Abstract
Background: Thiamine, riboflavin, niacin, vitamin B-6, folate, and vitamin B-12 are required to synthesize neurotransmitters that are potentially involved in the pathophysiology of premenstrual syndrome (PMS).
Objective: The objective was to evaluate whether B vitamin intake from food sources and supplements is associated with the initial development of PMS.
Design: We conducted a case-control study nested within the Nurses' Health Study II cohort. Participants were free of PMS at baseline (1991). After 10 y of follow up, 1057 women were confirmed as cases and 1968 were confirmed as controls. Dietary information was collected in 1991, 1995, and 1999 by using food-frequency questionnaires.
Results: Intakes of thiamine and riboflavin from food sources were each inversely associated with incident PMS. For example, women in the highest quintile of riboflavin intake 2–4 y before the diagnosis year had a 35% lower risk of developing PMS than did those in the lowest quintile (relative risk: 0.65; 95% CI: 0.45, 0.92; P for trend = 0.02). No significant associations between incident PMS and dietary intakes of niacin, vitamin B-6, folate, and vitamin B-12 were observed. Intake of B vitamins from supplements was not associated with a lower risk of PMS.
Conclusions: We observed a significantly lower risk of PMS in women with high intakes of thiamine and riboflavin from food sources only. Further research is needed to evaluate the effects of B vitamins in the development of premenstrual syndrome.
INTRODUCTION
Premenstrual syndrome (PMS) is a disorder characterized by physical and psychological symptoms that are manifested during the late luteal phase of the menstrual cycle and end shortly after the onset of menstruation. Although the true prevalence of PMS is unknown, it has been estimated that 15% of women of reproductive age in the United States meet the established clinical criteria for PMS (1). The pathophysiology of PMS remains unclear and is a matter of ongoing investigation. Current treatments for PMS include oral contraceptives, gonadotropin-releasing hormone agonists, and antidepressants—all of which have significant side effects. Therefore, prevention of PMS through identification of modifiable risk factors is of primary importance.
The pathophysiology of PMS may include an interaction of ovarian hormones with brain neurotransmitters, such as serotonin and γ-amino butyric acid (GABA) (2, 3). The B vitamins thiamine, niacin, riboflavin, vitamin B-6, folate, and vitamin B-12 are involved in the metabolism of neurotransmitters through different mechanisms. Riboflavin is needed to activate vitamin B-6, which is a cofactor in the generation of serotonin from the amino acid tryptophan. Niacin deficiency may lead to depletion of tryptophan, thereby reducing its availability to form serotonin (4). Thiamine is required for the metabolism of glucose and precursors of GABA. Vitamin B-12, vitamin B-6, and folate are associated with the formation of S-adenosyl-methionine and tetrahydrobiopterin, both of which are required for the metabolism of serotonin and dopamine (5, 6).
To our knowledge, no previous studies have examined whether intake of B vitamins may prevent the initial development of PMS. Previous studies of B vitamins and PMS generally have been limited to randomized clinical trials of the efficacy of vitamin B-6 at different doses as a treatment of premenstrual symptoms (7–14). Some (8, 9, 15) but not all (11–14) studies have found vitamin B-6 supplementation to reduce the occurrence and severity of symptoms. To our knowledge, no previous studies have assessed the association of PMS or menstrual symptoms with thiamine, niacin, riboflavin, folate, and vitamin B-12 intakes, although some clinical trials have evaluated supplements containing many of these vitamins as treatment of menstrual symptoms; the results suggest that B vitamin intake may be beneficial (16–18). We evaluated the association between intakes of thiamine, riboflavin, niacin, vitamin B-6, folate, and vitamin B-12 and the risk of incident PMS in a subset of women participating in the Nurses' Health Study II (NHS II).
SUBJECTS AND METHODS
The NHS II is a prospective cohort of 116,678 female US registered nurses, who replied to a mailed questionnaire in 1989 when they were 25–42 y of age. Information regarding various lifestyle factors and medical conditions has been collected by mailed questionnaire every 2 y. The response rate for each questionnaire cycle has been ≥89%. The study protocol was approved by the Institutional Review Board at Brigham and Women's Hospital.
Identification of cases and controls
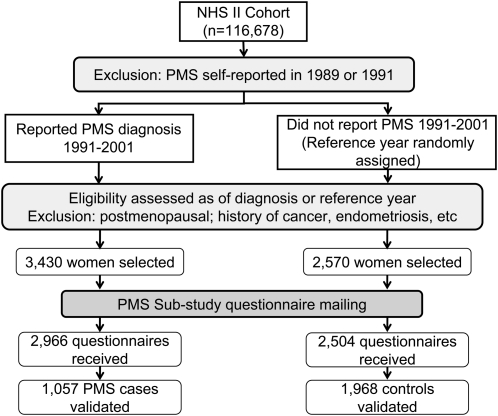
The establishment of the NHS II PMS Substudy was described in detail previously (19, 20). Briefly, from among all NHS II participants who had not reported a diagnosis of PMS in 1989 or 1991, we identified 3430 women who reported a new clinician-made diagnosis of PMS on an NHS II questionnaire between 1993 and 2001 (Figure 1). We assigned each woman a “reference year” equal to their diagnosis year, which we used to determine eligibility for the study and to assess menstrual symptoms and diet. We then identified 2570 women who did not report a diagnosis of PMS at any time between 1989 and 2001 to serve as potential controls; for these women, we assigned a randomly chosen year between 1993 and 2001 to be their reference year. Women with a diagnosis of cancer, endometriosis, usual irregular menstrual cycles, or infertility before their reference year were excluded from the initial selection of participants to prevent the inclusion of women with symptoms attributable to causes other than PMS. Because of our interest in dietary factors, we also excluded women reporting an implausible total calorie intake (<500 or ≥3500 kcal/d) on diet questionnaires completed in 1991 and 1995.
FIGURE 1.
Design of the Nurses' Health Study II (NHS II) Premenstrual Syndrome (PMS) Substudy, 1991–2001.
In 2002, we mailed participants a questionnaire based on the Calendar of Premenstrual Experiences designed by Mortola et al (21) to confirm the PMS diagnosis in cases and verify that controls did not have PMS. We asked participants to report the presence of any of 26 specific symptoms for at least several days each month for most months of the year in the specific 2 y before their individual reference year. We also included questions about the age at which symptoms started, the timing of symptom onset and cessation during an average menstrual cycle, and the severity of symptoms and their influence on personal relationships, social functioning, and work-related activities. This questionnaire was completed by 86.5% of the potential cases (n = 2966) and 97.4% of the potential controls (n = 2504).
Our PMS case definition was based on the criteria established by Mortola et al (21). We considered participants as validated cases if they reported the following: 1) the occurrence of at least one physical and one affective menstrual symptom; 2) their overall symptom severity to be moderate or severe or the effect of symptoms on life activities and social relationships to be moderate or severe; 3) symptoms beginning within 14 d of the onset of menstruation; 4) symptoms ending within 4 d of the onset of menses; and 5) symptoms absent in the week after menses ends. Ultimately, 1057 (35.6%) potential cases met these criteria and were included in the present analysis.
We considered women as validated controls if they, in addition to not reporting a diagnosis of PMS during the study period, reported either no menstrual symptoms or only mild symptoms with no substantial effect on life activities and interpersonal relationships. A total of 1968 (78.6%) potential controls met these criteria and were included in the present analysis.
The validity of our approach for assessing PMS symptoms was evaluated previously (20) in those participants from the PMS Substudy who reported a diagnosis of PMS for the first time in 2001 (n = 138) and controls whose reference year was 2001 (n = 377). Women who did not report prospective symptom charting as part of their diagnosis, but who met the Mortola criteria for PMS, were similar with regard to symptom timing and severity and the presence of physical symptoms to those who both reported prospective charting and who met the Mortola criteria (20).
Assessment of B vitamin intake and other factors
Participants completed a semiquantitative food-frequency questionnaire (FFQ) as part of their main NHS II questionnaires in 1991, 1995, and 1999 to estimate usual dietary intake of 131 foods and supplements during the previous year. Participants were asked to indicate how frequently they consumed a specific portion size of each food item, with 9 possible response options ranging from “never or less than once per month” to “6 or more times per day.” B vitamin–rich foods included on the FFQ included fortified cereals, milk, red meat, seafood, beans and lentils, bananas, and green leafy vegetables.
To calculate each participant's intake of B vitamins from foods, the portion size of a single serving of each food was multiplied by the reported intake frequency and then by the vitamin content of each food. Nutrient content was then summed across all foods. Finally, adjustment for total energy intake was performed by using the residual method (22).
Specific questions about the use of multivitamin and several individual vitamin supplements including vitamin B-6 were also included on each FFQ. Participants were asked to report whether they currently took multivitamins, how many they took per week (≤2, 3–5, 6–9, or ≥10 tablets) and the specific brand used. Women were also asked to specify their use and dose of individual vitamin B-6 supplements (<50, 50–99, 100–149, or ≥150 mg/d). Additional questions on regular use of niacin, folate, and B-complex supplements (yes or no) were also included. The FFQ administered in 1999 additionally queried specific doses of niacin (<50, 50–300, 400–800, or ≥900 mg/d). The validity and reliability of the FFQ was evaluated previously (23, 24). For example, the Pearson coefficients for correlation between total vitamin B-6 intake from the FFQ and the mean dietary intake of 4 diet records completed 3 mo apart was 0.58 after adjustment for total energy intake (23).
We collected information on other factors potentially associated with PMS and diet, such as age, smoking status, weight, pregnancy history, tubal ligation, and oral contraceptive use on biennial questionnaire throughout the study period. Height and menstrual cycle characteristics were assessed in 1989. Physical activity was assessed in 1991 and 1997. History of depression and use of antidepressants was assessed on the supplemental menstrual symptom questionnaire. Childhood trauma related to punitive parenting was assessed in 2001 with a separate questionnaire (25). Finally, information on the dietary intake of other nutrients, such as calcium and vitamin D, was assessed by FFQ.
Statistical analysis
Baseline characteristics of PMS cases and controls were compared by using Pearson chi-square and t tests. The correlation between intakes of individual B vitamins was assessed with Spearman correlation coefficients. We evaluated the association between PMS and thiamine, riboflavin, niacin, vitamin B-6, folate, and vitamin B-12 at several time points. Intakes from food sources and supplemental sources were analyzed separately. First, we divided participants into quintiles based on their intake of each vitamin from food sources during the 2–4-y period before their individual reference year. Quintile cutoffs were based on the distribution of intake in the entire NHS II cohort. For our analysis of intake of each vitamin from supplemental sources only, we classified women into 4 groups: nonsupplement users and tertiles of supplement users. We also evaluated B vitamin intake as assessed at baseline (1991) and during the 2 y preceding the reference year. All statistical analyses were conducted with SAS 9.1 software (SAS Institute Inc, Cary, NC).
By using logistic regression, we calculated relative risks (RRs) and 95% CIs comparing the risk of PMS in the highest 4 quintiles or categories to the lowest (referent). Multivariable RRs and 95% CIs were adjusted for age, diagnosis year, number of full-term pregnancies (pregnancies lasting ≥6 mo), body mass index [BMI; weight (in kg)/height2 (in m)], smoking status, tubal ligation, duration of oral contraceptive use, childhood trauma, antidepressant use, and dietary intakes of alcohol, potassium, calcium, and vitamin D. Analyses of intakes from food sources are adjusted for intake of the same vitamin from supplemental sources and vice versa. In additional analyses, we adjusted each B vitamin for the effect of the others. To evaluate linear trends across quintiles in the multivariable regression models, we used a Mantel extension test for trend, modeling the medians of each quintile or category as a continuous variable. We also conducted subanalyses restricted to women with no history of depression before diagnosis (n = 882 cases and 1819 controls) and to those not using oral contraceptives at baseline (n = 938 cases and 1779 controls). Additionally, we conducted a subanalysis of supplement use at baseline, excluding PMS cases who reported that their menstrual symptoms had started before the beginning of follow-up in 1991 (n = 329 cases). We assessed whether the B vitamin–PMS relation varied by age, BMI, alcohol intake, and smoking status, because these factors were previously associated with PMS risk (26–28). Finally, we assessed potential interactions between the B vitamins themselves.
RESULTS
Baseline characteristics of cases and controls are presented in Table 1. Compared with controls, cases were younger and had a higher mean BMI at baseline and at age 18 y. Cases were more likely than controls to be current or former smokers and to report the use of antidepressants and oral contraceptives and history of severe childhood trauma. We did not observe significant differences in other factors.
TABLE 1.
Age-standardized characteristics of premenstrual syndrome cases and controls at baseline (1991): Nurses' Health Study II Premenstrual Syndrome Substudy (1991–2001)1
| Characteristics | Cases(n = 1057) | Controls(n = 1968) | P |
| Age (y)2 | 34.4 ± 4.3 | 35.0 ± 3.9 | 0.00023 |
| BMI (kg/m2)4 | |||
| At baseline, 1991 | 24.6 ± 0.2 | 23.7 ± 0.1 | <0.00013 |
| At the age of 18 y | 21.4 ± 0.1 | 21.1 ± 0.1 | 0.033 |
| Age at menarche (y) | 12.4 ± 0.04 | 12.5 ± 0.03 | 0.083 |
| No. of full-term pregnancies (n)45 | 1.7 ± 0.04 | 1.7 ± 0.03 | 0.523 |
| Physical activity (METs/wk)4 | 23.0 ± 1.8 | 23.3 ± 1.3 | 0.883 |
| History of tubal ligation (%) | 16.8 | 18.2 | 0.346 |
| Ever used oral contraceptives (%) | 85.7 | 77.7 | <0.0016 |
| Smoking status (%) | |||
| Current smoker | 12.3 | 6.5 | <0.00016 |
| Past smoker | 26.5 | 18.2 | <0.00016 |
| Ever used antidepressant medications (%) | 12.1 | 4.7 | <0.00016 |
| History of childhood trauma (%) | 14.8 | 7.9 | <0.00016 |
All characteristics, except for age, were standardized to the age distribution of participants in 1991. METs, metabolic equivalents.
Values are means ± SDs.
Calculated by using the t statistic.
Values are means ± SEs.
Limited to parous women.
Calculated by using the chi-square statistic.
Strong correlations were observed between intakes of vitamins B-6, riboflavin, niacin, and thiamine from food sources (range of correlation coefficients: 0.16–0.64; all P < 0.001), with the strongest between niacin and vitamin B-6 (r = 0.64) (Table 2). Intake of vitamin B-12 was modestly correlated with intake of other B vitamins.
TABLE 2.
Spearman correlation coefficients for B vitamin intake from food sources 2–4 y before the reference year: Nurses' Health Study II Premenstrual Syndrome Substudy (1991–2001)1
| Thiamine | Riboflavin | Niacin | Vitamin B-6 | Folate | Vitamin B-12 | |
| Thiamine | 1.00 | |||||
| Riboflavin | 0.57 | 1.00 | ||||
| Niacin | 0.46 | 0.26 | 1.00 | |||
| Vitamin B-6 | 0.54 | 0.49 | 0.64 | 1.00 | ||
| Folate | 0.61 | 0.48 | 0.36 | 0.60 | 1.00 | |
| Vitamin B-12 | 0.20 | 0.54 | 0.23 | 0.30 | 0.16 | 1.00 |
All correlations were significant at P < 0.001. n = 3025.
We observed an inverse association between intake of thiamine and riboflavin from food sources and incidence of PMS (Table 3). After adjustment for age, vitamin D and calcium intakes, and other factors, women with the highest intake of thiamine (median: 1.93 mg/d) during the 2–4 y before the reference year had an RR of 0.75 (95% CI: 0.56, 1.00) compared with women with the lowest intake (median: 1.20 mg/d; P for trend = 0.04). Women in the highest quintile of riboflavin intake (median: 2.52 mg/d) had a 35% lower risk of developing PMS (RR: 0.65; 95% CI: 0.45, 0.92) compared with those in the lowest quintile (median: 1.38 mg/d; P for trend = 0.02). Dietary intakes of niacin, vitamin B-6, folate, and vitamin B-12 were not associated with incident PMS. Results from analyses of B vitamin intake at baseline were generally similar to those 2–4 y before the reference year (data not shown). For example, women in the highest quintile of thiamine intake at baseline had an RR of 0.76 (95% CI: 0.57, 1.01; P for trend = 0.02) compared with those in the lowest quintile. However, for riboflavin, women in the highest quintile of dietary riboflavin intake had an RR of 0.84 (95%CI: 0.58, 1.20; P for trend = 0.28) as compared with those in the lowest quintile of intake. The results based on intake 0–2 y before the reference year were also similar (data not shown).
TABLE 3.
Age- and multivariable (MV)-adjusted relative risks (RRs) of premenstrual syndrome by quintile (Q) of intake of thiamine, riboflavin, vitamin B-6, folate, and vitamin B-12 from food sources in the 2–4-y period before the reference year: Nurses' Health Study II Premenstrual Syndrome Substudy (1991–2001)
| Q1 | Q2 | Q3 | Q4 | Q5 | P for trend1 | |
| Thiamine (mg/d) | ||||||
| Median | 1.20 | 1.39 | 1.53 | 1.67 | 1.93 | |
| Case:control ratio | 185:314 | 214:364 | 227:400 | 218:417 | 211:469 | |
| Age-adjusted RR | 1.00 | 1.01 | 0.97 | 0.89 | 0.76 | 0.009 |
| MV-adjusted RR2 | 1.00 | 0.93 | 0.90 | 0.88 | 0.75 | 0.04 |
| 95% CI | (0.70, 1.24) | (0.68, 1.20) | (0.66, 1.18) | (0.56, 1.00) | ||
| Riboflavin (mg/d) | ||||||
| Median | 1.38 | 1.63 | 1.86 | 2.12 | 2.52 | |
| Case:control ratio | 195:318 | 198:382 | 241:396 | 220:405 | 201:463 | |
| Age-adjusted RR | 1.00 | 0.84 | 0.97 | 0.87 | 0.68 | 0.004 |
| MV-adjusted RR2 | 1.00 | 0.81 | 1.00 | 0.90 | 0.65 | 0.02 |
| 95% CI | (0.60, 1.08) | (0.74, 1.36) | (0.64, 1.26) | (0.45, 0.92) | ||
| Niacin (mg/d) | ||||||
| Median | 18.1 | 21.2 | 23.5 | 25.8 | 29.9 | |
| Case:control ratio | 203:397 | 212:425 | 239:382 | 188:406 | 213:354 | |
| Age-adjusted RR | 1.00 | 0.99 | 1.23 | 0.91 | 1.20 | 0.23 |
| MV-adjusted RR2 | 1.00 | 1.00 | 1.18 | 0.83 | 1.09 | 0.88 |
| 95% CI | (0.77, 1.30) | (0.90, 1.53) | (0.63, 1.10) | (0.83, 1.44) | ||
| Vitamin B-6 (mg/d) | ||||||
| Median | 1.56 | 1.83 | 2.05 | 2.28 | 2.71 | |
| Case:control ratio | 178:380 | 245:414 | 217:426 | 231:372 | 184:372 | |
| Age-adjusted RR | 1.00 | 1.27 | 1.09 | 1.33 | 1.07 | 0.69 |
| MV-adjusted RR2 | 1.00 | 1.18 | 1.02 | 1.14 | 0.96 | 0.56 |
| 95% CI | (0.90, 1.56) | (0.76, 1.36) | (0.85, 1.55) | (0.69, 1.32) | ||
| Folate (μg/d) | ||||||
| Median | 206 | 256 | 299 | 347 | 434 | |
| Case:control ratio | 198:348 | 207:403 | 223:399 | 231:398 | 196:416 | |
| Age-adjusted RR | 1.00 | 0.90 | 1.01 | 1.04 | 0.85 | 0.34 |
| MV-adjusted RR2 | 1.00 | 0.90 | 1.05 | 0.99 | 0.82 | 0.29 |
| 95% CI | (0.68, 1.18) | (0.79, 1.40) | (0.73, 1.34) | (0.59, 1.12) | ||
| Vitamin B-12 (μg/d) | ||||||
| Median | 3.3 | 4.6 | 5.5 | 6.6 | 9.0 | |
| Case:control ratio | 224:387 | 225:396 | 202:454 | 213:370 | 191:357 | |
| Age-adjusted RR | 1.00 | 0.97 | 0.77 | 0.98 | 0.92 | 0.60 |
| MV-adjusted RR2 | 1.00 | 0.96 | 0.79 | 0.93 | 0.89 | 0.54 |
| 95% CI | (0.74, 1.25) | (0.60, 1.03) | (0.70, 1.23) | (0.67, 1.19) | ||
Calculated by using the Mantel extension test for trend.
Adjusted for age in 1989 (<30, 30–34, 35–39, or ≥40 y), year of diagnosis (1993, 1994–1995, 1996–1997, 1998–1999, or 2000–2001), number of full-term pregnancies (0, 1–2, 3–4, or ≥5 pregnancies lasting ≥6 mo), BMI (in kg/m2; <20.0, 20.0–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9, or ≥30.0), pack-years of smoking (quintiles), tubal ligation (yes or no), duration of oral contraceptive use (never or 1–23, 24–71, 72–119, or ≥120 mo), antidepressant use (never or ever), history of childhood trauma score (5, 6–10, 11–15, or ≥16), and total intakes of alcohol, potassium, calcium, and vitamin D. The intake of each vitamin from food sources was also adjusted for intake of that vitamin from supplemental sources.
Further adjustment of each vitamin for the effect of the others produced similar but slightly attenuated results (data not shown). For example, after adjustment for riboflavin, niacin, vitamin B-6, folate, and vitamin B-12, women in the highest quintile of thiamine intake had an RR of 0.78 (95% CI: 0.53, 1.14; P for trend = 0.22) compared with those in the lowest quintile. After adjustment for thiamine, niacin, vitamin B-6, folate, and vitamin B-12, women in the highest quintile of riboflavin intake had an RR of 0.67 (95% CI: 0.43, 1.05; P for trend = 0.09) compared with those in the lowest quintile.
In general, women with supplemental intake of B vitamins had a higher risk of PMS than did nonusers (Table 4). For example, compared with women with no intake of thiamine from supplements during the 2–4 y before the reference year, the RRs in tertiles 1 through 3 were 1.41, 1.54, and 1.66, respectively (P for trend in users of thiamine supplements = 0.22). RRs were attenuated when we evaluated supplement intake measured at baseline and were higher when we assessed supplement intake 0–2 y before the reference year. For example, for thiamine, RRs for tertiles 1–3 compared with nonusers were 1.44, 1.45, and 1.50, respectively (P for trend =0.68) for supplemental intake at baseline and were 1.35, 1.44, and 1.77 (P for trend = 0.07) for supplement use 0–2 y before the reference year. In a subanalysis excluding women reporting that their symptoms began before the start of follow-up in 1991, use of B vitamin supplements was not associated with an increased risk of PMS. For example, RRs in tertiles 1–3 of thiamine use compared with nonuse were 1.16, 1.00, and 0.91, respectively (P for trend = 0.62).
TABLE 4.
Age- and multivariable-adjusted relative risks of premenstrual syndrome by tertile (T) of thiamine, riboflavin, vitamin B-6, folate, and vitamin B-12 from supplement use compared with nonuse of supplements: Nurses' Health Study II Premenstrual Syndrome Substudy (1991–2001)1
| Nonusers | T1 | T2 | T3 | P for trend2 | |
| Thiamine (mg/d) | |||||
| Median3 | 0.00 | 0.85 | 1.50 | 5.70 | |
| Case:control ratio3 | 538:1080 | 163:287 | 178:328 | 178:273 | |
| Baseline, 1991 | 1.00 | 1.44 (1.09, 1.88) | 1.45 (1.03, 2.04) | 1.50 (1.10, 2.06) | 0.68 |
| Baseline, excluding cases with symptoms before 19914 | 1.00 | 1.16 (0.76, 1.77) | 1.00 (0.58, 1.70) | 0.91 (0.55, 1.51) | 0.62 |
| 2–4 y before reference year | 1.00 | 1.41 (1.08, 1.85) | 1.54 (1.11, 2.14) | 1.66 (1.23, 2.26) | 0.22 |
| 0–2 y before reference year | 1.00 | 1.35 (1.04, 1.75) | 1.44 (1.05, 1.97) | 1.77 (1.33, 2.36) | 0.07 |
| Riboflavin (mg/d) | |||||
| Median3 | 0.00 | 0.96 | 1.70 | 5.70 | |
| Case:control ratio3 | 540:1081 | 179:310 | 158:290 | 180:287 | |
| Baseline, 1991 | 1.00 | 1.42 (1.07, 1.86) | 1.51 (1.06, 2.14) | 1.43 (1.03, 1.98) | 0.98 |
| Baseline, excluding cases with symptoms before 19914 | 1.00 | 1.17 (0.76, 1.80) | 1.14 (0.65, 1.98) | 0.98 (0.58, 1.65) | 0.82 |
| 2–4 y before reference year | 1.00 | 1.38 (1.05, 1.81) | 1.42 (1.00, 2.01) | 1.44 (1.05, 1.97) | 0.65 |
| 0–2 y before reference year | 1.00 | 1.24 (0.95, 1.62) | 1.39 (1.01, 1.91) | 1.71 (1.28, 2.30) | 0.05 |
| Niacin (mg/d) | |||||
| Median3 | 0.0 | 5.7 | 20.0 | 50.0 | |
| Case:control ratio3 | 535:1077 | 154:294 | 220:372 | 148:225 | |
| Baseline, 1991 | 1.00 | 1.34 (1.02, 1.76) | 1.69 (1.23, 2.33) | 1.77 (1.26, 2.48) | 0.22 |
| Baseline, excluding cases with symptoms before 19914 | 1.00 | 1.06 (0.69, 1.62) | 1.14 (0.69, 1.87) | 1.02 (0.59, 1.78) | 0.99 |
| 2–4 y before reference year | 1.00 | 1.33 (1.01, 1.74) | 1.81 (1.32, 2.47) | 2.07 (1.49, 2.87) | 0.01 |
| 0–2 y before reference year | 1.00 | 1.29 (1.00, 1.67) | 1.44 (1.05, 1.94) | 2.11 (1.56, 2.85) | 0.002 |
| Vitamin B-6 (mg/d) | |||||
| Median3 | 0.00 | 0.03 | 1.15 | 4.98 | |
| Case:control ratio3 | 288:626 | 242:460 | 234:463 | 293:419 | |
| Baseline, 1991 | 1.00 | 0.93 (0.74, 1.17) | 1.37 (1.04, 1.79) | 1.79 (1.34, 2.41) | 0.0004 |
| Baseline, excluding cases with symptoms before 19914 | 1.00 | 0.74 (0.51, 1.07) | 1.03 (0.68, 1.55) | 1.12 (0.70, 1.77) | 0.35 |
| 2–4 y before reference year | 1.00 | 1.09 (0.86, 1.37) | 1.45 (1.00, 1.92) | 2.08 (1.56, 2.78) | <0.0001 |
| 0–2 y before reference year | 1.00 | 1.05 (0.83, 1.33) | 1.43 (1.08, 1.90) | 2.10 (1.58, 2.79) | <0.0001 |
| Folate (μg/d) | |||||
| Median3 | 0 | 228 | 400 | 800 | |
| Case:control ratio3 | 553:1115 | 220:359 | 196:317 | 88:177 | |
| Baseline, 1991 | 1.00 | 1.53 (1.19, 1.98) | 1.69 (1.19, 2.41) | 1.11 (0.74, 1.66) | 0.05 |
| Baseline, excluding cases with symptoms before 19914 | 1.00 | 1.15 (0.76, 1.72) | 1.30 (0.74, 2.26) | 0.92 (0.51, 1.66) | 0.68 |
| 2–4 y before reference year | 1.00 | 1.57 (1.22, 2.03) | 2.05 (1.46, 2.87) | 1.43 (0.96, 2.13) | 0.25 |
| 0–2 y before reference year | 1.00 | 1.29 (0.99, 1.67) | 1.90 (1.40, 2.58) | 1.61 (1.15, 2.25) | 0.15 |
| Vitamin B-12 (μg/d) | |||||
| Median3 | 0 | 0.3 | 3.2 | 6.5 | |
| Case:control ratio3 | 295:647 | 260:462 | 258:411 | 244:448 | |
| Baseline, 1991 | 1.00 | 1.00 (0.79, 1.26) | 1.41 (1.09, 1.83) | 1.59 (1.13, 2.23) | 0.02 |
| Baseline, excluding cases with symptoms before 19914 | 1.00 | 1.25 (0.88, 1.78) | 1.17 (0.77, 1.78) | 1.20 (0.71, 2.04) | 0.72 |
| 2–4 y before reference year | 1.00 | 1.25 (1.00, 1.58) | 1.65 (1.25, 2.16) | 1.68 (1.19, 2.35) | 0.13 |
| 0–2 y before reference year | 1.00 | 1.25 (0.91, 1.71) | 1.75 (1.20, 2.55) | 1.45 (0.97, 2.17) | 0.26 |
In T1–T3, relative risks (95% CIs) were adjusted for age in 1989 (<30, 30–34, 35–39, or ≥40 y), year of diagnosis (1993, 1994–1995, 1996–1997, 1998–1999, or 2000–2001), number of full-term pregnancies (0, 1–2, 3–4, or ≥5 pregnancies lasting ≥6 mo), BMI (in kg/m2; <20.0, 20.0–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9, or ≥30.0), pack-years of smoking (quintiles), tubal ligation (yes or no), duration of oral contraceptive use (never or 1–23, 24–71, 72–119, or ≥120 mo), antidepressant use (never or ever), history of childhood trauma score (5, 6–10, 11–15, or ≥16), and total intakes of alcohol, potassium, calcium, and vitamin D.
Test for trend in users of supplements only; Mantel-extension test.
Medians and case-control ratios from 2 to 4 y before reference data.
Analysis included 329 cases and 1968 controls.
For analyses of both food and supplement intakes, the results from the analyses excluding participants who took antidepressants before diagnosis were similar to the results from the main analysis, as were the results excluding women who reported using oral contraceptives at baseline (data not shown). Stratified analyses found no evidence that the relationships between B vitamin intake and incidence of PMS were modified by age, BMI, alcohol intake, or smoking status (data not shown). Finally, we found no evidence of significant interactions between individual B vitamins, although our power for this analysis was relatively low (data not shown).
DISCUSSION
To our knowledge, this was the first study to examine the association between intakes of thiamine, riboflavin, niacin, vitamin B-6, folate, and vitamin B-12 and incident cases of PMS. We found that high intakes of thiamine and riboflavin from food sources were associated with a significantly lower incidence of PMS. No association between was found between dietary intakes of niacin, vitamin B-6, folate, and vitamin B-12 and incidence of PMS.
For both thiamine and riboflavin, the level of intake at which we observed a benefit was considerably above current recommendations. For thiamine (RDA: 1.1 mg/d) (29), we found that women consuming ≈1.9 mg/d had a 25% lower risk of PMS than did those consuming ≈1.2 mg/d. This level of intake can be achieved by consuming 2–3 servings/d of thiamine-rich foods, such as fortified cereals, legumes, nuts, and red meats such as pork. For riboflavin (RDA = 1.1 mg/d) (29), women consuming ≈2.5 mg/d had a 35% lower risk than did those consuming ≈1.4 mg/d. This level of intake can be achieved with 1–2 servings fortified cereal/d or 6–7 servings riboflavin-rich foods such as cow milk or soy milk, spinach, and red meats.
Although we found an inverse association of thiamine and riboflavin from food sources, we observed an increased risk associated with any supplemental intake of these and other B vitamins. These results likely reflect the use of B vitamins to treat menstrual symptoms developing before diagnosis. Despite the lack of consistent evidence, deficiencies in B vitamins are thought to be associated with menstrual symptom occurrence and severity, and supplements may be recommended by physicians for treatment of mild symptoms (1, 30–32). To evaluate the likelihood that the observed increased risks were due to this type of confounding by indication, we conducted separate analyses of the association of intake of B vitamin supplements at 3 time periods, hypothesizing that the risks would be higher when supplement use was assessed closer in time to diagnosis. We did, in fact, find that associations were strongest when supplement use was assessed 0–2 y before diagnosis and attenuated when use was assessed at baseline (ie, 2–10 y before diagnosis). Moreover, when we conducted a separate analysis excluding women who reported that their symptoms had already begun before the start of our follow-up period, intake of B vitamins from supplements was not associated with PMS risk.
Alternatively, the difference in our findings for riboflavin and thiamine from foods sources compared with supplements could be explained by differences in forms and bioavailability of these vitamins in different foods. In addition, other components in B vitamin–rich foods may be associated with risk of PMS. For example, milk is rich in riboflavin, calcium, and vitamin D, which have been shown to be associated with a decreased risk of PMS (19). We therefore adjusted for calcium and vitamin D in all analyses to reduce residual confounding by other nutrients.
Previous randomized controlled trials have found a beneficial effect of vitamin B-6 on PMS symptoms using doses up to 100 mg/d (7–9). For example, in 2007, Sharma et al (9) conducted a randomized clinical trial in 60 women who reported premenstrual symptoms and found that women who received a supplement of 100 mg pyridoxine/d for 3 mo showed a significant reduction in premenstrual symptoms as compared with placebo or bromocriptine (P < 0.01) (9). In our population, the doses of vitamin B-6 from supplements consumed were very low compared with those used in intervention studies; the median vitamin B-6 intake from supplements in the highest tertile was 4.98 mg/d. Hence, because of the low intakes in our population, we were unable to evaluate the association with “therapeutic” doses in incident cases of PMS and could have missed the potential beneficial effects. Other randomized clinical trials have evaluated the effects of supplements containing multiple B vitamins and other micronutrients on symptoms of PMS and observed some significant improvement (16–18).
B vitamin intakes from food sources were highly correlated in our study and also correlated with other nutrients that have been associated with PMS in previous studies, such as calcium and vitamin D (19, 33, 34). For example, the Spearman correlation between riboflavin and vitamin D was 0.74 and between riboflavin and calcium was 0.77 (P < 0.0001 for both). In addition, a biologic interaction was observed between individual B vitamins, which made it difficult to assess the specific effects of each individual vitamin. For example, riboflavin is required to form pyridoxal phosphate, which is the active form of vitamin B-6. To address these issues, we adjusted for a variety of nutrients in our analyses and evaluated confounding and effect modification of each B vitamin by the others. In addition, because the main NHS II questionnaires assessed a variety of reproductive and lifestyle variables, we were able to control for several important confounders, including smoking and use of oral contraceptives.
Because of the prospective design of our study and the large number of participants, we were unable to use prospective charting (ie, recording of daily symptoms for ≥2 cycles) for identification of PMS cases, as is recommended by the American Congress of Obstetricians and Gynecologists (1) and as is current practice for studies of prevalent PMS. However, we used established criteria to identify PMS cases and symptom-free controls and thus to compare women at the 2 extremes of the spectrum of menstrual symptom experience, thereby decreasing the likelihood of misclassification. The validity of our method was assessed previously (20), and we identified significant risk factors for PMS in previous studies in this population (19, 28, 35).
In conclusion, the results of this study suggest a possible benefit of high intakes of riboflavin and thiamine from food sources on the incidence of PMS. Because this is the first prospective study to evaluate the effects of these vitamins, additional studies of these relations are warranted, including randomized clinical trials of thiamine and riboflavin for the prevention and possibly the treatment of PMS.
Acknowledgments
The authors' responsibilities were as follows—POC-B: designed the study, conducted the data analysis, interpreted the results, and wrote the first draft of the manuscript; JEM and SEH: contributed to obtaining funding, the concept and design of the study, and data collection; WCW: contributed to the concept and design of the study and data collection; SRJ: contributed to obtaining funding and to the concept and design of the study; LC-T and AGR: contributed to the design of the study and interpretation of the results; CB: contributed to the design of the study and provided statistical advice; and ERB-J: designed the study, obtained funding, and contributed to the interpretation of the results and writing of the first draft of the manuscript. All authors helped edit the manuscript. None of the authors had a conflict of interest in relation to this article.
REFERENCES
- 1.American College of Obstetrics and Gynecology Practice Bulletin Clinical management guidelines for obstetricians-gynecologists. Obstet Gynecol 2000;95:1–910636492 [Google Scholar]
- 2.Backstrom T, Andreen L, Birzniece V, et al. The role of hormones and hormonal treatments in premenstrual syndrome. CNS Drugs 2003;17:325–42 [DOI] [PubMed] [Google Scholar]
- 3.Halbreich U. The etiology, biology, and evolving pathology of premenstrual syndromes. Psychoneuroendocrinology 2003;28(suppl 3):55–99 [DOI] [PubMed] [Google Scholar]
- 4.Stipanuk MH. Biochemical, physiological, & molecular aspects of human nutrition. 2nd ed. St Louis, MO: Saunders Elsevier, 2006 [Google Scholar]
- 5.Frankenburg FR. The role of one-carbon metabolism in schizophrenia and depression. Harv Rev Psychiatry 2007;15:146. [DOI] [PubMed] [Google Scholar]
- 6.Miller AL. The methylation, neurotransmitter, and antioxidant connections between folate and depression. Altern Med Rev 2008;13:216. [PubMed] [Google Scholar]
- 7.Wyatt KM, Dimmock PW, Jones PW, Shaughn O'Brien PM. Efficacy of vitamin B-6 in the treatment of premenstrual syndrome: systematic review. BMJ 1999;318:1375–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kashanian M, Mazinani R, Jalalmanesh S. Pyridoxine (vitamin B6) therapy for premenstrual syndrome. Int J Gynaecol Obstet 2007;96:43–4 [DOI] [PubMed] [Google Scholar]
- 9.Sharma P, Kulshreshtha S, Singh GM, Bhagoliwal A. Role of bromocriptine and pyridoxine in premenstrual tension syndrome. Indian J Physiol Pharmacol 2007;51:368–74 [PubMed] [Google Scholar]
- 10.Williams AL, Cotter A, Sabina A, Girard C, Goodman J, Katz DL. The role for vitamin B-6 as treatment for depression: a systematic review. Fam Pract 2005;22:532–7 [DOI] [PubMed] [Google Scholar]
- 11.Barr W. Pyridoxine supplements in the premenstrual syndrome. Practitioner 1984;228:425–7 [PubMed] [Google Scholar]
- 12.Berman MK, Taylor ML, Freeman E. Vitamin B-6 in premenstrual syndrome. J Am Diet Assoc 1990;90:859–61 [PubMed] [Google Scholar]
- 13.De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med 2000;9:131–9 [DOI] [PubMed] [Google Scholar]
- 14.Hagen I, Nesheim BI, Tuntland T. No effect of vitamin B-6 against premenstrual tension. A controlled clinical study. Acta Obstet Gynecol Scand 1985;64:667–70 [DOI] [PubMed] [Google Scholar]
- 15.Williams MJ, Harris RI, Dean BC. Controlled trial of pyridoxine in the premenstrual syndrome. J Int Med Res 1985;13:174–9 [DOI] [PubMed] [Google Scholar]
- 16.Goei GS, Abraham GE. Effect of a nutritional supplement, optivite, on symptoms of premenstrual tension. J Reprod Med 1983;28:527–31 [PubMed] [Google Scholar]
- 17.London RS, Bradley L, Chiamori NY. Effect of a nutritional supplement on premenstrual symptomatology in women with premenstrual syndrome: a double-blind longitudinal study. J Am Coll Nutr 1991;10:494–9 [DOI] [PubMed] [Google Scholar]
- 18.Stewart A. Clinical and biochemical effects of nutritional supplementation on the premenstrual syndrome. J Reprod Med 1987;32:435–41 [PubMed] [Google Scholar]
- 19.Bertone-Johnson ER, Hankinson SE, Bendich A, Johnson SR, Willett WC, Manson JE. Calcium and vitamin D intake and risk of incident premenstrual syndrome. Arch Intern Med 2005;165:1246–52 [DOI] [PubMed] [Google Scholar]
- 20.Bertone-Johnson ER, Hankinson SE, Johnson SR, Manson JE. A simple method of assessing premenstrual syndrome in large prospective studies. J Reprod Med 2007;52:779–86 [PubMed] [Google Scholar]
- 21.Mortola JF, Girton L, Beck L, Yen SS. Diagnosis of premenstrual syndrome by a simple, prospective, and reliable instrument: the calendar of premenstrual experiences. Obstet Gynecol 1990;76:302–7 [PubMed] [Google Scholar]
- 22.Willett WC. Nutritional epidemiology. 2nd ed New York, NY: Oxford University Press, 1998 [Google Scholar]
- 23.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 1985;122:51–65 [DOI] [PubMed] [Google Scholar]
- 24.Salvini S, Hunter DJ, Sampson L, et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 1989;18:858–67 [DOI] [PubMed] [Google Scholar]
- 25.Jun HJ, Rich-Edwards J, Boynton-Jarrett R, Austin SB, Frazier AL, Wright R. Child abuse and smoking among young women: the importance of severity, accumulation, and timing. J Adolesc Health 2008;43:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gold EB, Bair Y, Block G, et al. Diet and lifestyle factors associated with premenstrual symptoms in a racially diverse community sample: Study of Women's Health Across the Nation (SWAN). J Womens Health (Larchmt) 2007;16:641–56 [DOI] [PubMed] [Google Scholar]
- 27.Masho SW, Adera T, South-Paul J. Obesity as a risk factor for premenstrual syndrome. J Psychosom Obstet Gynaecol 2005;26:33–9 [DOI] [PubMed] [Google Scholar]
- 28.Bertone-Johnson ER, Hankinson SE, Johnson SR, Manson JE. Cigarette smoking and the development of premenstrual syndrome. Am J Epidemiol 2008;168:938–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Institute of Medicine Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Institute of Medicine. Panel on Folate, Other B Vitamins, and Choline. Washington, DC: National Academy Press, 1998 [PubMed] [Google Scholar]
- 30.Halbreich U. Algorithm for treatment of premenstrual syndromes (PMS): experts' recommendations and limitations. Gynecol Endocrinol 2005;20:48–56 [DOI] [PubMed] [Google Scholar]
- 31.Jarvis CI, Lynch AM, Morin AK. Management strategies for premenstrual syndrome/premenstrual dysphoric disorder. Ann Pharmacother 2008;42:967–78 [DOI] [PubMed] [Google Scholar]
- 32.Johnson SR. Premenstrual syndrome, premenstrual dysphoric disorder, and beyond: a clinical primer for practitioners. Obstet Gynecol 2004;104:845–59 [DOI] [PubMed] [Google Scholar]
- 33.Thys-Jacobs S, Starkey P, Bernstein D, Tian J. Calcium carbonate and the premenstrual syndrome: effects on premenstrual and menstrual symptoms. Premenstrual Syndrome Study Group. Am J Obstet Gynecol 1998;179:444–52 [DOI] [PubMed] [Google Scholar]
- 34.Thys-Jacobs S. Micronutrients and the premenstrual syndrome: the case for calcium. J Am Coll Nutr 2000;19:220–7 [DOI] [PubMed] [Google Scholar]
- 35.Bertone-Johnson ER, Hankinson S, Johnson S, Manson J. Timing of alcohol use and the incidence of premenstrual syndrome and probable premenstrual dysphoric disorder. J Womens Health (Larchmt) 2009;18:1945–53 [DOI] [PMC free article] [PubMed] [Google Scholar]