
| Distal factor | ||||||
| Resides in a dental HPSA | ||||||
| Yes | 3436 (63.7) | 0.32 | 0.49 | 0.63 | 0.72 | .07 |
| No | 1955 (36.3) | 0.33 | 0.49 | 0.66 | 0.76 | … |
Note. HPSA = Health Professional Shortage Area; IDD = intellectual or developmental disability. Elipses indicate results were not applicable.
From Kaplan-Meier survival curves (adjusted for censoring of data).
P value for comparison within categories; univariate log-rank test results for each covariate (unadjusted for other covariates).
Significance testing not reported because enrollment could extend beyond the time at which the first dental visit took place.
FIGURE 1.
KaplanMeier survival curves for newly Medicaid-enrolled children with and without an intellectual or developmental disability (IDD), and the time to first dental visit, in months: Iowa, 2005–2007.
Note. mrdd = mental retardation and developmental disability Log-rank test: P = .22. The dashed line represents children with IDD; the solid line, children without IDD.
Cox Regression Model
Table 3 presents results from the multiple-variable Cox regression model. Because one covariate—whether the child had a primary medical care visit—violated the proportional hazards assumption, we included this variable in the Cox regression model as a time-dependent covariate. We also tested for a potential interaction between the child and adult Medicaid enrollee variables and did not find evidence of a significant interaction (P = .56).
TABLE 3.
Final Cox Regression Model With Time-Dependent Covariate for Time to First Dental Visit for Children Aged 3–8 Years (N = 5391), After Medicaid Enrollment in 2005: Iowa, 2005–2007
| Covariate | AHR (95% CI) | Pa |
| Main independent variable | ||
| Identified with an IDD | ||
| Yes | 0.69 (0.31, 0.99) | .04 |
| No (Ref) | 1.00 | … |
| Ascribed factors | ||
| Clinical Risk Group | ||
| Healthy (1) (Ref) | 1.00 | … |
| Acute (2) | 1.14 (1.01, 1.29) | .032 |
| Chronic (3, 4) | 1.11 (0.95, 1.30) | .2 |
| Chronic (5-9) | 1.08 (0.95, 1.23) | .235 |
| Age, y | ||
| 3–5 (Ref) | 1.00 | … |
| 6–8 | 1.10 (1.03, 1.18) | .006 |
| Gender | ||
| Girl | 1.05 (0.98, 1.11) | .14 |
| Boy (Ref) | 1.00 | … |
| Proximal factor | ||
| Child had any primary medical care visit | ||
| Yes | 1.51 (1.38, 1.61) | .001 |
| No (Ref) | 1.00 | … |
| Time-dependent covariate: Primary medical care visit*log(time) | 0.87 (0.78, 0.96) | .009 |
| Immediate factors | ||
| At least one Medicaid-enrolled child in the household | ||
| Yes | 1.08 (1.00, 1.16) | .045 |
| No (Ref) | 1.00 | … |
| At least one Medicaid-enrolled adult in the household | ||
| Yes | 0.89 (0.81, 0.96) | .003 |
| No (Ref) | 1.00 | … |
| Intermediate factor | ||
| Degree of rurality of child's county of residence | ||
| Metropolitan (Ref) | 1.00 | … |
| Urban adjacent to metropolitan | 0.83 (0.76, 0.91) | .001 |
| Urban nonadjacent to metropolitan | 0.84 (0.76, 0.92) | .001 |
| Rural | 0.90 (0.78, 1.05) | .167 |
| Distal factor | ||
| Resides in a dental HPSA | ||
| Yes | 0.92 (0.83, 0.99) | .028 |
| No (Ref) | 1.00 | … |
Note. AHR = adjusted hazard ratio; CI = confidence interval; IDD = intellectual or developmental disability; HPSA = federally designated Health Professional Shortage Area; N/A = not applicable.
α = .05.
After adjusting for covariates, we found that newly Medicaid-enrolled children with IDD were 31% less likely to have had an earlier first dental visit than those without IDD (P = .04). Children with an acute condition were 14% more likely than healthy children to have earlier first dental visits. There was no significant difference in timing of first dental visits between healthy children and those with any chronic condition. Children aged 6 to 8 years were significantly more likely to have had earlier first dental visits than those aged 3 to 5 years (P < .01).
Children with a primary medical care visit were 1.5 times more likely to have had an earlier first dental visit (95% confidence interval [CI] = 1.38, 1.61; P < .001) than were those without a primary medical care visit, although the impact of this variable decreased over time (P = .009). In other words, the benefits associated with primary medical care visits appeared to be stronger initially and to decline with time. There were no significant differences in the time to first dental visit by gender. Children with another Medicaid-enrolled child in the same household were 8% more likely to have had an earlier first dental visit (adjusted hazard ratio [AHR] = 1.08; 95% CI = 1.00, 1.16; P = .045), whereas those with a Medicaid-enrolled adult in the same household were 11% less likely to have had an earlier first dental visit (AHR = 0.89; 95% CI = 0.81, 0.96; P = .003). Children in nonmetropolitan areas were generally less likely to have had earlier first dental visits, as were those who lived in a dental HPSA.
DISCUSSION
This is the first published study to examine the time to first dental visit for newly Medicaid-enrolled children with and without IDD. From a public health perspective, not only do earlier first dental visits provide an opportunity to prevent disease; they also may result in less invasive and less costly interventions when treatment is required. Our findings suggest that newly Medicaid-enrolled children with IDD were significantly less likely to have had earlier first dental visits than those without IDD. In addition, other factors—such as age, primary medical care visits, family structure, and not living in a dental HPSA—were also associated with earlier first dental visits. Our study has 3 main strengths: (1) use of both diagnosis-based and non-diagnosis-based case-finding criteria to identify children with and without IDD, (2) an assessment of utilization over multiple years, and (3) adjustment for overall health status.
Compared with previous findings reported by Damiano et al., the proportion of children in our study with a first dental visit within 6 months of enrollment (0.32) was similar to the rates for newly enrolled children in the Iowa Separate State Children's Health Insurance Program (S-SCHIP) 2 or S-SCHIP 3 dental plans (0.30–0.36), which offer more generous reimbursement rates.40 In addition, the proportion of children in our study with a first dental visit within 6 months of enrollment was higher than that of children enrolled in the less generous S-SCHIP 1 dental plan or Medicaid dental program (0.21–0.23). Furthermore, the cumulative year 1 utilization rate from our study (0.49) was 7 points higher than the rate reported for newly Medicaid-enrolled children aged younger than 19 years in the Damiano et al. study (0.42). One explanation for this difference is that our study focused on children in groups that typically have higher rates of dental utilization.32 In light of the potential for overestimated utilization rates, we can surmise that our cumulative 3-year rate for children in the Medicaid program was lower than that for new SCHIP enrollees in Damiano et al.40 This is consistent with previous findings by Brickhouse et al. that Medicaid-enrolled children had worse access to dental care than their SCHIP-enrolled counterparts.41
There are no other studies in the literature to which our results could be compared. In the context of available studies, our findings suggest that although short-term utilization for children enrolled in Medicaid was similar to that of SCHIP enrollees, in the long term, children in Medicaid were less likely to use dental care.
We see 3 possible explanations for the difference in time to first dental visit for children by IDD status. (1) Caregivers of children with IDD may have difficulties finding a dentist willing to see their child, which could lead to delayed first dental visits. (2) Caregivers of children with IDD, many of whom see a health care professional, may receive inconsistent information on when the first dental visit should take place, which could lead to confusion. (3) Children with IDD may have other medical problems that require more immediate attention than oral health. These factors suggest that improving access to dental care for children with IDD will require interventions that focus on caregivers as well as dentists and other medical professionals.
After adjusting for other factors, we found that children aged 6 to 8 years were more likely to have earlier first dental visits than children aged 3 to 5 years. Dentists may be more willing to see older children because they are easier to manage in the office. An equally plausible explanation is that older children have greater unmet demand for dental care. In other words, among children newly enrolled in Medicaid, an older child might access dental care sooner than a younger child because of higher levels of accumulated disease and greater perceived need for care. However, the types of treatment required by older children are likely to be more costly and invasive.42 Given the cumulative nature of dental caries, one way to reduce pent-up demand for care in the long term is to ensure proper access to earlier first dental visits and to provide appropriate preventive dental care for high-risk children.43
We found that primary medical care visits were related to earlier first dental visits, which is consistent with previous work.32,44 Selection bias cannot be ruled out as an alternative explanation for this finding, but it appears that children who access prevention-oriented medical care are more likely to exhibit desirable dental utilization patterns. Pediatricians, family practice physicians, and other health care professionals play a critical role in reinforcing positive behaviors related to oral health, performing oral health screenings, delivering appropriate preventive dental care, and referring children to a dentist by age 12 months.45–52 Thus, medical visits are a potential conduit through which a publicly insured child's access to earlier first dental visits can be improved. We expect future research to further clarify the relationship between the timing and frequency of specific types of medical care use and dental utilization.
Also consistent with previous findings is the significance of family-structure variables (e.g., whether there was another child or adult also enrolled in Medicaid).32 The positive relationship between having multiple children from the same household enrolled in Medicaid and earlier first dental visits is an indication that the caregivers for these children may have an easier time coordinating dental appointments. Furthermore, caregivers of a child with a history of dental disease and treatment might be more inclined to take younger siblings in for earlier first dental visits, to avoid caries-related morbidities. The negative relationship we observed between the adult variable and dental utilization suggests that these households have life stressors that make it difficult for caregivers to take their children in for earlier first dental visits. What our data do not tell us is the adults’ Medicaid enrollment status at or near the time of the children's first dental visit. Given the relationship between access to dental care for children and caregivers, a child with a caregiver who lost eligibility at a critical time may have missed an opportunity to visit the dentist. Enrolling adults from households with a Medicaid-enrolled child reduces the likelihood of the child losing Medicaid benefits,53 which might ensure adequate access to dental care for the entire household.
Finally, our results suggest that children living in a dental HPSA and in nonmetropolitan areas were less likely to have earlier first dental visits. These findings are not surprising, given that HPSAs are regions with a limited number or maldistribution of dentists. Children living in a dental HPSA or in rural areas may have to travel longer distances to access dental care, which requires reliable transportation; also, a caregiver often must take time off from work. These findings indicate the need for policies aimed at increasing the number of dentists practicing in dental HPSAs through incentives such as student loan forgiveness.
Collectively, our results support the conceptual model of oral health disparities by Patrick et al., which proposes that ascribed, proximal, immediate, intermediate and distal factors are important determinants of access to dental care.35 Variables from all 5 conceptual domains were significantly associated with the time to first dental visit for newly Medicaid-enrolled children in our sample. This suggests that the determinants of first dental visits are complex and operate at multiple levels. Given the complexity of dental care access, future interventions and research will need to focus on multilevel models and analytic methods. Given the magnitude of the hazard ratios, it appeared that previous access to primary medical care, a distal factor, was the most important determinant of earlier first dental visits for Medicaid-enrolled children aged 3 to 8 years. The relationship between medical and dental care utilization has implications for the development of medical office-based clinical interventions aimed at increasing access to dental care services for publicly insured children.
This study has a number of limitations. First, the generalizability of our findings is limited to children aged 3 to 8 years who were newly enrolled in Medicaid. We focused our study on younger children because this is a time when dental care has both immediate benefits and benefits that can last throughout childhood.54,55 Children with IDD, on average, require intensive, costly medical care,56 which means that most are enrolled in Medicaid from a young age so they can access these services. Second, our definition of baseline did not allow us to account for children who moved after baseline. Housing instability makes it difficult to establish and maintain a dental home, a potentially problematic phenomenon for Medicaid-enrolled households. Future studies might examine this issue with a fluid model that takes into account changes in the place of residence.
Third, it is possible that we overestimated the proportion of children without a visit within 3 years (25%) because a child could have accessed dental care through private dental insurance provided by a caregiver. Fourth, we were unable to include in our models the behavioral determinants of access, which are critical in the oral health disparities model by Patrick et al.35 This limitation can be addressed in the future by collecting data from caregivers and dentists and linking these data to dental claims files. Finally, the lack of clinical data prevented us from assessing the level of unmet dental need, another limitation that should be addressed in future investigations.
In conclusion, the results of this study suggest a significant difference in the time to first dental visit for newly enrolled IDD and non-IDD children in the Iowa Medicaid program. Other factors, such as primary medical care visits, older age, family structure, and not living in a dental HPSA, were significantly associated with earlier first dental visits.
What is most worrisome is that after 3 years, 1 in 4 children failed to access any dental care. This brings attention to a larger problem: all Medicaid-enrolled children encounter barriers to access. Although dental visits are not a panacea for reducing oral health disparities, they are an important part of ensuring optimal oral health, especially if these visits are timed appropriately. Future research efforts should focus on identifying the behavior-related determinants of first dental visits, especially from caregivers and dentists. This information can then be used to develop clinical interventions and policies aimed at improving access to earlier first dental visits and eliminating disparities in access to dental care for all Medicaid-enrolled children.
Acknowledgments
We would like to thank the 3M Corporation for providing a no-cost research license for the Clinical Risk Grouping software. This study was supported by the National Institutes of Health/National Institute of Dental and Craniofascial Research (grants T32-DE014678-06 and K08-DE020856) and by funding from the Iowa Department of Human Services.
Human Participant Protection
This study protocol was approved by the institutional review board of the University of Iowa.
References
- 1.Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001 [PubMed] [Google Scholar]
- 2.Roberts MW. Dental health of children: where we are today and remaining challenges. J Clin Pediatr Dent. 2008;32(3):231–234 [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Dept of Health and Human Services; 2000 [Google Scholar]
- 4.American Academy on Pediatric Dentistry Clinical Affairs Committee—Infant Oral Health Subcommittee; American Academy on Pediatric Dentistry Council on Clinical Affairs Guideline on infant oral health care. Pediatr Dent. 2008–2009;30(7 suppl):90–93 [PubMed] [Google Scholar]
- 5.American Academy of Pediatric Dentistry Council on Clinical Affairs Policy on use of a caries-risk assessment tool (CAT) for infants, children, and adolescents. Pediatr Dent. 2005–2006;27(7 suppl):25–27 [PubMed] [Google Scholar]
- 6.Nowak AJ, Casamassimo PS. Using anticipatory guidance to provide early dental intervention. J Am Dent Assoc. 1995;126(8):1156–1163 [DOI] [PubMed] [Google Scholar]
- 7.Sanchez OM, Childers NK. Anticipatory guidance in infant oral health: rationale and recommendations. Am Fam Physician. 2000;61(1):115–120, 123–124 [PubMed] [Google Scholar]
- 8.Hale KJ. American Academy of Pediatrics Section on Pediatric Dentistry. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5, pt 1):1113–1116 [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Pediatric Dentistry Clinical Affairs Committee, American Academy of Pediatric Dentistry Council on Clinical Affairs Guideline on periodicity of examination, preventive dental services, anticipatory guidance, and oral treatment for children. Pediatr Dent. 2005–2006;27(7 suppl):84–86 [PubMed] [Google Scholar]
- 10.Ramseier CA, Leiggener I, Lang NP, Bagramian RA, Inglehart MR. Short-term effects of hygiene education for preschool (kindergarten) children: a clinical study. Oral Health Prev Dent. 2007;5(1):19–24 [PubMed] [Google Scholar]
- 11.Livny A, Vered Y, Slouk L, Sgan-Cohen HD. Oral health promotion for schoolchildren—evaluation of a pragmatic approach with emphasis on improving brushing skills. BMC Oral Health. 2008;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naidoo S, Myburgh N. Nutrition, oral health and the young child. Matern Child Nutr. 2007;3(4):312–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kasila K, Poskiparta M, Kettunen T, Pietila I. Variation in assessing the need for change of snacking habits in schoolchildren's oral health counselling. Int J Paediatr Dent. 2008;18(2):107–116 [DOI] [PubMed] [Google Scholar]
- 14.Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care-seeking for children's oral health among low-income caregivers. Am J Public Health. 2005;95(8):1345–1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akpabio A, Klausner CP, Inglehart MR. Mothers’/guardians’ knowledge about promoting children's oral health. J Dent Hyg. 2008;82(1):12. [PubMed] [Google Scholar]
- 16.Azarpazhooh A, Main PA. Pit and fissure sealants in the prevention of dental caries in children and adolescents: a systematic review. J Can Dent Assoc. 2008;74(2):171–177 [PubMed] [Google Scholar]
- 17.Azarpazhooh A, Main PA. Fluoride varnish in the prevention of dental caries in children and adolescents: a systematic review. J Can Dent Assoc. 2008;74(1):73–79 [PubMed] [Google Scholar]
- 18.Miller EK, Vann WF., Jr The use of fluoride varnish in children: a critical review with treatment recommendations. J Clin Pediatr Dent. 2008;32(4):259–264 [DOI] [PubMed] [Google Scholar]
- 19.Gibson TJ, Nash DA. Practice patterns of board-certified pediatric dentists: frequency and method of cleaning children's teeth. Pediatr Dent. 2004;26(1):17–22 [PubMed] [Google Scholar]
- 20.Nainar SM, Redford-Badwal DA. Survey of dental prophylaxes rendered by pediatric dentists in New England. J Contemp Dent Pract. 2004;5(4):14–22 [PubMed] [Google Scholar]
- 21.Feigal RJ, Jensen ME, Mensing CA. Dental caries potential of liquid medications. Pediatrics. 1981;68(3):416–419 [PubMed] [Google Scholar]
- 22.Ferguson Fs, Cinotti D. Home oral health practice: the foundation for desensitization and dental care for special needs. Dent Clin North Am. 2009;53(2):375–387, xi [DOI] [PubMed] [Google Scholar]
- 23.Casamassimo PS, Seale NS, Ruehs K. General dentists’ perceptions of educational and treatment issues affecting access to care for children with special health care needs. J Dent Educ. 2004;68(1):23–28 [PubMed] [Google Scholar]
- 24.Wolff AJ, Waldman HB, Milano M, Perlman SP. Dental students’ experiences with and attitudes toward people with mental retardation. J Am Dent Assoc. 2004;135(3):353–357 [DOI] [PubMed] [Google Scholar]
- 25.Finger ST, Jedrychowski JR. Parents’ perception of access to dental care for children with handicapping conditions. Spec Care Dentist. 1989;9(6):195–199 [DOI] [PubMed] [Google Scholar]
- 26.Nainar SM. Dentists’ ranking of Medicaid reimbursement rates as a measure of their pediatric Medicaid participation. ASDC J Dent Child. 2000;67(6):422–424 [PubMed] [Google Scholar]
- 27.Mayer ML, Stearns SC, Norton EC, Rozier RG. The effects of Medicaid expansions and reimbursement increases on dentists’ participation. Inquiry. 2000;37(1):33–44 [PubMed] [Google Scholar]
- 28.Al Agili DE, Pass M, Bronstein J, Lockwood S. Medicaid participation by private dentists in Alabama. Pediatr Dent. 2007;29(4):293–302 [PubMed] [Google Scholar]
- 29.Iben P, Kanellis MJ, Warren J. Appointment-keeping behavior of Medicaid-enrolled pediatric dental patients in eastern Iowa. Pediatr Dent. 2000;22(4):325–329 [PubMed] [Google Scholar]
- 30.Schultz ST, Shenkin JD, Horowitz AM. Parental perceptions of unmet dental need and cost barriers to care for developmentally disabled children. Pediatr Dent. 2001;23(4):321–325 [PubMed] [Google Scholar]
- 31.Slayton RL, Damiano PC, Willard JC. Perceived dental needs of children enrolled in Iowa's Medicaid Supplemental Security Income (SSI) health plan. ASDC J Dent Child. 2001;68(3):206–210 [PubMed] [Google Scholar]
- 32.Chi DL, Momany ET, Kuthy RA, Chalmers JM, Damiano PC. Preventive dental utilization for Medicaid-enrolled children in Iowa identified with intellectual and/or developmental disability. J Public Health Dent. 2010;70(1):35–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Virnig BA, Ash A, Kind S, Mesler DE. Survival analysis using Medicare data: example and methods. Health Serv Res. 2000;35(5, pt 3):86–101 [PMC free article] [PubMed] [Google Scholar]
- 34.Kanellis MJ, Damiano PC, Momany ET. Utilization of dental services by Iowa Medicaid-enrolled children younger than 6 years old. Pediatr Dent. 1997;19(5):310–314 [PubMed] [Google Scholar]
- 35.Patrick DL, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6(suppl 1):S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Dental Association Current Dental Terminology 2005. Chicago, IL: American Dental Association; 2005 [Google Scholar]
- 37.Hughes JS, Averill RF, Eisenhandler J, et al. Clinical Risk Groups (CRGs): a classification system for risk-adjusted capitation-based payment and health care management. Med Care. 2004;42(1):81–90 [DOI] [PubMed] [Google Scholar]
- 38.US Department of Agriculture Economic Research Service Rural-urban continuum codes. Available at: http://www.ers.usda.gov/Data/RuralUrbanContinuumCodes. Updated November 3, 2004. Accessed October 8, 2010
- 39.SAS [computer program] Version 9.1 Cary, NC: SAS Institute; 2002–2003 [Google Scholar]
- 40.Damiano P, Momany ET, Carter KD, Jones MP, Askelson NM. Time to first dental visit after initially enrolling in Medicaid and S-SCHIP. Med Care. 2008;46(12):1234–1239 [DOI] [PubMed] [Google Scholar]
- 41.Brickhouse TH, Rozier RG, Slade GD. The effect of two publicly funded insurance programs on use of dental services for young children. Health Serv Res. 2006;41(6):2033–2053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nainar SM, Crall JJ. Caries experience in inner-city preschoolers at the time of their initial dental visit. ASDC J Dent Child. 1997;64(6):421–424 [PubMed] [Google Scholar]
- 43.Maurer SM, Boggs AM, Mourino AP, Farrington FH. Recall intervals: effect on treatment needs of the handicapped patient: a retrospective study. J Clin Pediatr Dent. 1996;20(2):123–126 [PubMed] [Google Scholar]
- 44.Milgrom P, Mancl L, King B, Weinstein P, Wells N, Jeffcott E. An explanatory model of the dental care utilization of low-income children. Med Care. 1998;36(4):554–566 [DOI] [PubMed] [Google Scholar]
- 45.Caspary G, Krol DM, Boulter S, Keels MA, Romano-Clarke G. Perceptions of oral health training and attitudes toward performing oral health screenings among graduating pediatric residents. Pediatrics. 2008;122(2):e465–e471 [DOI] [PubMed] [Google Scholar]
- 46.Clemmens DA, Kerr AR. Improving oral health in women: nurses’ call to action. MCN Am J Matern Child Nurs. 2008;33(1):10–14, quiz 15–16 [DOI] [PubMed] [Google Scholar]
- 47.dela Cruz GG, Rozier RG, Slade G. Dental screening and referral of young children by pediatric primary care providers. Pediatrics. 2004;114(5):e642–e652 [DOI] [PubMed] [Google Scholar]
- 48.Douglass JM, Douglass AB, Silk HJ. Infant oral health education for pediatric and family practice residents. Pediatr Dent. 2005;27(4):284–291 [PubMed] [Google Scholar]
- 49.Krol DM. Educating pediatricians on children's oral health: past, present, and future. Pediatrics. 2004;113(5):e487–e492 [DOI] [PubMed] [Google Scholar]
- 50.Lewis CW, Grossman DC, Domoto PK, Deyo RA. The role of the pediatrician in the oral health of children: a national survey. Pediatrics. 2000;106(6):E84. [DOI] [PubMed] [Google Scholar]
- 51.Schafer TE, Adair SM. Prevention of dental disease: the role of the pediatrician. Pediatr Clin North Am. 2000;47(5):1021–1042, v-vi [DOI] [PubMed] [Google Scholar]
- 52.Slade GD, Rozier RG, Zeldin LP, Margolis PA. Training pediatric health care providers in prevention of dental decay: results from a randomized controlled trial. BMC Health Serv Res. 2007;7:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sommers BD. Insuring children or insuring families: do parental and sibling coverage lead to improved retention of children in Medicaid and CHIP? J Health Econ. 2006;25(6):1154–1169 [DOI] [PubMed] [Google Scholar]
- 54.Savage MF, Lee JY, Kotch JB, Vann WF., Jr Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114(4):e418–e423 [DOI] [PubMed] [Google Scholar]
- 55.Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. Am J Public Health. 1992;82(12):1663–1668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vladeck BC. Where the action really is: Medicaid and the disabled. Health Aff (Millwood). 2003;22(1):90–100 [DOI] [PubMed] [Google Scholar]