Abstract
Aims
Infection is a serious complication of pacemaker (PM) systems. Although the rate of infection has been debated, the figures are largely unknown. We therefore studied the incidence of PM infection and its associated risk factors in the Danish population.
Methods and results
Since 1982, all PM implantation and removal procedures performed in Denmark have been prospectively recorded in the Danish Pacemaker Register. All patients (n = 46299) who underwent implantation between 1982 and 2007 were included. The total length of surveillance was 236 888 PM-years. The incidence of infection was calculated according to the total number of PM-years. The incidence of surgical site infection (≤365 days after PM implantation) was compared with later infection in first implant and replacement procedures. Multiple-record and multiple-event-per-subject proportional hazards analyses were used to identify the independent risk factors of PM infection. Surgical site infection occurred in 192 cases after first implantation (incidence rate 4.82/1000 PM-years), and in 133 cases after replacement (12.12/1000 PM-years). Infections occurring more than 365 days after the first implantation occurred in 153 cases (1.02/1000 PM-years), and in 118 cases after replacement (3.26/1000 PM-years). Independent factors associated with an increased risk of PM infection were a greater number of PM operations (including replacements), male sex, younger age, implantation during the earliest part of the study period, and absence of antibiotics (P< 0.001).
Conclusion
The overall risk of infection after PM implantation was low. A greater number of operations augmented the risk of infection. This should be taken into account when considering revisions of PM systems.
Keywords: Pacemakers, Complications, Infection, Registries
Introduction
Implantation of a permanent pacemaker (PM) has been widely accepted and implemented worldwide as the treatment of choice for bradyarrhythmias.1
Infection in a permanently implanted PM is a serious complication. It may occur either as a surgical site infection (SSI), occurring within 1 year after implantation,2 or as late-onset lead endocarditis. Pacemaker implantation rates are on the rise worldwide,1 and the population of patients living with a PM is growing. As a consequence, PM infections are also increasing. It has been suggested that the relative rates of infection are increasing;3,4 however, no large studies support this suggestion, and the overall statistics for PM infection remain largely unknown.
A number of small studies5–10 as well as one larger prospective study11 have identified risk factors for infection in permanent PM systems. However, the results of these studies are somewhat contradictory, and the risk factors for such infections have not been studied in a large cohort. The Danish Pacemaker Register (DPR), a prospective record of all implantations and removals of permanent PMs and PM-leads in Denmark since 1982, offers a unique opportunity to study the short- and long-term incidences of infection in permanently implanted PM systems, as well as their associated risk factors.
Methods
Study group
All Danish patients who underwent PM implantation or reoperation with changes in hardware between 1 January 1982 and 31 December 2007 were included in the study. Patients with an implanted cardioverter-defibrillator (ICD) were excluded from the study. A minor fraction had their first PM implanted before 1982; these patients were included at the time of their first PM replacement. Patients were followed from the first PM implantation after January 1982 until death, loss to follow-up, discontinuation of PM treatment, or until 31 December 2007. Each patient's vital status as of 31 December 2007 was obtained from the Central Population Registry.
The DPR contains data from all Danish patients who received a permanent PM after 1 January 1982. Data collection was based on reports from all 14 centres in Denmark that perform implantations of permanent PM systems. Five of these centres were high-volume university clinics, and nine were non-university clinics with lower patient volumes. The implantation practice in the study period has shifted from unipolar leads with passive fixation to predominantly bipolar leads with active fixation in the recent years. Cephalic cut-down was used for venous access in more than half of the patients and epicardial approach in <1%.
Pacemaker treatment in Denmark is standardized through a national reference program. All clinics adhered to these standards except for one, in which no preoperative antibiotics were administered when first-time PM implantations were performed. All clinics used preoperative antibiotics for patients undergoing PM replacements or reoperations. Local guidelines determined the type and dosage of antibiotics, but these data are not available in the study. All reoperations that involved changes to the implanted hardware were recorded in the register, while reoperations without hardware changes were not. The number of reoperations prior to actual implantation were counted for each patient and included in the analysis.
The reason for replacement or removal of a PM was recorded as ‘normal-end-of-life’, ‘technical failure’, or ‘surgical reason’. The latter category included the four sub-categories ‘infection’, ‘mechanical protrusion’, ‘erosion’, or ‘wound pain’, which were considered to be infected PM systems and constituted the primary outcome. The infections were not sub-classified as either wound infection or endocarditis, but all infections occurring within 1 year after PM implantation were considered to be SSIs in accordance with current guidelines.2 Infections occurring beyond this period were categorized as late infections.
The indication for implantation of a permanent PM system was recorded at the time of first implantation, according to a predefined classification. This was divided into four major groups: atrioventricular (AV) block, sinus node disease, atrial fibrillation with bradycardia, and ‘other’. The mode of pacing at first PM implantation was classified as single chamber AAI- or VVI-pacing, or dual chamber DDD pacing [including cardiac resynchronization therapy (CRT)]. A surrogate index for the duration and complexity of the procedure was constructed by counting the number of pieces of hardware implanted and removed during the same procedure.
Statistical analyses
Multiple-record and multiple-event per subject proportional hazards analyses were used to identify independent risk factors of PM infection. This model allowed the evaluation of time-dependent prognostic factors and multiple events per subject. It also allowed for gaps in the observations.
The factors considered in the univariate and multivariate analyses are shown in Table 2. All factors except sex and indication for PM implantation were considered to be time-dependent and were allowed to change with each new implantation.
Table 2.
Infection of pacemaker systems and its associated risk factors
| Variable | Devices | Device-years | Events | Univariate |
Multivariatea |
|||
|---|---|---|---|---|---|---|---|---|
| Hazard ratio95% CI | P-value | Hazard ratio95% CI | P-value | |||||
| Implantation | ||||||||
| First | 44 630 | 189 687 | 345 | 1 | <0.001 | b | ||
| Replacement | 12 027 | 47 201 | 251 | 2.79(2.38–3.28) | ||||
| Infection | ||||||||
| ≤365 days | 56 657 | 50 821 | 325 | 1 | <0.001 | 1 | <0.001 | |
| >365 days | 45 420 | 186 067 | 271 | 0.16(0.08–0.31) | <0.001 | 0.35(0.17–0.61) | ||
| Sex | ||||||||
| Male | 30 294 | 121 238 | 384 | 1 | <0.001 | 1 | <0.001 | |
| Female | 26 363 | 115 650 | 212 | 0.60(0.51–0.71) | 0.67(0.57–0.80) | |||
| Age | ||||||||
| 0–19 | 571 | 2499 | 22 | 1.63(0.96–2.78) | 1.41(0.83–2.38) | |||
| 20–49 | 2551 | 14 352 | 69 | 1 | <0.001 | 1 | <0.001 | |
| 50–59 | 3938 | 21 045 | 9 | 0.75(0.55–1.03) | 0.79(0.58–1.08) | |||
| 60–69 | 9527 | 46 552 | 150 | 0.62(0.47–0.83) | 0.68(0.51–0.90) | |||
| 70–79 | 19 186 | 86 155 | 181 | 0.39(0.29–0.51) | 0.44(0.34–0.59) | |||
| 80–89 | 17 812 | 59 396 | 89 | 0.24(0.17–0.32) | 0.29(0.21–0.39) | |||
| 90– | 3072 | 6888 | 6 | 0.11(0.05–0.25) | 0.31(0.06–0.30) | |||
| Year of implantation | ||||||||
| 1982–84 | 2033 | 14 357 | 63 | 1 | <0.001 | 1 | <0.001 | |
| 1985–89 | 7614 | 46 755 | 102 | 0.53(0.39–0.72) | 0.58(0.43–0.78) | |||
| 1990–94 | 8618 | 44 937 | 89 | 0.44(0.32–0.59) | 0.45(0.33–0.61) | |||
| 1995–99 | 10 693 | 53 120 | 105 | 0.41(0.31–0.56) | 0.42(0.31–0.56) | |||
| 2000–04 | 16 146 | 62 560 | 144 | 0.42(0.32–0.55) | 0.40(0.31–0.53) | |||
| 2005–07 | 11 553 | 15 159 | 93 | 0.65(0.47–0.89) | 0.60(0.44–0.82) | |||
| High volume centre | ||||||||
| No | 37 764 | 167 489 | 425 | 1 | 0.160 | |||
| Yes | 18 893 | 69 398 | 171 | 0.88(0.73–1.06) | ||||
| Preoperative antibiotics | ||||||||
| Yes | 51 473 | 213 911 | 516 | 1 | <0.001 | 1 | <0.001 | |
| No | 5184 | 22 976 | 80 | 2.27(1.76–2.91) | 2.33(1.81–2.98) | |||
| Pacing mode | ||||||||
| AAI | 4874 | 22 116 | 42 | 1 | 0.005 | |||
| VVI | 25 334 | 115 482 | 245 | 1.18(0.84–1.65) | ||||
| DDD | 26 449 | 99 289 | 309 | 1.49(1.07–2.08) | ||||
| Indication | ||||||||
| AV block | 24 854 | 103 365 | 322 | 1 | <0.001 | |||
| Sick sinus syndrome | 18 452 | 80 358 | 151 | 0.61(0.50–0.75) | ||||
| Atrial fibrillation | 7354 | 25 521 | 44 | 0.51(0.37–0.69) | ||||
| Other | 5997 | 27 644 | 79 | 0.89(0.76–1.26) | ||||
| Prior procedures | ||||||||
| 0 | 44 556 | 186 357 | 323 | 1 | <0.001 | 1 | <0.001 | |
| 1 | 9235 | 38 701 | 180 | 2.62(2.19–3.14) | 2.74 | (2.27–3.31) | ||
| 2 | 2035 | 8784 | 57 | 3.69(2.78–4.88) | 3.76 | (2.78–5.08) | ||
| 3 | 586 | 2268 | 20 | 5.80(4.04–8.33) | 5.49 | (3.71–8.13) | ||
| 4+ | 245 | 775 | 16 | 11.02(4.89–24.8) | 8.68 | (3.63–20.8) | ||
| Complexity of the procedurec | ||||||||
| 2 | 28 887 | 131 238 | 262 | 1 | <0.001 | |||
| 3 | 24 144 | 91 674 | 254 | 1.22(1.02–1.46) | ||||
| 4 | 3626 | 13 974 | 80 | 2.56(1.98–3.32) | ||||
| Prior infection | ||||||||
| No | 11 345 | 46 588 | 239 | 1 | 0.120 | |||
| Yes | 682 | 612 | 12 | 1.58(0.89–2.80) | ||||
Results of univariate and multivariate proportional hazards analyses.
aFor the multivariate analysis, only the risk factors in the final model are presented.
bThe variable ‘first pacemaker implantation vs. pacemaker replacement’ was excluded from the multivariate analyses, as a large number of the ‘prior procedures’ consisted of PM replacements.
cA surrogate index for the duration and complexity of the procedure was constructed by counting the number of hardware pieces implanted and removed during the same procedure.
Separate preliminary models were analysed for first implantations and replacements, as well as for early (≤365 days) and late (>365 days) infections. This analysis justified a model without interaction terms.
Patients were censored at the time of death or other termination of PM treatment, such as discontinuation of PM use upon upgrade to an ICD system or loss to follow-up. Results are presented as hazard ratios ±95% confidence intervals for the univariate analysis. For the multivariate analysis, only the risk factors in the final model are presented. All tests were two sided, and the P-value threshold for significance was 5%.
Incidence of PM infection was calculated as the rate of infection per 1000 device-days.12 Statistical analyses were performed using the R software (version 2.7.1 for Windows).
Results
Patients
Patient characteristics at the time of first PM implantation are shown in Table 1.
Table 1.
Patient characteristics
| Variable | Patients at first pacemaker implant (n =44630) |
|---|---|
| Sex (n, %) | |
| Male | 24 023, 53.8% |
| Female | 20 607, 46.2% |
| Age (median, 25–75% interquartile range) | 76, 68–82 |
| Pacing mode (n, %) | |
| AAI | 4084, 9.2% |
| VVI | 20 140, 45.1% |
| DDD | 19 504, 43.7% |
| CRT | 902, 2.0% |
| Indication (n, %) | |
| AV block | 19 408, 43.5% |
| Sick sinus syndrome | 14 598, 32.7% |
| Atrial fibrillation | 6258, 14.0% |
| Other | 4366, 9.8% |
| Complexity of the procedurea | |
| 2 | 24 210, 54.2% |
| 3 | 19 603, 43.9% |
| 4+ | 817, 0.8% |
aA surrogate index for the duration and complexity of the procedure was constructed by counting the number of hardware pieces implanted and removed during the same procedure.
A total of 46 299 patients underwent one or more PM implantations during the study period. The first implantation was performed in 44 630 patients during the study period, and prior to the start of the study period in 1669 patients. One or more PM replacements were carried out in 8380 patients. A total of 2498 patients underwent one or more PM reoperations consisting of lead replacements without PM replacement. The total follow-up was 236 888 device-years.
During the study period, 26 552 deaths occurred. The number of patients lost to follow-up was 170, and PMs were removed without replacement in 342 patients. The remaining 19 235 patients were living with an implanted PM at the end of the study period. The total number of PMs implanted during the study period was 56 657.
A subgroup of 902 patients in the DDD group received a CRT system as a first time implant. In total, 1127 CRT devices were implanted.
Infections
A total of 596 PMs were removed due to infection: 345 after the first PM implantation (incidence 1.82/1000 PM-years) and 251 after replacement (incidence 5.32/1000 PM-years).
‘Infection’ was listed as the reason for removal of these PMs in 461 cases (77.3%); a minority of removals were attributed to other clinical presentations of infection, such as ‘mechanical protrusion’ in 77 cases (12.9%), ‘erosion’ in 44 cases (7.4%), and ‘wound pain’ in 14 cases (2.3%).
In 542 of these patients, one PM removal was performed due to infection, and 27 patients underwent two PM removals.
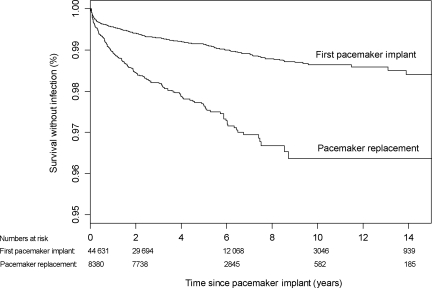
The time to PM infection is illustrated by Kaplan–Meier plots in Figure 1.
Figure 1.
Kaplan–Meier plot of the time to infection after first pacemaker implantation (n= 44631) and after pacemaker replacements (n= 8380).
Surgical site infection (≤365 days after PM implantation)2 occurred in 192 cases after the first PM implantation (incidence rate 4.82/1000 PM-years), and in 133 cases after PM replacement (12.12/1000 PM-years). Infections after 365 days post-implantation occurred in 153 cases after first PM implantation (1.02/1000 PM-years), and in 118 cases after PM replacement (3.26/1000 PM-years).
The risk of SSI was significantly higher than the risk of infection after 365 days post-implantation for both first implantations and replacement procedures. The risk of SSI relative to the risk of later infection did not differ significantly between first implantations and replacement procedures.
Risk factors associated with infection
Univariate proportional hazards analyses indicated that all potential risk factors studied were significant, except for high-volume centre vs. low-volume centre and for prior infection (Table 2). In summary, the following factors were associated with an increased risk of PM removal due to infection: PM replacement vs. first PM implantation, male sex, younger age, implantation during the earliest part of the study period, absence of prophylactic antibiotics (but only for first PM implantations), dual chamber pacing mode, AV block as an indication for pacing, greater number of PM operations, and greater complexity of the procedure.
In the multivariate analyses, ‘prior procedures’ was included as a variable. A large number of these prior procedures consisted of PM replacements, and therefore the variable ‘first PM implantation vs. PM replacement’ was excluded from the multivariate analyses. In the final multivariate statistical model, pacing mode, indication for pacing, and complexity of the procedure were not found to be significantly associated with a risk of PM infection. Thus, the following risk factors were independently associated with an increased risk of PM removal due to infection in the final multivariate model: male sex, younger age, implantation during the earliest part of the study period, absence of prophylactic antibiotics (during the first PM implantation), and greater number of PM operations (Table 2).
Discussion
To our knowledge, the present study represents the largest population-based study of PM infections and associated risk factors to date and reports reliable rates for the risk of infection after first PM implantations and PM replacements. Repeated operative procedures after the first PM implantation were associated with a substantial incremental risk of PM infection. Conversely, female sex, older age, and preoperative antibiotics given at the first PM implantations were associated with a lower risk of later PM infection. The pacing mode, indication for pacing, and complexity of the procedure were not independently associated with the risk of later PM infection. Although the majority of infections occurred within the first year of follow-up, a large number of infections were found to occur during the late follow-up period, >1 year post-implantation. This very late onset of infection is consistent with the findings from other studies that consider extended follow-up periods8–10 and with the current understanding of slowly progressing, implant-related infection.13 The defined 1 year period post-implant surgery for SSI may be more or less arbitrary,2 and in our study we were not able to distinguish between clinical SSI and lead endocarditis. The significant number of infections occurring later than 1 year after implantation highlights the continued need for long-term clinical follow-up of PM patients.
Rates of infection
The incidence of PM in our population was 1.82 per 1000 PM-years after the first implantation. This is similar to the rate of 1.9 per 1000 device-years reported in a smaller, retrospective, population-based cohort study.9 Other epidemiological studies that include long-term follow-up have calculated cumulative rates per patient or device and report infection rates of 2.210 and 1.6%,8 respectively. Studies examining shorter follow-up periods report infection rates of only 0.6811 and 1%.14 However, these studies failed to report weighted incidences.12 In contrast to our study, these prior studies also reported infections after implantation of ICD systems. The effect of this difference is unclear; the rate of infection in ICD systems has been reported to be similar to the rates observed for PM systems,8,10,11 with the exception of one study that demonstrated a higher risk of infection in ICD patients.11 This is likely explained by the higher proportion of abdominal, non-transvenous ICD systems.
The incidence of SSI was 4.82/1000 PM-years after first PM implantation and 12.12/1000 PM-years after PM replacement. This is comparable with the rates observed in other fields of prosthesis implant surgery, as a recent extensive review of 1707 cases of hip and knee arthroplasty demonstrated SSI rates of 1.32 and 1.83%, respectively.15 Although the setting described in the review differs from that of our study and there is a general lack of data on SSI in implant surgery, we find our incidences of SSI in PM implantation to be acceptable.
Based on estimates from Medicare3 and the National Hospital Discharge Survey,4 the incidence of infections in implanted devices is assumed to be rising. This assumption could not be confirmed in the present population-based study, which demonstrated a fairly constant rate of infection after implantation of permanent PM systems over the past 20 years. The rate of infection after implantation of more complex CRT systems in patients with severe heart failure within the last decade may be higher, but it has not yet been studied in suitably large patient cohorts.
Prior procedures
The substantially elevated risk of infection after PM replacements and other repeated procedures observed in the present study has been reported previously.8,10,11,16 A recent randomized trial found a higher rate of infection after first implantations compared with after PM replacements.17 In this trial, however, follow-up was carried out for only 6 months, and the number of infected patients reached 13 in the two treatment arms. Four of these patients presented with superficial infections that were treated with antibiotics. The increased risk of infection after repeated procedures argues strongly that industry should improve PM batteries and that physicians should increase device longevity by appropriately programming PM parameters. Furthermore, the increased risk of infection after repeated procedures should be considered in the decision-making process when handling device recalls,18 which are a common reason for premature repeated procedures. In each patient, the benefits of replacing the hardware should be balanced with the increased risk of device infection.
At first glance, the higher risk of infection after repeated procedures (most often simple PM replacements) is unexpected, as these procedures most often involve only a minor surgical revision and are short-lasting compared with first implantations. It is generally recognized, however, that revision surgery is an important risk factor for the infection of an implanted prosthesis or device.19 Our findings could likely be explained by the fact that PM pockets can be colonized by bacteria, even in the absence of any initial clinical signs of infection.20 In combination with the limited immunological response of the fibrous and poorly vascularized PM pocket that is opened during replacement or revision procedures,21 the rapid formation of a microbial biofilm22 by either latent or perioperative inoculation of pathogens may be favoured, thereby allowing pocket infection.
Preoperative antibiotics
No single, sufficiently powered randomized trial has been performed to evaluate the effects of preoperative antibiotics on the long-term incidence of infection in PM treatment. A meta-analysis performed in 1998 revealed that preoperative administration of prophylactic antibiotics is effective in reducing the risk of infection,23 and antibiotic prophylaxis before PM implantation has been recommended for the last decade.2,24 The omission of systemically administered prophylactic antibiotics during the first implantation was confirmed to be an important risk factor for infection in the present study, whereas prophylactic antibiotics were used in all reoperations. Other studies11,17,25 confirming the beneficial effects of antibiotics, irrespective of the dosing regimen used, have included both first PM implantations and reoperations. To date, however, no study has separately analysed the effects on first implantations vs. reoperations. The immune response is altered in the device pocket as a consequence of the presence of a foreign body,21,26 and antimicrobial agents have been shown to have a limited effect on biofilm-associated bacterial infections.27 It has therefore been suggested that the future antimicrobial strategy employed in implantation surgery should include local antimicrobial applications,28 although such an approach has not been tested in prospective trials.
Other procedure-related factors
A higher rate of infection was observed during the earliest period, from 1982 to 1984, than during the subsequent 23 years. A possible explanation for these findings is that these procedures were often shared by thoracic surgeons and cardiologists, thus making the procedure more complicated.
In contrast, three potentially important procedure-related factors—the size of the implanting centre, the complexity of the procedure, and the number of leads—did not influence the rate of infection. This is consistent with the results of previous studies.10,11 These results underscore the importance of other procedure-related factors, namely the use of preoperative antibiotics and repeated procedures.
In Denmark, implantation of PMs is performed only in hospitals with a fairly high implantation volume, and the majority of procedures are carried out by experienced cardiologists.29 Thus, the present findings regarding higher- and lower-volume centres cannot necessarily be generalized to clinics with limited experience and/or a very low implantation volume (< 50 PM implantations per year).
Patient factors
We found that male sex was an important risk factor, consistent with the findings of Catanchin.8 Surprisingly, we observed an inverse relationship between increasing age and the risk of infection, with the rate of infection highest in children and adolescents and declining with age. Prior studies8–11 have not demonstrated this relationship between age and infection rate, most likely due to the presence of low numbers of children and adolescents in their study populations. Young patients are more likely to possess non-transvenous systems, which bear a higher rate of infection.30 For reasons that remain unclear, the declining risk of infection with age was sustained in older age groups. Factors such as the presence of less firm subcutaneous connective tissue, which would permit less traumatic formation of the PM pocket, as well as a less aggressive immune response against low-virulence bacteria with increasing age could theoretically play a role. Another possibility is that physicians might be more reluctant to perform a full and potentially hazardous extraction procedure in elderly, more fragile PM patients, and may therefore pursue a more conservative treatment.
Limitations
The present study is a retrospective analysis, and thus bears the inherent limitations of such studies. The data, however, were reported prospectively to the register, reducing some of these limitations. With a 25-year-long period of reporting and follow-up, we find it very unlikely that the data are flawed by systematic bias caused by single operators or clinics. The DPR, however, has been subject to an external audit documenting the quality of the data.29
Any reporting of complications to a register is subject to underreporting, as well as to inappropriate classification of the causal explanation at the time of PM removal. The infection rates observed therefore represent minimal numbers, with a risk of underestimating the problem. Furthermore, the DPR was not exclusively set up to monitor device infections, and several potential risk factors such as renal dysfunction and diabetes mellitus were not available in the current analysis. The large number of patients and the completeness of follow-up should counterbalance the inherent weakness of registry-based studies.
We were not able to distinguish whether removal of the PM system was due to infection arising from a device pocket infection or from a bloodstream infection of the intravascular portion of the system. However, data suggest an overlap between these two events.5,31
Conclusion
The incidence of infection after first PM implantation was 1.82/1000 PM-years in this nationwide cohort of 46 299 consecutive PM patients with long-term follow-up. The rate of infection was significantly higher after PM replacement procedures, for which 5.32/1000 PM-years was observed. Repeated operative procedures after the first PM implantation were associated with a substantial incremental risk of PM infection. Female sex, older age, and administration of preoperative antibiotics in the first PM implantation were associated with a decreased risk of later PM infection. Pacing mode, indication for pacing, and procedure complexity were not independently associated with the risk of later PM infection.
Funding
The study was sponsored by The Danish Pacemaker Register; a self-owned and independent institution. Funding to pay the Open Access publication charges for this article was provided by The Danish Pacemaker Register.
Conflict of interest: none declared.
References
- 1.Mond HG, Irwin M, Ector H, Proclemer A. The world survey of cardiac pacing and cardioverter-defibrillators: calendar year 2005 an International Cardiac Pacing and Electrophysiology Society (ICPES) project. Pacing Clin Electrophysiol. 2008;31:1202–1212. doi: 10.1111/j.1540-8159.2008.01164.x. doi:10.1111/j.1540-8159.2008.01164.x. [DOI] [PubMed] [Google Scholar]
- 2.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–278. doi: 10.1086/501620. doi:10.1086/501620. [DOI] [PubMed] [Google Scholar]
- 3.Cabell CH, Heidenreich PA, Chu VH, Moore CM, Stryjewski ME, Corey GR, Fowler VG., Jr Increasing rates of cardiac device infections among Medicare beneficiaries: 1990–1999. Am Heart J. 2004;147:582–586. doi: 10.1016/j.ahj.2003.06.005. doi:10.1016/j.ahj.2003.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Voigt A, Shalaby A, Saba S. Rising rates of cardiac rhythm management device infections in the United States: 1996 through 2003. J Am Coll Cardiol. 2006;48:590–591. doi: 10.1016/j.jacc.2006.05.016. doi:10.1016/j.jacc.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 5.Klug D, Wallet F, Lacroix D, Marquie C, Kouakam C, Kacet S, Courcol R. Local symptoms at the site of pacemaker implantation indicate latent systemic infection. Heart. 2004;90:882–886. doi: 10.1136/hrt.2003.010595. doi:10.1136/hrt.2003.010595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chamis AL, Peterson GE, Cabell CH, Corey GR, Sorrentino RA, Greenfield RA, Ryan T, Reller LB, Fowler VG., Jr. Staphylococcus aureus bacteremia in patients with permanent pacemakers or implantable cardioverter-defibrillators. Circulation. 2001;104:1029–1033. doi: 10.1161/hc3401.095097. doi:10.1161/hc3401.095097. [DOI] [PubMed] [Google Scholar]
- 7.Eberhardt F, Bode F, Bonnemeier H, Boguschewski F, Schlei M, Peters W, Wiegand UK. Long term complications in single and dual chamber pacing are influenced by surgical experience and patient morbidity. Heart. 2005;91:500–506. doi: 10.1136/hrt.2003.025411. doi:10.1136/hrt.2003.025411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Catanchin A, Murdock CJ, Athan E. Pacemaker infections: a 10-year experience. Heart Lung Circ. 2007;16:434–439. doi: 10.1016/j.hlc.2007.02.097. doi:10.1016/j.hlc.2007.02.097. [DOI] [PubMed] [Google Scholar]
- 9.Uslan DZ, Sohail MR, St Sauver JL, Friedman PA, Hayes DL, Stoner SM, Wilson WR, Steckelberg JM, Baddour LM. Permanent pacemaker and implantable cardioverter defibrillator infection: a population-based study. Arch Intern Med. 2007;167:669–675. doi: 10.1001/archinte.167.7.669. doi:10.1001/archinte.167.7.669. [DOI] [PubMed] [Google Scholar]
- 10.Lekkerkerker JC, van Nieuwkoop C, Trines SA, van der Bom JG, Bernards A, van de Velde ET, Bootsma M, Zeppenfeld K, Jukema JW, Borleffs JW, Schalij MJ, van Erven L. Risk factors and time delay associated with cardiac device infections: Leiden device registry. Heart. 2009;95:715–720. doi: 10.1136/hrt.2008.151985. doi:10.1136/hrt.2008.151985. [DOI] [PubMed] [Google Scholar]
- 11.Klug D, Balde M, Pavin D, Hidden-Lucet F, Clementy J, Sadoul N, Rey JL, Lande G, Lazarus A, Victor J, Barnay C, Grandbastien B, Kacet S. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: results of a large prospective study. Circulation. 2007;116:1349–1355. doi: 10.1161/CIRCULATIONAHA.106.678664. doi:10.1161/CIRCULATIONAHA.106.678664. [DOI] [PubMed] [Google Scholar]
- 12.McKibben L, Horan T, Tokars JI, Fowler G, Cardo DM, Pearson ML, Brennan PJ. Guidance on public reporting of healthcare-associated infections: recommendations of the Healthcare Infection Control Practices Advisory Committee. Am J Infect Control. 2005;33:217–226. doi: 10.1016/j.ajic.2005.04.001. doi:10.1016/j.ajic.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Uslan DZ. Infections of electrophysiologic cardiac devices. Expert Rev Med Devices. 2008;5:183–195. doi: 10.1586/17434440.5.2.183. doi:10.1586/17434440.5.2.183. [DOI] [PubMed] [Google Scholar]
- 14.Leon AR, Abraham WT, Curtis AB, Daubert JP, Fisher WG, Gurley J, Hayes DL, Lieberman R, Petersen-Stejskal S, Wheelan K. Safety of transvenous cardiac resynchronization system implantation in patients with chronic heart failure: combined results of over 2,000 patients from a multicenter study program. J Am Coll Cardiol. 2005;46:2348–2356. doi: 10.1016/j.jacc.2005.08.031. doi:10.1016/j.jacc.2005.08.031. [DOI] [PubMed] [Google Scholar]
- 15.Bolon MK, Hooper D, Stevenson KB, Greenbaum M, Olsen MA, Herwaldt L, Noskin GA, Fraser VJ, Climo M, Khan Y, Vostok J, Yokoe DS. Improved surveillance for surgical site infections after orthopedic implantation procedures: extending applications for automated data. Clin Infect Dis. 2009;48:1223–1229. doi: 10.1086/597584. doi:10.1086/597584. [DOI] [PubMed] [Google Scholar]
- 16.Marschall J, Hopkins-Broyles D, Jones M, Fraser VJ, Warren DK. Case-control study of surgical site infections associated with pacemakers and implantable cardioverter-defibrillators. Infect Control Hosp Epidemiol. 2007;28:1299–1304. doi: 10.1086/520744. doi:10.1086/520744. [DOI] [PubMed] [Google Scholar]
- 17.Oliveira JC, Martinelli M, Nishioka SAD, Varejao T, Uipe D, Pedrosa AAA, Costa R, Danik SB. Efficacy of antibiotic prophylaxis before the implantation of pacemakers and cardioverter-defibrillators: results of a large, prospective, randomized, double-blinded, placebo-controlled trial. Circ Arrhythm Electrophysiol. 2009;2:29–34. doi: 10.1161/CIRCEP.108.795906. doi:10.1161/CIRCEP.108.795906. [DOI] [PubMed] [Google Scholar]
- 18.Costea A, Rardon DP, Padanilam BJ, Fogel RI, Prystowsky EN. Complications associated with generator replacement in response to device advisories. J Cardiovasc Electrophysiol. 2008;19:266–269. doi: 10.1111/j.1540-8167.2007.01047.x. doi:10.1111/j.1540-8167.2007.01047.x. [DOI] [PubMed] [Google Scholar]
- 19.Esposito S, Leone S. Prosthetic joint infections: microbiology, diagnosis, management and prevention. Int J Antimicrob Agents. 2008;32:287–293. doi: 10.1016/j.ijantimicag.2008.03.010. doi:10.1016/j.ijantimicag.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Pichlmaier M, Marwitz V, Kuhn C, Niehaus M, Klein G, Bara C, Haverich A, Abraham WR. High prevalence of asymptomatic bacterial colonization of rhythm management devices. Europace. 2008;10:1067–1072. doi: 10.1093/europace/eun191. doi:10.1093/europace/eun191. [DOI] [PubMed] [Google Scholar]
- 21.Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20:86–100. doi: 10.1016/j.smim.2007.11.004. doi:10.1016/j.smim.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Subbiahdoss G, Kuijer R, Grijpma DW, van der Mei HC, Busscher HJ. Microbial biofilm growth vs. tissue integration: ‘the race for the surface’ experimentally studied. Acta Biomater. 2009;5:1399–1404. doi: 10.1016/j.actbio.2008.12.011. doi:10.1016/j.actbio.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 23.Da Costa A, Kirkorian G, Cucherat M, Delahaye F, Chevalier P, Cerisier A, Isaaz K, Touboul P. Antibiotic prophylaxis for permanent pacemaker implantation: a meta-analysis. Circulation. 1998;97:1796–1801. doi: 10.1161/01.cir.97.18.1796. [DOI] [PubMed] [Google Scholar]
- 24.Baddour LM, Bettmann MA, Bolger AF, Epstein AE, Ferrieri P, Gerber MA, Gewitz MH, Jacobs AK, Levison ME, Newburger JW, Pallasch TJ, Wilson WR, Baltimore RS, Falace DA, Shulman ST, Tani LY, Taubert KA. Nonvalvular cardiovascular device-related infections. Circulation. 2003;108:2015–2031. doi: 10.1161/01.CIR.0000093201.57771.47. doi:10.1161/01.CIR.0000093201.57771.47. [DOI] [PubMed] [Google Scholar]
- 25.Sohail MR, Uslan DZ, Khan AH, Friedman PA, Hayes DL, Wilson WR, Steckelberg JM, Stoner SM, Baddour LM. Risk factor analysis of permanent pacemaker infection. Clin Infect Dis. 2007;45:166–173. doi: 10.1086/518889. doi:10.1086/518889. [DOI] [PubMed] [Google Scholar]
- 26.Schierholz JM, Beuth J. Implant infections: a haven for opportunistic bacteria. J Hosp Infect. 2001;49:87–93. doi: 10.1053/jhin.2001.1052. doi:10.1053/jhin.2001.1052. [DOI] [PubMed] [Google Scholar]
- 27.del Pozo JL, Patel R. The challenge of treating biofilm-associated bacterial infections. Clin Pharmacol Ther. 2007;82:204–209. doi: 10.1038/sj.clpt.6100247. doi:10.1038/sj.clpt.6100247. [DOI] [PubMed] [Google Scholar]
- 28.Zilberman M, Elsner JJ. Antibiotic-eluting medical devices for various applications. J Control Release. 2008;130:202–215. doi: 10.1016/j.jconrel.2008.05.020. doi:10.1016/j.jconrel.2008.05.020. [DOI] [PubMed] [Google Scholar]
- 29.Moller M, Arnsbo P, Asklund M, Christensen PD, Gadsboll N, Svendsen JH, Klarholt E, Kleist KE, Mortensen PT, Pietersen A, Simonsen EH, Thomsen PE, Vesterlund T, Wiggers R. Quality assessment of pacemaker implantations in Denmark. Europace. 2002;4:107–112. doi: 10.1053/eupc.2002.0234. doi:10.1053/eupc.2002.0234. [DOI] [PubMed] [Google Scholar]
- 30.Lai KK, Fontecchio SA. Infections associated with implantable cardioverter defibrillators placed transvenously and via thoracotomies: epidemiology, infection control, and management. Clin Infect Dis. 1998;27:265–269. doi: 10.1086/514673. doi:10.1086/514673. [DOI] [PubMed] [Google Scholar]
- 31.Klug D, Wallet F, Kacet S, Courcol RJ. Detailed bacteriologic tests to identify the origin of transvenous pacing system infections indicate a high prevalence of multiple organisms. Am Heart J. 2005;149:322–328. doi: 10.1016/j.ahj.2004.07.032. doi:10.1016/j.ahj.2004.07.032. [DOI] [PubMed] [Google Scholar]