Abstract
PURPOSE
The aim of this study was to identify in vitro antimicrobial activity of the tissue conditioner containing silver nanoparticles on microbial strains, Staphylococcus aureus, Streptococcus mutans and Candida albicans.
MATERIALS AND METHODS
Experimental disc samples (20.0×3.0 mm) of tissue conditioner (GC Soft-Liner, GC cooperation, Tokyo, Japan) containing 0.1 - 3.0% silver nanoparticles (0%: control) were fabricated. Samples were placed on separate culture plate dish and microbial suspensions (100 µL) of tested strains were inoculated then incubated at 37℃. Microbial growth was verified at 24 hrs and 72 hrs and the antimicrobial effects of samples were evaluated as a percentage of viable cells in withdrawn suspension (100 µL). Data were recorded as the mean of three colony forming unit (CFU) numerations and the borderline of the antimicrobial effect was determined at 0.1% viable cells.
RESULTS
A 0.1% silver nanoparticles combined to tissue conditioner displayed minimal bactericidal effect against Staphylococcus aureus and Streptococcus mutans strains, a 0.5% for fungal strain. Control group did not show any microbial inhibitory effect and there were no statistical difference between 24 hrs and extended 72 hrs incubation time (P > .05).
CONCLUSION
Within the limitation of this in vitro study, the results suggest that the tissue conditioner containing silver nanoparticles could be an antimicrobial dental material in denture plaque control. Further mechanical stability and toxicity studies are still required.
Keywords: Silver nanoparticles, Tissue conditioner, Antimicrobial effect
INTRODUCTION
Tissue conditioners have been commonly used to enhance the recovery of denture-bearing tissues from trauma, damage or residual ridge resorption usually caused by ill-fitting dentures. However, these materials are degenerated with time and are easily degradable and occasionally are susceptible to colonization by microorganisms.1 Microbial growth results from the adherence of microbial cells are promoted by rough surface, and from adhesive interactions between Candida species and oral bacteria, mostly Candida albicans and oral streptococci.2,3 Moreover, Staphylococcus aureus, giving rise to pharyngeal and respiratory infections, has been isolated from dentures and the oral cavity in elderly patients with decreased immunological activity.4,5 Therefore, the maintenance of tissue conditioners and the prevention of the accumulation of microorganisms on such materials are of great importance. Tissue conditioners could be kept clean by mechanical and chemical methods. However, it is also known that these methods can cause considerable damage to tissue conditioners6,7 and to some geriatric or hospitalized patients, even denture cleansing might be compromised owing to cognitive impairment, reduced motor dexterity and memory loss. Systemic or local antibiotic agents have been prescribed for eliminating the bacterial population, however, with microbial resistance and the health-care costs being surged, the researching on antimicrobial denture base or lining material is needed for its prevention and care.8,9 Several in vitro and in vivo studies have shown the beneficial effects of antimicrobial agents combined in tissue conditioners.10-12 However, bacteria may induce stomatitis13,14 and no potentially effective and persistent antimicrobial agent to be incorporated has been developed.
Silver (Ag) has been well known for its antimicrobial characteristic and has a long history15 of application in medicine with a well tolerated tissue response and low toxicity profile and it is more toxic than many other metals against a broad spectrum of sessile bacteria and fungi which colonize on plastic surface.16,17 Such characteristics have led to drawing an attention recently due to the emergence of antibiotic resistant bacteria as a result of overuse of antibiotics and far lower propensity to induce microbial resistance than antibiotics. Silver containing materials are already used as prostheses, such as the technology of central venous catheter, vascular graft and wound dressing.18,19 Particularly, silver nanoparticles (Ag°), the nano-sized (nm) inorganic particle form of silver, with its rapid and broad-spectrum efficacy and its sustained silver cation (Ag+) release18,19 appears to be more effective means of prophylaxis than micro-sized silver powder (µm) which shows lower antimicrobial activity owing to its limited surface.19,20
The objectives of present study were to examine in vitro: (i) the antimicrobial effect of the modified tissue conditioner containing silver nanoparticles towards nosocomial respiratory infection-causing bacteria, Staphylococcus aureus (S. aureus), oral endogenous bacteria Streptococcus mutans (S. mutans) and a fungal species associated with denture stomatitis, Candida albicans (C. albicans) and (ii) the dose of silver nanoparticles necessary to obtain as the antiseptic material.
MATERIALS AND METHODS
1. Preparation of silver nanoparticles
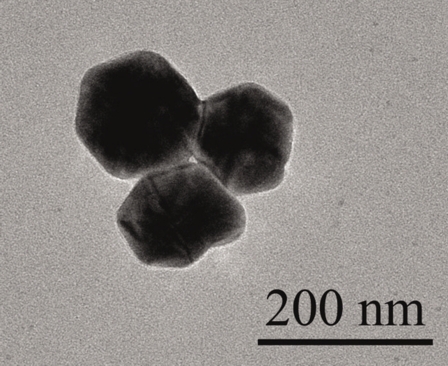
Ag° was prepared as the following the procedure. Aqueous silver sol was prepared with 10.0 mM of analytical grade AgNO3 in distilled water and 2.0% PVP (Polyvinyl Pyrrolidon) was used as stabilizer. All solutions were deaerated by bubbling with argon gas for 1 hour and then they were irradiated in the field of 20 KGy 60Co Gamma-ray sources. The image of prepared Ag° was shown through the TEM (Transmission Electron Microscope) view (Fig. 1).
Fig. 1.
TEM view of a prepared Ag° used in this study. The average size of nano particles was approximately 100 - 120 nm.
2. Sample fabrication (Ag°-tissue conditioner)
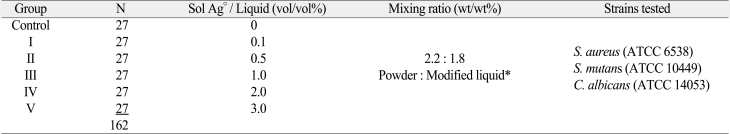
The tissue conditioner selected in this study was GC Soft-Liner (GC cooperation, Tokyo, Japan) supplied as powder and liquid. Doses of Ag° added to the conditioner liquid are shown in Table 1. Colloidal Ag° was preliminary combined and homogenized with the conditioner liquid in a sterile glass beaker at the concentration ranging from 0 (control), 0.1, 0.5, 1.0, 2.0 to 3.0% (vol/vol %: Colloidal Ag°/conditioner liquid) respectively. Immediately afterwards, the conditioner powder was added and mixed for 30 seconds at designated powder/liquid ratio as manufacturer's instruction. In order to fabricate samples into uniform shape with regular surface, the mixed paste of conditioner was poured onto a custom-made brass mould with the hole (20 mm diameter × 3.0 mm depth). The mixed paste was sandwiched between glass-slides until it was solidified under humid condition. The total 162 samples were prepared and they were divided into six groups (n = 27) according to the concentration of Ag° incorporated. Then, within a group, nine samples were assigned to each strain. Before microbial assay, all samples were sterilized with ethylene oxide gas for 24 hrs to ensure the initial sterility of samples.
Table 1.
The classification of experimental groups
*Sol Ag° + conditioner liquid
3. Microorganisms
Three standard strain organisms were used: S. aureus (ATCC 6538), S. mutans (ATCC 10449) and C. albicans (ATCC 14053). Microbial suspensions were obtained from single colony isolated on agar plates, inoculated in appropriate broth for overnight cultures. Bacterial strains were grown in brainheart infusion (BHI) (Difco, Franklin Lakes, NJ, USA) broth and onto Mueller Hinton agar plates at 37℃ and C. albicans strain was grown in Schaedler broth (Difco, Franklin Lakes, NJ ,USA) and onto Sabouraud agar plates (Difco, Franklin Lakes, NJ, USA) at 30℃. After incubating microbial cells at 37℃ overnight, optical density (OD) of the suspension at 600 nm was adjusted to 1.0 using a spectrophotometer (Milton Roy spectrophotometer 20D+, Milton Roy, Ivyland, USA). The suspension was diluted with phosphate-buffered saline (pH 7.4) to 1:100 and suspended to final concentration of 1.0 × 107 cells/mL.14,21
4. Antimicrobial assay
Each disc sample of Ag°-tissue conditioner and control were placed on the flat bottom of the separate 12-well cell culture plate (Costa®, Corning, New York, USA) of 22.1 mm well diameter and 100 µL of initial microbial suspensions in 1.0 ml of Sabouraud broth were inoculated to each well and incubated at 37℃. After incubation for 24 hrs and 72 hrs for extended contact period, suspension (100 µL) was withdrawn, viable cells (CFU: Colony Forming Unit) in the suspension were determined by using the spread plate method at a level of detection within 500 CFU per plate through the serial dilution. Assays were independently performed with three repetitive tests and data were recorded as means and standard deviations. According to conventional standards,22,23 the borderline of antimicrobial effect was determined at 0.1% viable cells; 99.9% reduction of CFU as the minimum bactericidal concentration (MBC) of antibiotics. Data were analyzed by oneway ANOVA and Student t-test at a 0.05 probability level.
RESULTS
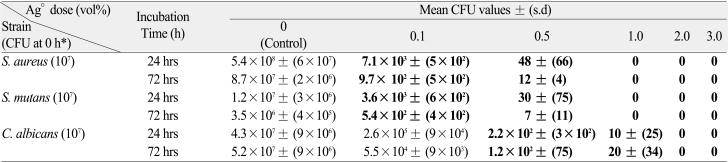
The antimicrobial effects of tissue conditioner with Ag° against S. aureus, S. mutans and C. albicans were demonstrated as the mean viable cells (CFU) after 24 and 72 hrs incubation time (Table 2). When compared to CFU at 0 hour, Control group (0% Ag°) did not showed any microbial inhibitory effect against all tested strains. For two bacterial strains, S. aureus and S. mutans, Ag°-tissue conditioner samples showed the minimal bactericidal effects (MBC) at the dose of above 0.1% and no viable cells were detected (no CFU) from the conditions of 1.0% above. And for fungal strain of C. albicans, Ag°-tissue conditioner samples showed the minimal fungicidal concentration at the dose of above 0.5% and no CFU was detected in 2.0% above. There was no statistical difference between 24 hrs and extended 72 hrs incubation time (P > .05) for the antimicrobial effect.
Table 2.
In vitro antiseptic properties of a tissue conditioner disc samples combined with a silver nanoparticle (0 - 3.0 %) against S. aureus, S. mutans and C. albicans. Results are expressed in CFU count with standard deviation
*: Starting inoculums: 107 CFU
Figures in bold represent values statistically different from control (P < .05).
DISCUSSION
In the present work, the addition of Ag° to tissue conditioner yielded bactericidal and fungicidal properties for three reference strains, S. aureus, S. mutans and C. albicans. These microbial species tested are currently recommended to test antiseptic molecules.24 S. aureus, a pathogen causing respiratory infections, has often been isolated from dentures and the oral cavity4,25 and dentures have recently been reported to be a carriage of this pathogen.26 S. mutans has been associated closely with the pathogenesis of dental caries, which is of limited clinical significance for denture wearers.27 However, extensive plaque formation on denture might also contribute to the decay of residual natural teeth and to the inflammation of gingival tissue adjacent to the denture.27 C. albicans can be regularly isolated, suggesting a pathogenic association between bacteria and fungi related with denture stomatitis.
For evaluating the antimicrobial effect in present study, a small volume of microbial suspension (100 µL) was used. The oral microbe would appear to be in a stationary phase rather than in growing phase, because the nutrition is limited under the antibodies and the antimicrobial enzymes existing in the oral cavity.28 The assays tested with samples immersed in a large volume of microbial suspension could not reproduce in vivo tissue conditioner which closely contacts the gingival mucosa.11 Microorganisms in suspension (planktonic phase) are sensitive to lower antiseptic concentrations than microbe colonizing surfaces and protected by a biofilm.29 In this study, the microbes were adjusted to the stationary phase to be suspended in broth. And as no criterion of the antimicrobial effect on dental material has been established so far, the concept of minimum bactericidal concentration (MBC) of antibiotics was thus adopted as the antimicrobial concentration at more than 99.9% elimination of the organisms.22,23
The present microbial assay confirmed that the susceptibility of C. albicans to Ag°-tissue conditioner sample (0.5%) was less than to the samples (0.1%) of two bacterial strains. It is reported that Ag and silver-based compounds are highly toxic to prokaryotic cell showing strong biocidal effects on as bacteria species,17 while Ag showed less effect on eukaryotic cell such as mold and yeasts.30 The control group displayed no inhibitory effect against tested strains though tissue conditioner itself possesses antimicrobial effects due to ingredients such as plasticizers and ethanol.31 Other studies also showed various antimicrobial effects on C. albicans and S. aureus, but these findings were at variance with previously reported findings indicating that such materials have little antimicrobial effect.1,32
The present study could not jump to conclude whether the antimicrobial effect was resulted from release of silver cation from the modified sample to incubation medium or direct contact between Ag°-tissue conditioner and microbial cells. Because the mechanism of the antimicrobial effect of silver supported compound has not been fully explained yet. It was suggested that as a result of the catalytic action of silver, oxygen is converted into active oxygen (including hydroxyl radicals) by the action of light energy and/or H2O in the air or water only at polar surfaces. These active oxygen radicals cause the structural damage in bacteria and lead to the damage or even the death of the microorganisms, so called "oligodynamic action of silver".19,33
It is desirable for dental materials to have a low susceptibility to oral microorganism adhesion. The results of the present study implicate that Ag° added tissue conditioner might act like latent antimicrobial material and it could provide the additional benefit of antimicrobial effect even if dentures are worn at night, therefore, could be used as an one of the alternative therapy for denture stomatitis resistant to conventional treatment or geriatric denture bearing patients under medically compromised status.34 However, further studies are still required to clarify the optimal concentration of Ag°, regarding the silver content, the possible disruption of oral microflora and toxic effects of silver with excess Ag°and mechanical stability should be also considered for the proper and safe clinical application.35
CONCLUSION
Within the limitations of present in vitro study, the modified tissue conditioner combined with silver nanoparticles displayed antimicrobial properties against S. aureus, S. mutans at 0.1% Ag° incorporated and C. albicans at 0.5% Ag° incorporated after a 24 hrs and 72 hrs incubation period. Further studies of cell toxicity and physical stability are still required for its clinical use.
Footnotes
The present research has been conducted by the Research Grant of Samsung Eye Center in 2009.
References
- 1.Okita N, Orstavik D, Orstavik J, Ostby K. In vivo and in vitro studies on soft denture materials: microbial adhesion and tests for antibacterial activity. Dent Mater. 1991;7:155–160. doi: 10.1016/0109-5641(91)90035-w. [DOI] [PubMed] [Google Scholar]
- 2.Radford DR, Challacombe SJ, Walter JD. Denture plaque and adherence of Candida albicans to denture-base materials in vivo and in vitro. Crit Rev Oral Biol Med. 1999;10:99–116. doi: 10.1177/10454411990100010501. [DOI] [PubMed] [Google Scholar]
- 3.Nair RG, Samaranayake LP. The effect of oral commensal bacteria on candidal adhesion to denture acrylic surfaces. An in vitro study. APMIS. 1996;104:339–349. doi: 10.1111/j.1699-0463.1996.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 4.Wilkieson C, Samaranayake LP, MacFarlane TW, Lamey PJ, MacKenzie D. Oral candidosis in the elderly in long term hospital care. J Oral Pathol Med. 1991;20:13–16. doi: 10.1111/j.1600-0714.1991.tb00880.x. [DOI] [PubMed] [Google Scholar]
- 5.Rossi T, Laine J, Eerola E, Kotilainen P, Peltonen R. Denture carriage of methicillin-resistant Staphylococcus aureus. Lancet. 1995;345:1577. doi: 10.1016/s0140-6736(95)91129-4. [DOI] [PubMed] [Google Scholar]
- 6.Harrison A, Basker RM, Smith IS. The compatibility of temporary soft materials with immersion denture cleansers. Int J Prosthodont. 1989;2:254–258. [PubMed] [Google Scholar]
- 7.Nikawa H, Iwanaga H, Hamada T, Yuhta S. Effects of denture cleansers on direct soft denture lining materials. J Prosthet Dent. 1994;72:657–662. doi: 10.1016/0022-3913(94)90300-x. [DOI] [PubMed] [Google Scholar]
- 8.De Visschere LM, Grooten L, Theuniers G, Vanobbergen JN. Oral hygiene of elderly people in long-term care institutions-a cross-sectional study. Gerodontology. 2006;23:195–204. doi: 10.1111/j.1741-2358.2006.00139.x. [DOI] [PubMed] [Google Scholar]
- 9.Casemiro LA, Gomes Martins CH, Pires-de-Souza Fde C, Panzeri H. Antimicrobial and mechanical properties of acrylic resins with incorporated silver-zinc zeolite - part I. Gerodontology. 2008;25:187–194. doi: 10.1111/j.1741-2358.2007.00198.x. [DOI] [PubMed] [Google Scholar]
- 10.Quinn DM. The effectiveness, in vitro, of miconazole and ketoconazole combined with tissue conditioners in inhibiting the growth of Candida albicans. J Oral Rehabil. 1985;12:177–182. doi: 10.1111/j.1365-2842.1985.tb00633.x. [DOI] [PubMed] [Google Scholar]
- 11.Truhlar MR, Shay K, Sohnle P. Use of a new assay technique for quantification of antifungal activity of nystatin incorporated in denture liners. J Prosthet Dent. 1994;71:517–524. doi: 10.1016/0022-3913(94)90193-7. [DOI] [PubMed] [Google Scholar]
- 12.Chow CK, Matear DW, Lawrence HP. Efficacy of antifungal agents in tissue conditioners in treating candidiasis. Gerodontology. 1999;16:110–118. doi: 10.1111/j.1741-2358.1999.00110.x. [DOI] [PubMed] [Google Scholar]
- 13.Koopmans AS, Kippuw N, de Graaff J. Bacterial involvement in denture-induced stomatitis. J Dent Res. 1988;67:1246–1250. doi: 10.1177/00220345880670091901. [DOI] [PubMed] [Google Scholar]
- 14.Budtz-Jörgensen E, Theilade E, Theilade J, Zander HA. Method for studying the development, structure and microflora of denture plaque. Scand J Dent Res. 1981;89:149–156. doi: 10.1111/j.1600-0722.1981.tb01665.x. [DOI] [PubMed] [Google Scholar]
- 15.Fu J, Ji J, Fan D, Shen J. Construction of antibacterial multilayer films containing nanosilver via layer-by-layer assembly of heparin and chitosan-silver ions complex. J Biomed Mater Res A. 2006;79:665–674. doi: 10.1002/jbm.a.30819. [DOI] [PubMed] [Google Scholar]
- 16.Slawson RM, Lee H, Trevors JT. Bacterial interactions with silver. Biol Met. 1990;3:151–154. doi: 10.1007/BF01140573. [DOI] [PubMed] [Google Scholar]
- 17.Zhao G, Stevens SE., Jr Multiple parameters for the comprehensive evaluation of the susceptibility of Escherichia coli to the silver ion. Biometals. 1998;11:27–32. doi: 10.1023/a:1009253223055. [DOI] [PubMed] [Google Scholar]
- 18.Alt V, Bechert T, Steinrücke P, Wagener M, Seidel P, Dingeldein E, Domann E, Schnettler R. An in vitro assessment of the antibacterial properties and cytotoxicity of nanoparticulate silver bone cement. Biomaterials. 2004;25:4383–4391. doi: 10.1016/j.biomaterials.2003.10.078. [DOI] [PubMed] [Google Scholar]
- 19.Samuel U, Guggenbichler JP. Prevention of catheter-related infections: the potential of a new nano-silver impregnated catheter. Int J Antimicrob Agents. 2004;23:S75–S78. doi: 10.1016/j.ijantimicag.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Wright JB, Lam K, Hansen D, Burrell RE. Efficacy of topical silver against fungal burn wound pathogens. Am J Infect Control. 1999;27:344–350. doi: 10.1016/s0196-6553(99)70055-6. [DOI] [PubMed] [Google Scholar]
- 21.Chandra J, Mukherjee PK, Leidich SD, Faddoul FF, Hoyer LL, Douglas LJ, Ghannoum MA. Antifungal resistance of candidal biofilms formed on denture acrylic in vitro. J Dent Res. 2001;80:903–908. doi: 10.1177/00220345010800031101. [DOI] [PubMed] [Google Scholar]
- 22.Bruns W, Keppeler H, Baucks R. Suppression of intrinsic resistance to penicillins in Staphylococcus aureus by polidocanol, a dodecyl polyethyleneoxid ether. Antimicrob Agents Chemother. 1985;27:632–639. doi: 10.1128/aac.27.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gristina AG, Jennings RA, Naylor PT, Myrvik QN, Webb LX. Comparative in vitro antibiotic resistance of surface-colonizing coagulase-negative staphylococci. Antimicrob Agents Chemother. 1989;33:813–816. doi: 10.1128/aac.33.6.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reverdy ME, Martra A, Fleurette J. Application of a micromethod to the study of the bactericidal activity of 2 antiseptics based on chlorhexidine gluconate. Pathol Biol (Paris) 1986;34:688–693. [PubMed] [Google Scholar]
- 25.Steinberg D, Eyal S. Early formation of Streptococcus sobrinus biofilm on various dental restorative materials. J Dent. 2002;30:47–51. doi: 10.1016/s0300-5712(01)00058-6. [DOI] [PubMed] [Google Scholar]
- 26.Satou J, Fukunaga A, Morikawa A, Matsumae I, Satou N, Shintani H. Streptococcal adherence to uncoated and saliva-coated restoratives. J Oral Rehabil. 1991;18:421–429. doi: 10.1111/j.1365-2842.1991.tb01687.x. [DOI] [PubMed] [Google Scholar]
- 27.Hahnel S, Rosentritt M, Bürgers R, Handel G. Adhesion of Streptococcus mutans NCTC 10449 to artificial teeth: an in vitro study. J Prosthet Dent. 2008;100:309–315. doi: 10.1016/S0022-3913(08)60212-7. [DOI] [PubMed] [Google Scholar]
- 28.Abe Y, Ishii M, Takeuchi M, Ueshige M, Tanaka S, Akagawa Y. Effect of saliva on an antimicrobial tissue conditioner containing silver-zeolite. J Oral Rehabil. 2004;31:568–573. doi: 10.1111/j.1365-2842.2004.01267.x. [DOI] [PubMed] [Google Scholar]
- 29.Baehni PC, Takeuchi Y. Anti-plaque agents in the prevention of biofilm-associated oral diseases. Oral Dis. 2003;9:23–29. doi: 10.1034/j.1601-0825.9.s1.5.x. [DOI] [PubMed] [Google Scholar]
- 30.Christensen M, Rungby J, Mogensen SC. Effects of selenium on toxicity and ultrastructural localization of mercury in cultured murine macrophages. Toxicol Lett. 1989;47:259–270. doi: 10.1016/0378-4274(89)90144-6. [DOI] [PubMed] [Google Scholar]
- 31.Matsuura T, Abe Y, Sato Y, Okamoto K, Ueshige M, Akagawa Y. Prolonged antimicrobial effect of tissue conditioners containing silver-zeolite. J Dent. 1997;25:373–377. doi: 10.1016/s0300-5712(96)00050-4. [DOI] [PubMed] [Google Scholar]
- 32.Mäkilä E, Hopsu-Havu VK. Mycotic growth and soft denture lining materials. Acta Odontol Scand. 1977;35:197–205. doi: 10.3109/00016357709004655. [DOI] [PubMed] [Google Scholar]
- 33.Feng QL, Wu J, Chen GQ, Cui FZ, Kim TN, Kim JO. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J Biomed Mater Res. 2000;52:662–668. doi: 10.1002/1097-4636(20001215)52:4<662::aid-jbm10>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 34.Geerts GA, Stuhlinger ME, Basson NJ. Effect of an antifungal denture liner on the saliva yeast count in patients with denture stomatitis: a pilot study. J Oral Rehabil. 2008;35:664–669. doi: 10.1111/j.1365-2842.2007.01805.x. [DOI] [PubMed] [Google Scholar]
- 35.Petering HG. Pharmacology and toxicology of heavy metals: Silver. Pharmacol Ther. 1976;1:127–130. [Google Scholar]