ABSTRACT
Purpose: To further investigate the construct validity of the Community Balance and Mobility Scale (CB&M), developed for ambulatory individuals with traumatic brain injury (TBI).
Methods: A convenience sample of 35 patients with TBI (13 in-patients, 22 outpatients) was recruited. Analyses included a comparison of CB&M and Berg Balance Scale (BBS) admission and change scores and associations between the CB&M and measures of postural sway, gait, and dynamic stability; the Community Integration Questionnaire (CIQ); and the Activities-specific Balance Confidence (ABC) Scale.
Results: Mean admission scores on the BBS and the CB&M were 53.6/56 (SD=4.3) and 57.8/96 (SD=23.3) respectively. Significant correlations were demonstrated between the CB&M and spatiotemporal measures of gait, including walking velocity, step length, step width, and step time; measures of dynamic stability, including variability in step length and step time; and the ABC (p<0.05). Significant correlations between the CB&M and CIQ were revealed with a larger data set (n=47 outpatients) combined from previous phases of research.
Conclusions: In patients with TBI, the CB&M is less susceptible to a ceiling effect than the BBS. The construct validity of the CB&M was supported, demonstrating associations with laboratory measures of dynamic stability, measures of community integration, and balance confidence.
Key Words: balance, brain injuries, posture, mobility limitations, outcome assessment
RÉSUMÉ
Objectif : Approfondir les recherches afin d'établir la validité de l'échelle communautaire d'équilibre et de mobilité (Community Balance and Mobility Scale, ou CB&M) créée pour les individus ambulatoires avec traumatisme crânien.
Méthode : Un échantillon de commodité de 35 patients (13 patients hospitalisés, 22 patients externes) avec traumatisme crânien a été constitué. Les analyses réalisées comprenaient la comparaison à l'admission à la CB&M avec l'échelle d'équilibre de Berg (BBS), des changements de cote et des associations entre la CB&M et les mesures de balancement postural, de démarche et de stabilité dynamique, avec le questionnaire d'intégration communautaire (CIQ) et l'échelle ABC de confiance à l'équilibre lors d'activités précises.
Résultats : La moyenne des cotes à l'admission sur les échelles BBS et CB&M a été de 53,6/56 (écart-type=4,3) et de 57,8/96 (écart-type=23,3), respectivement. Des corrélations considérables ont été démontrées entre la CB&M et les mesures spatiotemporelles de la démarche, notamment la vélocité de la marche, la longueur des pas, la durée des pas; les mesures de stabilité dynamique, y compris les variations dans la longueur et la durée des pas; et l'ABC (p<0,05). Des corrélations considérables entre la CB&M et le CIQ ont été constatées dans un ensemble de données plus large (n=47 patients externes) combiné aux phases précédentes de la recherche.
Conclusions : Chez les patients qui ont subi un traumatisme crânien, la CB&M est moins susceptible de plafonner que l'échelle BBS. La validité construite de la CB&M est appuyée et démontre les associations entre les mesures en laboratoire de la stabilité dynamique, les mesures d'intégration communautaire et la confiance en l'équilibre.
Mots clés : équilibre, évaluation des résultats, limites à la mobilité, posture, traumatisme crânien
INTRODUCTION
Traumatic brain injury (TBI) is a pressing public-health and medical problem, affecting approximately 10 million people worldwide each year.1 In Canada, 6,000 new, permanently disabling TBIs are sustained each year, and TBI is the primary cause of death and disability for people under the age of 40.2 For the brain-injury survivor, therefore, the activity limitations and participation restrictions can be long-term and complex, because of the initial age of the population at the time of injury and the diversity and degree of sequelae. If evidence-based rehabilitative services are to be provided to this population, it is critical that clinical outcome measures appropriate to the patient's degree of impairment, activity, and participation be developed and used.
Many individuals achieve independent ambulation in the early stages of recovery from brain injury.3,4 In a study of 116 patients with severe TBI, Katz et al.3 found that independence in ambulation was achieved at a mean recovery time of 5.7±4.3 weeks. Similarly, Swaine and Sullivan4 reported that 50% of subjects with TBI were able to ambulate independently for 25 m on both even and uneven ground within 6 weeks. Nonetheless, subjective complaints of balance and walking difficulties have been documented as one of the most persistent and common long-term concerns, even many years post-injury,5,6 which indicates that evaluation of balance and mobility needs further exploration.
Surprisingly few studies have examined dynamic stability and gait after TBI. Some studies, however, have identified a group of individuals with TBI who have persistent balance and mobility deficits despite being able to walk independently and having high scores on standard clinical balance measures7,8 or normal neurological and musculoskeletal clinical exams.9,10 Using laboratory measures, these studies have demonstrated that subjects with TBI walk significantly more slowly9,10 and with decreased step lengths7 relative to their healthy peers. In addition, McFadyen et al. reported that when walking in a more complex environment requiring obstacle crossings, individuals with TBI demonstrated a more “cautious” gait, with significantly slower crossing speeds for trail limb versus lead limb and a tendency toward increased foot clearances.7 Patients with TBI were also found to have significantly greater centre-of-mass displacement and velocity in the mediolateral direction when walking on level ground9 and during obstacle crossings10 relative to healthy peers. Increased variability in step time and step length when walking at a fast pace or with eyes closed has also been observed.8 The above-mentioned studies suggest that dynamic instability and locomotor dyscontrol may persist after TBI. These deficits may be exacerbated by more challenging conditions or more complex environments and may not be captured by existing clinical measures of balance and mobility.
We developed the Community Balance and Mobility Scale (CB&M) in response to the needs of clinical practice to identify postural instability and evaluate change following intervention in ambulatory individuals with TBI who are functioning at a high level with respect to independence and capacity for velocity and distance.11 The CB&M is a 13-item, 6-point scale that measures performance of more challenging balance and mobility tasks that require speed, precision, accuracy, and sequencing of movement components representative of underlying motor skills necessary for function and participation within the community. Items include tandem walking, rapid step-ups, running with an abrupt stop, transitioning from forward to backward walking, and walking while looking laterally (see Appendix for the full list of CB&M items).
Measurement properties of the scale have been investigated in three phases. In the first phase, content validity was verified by patients with TBI and clinicians. Discriminant validity of the CB&M was also demonstrated by the scale's ability to differentiate patients along the continuum of care.11 Comparisons of CB&M scores with preferred pace (r=0.53, p<0.001) and maximal walking velocity (r=0.64, p<0.001) supported the preliminary analysis of the scale's construct validity. Further, patients who scored higher (n=11) or lower (n=6) than 50/96 on the CB&M demonstrated significantly different scores on the Community Integration Questionnaire (p=0.004), which suggests that there may be a balance score threshold below which community participation may be reduced.11
In the second phase, we demonstrated that the CB&M can be administered with high levels of intrarater, interrater, and test–retest reliability and of internal consistency (intra-class correlation coefficients [ICCs]=0.977, 0.977, 0.975, α=0.96, respectively).11
The goal of this third phase of research was to further establish the construct validity of the CB&M. Specifically, the objectives were
to determine whether the CB&M is better able than a commonly used clinical measure of balance (the Berg Balance Scale) to capture change in balance and mobility for a higher-functioning population; and
to determine the degree of association between CB&M scores and other measures thought to have related theoretical constructs, including laboratory measures of postural control, gait, and dynamic stability and measures of balance confidence and community participation.
METHODS
This research was approved by the Office of Research Services, University of Toronto, and by the Research Ethics Board of the Toronto Rehabilitation Institute.
Participants
Thirty-five subjects were recruited for this study from neuro-rehabilitation in-patient and outpatient services at the Toronto Rehabilitation Institute and from two private community clinics. Inclusion criteria were a diagnosis of TBI, age between 18 and 60 years, adequate ability to follow verbal commands, and provision of informed consent to participate. Because the purpose of the CB&M is to evaluate higher-functioning individuals, patients included were those who, at a minimum, could ambulate indoors with supervision, with or without a gait aid.
Measures
Berg Balance Scale
Originally designed to evaluate balance impairment in elderly individuals with and without neurological conditions, the Berg Balance Scale (BBS) is widely used in clinical settings with many patient populations.12 The measure consists of 14 items rated on a scale from 0 to 4, indicating progressive levels of performance, for a maximum score of 56. The items include maintaining static positions (standing unsupported in usual stance, with feet together, in tandem and unilateral stance) and basic functional tasks (transferring; reaching forward and picking up an object from the floor). The BBS has proven reliability, with intra-class correlation coefficients of 0.91 and 0.99 for interrater reliability in older adults and patients with stroke respectively, and 0.92 and 0.98 for test–retest reliability in older adults and patients with stroke respectively.12 Studies have also established the content, concurrent, and construct validity of the scale in the elderly and in patients with stroke.12,13
Laboratory Measures of Postural Control and Gait
Force-plate data were acquired at a temporal resolution of 200 Hz by a portable force-plate system (AMTI, Watertown, MA). Subjects completed three trials of 30 seconds' duration for the following six tasks: standard stance and tandem stance, right foot forward and left foot forward, all under both eyes open and eyes closed conditions. The force-plate measures of postural sway collected were centre-of-pressure (COP) amplitude and velocity, which were calculated for each of the six conditions. COP amplitude was defined as the root mean square (RMS) of the two-dimensional (anteroposterior and mediolateral) displacement; COP velocity was defined as the length of the two-dimensional COP path divided by the trial duration.
Spatial and temporal parameters of gait were recorded using a pressure-sensitive mat (GAITRite, CIR Systems Inc., Clifton, NJ), which has been found to be a reliable and valid method of measuring gait.14 The mat is 4.6 m long and 0.9 m wide, with a spatial resolution of 1.27 cm and a temporal resolution of 100 Hz. Subjects were asked to walk over the mat three times, wearing their regular footwear, in the following five conditions: at a preferred pace, at a fast pace, with eyes closed, walking and looking left, and walking and looking right. These conditions were included to provide a range of challenging walking conditions against which the CB&M scores could be compared. The spatial and temporal measures of gait collected were walking velocity and mean and variability of step length, step time, and step width.
Studies have suggested that there is a positive relationship between increased step-to-step variability and reduced control of dynamic stability.15,16 We therefore used the gait-variability findings collected from the pressure-sensitive mat as a marker of postural dyscontrol during walking. Variability of step length, time, and width were calculated using the coefficient of variation (CV=standard deviation÷mean×100),17 treating data from the three trials as one continuous walk from which one mean and standard-deviation (SD) value was calculated for each condition.
Measures of Community Participation and Balance Confidence
The Community Integration Questionnaire (CIQ) is a 15-item measure developed for persons with TBI to assess the individual's participation in his or her community environment.18 The CIQ has three sub-scales specific to home integration, social integration, and productive activity. The instrument has established test–retest reliability, internal consistency, and construct validity; scores are able to differentiate between individuals with TBI and individuals with no apparent disabilities and between persons with TBI living independently and those living in a supported community situation or in an institution.18
The Activities-specific Balance Confidence (ABC) Scale is a 16-item self-report questionnaire.19 Individuals are asked to rate their degree of confidence from 0% (no confidence) to 100% (extremely confident) in their ability to perform common activities within the home and community, such as using stairs, getting into and out of a car, and walking on icy sidewalks. The average of the item scores yields a score ranging from 0 to 100; higher scores reflect greater degrees of balance self-efficacy. The scale demonstrates good test–retest reliability and high internal consistency and is able to discriminate between fallers and non-fallers and between low- and high-mobility groups.19
The CIQ and ABC are intended to reflect abilities, self-efficacy, and participation in the community environment. These measures were therefore administered only to the community-dwelling outpatient participants.
Design and Procedures
The clinical physical therapists who participated in this research as evaluators completed a 2-hour training session on the use of the CB&M. To ensure consistency of scoring, the training included a review and group discussion of a videotaped assessment of a patient with TBI.
To investigate objective 1, the CB&M and the BBS were administered to each participant by his or her treating physical therapist on admission to the in-patient or outpatient care setting and again at discharge or 10 weeks after the initial assessment, whichever was earlier. To investigate objective 2, assessments were completed at one time point only. In-patient and outpatient participants completed postural control and gait assessments on the force plate and GAITRite systems within 5 days of the admission CB&M assessment. As noted above, the CIQ and ABC were administered to outpatients only, at the time of initial assessment.
Additional patient characteristics collected were age, gender, rehabilitation setting (in-patient or outpatient), and time since injury. Measures of severity of TBI, such as Glasgow Coma Scale and Post-Traumatic Amnesia scores, were not consistently available and therefore were not included. Data on participants' functional ambulation status, including level of independence in indoor and outdoor environments, use of gait aids, and walking endurance, were collected from physical therapy assessments.
Data Analysis
Descriptive statistics were used to identify means and standard deviations of all outcome variables. Standardized response means (the mean change score divided by the standard deviation of the change score)20 were calculated for both the BBS and the CB&M to quantify the ability of these measures to capture change.
All data were tested for normality. Pearson product–moment correlations were used to analyze the degree of association between CB&M total scores and force-plate measures of postural sway, spatiotemporal measures of gait, and the ABC. Spearman rank correlations were used to analyze associations between the CB&M and the CIQ, given the ordinal nature of the latter measure. Correlation coefficients (r) <0.25 were considered to indicate no or little relationship; those between 0.25 and 0.50, a fair relationship; those between 0.50 and 0.75, a moderate to good relationship; and values <0.75, an excellent correlation.21 SigmaStat 3.0 statistical software (Systat Software Inc., San Jose, CA) was used for data analysis.
RESULTS
Description of the Sample
A total of 35 patients with TBI (13 in-patients and 22 community-dwelling outpatients) were tested. Participant characteristics are summarized in Table 1. The group's mean preferred walking velocity approached age-referenced healthy values, and the group's mean maximal walking velocity was within age-referenced healthy values;22 88% and 56% of the total sample were able to walk independently indoors and outdoors, respectively, while 85% of the total sample were able to walk distances of more than 500 m.
Table 1.
Characteristics of the Total Sample and Sub-sets of In-Patient and Outpatient Participants
| In-Patient (n=13) |
Outpatient (n=22) |
All (n=35) |
|
|---|---|---|---|
| Age (mean±SD years) | 26.2±9.7 | 30.1±11.4 | 28.7±10.6 |
| Gender (Male:Female) | 10:3 | 15:7 | 25:10 |
| Time post-injury (mean±SD weeks) | 7.3±3.2 | 42.2±58.8 | 29.0±48.6 |
| Walking Status | |||
| Indoor Ambulation (n)* | |||
| Supervision required | 3 | 1 | 4 |
| Independent with SPC | 2 | 1 | 3 |
| Independent with no aid | 8 | 17 | 25 |
| Outdoor Ambulation (n)* | |||
| Supervision required | 11 | 3 | 14 |
| Independent with SPC | 1 | 1 | 2 |
| Independent with no aid | 1 | 15 | 16 |
| Mean walking velocity (m/sec) | |||
| Self-paced | 1.05±0.28 | 1.19±0.37 | 1.14±0.34 |
| Maximal pace | 1.54±0.48 | 1.95±0.65 | 1.80±0.62 |
| Endurance** | |||
| <100 m | 1 | 1 | 2 |
| <500 m | 2 | 1 | 3 |
| <1,000 m | 5 | 3 | 8 |
| >1,000 m | 5 | 15 | 20 |
SPC=single-point cane
Outpatient missing data (n=3)
Outpatient missing data (n=2)
The number of participants included in the analyses varied for the two objectives because of missing data and the initial unavailability of certain laboratory technology; 26 participants were included in the analysis comparing the CB&M to the BBS, and 27 in analyses comparing the CB&M to the lab measures.
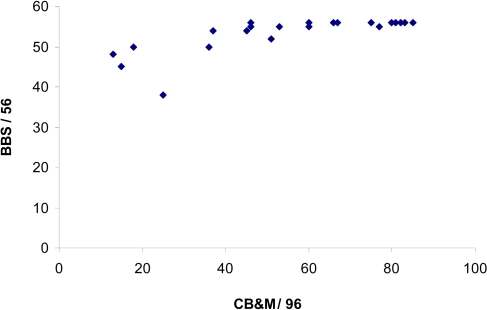
Comparison of the Community Balance and Mobility Scale to the Berg Balance Scale
Mean time between admission and discharge BBS and CB&M balance assessments was 7.6 weeks (SD=4.8 weeks). BBS and CB&M scores at admission are displayed in Figure 1. Scores are near or at the ceiling for the BBS (mean=53.6/56, SD=4.3) for this study population, in contrast to the wide distribution of CB&M admission scores (mean=57.8/96, SD=23.3). Change scores from admission to discharge were 1.2 (SD 3.1) for the BBS versus 13.0 (SD 9.9) for the CB&M. Standardized response means for the BBS and CB&M were 0.40 and 1.3 respectively.
Figure 1.
Relationship between Berg Balance Scale (BBS) and Community Balance and Mobility Scale (CB&M) total scores for 26 patients with TBI admitted into a rehabilitation setting
Association of Community Balance and Mobility Scale Scores with Measures of Postural Sway, Gait, and Dynamic Stability
The mean CB&M score for the 27 subjects who were evaluated with lab technology was 65.8/96 (SD=19.2).
There were no significant correlations between CB&M total scores and measures of COP amplitude or velocity in any of the six tasks. The relationship between balance scores and COP amplitude within the tandem stance (right leg forward) task in the eyes closed condition approached significance (r=−0.70, p=0.056), but only a few participants (n=8) were able to complete this more challenging task.
Spatiotemporal values of gait for the participants are displayed in Table 2; associations between the CB&M and these measures are displayed in Table 3. There were significant correlations of a moderate to good or excellent magnitude between CB&M scores and velocity, step length, step width, and step time across all walking conditions.
Table 2.
Mean Spatiotemporal Measures of Gait*
| Gait Variable | Preferred Pace | Fast Pace |
|---|---|---|
| Velocity (m/s) | 1.15±0.33 | 1.87±0.60 |
| Step Length (cm) | 66.22±13.45 | 79.34±15.63 |
| Step Width (cm) | 10.35±3.22 | 15.77±26.80 |
| Step Time (s) | 0.68±0.44 | 0.52±0.35 |
| Step-Length Variability (% CV) | 4.63±2.18 | 5.28±4.39 |
| Step-Width Variability (% CV) | 29.01±10.29 | 34.96±14.23 |
| Step-Time Variability (% CV) | 4.75±3.20 | 7.07±4.59 |
CV=coefficient of variation
Values reflect group means±standard deviations for 27 participants.
Table 3.
Relationship between Community Balance and Mobility (CB&M) Scale Total Scores and Spatiotemporal Measures of Gait (n=27)
| Gait Variable | Pearson Correlations with CB&M Scale Scores* |
||||
|---|---|---|---|---|---|
| Preferred Pace r (p) |
Fast Pace r (p) |
Eyes Closed r (p) |
Walk Look Left r (p) |
Walk Look Right r (p) |
|
| Velocity | 0.77 (<0.001) | 0.87 (<0.001) | 0.67 (<0.001) | 0.84 (<0.001) | 0.83 (<0.001) |
| Step length | 0.80 (<0.001) | 0.80 (<0.001) | 0.73 (<0.001) | 0.86 (<0.001) | 0.84 (<0.001) |
| Step width | −0.45 (0.018) | −0.38 (0.048) | −0.48 (0.011) | −0.53 (0.004) | −0.58 (0.002) |
| Step time | −0.55 (0.003) | −0.61 (<0.001) | −0.52 (0.006) | −0.54 (0.004) | −0.53 (0.004) |
| Step-length variability | −0.66 (<0.001) | −0.14 (0.47) | −0.58 (0.002) | −0.51 (0.006) | −0.66 (<0.001) |
| Step-width variability | 0.28 (0.20) | 0.30 (0.13) | −0.46 (0.017) | −0.49 (0.010) | 0.31 (0.12) |
| Step-time variability | −0.70 (<0.001) | −0.14 (0.47) | −0.51 (0.007) | −0.68 (<0.001) | −0.69 (<0.001) |
Bolded values indicate significant correlations.
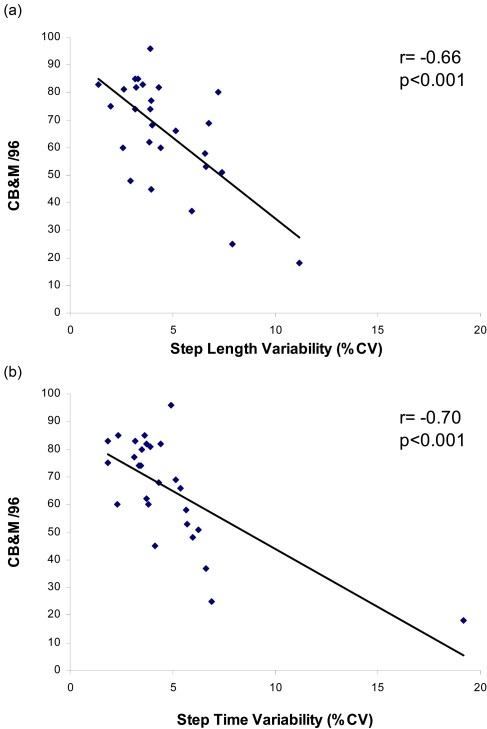
Significant negative correlations of a moderate to good magnitude were also demonstrated between CB&M scores and measures of dynamic instability, including variability in step length and step time, across all walking conditions except fast pace. Figure 2 displays these associations for step-length variability and step-time variability in the preferred pace condition. With the outlier removed (see Figure 2b), the correlation between total CB&M scores and step-time variability remained significant and of a moderate to good magnitude (r=−0.66, p<0.001). Significant negative correlations between CB&M balance scores and variability in step width were also demonstrated in the eyes closed and walking and looking left conditions.
Figure 2.
Relationship between Community Balance & Mobility Scale (CB&M) total scores and variability (%CV) in step length (a) and step time (b) for 27 participants in preferred pace walking conditions
Given the above-mentioned associations between CB&M scores and both velocity and step-to-step variability, we also conducted a follow-up analysis to examine the association between the latter two variables. Velocity during preferred pace conditions was significantly correlated to both step-time variability (r=−0.63, p<0.001) and step-length variability (r=−0.59, p=0.001).
Association of Community Balance and Mobility Scale Scores with Measures of Community Participation and Balance Confidence
Eighteen of the 22 outpatients completed the CIQ and ABC. Mean CB&M, CIQ, and ABC scores were 71.7/96 (SD=16.6), 16.2/29 (SD=6.6), and 77.4/100 (SD=14.1) respectively.
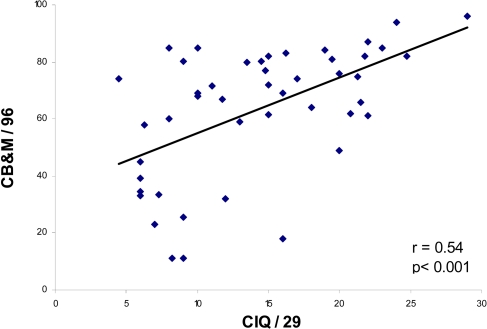
The correlation between CB&M and CIQ scores was not significant (r=0.41, p=0.09). The CIQ was collected as an indicator of community participation during previous phases of research that explored the measurement properties of the CB&M.11 There were no significant differences between the outpatients in this study (n=18) and those involved in previous phases of research to whom the CIQ was administered (n=29) in terms of age (p=0.24), gender (p=0.38), time post-injury (p=0.69), or preferred walking velocity (p=0.07). The groups also demonstrated similar levels of functional walking status: 79% of current participants and 84% of participants in previous phases were able to walk outdoors independently with no aid, and 90% and 86%, respectively, were able to walk distances of more than 500 m. Given the similar populations, and to increase the power of any potential association not evident from the small outpatient sample size of the current study, we performed a follow-up analysis with a larger combined data set consisting of outpatient participants from all phases (n=47).
A significant correlation of a moderate to good magnitude (r=0.54, p<0.001) was demonstrated between the CB&M and CIQ scores using the larger data set. Inspection of the scatter plot (see Figure 3) also suggested that individuals with CB&M scores above 45 had a wider range of CIQ scores, whereas the cluster of individuals with CB&M scores of 45 or less had a lower and more limited range of CIQ scores. Post hoc t-tests revealed a significant difference (p<0.001) in CIQ scores between participants with CB&M scores below 45 (n=11, mean CIQ score=8.4/29, SD=3.1) and those with scores above 45 (n=36, mean CIQ score=16.0/29, SD=5.9).
Figure 3.
Relationship between Community Balance and Mobility Scale (CB&M) scores and Community Integration Questionnaire (CIQ) scores for 47 community-dwelling patients with traumatic brain injury
Initial analysis did not show a correlation between CB&M scores and ABC scores (r=0.03, p=0.90). After the removal of data for a participant who had a low CB&M score (18/96) but a high ABC score (98/100), however, a significant relationship between CB&M and ABC scores emerged (r=0.60, p=0.011).
DISCUSSION
The ability to balance is critical to the performance of most activities of daily living and a determinant of ambulatory activity level.23 Problems with balance and mobility are reported to be one of the most common and long-standing concerns for community-dwelling individuals following TBI.5,6 Objective laboratory measures of postural control and gait7,9,10 have demonstrated that postural instability and locomotor dyscontrol persist in ambulatory individuals after TBI, even where there are minimal or no observable neurological deficits, and may become more apparent during challenging tasks or in challenging environments.7,8,10 The CB&M was developed for use in clinical settings to evaluate the complex locomotor skills underlying the more challenging tasks required for full functioning in the community.
The present study has established that the CB&M was better able than the commonly used BBS to capture change in this group of patients with TBI. Construct validity of the CB&M is further supported by the association of CB&M scores with performance on specific measures of dynamic stability and gait and with measures of patients' perceptions of community integration and balance confidence.
The minimal values for walking velocity and endurance required for functional community ambulation have been identified as 1.3–1.4 m/s and 480–593 m24,25 respectively. The majority of individuals with TBI in this study, in both in-patient and outpatient settings, met or surpassed these criteria for functional community ambulation. From a clinical perspective, therefore, they would be deemed to be at a high level of functional mobility.
Our patient sample scored at the ceiling of the BBS but exhibited a wide distribution of CB&M scores. This indicates that there is a risk of false negative results when using the BBS with this population; the BBS was originally designed to assess a lower level of ability. Our findings support the use of the CB&M, with its more challenging items, to reveal and quantify deficits that persist even in the highly ambulatory individual.
Construct validity was further examined by determining the relationship between CB&M scores and laboratory measures of postural control and gait. The lack of statistically significant associations between CB&M scores and static measures of postural sway suggests that the challenges and underlying mechanisms of postural control may be different in standing behaviours than in walking behaviours and, therefore, that measures of static task conditions may not effectively evaluate dynamic stability.26,27
In contrast, the relationships between the CB&M and most spatiotemporal measures of gait were statistically significant and of a moderate to good or excellent magnitude. A significant relationship between CB&M scores and gait velocity was also demonstrated during earlier, preliminary investigations of validity.11 It is not clear why the correlations are somewhat stronger in the present study, since the characteristics of the populations in the current research and those in previous phases were similar. Regardless, the present study confirms that there is a strong relationship between CB&M scores and gait velocity.
In the absence of measures appropriate for the individuals with high levels of functional mobility, clinicians often use velocity as an overall measure of walking capacity and preparedness for community mobility. In the present study, we noted that participants' walking velocities approached or fell within healthy age-referenced values22 and met criteria for functional community ambulation.24,25 The distribution of CB&M scores, however, indicated a wide range of balance and mobility deficits for these same participants. This may suggest that the CB&M is more sensitive than the surrogate measure of walking velocity in capturing deficits in this TBI group; however, this question requires further study.
Gait variability is thought to reflect the degree of control of the centre of mass over the base of support when walking. The relationship between CB&M scores and measures of variability in step length and step time were significant and of moderate to good magnitude in most walking conditions. This finding supports the underlying construct of the CB&M as a measure of higher-level dynamic balance.
Interestingly, no significant association between CB&M scores and step-to-step variability was demonstrated in the fast pace walking condition. We originally anticipated that the increased challenge of this condition would expose a greater degree of dynamic instability, and this hypothesis was partially supported by the increased mean step-to-step variability values in the fast pace versus preferred pace walking conditions. The increase in between-subject variability for fast pace conditions, however, may be noteworthy. It is possible that an association between the CB&M and step-to-step variability in fast pace conditions exists but was masked by the increased between-subject variability demonstrated in these conditions.
Follow-up analysis also revealed a significant negative relationship between velocity and step-to-step variability, as well as a strong correlation between velocity and CB&M balance scores. We therefore cannot rule out the possibility that the above-mentioned association between CB&M scores and step-to-step variability was a result of these variables' relationship with gait speed: participants' CB&M scores may have been influenced by both dynamic stability and speed of performance.
An important aspect of demonstrating the validity of the CB&M was to demonstrate a relationship with measures of community integration and balance self-efficacy. Positive correlations were found between the CB&M and the CIQ; a stronger and statistically significant association was revealed when values were obtained from a larger pooled data set of outpatients. A significant correlation between CB&M and ABC scores was also demonstrated when an outlier was removed. Therapist feedback suggested that this outlying data point (combining high balance confidence with a low balance score) may have reflected the reduced insight specific to this participant.
The positive associations between the CB&M and the CIQ and between the CB&M and the ABC support the validity of the underlying constructs of the CB&M, wherein individuals demonstrating higher-level balance and mobility skills tend to be those who report higher degrees of community integration and balance confidence in performing activities of daily living both within and outside the home. Of interest is the potential threshold of CB&M scores below which the individual's community integration, as measured by the CIQ, may be limited. The differences in community integration between those at higher CB&M scores and those at lower CB&M scores became apparent in preliminary investigations of the measurement properties of the CB&M, and these findings were supported using the larger data set of outpatients across all three phases of research. Although this question requires further investigation, CB&M scores may be useful in identifying those at risk of poor community participation.
During the course of our research, another measure with a similar purpose, the High-Level Mobility Assessment Tool (HiMAT),28 has been developed to evaluate balance and mobility in the higher-functioning individual with TBI, which confirms the clinical need for this type of measure. The CB&M and the HiMAT appear to share some similar tasks; the major differences may lie in the underlying constructs and the approach to measurement. The final version of the HiMAT scoring criteria quantifies the task through speed and distance of performance,29 whereas the CB&M evaluation includes speed and distance as well as quantification of behaviours such as precision (e.g., foot placement on a line), path trajectory (e.g., when walking and looking), and balance strategies used (e.g., change in support strategy). It would be interesting for future research to compare and contrast these measures more thoroughly.
In this study we have used measures of gait, dynamic instability, and participation as proxy criterion standards in the absence of a gold standard. Moderate to good and excellent correlations between these measures and the CB&M have been demonstrated, the strength of which supports the constructs of the CB&M. The associations do not suggest, however, that these measures are interchangeable. We have limited our focus in this study to the statistical significance of associations, but the clinical significance of the CB&M scores in relation to concepts of community mobility and participation is an important area for future study.
LIMITATIONS
The sample of convenience used in the present study may not be representative of all ambulatory individuals after TBI, and participants may be higher-functioning than patients commonly seen for rehabilitation to address balance or gait retraining. Further investigations of the CB&M should include patients who are less independent in walking and community mobility.
The order of the laboratory measures of standing and walking was not randomized; therefore, the results may have been limited by a learning or fatigue effect. However, we do not believe that this significantly affected the results, given that participants were characterized as having high levels of walking endurance (i.e., 85% of participants were able to walk distances greater than 500 m). Further, the positive correlations between CB&M scores and spatiotemporal measures of gait were of similar magnitude across all test conditions.
The study also included limited information about the type and severity of participants' brain injury, for example, as measured by the Glasgow Coma Scale (GCS). However, since a previous study reported that the GCS is a poor predictor of future locomotor ability,7 we feel that it was appropriate to characterize the participants by their ambulatory status at the time of testing.
CONCLUSIONS
The findings of this study support the CB&M as a valid measure for detecting persistent balance and mobility deficits and evaluating change in the ability of ambulatory patients with TBI who are returning to community living. While the CB&M was better able than the BBS to capture change in balance for this population, future research should focus on establishing clinically important change values. Studies are also underway to establish healthy age-referenced values in order to assist clinicians in interpreting scores at this higher level of ability.
Key Messages
What Is Already Known on This Topic
Deficits in dynamic stability and locomotor control may persist in individuals with traumatic brain injury (TBI) who have minimal findings on clinical examinations. These deficits may not be captured by existing clinical measures of balance and mobility. The Community Balance and Mobility Scale (CB&M) was developed in response to the needs of clinical practice to identify high-level balance problems and evaluate change following intervention in this population. Initial phases of research have established the CB&M's intrarater, interrater, and test–retest reliability and aspects of its validity.
What This Study Adds
This study further established the construct validity of the CB&M. The CB&M was less susceptible to a ceiling effect than the commonly used Berg Balance Scale and better able to capture change in an ambulatory population with TBI. CB&M scores demonstrated significant associations with laboratory measures of dynamic stability and gait and with self-report measures of participation and confidence in the community. This study's findings support the CB&M as a valid measure for detecting dynamic instability and evaluating the change in ability of patients with TBI returning to community living.
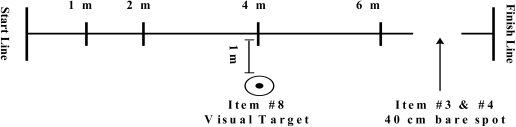
Appendix:
Community Balance and Mobility Scale Track and Items
 |
|---|
| 1. Unilateral Stance (R & L)* Stand 45 seconds on one leg in a steady & coordinated manner. |
| 2. Tandem Walk Walk 7 consecutive heel-toe steps in good alignment. |
| 3. 180° Tandem Pivot Pivot 180 degrees, beginning & ending in tandem stance. |
| 4. Lateral Foot Scooting (R & L) Pivot laterally on one foot to traverse 40 cm. |
| 5. Hopping Forward (R & L) Hop twice on one foot to travel forwards 1 m and maintain stability on landing. |
| 6. Crouch & Walk* Pick up an object from the floor while in the midst of walking forward and proceed without pausing. |
| 7. Lateral Dodging* Rapidly cross one foot over the other with precise foot placement while moving laterally along the track and respond to an unexpected command to reverse direction. |
| 8. Walking & Looking (R & L)* Maintain gaze on a target placed lateral to the track, as one walks forwards and past the target and attempt to maintain a straight trajectory. |
| 9. Running with Controlled Stop* Run for 8 metres and control an abrupt stop. |
| 10. Forward to Backward Walking* Rapid change in direction by turning at mid-way point of track to switch from forward to backward walking. |
| 11. Walk, Look & Carry (R & L)* As per #8 but performed while carrying weighted bags. |
| 12. Descending Stairs |
| 13. Step-Ups (R & L)* Step rapidly on & off a step. |
Items are timed.
R=right; L=left
Source: Howe JA, Inness EL, Venturini A, Williams JI, Verrier MC. The Community Balance and Mobility Scale: a balance measure for individuals with traumatic brain injury. Clin Rehabil. 2006;20(10):885–95. © 2006 SAGE Publications. Reprinted by permission of SAGE.
Inness EL, Howe J, Niechwiej-Szwedo E, Jaglal SB, McIlroy WE, Verrier MC. Measuring balance and mobility after traumatic brain injury: validation of the Community Balance and Mobility Scale (CB&M). Physiother Can. 2011;preprint. doi:10.3138/ptc.2009-45
REFERENCES
- 1.Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: a global perspective. Neurorehabil. 2007;22:341–53. [PubMed] [Google Scholar]
- 2.Hamilton Brain Injury Association. Brain injury facts [Internet] Hamilton: The Association; n.d.. [cited 2010 July 5]. Available from: http://www.hbia.ca/brain_injury.html. [Google Scholar]
- 3.Katz DI, White DK, Alexander MP, Klein RB. Recovery of ambulation after traumatic brain injury. Arch Phys Med Rehabil. 2004;85:865–9. doi: 10.1016/j.apmr.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 4.Swaine BR, Sullivan SJ. Longitudinal profile of early motor recovery following severe traumatic brain injury. Brain Inj. 1996;10:347–66. doi: 10.1080/026990596124368. doi: 10.1080/026990596124368. [DOI] [PubMed] [Google Scholar]
- 5.Hillier SL, Sharpe MH, Metzer J. Outcomes 5 years post-traumatic brain injury with further reference to neurophysical impairment and disability. Brain Inj. 1997;11:661–75. doi: 10.1080/026990597123214. [DOI] [PubMed] [Google Scholar]
- 6.Dean S, Colantonio S, Ratcliff G, Chase S. Clients' perspectives on problems many years after traumatic brain injury. Psychol Rep. 2000;86:653–8. doi: 10.2466/pr0.2000.86.2.653. [DOI] [PubMed] [Google Scholar]
- 7.McFadyen BJ, Swaine B, Dumas D, Durand A. Residual effects of a traumatic brain injury on locomotor capacity: a first study of spatiotemporal patterns during unobstructed and obstructed walking. J Head Trauma Rehabil. 2003;18:512–25. doi: 10.1097/00001199-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Niechiej-Szwedo E, Inness EL, Howe JA, Jaglal S, McIlroy WE, Verrier MC. Changes in gait variability during different challenges to mobility in patients with traumatic brain injury. Gait Posture. 2007;25:70–7. doi: 10.1016/j.gaitpost.2006.01.002. doi: 10.1016/j.gaitpost.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Basford JR, Chou L, Kaufman K, Brey RH, Walker A, Malec JF, et al. An assessment of gait and balance deficits after traumatic brain injury. Arch Phys Med Rehabil. 2003;84:343–9. doi: 10.1053/apmr.2003.50034. doi: 10.1053/apmr.2003.50034. [DOI] [PubMed] [Google Scholar]
- 10.Chou LS, Kaufman KR, Walker-Rabatan AE, Brey RH, Basford JR. Dynamic instability during obstacle crossing following traumatic brain injury. Gait Posture. 2004;20:245–54. doi: 10.1016/j.gaitpost.2003.09.007. doi: 10.1016/j.gaitpost.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 11.Howe JA, Inness EL, Venturini A, Williams JI, Verrier MC. The Community Balance and Mobility Scale: a balance measure for individuals with traumatic brain injury. Clin Rehabil. 2006;20:885–95. doi: 10.1177/0269215506072183. [DOI] [PubMed] [Google Scholar]
- 12.Berg K, Wood-Dauphinee SL, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27:27–36. [PubMed] [Google Scholar]
- 13.Berg K, Wood-Dauphinee SL, Williams JI, Maki BE. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl.2):S7–11. [PubMed] [Google Scholar]
- 14.Bilney B, Morris M, Webster K. Concurrent related validity of the GAITRite walkway system for quantification of the spatial and temporal parameters of gait. Gait Posture. 2003;17:68–74. doi: 10.1016/s0966-6362(02)00053-x. doi: 10.1016/S0966-6362(02)00053-X. [DOI] [PubMed] [Google Scholar]
- 15.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear? J Am Geriatr Soc. 1997;45:313–20. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 16.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–6. doi: 10.1053/apmr.2001.24893. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 17.Zar JH. Biostatistical analysis. 2nd ed. Englewood Cliffs (NJ): Prentice Hall; 1984. [Google Scholar]
- 18.Willer B, Rosenthal M, Kreutzer JS, Gordon WA, Rempel R. Assessment of community integration following rehabilitation for traumatic brain injury. J Head Trauma Rehabil. 1993;8:75–87. doi: 10.1097/00001199-199308020-00009. [Google Scholar]
- 19.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A-Biol. 1995;50A:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 20.Wright JG, Young NL. A comparison of different indices of responsiveness. J Clin Epidemiol. 1997;50:239–46. doi: 10.1016/s0895-4356(96)00373-3. doi: 10.1016/S0895-4356(96)00373-3. [DOI] [PubMed] [Google Scholar]
- 21.Colton T. Statistics in medicine. Boston: Little, Brown; 1974. [Google Scholar]
- 22.Oberg T, Karsznia A, Oberg K. Basic gait parameters: reference data for normal subjects, 10–79 years of age. J Rehabil Res Dev. 1993;30:210–23. [PubMed] [Google Scholar]
- 23.Michael KM, Allen JK, Macko RF. Reduced ambulatory activity after stroke: the role of balance, gait and cardiovascular fitness. Arch Phys Med Rehabil. 2005;86:1552–6. doi: 10.1016/j.apmr.2004.12.026. doi: 10.1016/j.apmr.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 24.Lerner-Frankiel MB, Vargas S, Brown M, Krusell L, Schoneberger W. Functional community ambulation: what are your criteria? Clin Manage. 1986;6:12–5. [Google Scholar]
- 25.Robinett CS, Vondran MA. Functional ambulation velocity and distance requirements in rural and urban communities. Phys Ther. 1988;9:1371–3. doi: 10.1093/ptj/68.9.1371. [DOI] [PubMed] [Google Scholar]
- 26.Wade LD, Canning CG, Fowler V, Velmingham K, Baguley IJ. Changes in postural sway and performance of functional tasks during rehabilitation after traumatic brain injury. Arch Phys Med Rehabil. 1997;78:1107–11. doi: 10.1016/s0003-9993(97)90136-2. doi: 10.1016/S0003-9993(97)90136-2. [DOI] [PubMed] [Google Scholar]
- 27.Weinstein CJ, Gardner ER, McNeal DR, Bartos PS, Nicholson DE. Standing balance training: effect on balance and locomotion in hemiparetic adults. Arch Phys Med Rehabil. 1989;70:755–62. [PubMed] [Google Scholar]
- 28.Williams G, Robertson V, Greenwood K, Goldie P, Morries ME. The High-level Mobility Assessment Tool (HiMAT) for traumatic brain injury, part 1: item generation. Brain Inj. 2005;19:925–32. doi: 10.1080/02699050500058687. doi: 10.1080/02699050500058687. [DOI] [PubMed] [Google Scholar]
- 29.Williams G, Robertson V, Greenwood K, Goldie P, Morries ME. The High-level Mobility Assessment Tool (HiMAT) for traumatic brain injury, part 2: content validity and discriminability. Brain Inj. 2005;19:833–43. doi: 10.1080/02699050500058711. doi: 10.1080/02699050500058711. [DOI] [PubMed] [Google Scholar]