ABSTRACT
Purpose: To describe the performance of the pillow that participants usually slept on with respect to retiring and waking cervico-thoracic symptoms, pillow comfort, and sleep quality.
Methods: Participants (n=106) were systematically recruited for a field trial comparing their own pillow and five trial pillows. Participants provided daily retiring and waking symptom reports and sleep-quality and pillow-comfort ratings prospectively for 1 week on each pillow. Linear and logistic regression models were used to investigate the relationship between pillow use, age, gender, sleep quality, pillow comfort, and waking and temporal (overnight) symptom reports.
Results: No waking symptoms were reported by 42.5% of participants on their own pillow. Regular waking symptoms, failure to relieve retiring symptoms, uncomfortable pillows, and/or poor-quality sleep were reported by over 50% of participants. All participants who reported poor sleep quality also reported poor pillow comfort. Pillow-comfort reports were not related to any waking symptom report; however, reports of poor sleep quality were significantly related to waking cervical stiffness (adjusted odds ratio [AOR]=4.3 [Confidence Interval (CI): 1.3–15.6]) and scapula pain (AOR=6.1 [CI: 1.1–31.6]). Feather pillow users provided consistently low reports of pillow comfort and sleep quality.
Conclusion: Many participants appear to have made poor pillow choices, as poor sleep quality, low pillow comfort, and waking symptoms were common. Further research is required to understand why people choose particular pillows to sleep on, as well as to identify the best fit between person and pillow to optimize sleep quality and reduce waking symptoms.
Key Words: cervical spine, headache, pain, pillow, sleep quality, stiffness, temporal change
RÉSUMÉ
Objectif : Décrire le rendement de l'oreiller sur lequel les participants dorment habituellement en ce qui a trait aux symptômes cervicothoraciques d'éveil et de retrait, au confort de l'oreiller et à la qualité du sommeil.
Méthode : Les participants (n=106) ont été systématiquement recrutés pour un essai sur le terrain dont l'objectif était de comparer leur propre oreiller à cinq autres modèles qu'ils essaieraient. Les participants ont préparé des rapports quotidiens sur leurs symptômes d'éveil et de sommeil et sur la qualité de leur sommeil, et ils devaient évaluer le confort de chaque oreiller de manière prospective pendant une semaine. Des modèles de régression linéaires et logistiques ont été utilisés pour étudier la relation entre l'utilisation de l'oreiller, l'âge, le sexe, la qualité du sommeil, le confort de l'oreiller, l'éveil et les rapports temporels de symptômes (sur toute une nuit).
Résultats : Aucun symptôme d'éveil n'a été signalé chez 42,5 % des participants lors de l'utilisation de leur propre oreiller. Des symptômes d'éveil réguliers, une incapacité à soulager les symptômes de retrait, un oreiller inconfortable et un sommeil de mauvaise qualité ont été signalés par 50 % des participants. Tous les participants qui ont déclaré avoir un sommeil de piètre qualité ont dit aussi avoir un oreiller peu confortable. Les rapports sur le confort des oreillers n'étaient pas liés à quelque rapport d'éveil que ce soit ; toutefois, des rapports qui signalaient un sommeil de mauvaise qualité étaient liés de manière significative à une raideur cervicale à l'éveil (ratio d'incidence approché [RIA] de 4,3 [intervalle de confiance (IC) de 1,3–15,6]) et à une douleur à l'omoplate (RIA de 6,1 [IC de 1,1–31,6]). Les utilisateurs d'oreillers de plumes fournissaient constamment des rapports de faible confort de l'oreiller et de piètre qualité de sommeil.
Conclusion : Plusieurs participants semblent avoir fait un mauvais choix d'oreiller, puisqu'un sommeil de piètre qualité, de l'inconfort avec leur oreiller et des symptômes d'éveil étaient communs. Plus de recherches seront nécessaires pour comprendre pourquoi ces personnes ont choisi ces oreilles pour dormir, et pour identifier le meilleur oreiller pour chaque personne, afin d'optimiser la qualité de leur sommeil et de réduire les symptômes d'éveil.
Mots clés : changement temporel, colonne cervicale, douleur, maux de tête, oreiller, qualité du sommeil, raideur
INTRODUCTION
Anecdotally, patients often report being unhappy with the performance of the pillow they sleep on. Health care practitioners are often asked by patients to recommend pillows that will improve the quality of their sleep and/or alleviate waking cervical symptoms.1 There is a growing body of evidence on the interaction between the human body and sleeping surfaces; however, this has not led to clear recommendations on the best fit between pillows, mattresses, and people.2–5
With a myriad of pillow designs and a wealth of unsubstantiated information about different pillow types currently available, patients and health care providers may well be confused about which pillow to choose and what waking symptoms should be expected following a “usual” night's sleep. There is a slowly growing body of evidence on sleeping posture, pillow performance and comfort, and waking symptoms that largely supports the individual nature of satisfaction with specific sleeping surfaces.6–14
Our large-scale telephone survey reported a high frequency of waking symptoms reported by generally healthy people in a “usual” week, sleeping on a range of pillow types.15,16 We recently compared the frequency of waking cervical pain during a random-allocation field trial of five new commonly used pillows (polyester, foam regular, foam contour, feather, and latex) and participants' own pillows. The trial pillows produced clearly different frequencies of prospectively reported waking pain, again indicating the variable fit between person and pillow even when using new pillows. New latex, polyester, and foam contour pillows produced consistently lower frequencies of waking cervical pain than new foam regular or feather pillows.17 The findings of this trial provide further support for the variable performance with respect to waking pain of pillows on which individuals sleep. By comparing the responses of a sub-group of subjects who participated in both the survey and the experimental study, we found that waking symptoms, pillow comfort, and sleep quality attributable to participants' own pillows were reported consistently over time.17 Participants mostly discarded foam regular and feather pillows for another pillow type within 18 months, while polyester, foam contour, and latex pillows showed greater longevity.17
This paper reports the frequency of waking symptoms (cervical pain, stiffness, headache, and scapula pain), overnight (temporal) change in these symptoms, pillow comfort, and sleep quality when participants slept on their own pillow (presumed to be their pillow of choice). We hypothesized that fewer waking symptoms would be reported and that retiring symptoms would be relieved overnight in participants who reported a comfortable “own” pillow and a good night's sleep.
METHODS
Study Purpose
This paper reports data on the performance of participants' own pillows, which were extracted from our previously reported pillow trial.18 This field trial tested differences in performance of five experimental pillows with respect to retiring and waking symptoms (pain, stiffness, headache, and scapula pain) compared with participants' usual pillow. Individuals were eligible to participate if they were over 18 years old, generally slept on their side with one pillow, had not suffered an injury to the neck in the previous 12 months, and were not actively seeking treatment for cervico-thoracic spine pain.
All further reference to pillows in this paper refers to participants' own pillows (the pillow on which each participant was usually sleeping during the trial).
Ethics approval for this study was provided by the Human Research Ethics Committee of the authors' university.
Sample Size
No previous similar studies had been conducted that could assist with sample-size calculations. We considered that a sample size of 100 participants was the largest feasible, given the study's time and funding constraints.
Participants were systematically age-cluster-sampled from the pool of randomly selected participants in the earlier survey,16,17 supplemented as required by respondents to newspaper advertisements. Age clusters were young (<40 years), middle (40–59 years), and old (≥60 years), in accordance with the categories used by the Australian Bureau of Statistics.19
Data Collection
Participants were asked to provide 7 consecutive days' data on their pillow, recorded in a tick-box diary each evening (retiring symptoms) and each morning (disrupted sleep, waking symptoms, sleep quality, and pillow comfort).17,18 They were asked to report the presence of “neck pain,” “neck stiffness,” “headache,” and “pain between the shoulder blades.” If these symptoms were present on waking, participants were asked to report the duration of the symptoms (1 hour or less, half a day, or all day). Participants also reported if they believed their sleep had been disrupted or that their waking symptoms were related to a factor other than the pillow. Where participants provided a known reason in the daily diary for disrupted sleep or waking symptoms—for example, illness or a noisy environment—the data for these days were excluded from analysis of symptom production, as the study sought information on waking symptoms and disrupted sleep potentially related to pillow use only. When reporting overnight pillow comfort, participants chose from the categories perfectly comfortable, quite comfortable, barely comfortable, and uncomfortable; when reporting sleep quality, they chose from the categories poor, fair, good, and excellent.
Data Management
For each night during which there was no known reason for sleep disturbance, waking symptoms were collated into the categories no problems, occasional short-term problems (lasting up to 1 hour, 1–3×/week), regular short-term problems (lasting up to 1 hour, >3×/week), occasional longer-term problems (lasting half a day, 1–3×/week), or regular longer-term problems (lasting half a day, >3×/week). To evaluate temporal symptom patterns, change in symptoms overnight was classified into four groups (1=no retiring or waking symptoms, 2=retiring as well as waking symptoms, 3=retiring symptoms not present on waking, and 4=no retiring symptoms but waking symptoms). Where symptoms were not present on retiring but were present on waking (group 4), in the absence of other reasons for waking symptoms, we assumed that pillow type contributed to symptom production. Conversely, where symptoms were present on retiring but not on waking (group 3), we hypothesized that the pillow might have contributed to symptom relief. Where there was no change in retiring symptoms on waking (groups 1 and 2), we assumed that the pillow had no role to play. Pillow comfort ratings of perfectly comfortable and quite comfortable were considered to indicate high pillow comfort, while ratings of barely comfortable and uncomfortable were considered to indicate low pillow comfort. Sleep-quality ratings of poor and fair were combined to indicate low sleep quality, while good and excellent indicated high sleep quality.
Daily diary scores of sleep quality and pillow comfort were collated into consistently low, variable, and consistently high sleep quality and pillow comfort for each participant.
Data Analysis
Waking symptoms were compared for six gender and age groups: young women (aged 18–39 years), older men (aged 60+ years), and so on. We considered differences between those participants who reported no waking symptoms of any kind and those who reported one or more waking symptoms. Linear regression models (reported as r2 values) were used to establish the association between interval measures of pillow comfort and sleep quality. Step-wise addition of age (as an equal-interval measure) and gender (as a dummy binary variable) to this model tested their potential confounding influences. A significant confounding effect was identified when the r2 value changed by more than 0.1 after each addition.
Logistic regression models, reported as odds ratios (ORs) with 95% confidence intervals (95% CI), were used to establish the association between binary forms of pillow comfort, sleep quality, and waking symptoms. Crude ORs are overall measures of the association between the outcome (in this case, any event of stiffness, headache, or scapula/arm pain compared with none) and exposures (in this case, poor/fair sleep quality vs. good/excellent quality and barely comfortable / uncomfortable pillows vs. perfectly comfortable / quite comfortable pillows). Adjusted odds ratios (AORs) were then reported, which took into account the influence of age and gender. When we adjusted the crude ORs by the potential confounders, the true nature of the association between exposure and outcome became clearer. The confounding effect of age was considered using three independent levels of age (young, middle, old), with the young level designated as the default comparator. Gender was treated as a binary variable, with male as the default comparator. At each logistic regression step, when the confidence interval did not incorporate the value 1, the association was deemed significant. A significant confounding effect was identified when the likelihood ratio (a measure of the variance in the model) changed significantly with the addition of the independent variables to the model (p<0.05).
Generalized linear models tested the influence of pillow type on the mean interval ratings of sleep quality and pillow comfort. Statistical Analysis System (SAS) version 9.2 (SAS Institute Inc., Cary, NC) was used for all analysis.
RESULTS
Participants
A total of 58 participants in the telephone survey15,16 and 48 participants recruited via newspaper advertising were invited to participate in the study, and all agreed to do so. All 106 participants provided 7 days' retiring and waking data on the pillow they chose to sleep on at the time of the study (n=742 observations). Known reasons for disturbed sleep were provided on 107 mornings, and these data were excluded from the analysis reported here. The remaining observations (n=635) were classified as valid.
No Waking Symptoms
Forty-five participants (42.5% of the sample) reported no waking symptoms of any type on their pillow. The demographic details of this “no symptom” group are reported in Table 1. There was a difference that trended toward significance in this group's gender composition (37.7% male (95% CI: 23.6%–52.0%, p=0.06). There was no significant difference in gender–age group distribution (χ2=0.90, df=2, p=0.26). When each symptom type was considered separately, we found that 43.5% of the sample reported no waking cervical pain, 34.9% reported no waking stiffness, 42.6% reported no waking headache, and 43.5% reported no scapula pain.
Table 1.
Age and gender proportions of subjects reporting no retiring or waking symptoms
| Age <40 years | Age 40–59 years | Age 60+ years | |
|---|---|---|---|
| Women | 13.5% (n= 14) | 24.4% (n=26) | 24.4% (n= 26) |
| Men | 6.6% (n=7) | 20.1% (n=21) | 11.0% (n=12) |
Waking Symptoms
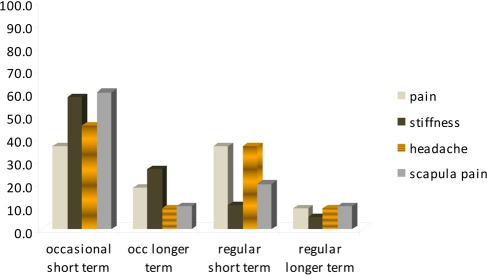
The majority of waking symptoms occurred occasionally and lasted up to 1 hour; stiffness was the most commonly reported symptom. There was, however, a group of participants who regularly reported long-term symptoms from sleeping on their pillow (see Figure 1). There were no gender or age associations with the type or duration of waking symptoms.
Figure 1.
Frequency and type of waking symptoms for participants who reported any waking symptom and who did not have disturbed sleep
Temporal Change in Symptoms
Retiring symptoms alleviated by morning (potentially influenced by sleeping on participants' own pillows) were reported by only a small percentage of participants. Alleviation of retiring symptoms was reported at least once during the trial week by 8.5% of participants for cervical pain, 4.7% for cervical stiffness, 10.5% for headache, and 8.6% for scapula pain. On the other hand, production of symptoms overnight or maintenance of retiring symptoms was reported more commonly—at least once in the trial week—by 17.9% of participants for cervical pain, 35.8% for cervical stiffness, 16.0% for headache, and 19.9% for scapula pain. Only three participants (2.8%) reported production and/or maintenance of all four retiring symptoms over the trial week; 10.2% (n=11) reported production and/ or maintenance of three out of four retiring symptoms over the week, and 24.0% (n=25) reported production and/or maintenance of two out of four retiring symptoms.
Cervical stiffness was the symptom most commonly reported as being produced overnight or not relieved by sleep on participants' own pillow and potentially related to pillow performance (see Figure 2).
Figure 2.
Temporal symptom patterns
Pillow Comfort, Sleep Quality, and Waking Symptoms
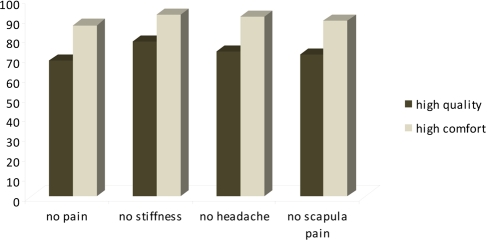
The study found that pillow comfort and sleep quality were moderately associated (r2=0.55, p=0.02) and that neither age nor gender exerted a significant influence on this association (r2 values changed by less than 0.1 with each addition). However, pillow comfort and sleep quality did not necessarily correlate with reports of waking symptoms: some participants reported an uncomfortable or poor-quality night's sleep but no waking symptoms, while others reported a comfortable or good-quality night's sleep and yet had waking symptoms. Figure 3 reports on a subset of data for participants who reported no waking symptoms at all (n=45), highlighting the fact that even though these participants regularly woke with no symptoms, their reports of sleep quality and pillow comfort were not always high. Conversely, up to 5.3% of participants who reported high pillow comfort also reported waking symptoms, while up to 9.6% of those who reported high sleep quality also reported waking symptoms (see Table 2).
Figure 3.
Reports of high-quality sleep and high pillow comfort by participants reporting no waking symptoms of any type
Table 2.
Longevity of waking symptoms reported by participants who reported high pillow comfort, high sleep quality, and waking symptoms
| Occasional Short-Term |
Occasional Longer-Term |
Regular Short-Term |
Regular Longer-Term |
|
|---|---|---|---|---|
| High pillow comfort (% participants in each symptom category) | ||||
| Cervical pain | 0 | 1.8 | 5.3 | 1.8 |
| Cervical stiffness | 5.3 | 5.3 | 0 | 1.8 |
| Headache | 5.3 | 0 | 0 | 0 |
| Scapula pain | 3.6 | 0 | 1.8 | 4 |
| High sleep quality (% participants in each symptom category) | ||||
| Cervical pain | 1.3 | 2.5 | 4.9 | 1.3 |
| Cervical stiffness | 9.6 | 3.7 | 1.3 | 1.3 |
| Headache | 3.7 | 1.3 | 2.5 | 0 |
| Scapula pain | 3.7 | 1.3 | 2.5 | 0 |
Pillow Comfort, Sleep Quality, and Temporal Change in Symptoms
Neither high pillow-comfort nor high sleep-quality ratings guaranteed symptom-free waking. This was most common with respect to production or maintenance of cervical stiffness (see Table 3). We therefore rejected our hypothesis that those participants whose symptoms were relieved overnight, or who had no symptoms, would rate their sleep quality and pillow comfort high and that those whose symptoms were produced or maintained overnight would rate their pillow comfort and sleep quality lower.
Table 3.
Percentage of participants in categories of high pillow comfort and high sleep quality who reported no retiring or waking symptoms, retiring but no waking symptoms, and waking symptoms that were either present on retiring and not relieved or occurred overnight (not present on retiring, but present on waking)
|
No Retiring or Waking Symptoms |
Retiring But No Waking Symptoms |
Production of Waking Symptoms or Maintenance of Retiring Symptoms |
|
|---|---|---|---|
| High pillow comfort (% of participants in each category) | |||
| Cervical pain | 84.2 | 1.7 | 14.1 |
| Cervical stiffness | 77.2 | 1.8 | 21.0 |
| Headache | 82.6 | 10.6 | 6.9 |
| Scapula pain | 79.4 | 8.3 | 12.3 |
| High sleep quality (% of participants in each category) | |||
| Cervical pain | 79.6 | 4.8 | 15.7 |
| Cervical stiffness | 67.5 | 4.8 | 27.7 |
| Headache | 75.9 | 12.1 | 12.0 |
| Scapula pain | 73.5 | 9.6 | 16.9 |
Table 4 reports on the association between pillow comfort, sleep quality, and waking symptoms using ORs (both crude and adjusted by gender and age) and 95% CIs. Poor sleep quality and poor pillow comfort were so strongly related that their association could not be calculated as an OR: all participants who reported poor sleep quality also reported poor pillow comfort. After adjustment for gender and age, sleep quality was strongly and significantly related to waking stiffness and scapula pain, and its association with waking headache trended toward significance.
Table 4.
Crude (COR) association between pillow comfort, sleep quality, and waking symptoms, adjusted for age and gender (AOR)*
| Pillow Comfort | Waking Cervical Pain | Waking Cervical Stiffness | Waking Headache | Waking Scapula Pain | |
|---|---|---|---|---|---|
| Sleep quality: Poor, Fair | |||||
| OR (95% CI) | Not calculable** | 2.66 (0.77–10.24) | 2.64 (0.98–7.82) | 3.83 (0.92–15.97) | 3.23 (0.82–13.75) |
| AOR (95% CI) | 2.73 (0.75–10.48) | 4.32 (1.25–15.61) | 4.12 (0.93–18.82) | 6.13 (1.12–31.56) | |
| Pillow comfort: Uncomfortable or Barely comfortable | |||||
| OR (95%CI) | n/a | 2.44 (0.58–11.83) | 1.15 (0.34–3.56) | 2.32 (0.62–8.65) | 1.72 (0.44–6.97) |
| AOR (95%CI) | n/a | 2.33 (0.44–11.55) | 2.12 (0.56–8.86) | 2.32 (0.52–10.66) | 4.12 (0.73–25.13) |
Figures in bold type indicate statistically significant findings.
All subjects who reported poor sleep quality also reported poor pillow comfort.
OR=crude odds ratio; AOR=adjusted odds ratio; 95%CI=95% confidence interval
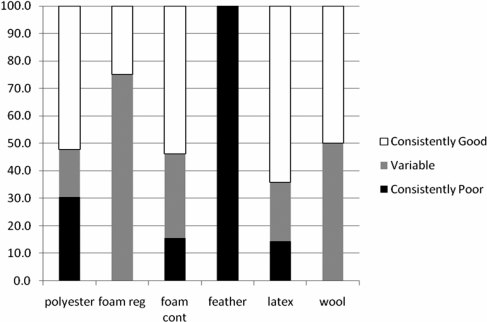
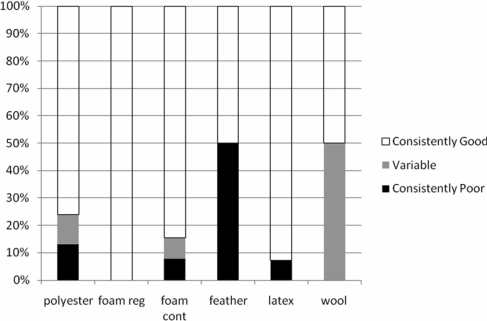
The data were further investigated to identify whether specific pillow shapes and fillers were associated with better sleep quality or better pillow comfort. All participants in the field trial had been invited to present their pillows for inspection, and 81 participants did so (76.4% of the sample). Polyester pillows were by far the most popular choice to sleep on (58.9%), followed by foam contour (15.8%), latex (rubber) (14.7%), foam regular (5.2%), feather (3.2%), and wool (2.1%).
There was no significant difference in sleep-quality or pillow-comfort scores for the different pillow types (p=0.52). Nevertheless, Figures 4 and 5 highlight how, over 7 consecutive days of data collection, the feather-pillow users all rated their sleep quality and pillow comfort consistently low, while users of polyester and latex pillows rated their sleep quality and pillow comfort consistently high. Figures 4 and 5 report the frequency of each pillow type in each category of sleep quality and pillow comfort. Feather-pillow users were most likely to report both poor sleep quality and poor pillow comfort, while latex-pillow users consistently reported high pillow comfort and high sleep quality. Use of a foam regular pillow resulted in consistently high pillow comfort ratings but variable reports of sleep quality.
Figure 4.
Patterns of “own” pillow type for sleep-quality reports over 1 week
Figure 5.
Patterns of pillow comfort reports over 1 week for participants using their own pillows
DISCUSSION
We hypothesized that individuals would choose to sleep on a pillow that supports good-quality sleep, is comfortable, and is not associated with waking symptoms. However, regular waking symptoms, retiring symptoms that persist on waking, uncomfortable pillows, and poor-quality sleep were reported by more than 50% of participants sleeping on their own pillows. After adjustment for age and gender influences, there remained a strong and significant association between reported poor-quality sleep and waking with cervical stiffness and scapula pain. However, there was no association between pillow comfort and waking symptoms, despite adjusting the association for gender and age effects, which suggests that participants' perceptions of pillow comfort and their reports of waking symptoms are independent. This finding suggests that for healthy side-sleepers without known reasons for disrupted sleep, the choice of pillow may be only one factor related to a poor night's sleep.
Our study found that feather pillows were associated with lower ratings of sleep quality and pillow comfort, while latex and polyester pillows were consistently associated with higher ratings. Our experimental study considering new (trial) pillows of the same type and waking cervical pain produced similar findings.18
The high correlation between reports of low sleep quality and reports of low pillow comfort may indicate that participants blamed their pillows for poor-quality sleep. In fact, however, other factors that significantly constrain sleep quality, such as the presence of a medical condition, past history of injury or accident to the cervical spine, sleep position, and nocturnal bruxism, may all contribute to reports of low sleep quality.15 We attempted to control these effects by including only healthy individuals without recent neck injury who slept in side-lying position with a single pillow. However, psychological distress was not measured in this study, and as this factor has the capacity to constrain sleep quality, it should be considered in future studies.20 Further, the effect of a past history of significant cervical or thoracic injury should be considered. A tendency to misattribute blame for low sleep quality to one's pillow may account for the patient population who endlessly search for the ideal pillow.
The high rate of waking symptom reports and the variability in reports of pillow comfort and sleep quality for participants' own pillows underscore the difficulty that individuals may have in choosing a pillow and deciding when to change pillows. A high percentage of participants reported that their retiring symptoms were not relieved by sleeping overnight on their pillow, which suggests that participants' own pillows, in many instances, did not provide adequate support to the head and neck. Given the cost of new pillows and the variable claims made by manufacturers about pillows' performance, consumers are faced with a difficult decision every time they decide to purchase a new pillow, unless they belong to the minority who have no regular waking symptoms, whose sleep is of good quality, and whose previous pillow choice was comfortable.
LIMITATIONS
Limitations of this study include bias introduced by volunteer sampling and reliance on participant self-report of confounders such as work and recreational activities, stress, illness, and alcohol use that may contribute to symptom production. Further, although pillows were grouped according to content and shape, variation due to pillow age, thickness, and hardness is likely to have been present.
CONCLUSION
The findings of this study suggest that many people may be sleeping on the wrong pillow (for them), as indicated by compromised sleep quality, low pillow comfort, and the presence of waking symptoms. Thus, when conducting comparative research on pillow performance, researchers cannot assume that individuals' usual pillow is an appropriate comparator, nor that it will consistently perform well in terms of alleviating retiring symptoms, ensuring an absence of waking symptoms, being comfortable, or contributing to high-quality sleep. There appeared to be a strong relationship between sleep quality and waking symptoms (stiffness, headache, and scapula pain); when the relationship was adjusted for gender and age, however, the associations between sleep quality and waking cervical pain and between pillow comfort and any waking symptom were less convincing. This finding highlights the potential for men and women in different age groups to be suited to specific types of pillows.
An important direction for pillow research is to understand how individuals decide which type of pillow to use regularly and when and why they decide to replace their current pillow or change to a new pillow type. On the basis of our study findings, an individual's own pillow cannot be assumed to lead to symptom-free waking or to reflect the performance of an “ideal” pillow.
KEY MESSAGES
What Is Already Known on This Topic
There is scant knowledge about how different pillows perform in terms of waking symptoms, temporal relief of symptoms, pillow comfort, or assisting quality sleep. Thus, there is little information to assist individuals in choosing a pillow for personal use.
What This Study Adds
This study provides rare information on the performance of pillows on which individuals usually sleep with respect to waking symptoms, temporal relief of symptoms, pillow comfort, and sleep quality. The findings indicate that latex, foam contour, and polyester pillows perform better than foam regular or feather pillows, and that men and women of different ages may have different pillow preferences.
Gordon SJ, Grimmer-Somers K. Your pillow may not guarantee a good night's sleep or symptom-free waking. Physiother Can. 2010;preprint. doi:10.3138/ptc.2010-13
REFERENCES
- 1.Wellings H. Choosing the right pillow. Today Tonight [Internet] 2007. Nov 13, [cited 2009 Mar 7]. Available from: http://au.todaytonight.yahoo.com/article/41403/consumer/choosing-right-pillow.
- 2.Shields N, Capper J, Polak T, Taylor N. Are cervical pillows effective in reducing neck pain? New Zeal J Physiother. 2006;34:3–9. [Google Scholar]
- 3.DeVocht JW, Wilder DG. Biomechanical evaluation of four different mattresses. Appl Ergon. 2006;37:297–304. doi: 10.1016/j.apergo.2005.07.002. doi: 10.1016/j.apergo.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Keller BP, Lubbert PH. Tissue-interface pressures on three different support-surfaces for trauma patients. Injury. 2005;36:946–8. doi: 10.1016/j.injury.2004.09.017. doi: 10.1016/j.injury.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 5.Lahm R, Iaizzo PA. Physiologic responses during rest on a sleep system at varied degrees of firmness in a normal population. Ergonomics. 2002;45:798–815. doi: 10.1080/00140130210159968. doi: 10.1080/00140130210159968. [DOI] [PubMed] [Google Scholar]
- 6.Buckle P, Fernandes A. Mattress evaluation: assessment of contact pressure, comfort and discomfort. Appl Ergon. 1998;29:35–9. doi: 10.1016/s0003-6870(97)00023-9. doi: 10.1016/S0003-6870(97)00023-9. [DOI] [PubMed] [Google Scholar]
- 7.Boyd DM. System and method for selecting a pillow and mattress. 2006 Dec 14; US Pat. app. no. 11/610/776. Publication no. US 2007/0086947 A1.
- 8.Persson L, Moritz U. Neck support pillows: a comparative study. J Manip Physiol Ther. 1998;21:237–40. [PubMed] [Google Scholar]
- 9.Hagino C, Boscariol J, Dover L, Letendre R, Wicks M. Before/after study to determine the effectiveness of the Align-Right cylindrical cervical pillow in reducing chronic neck pain severity. J Manip Physiol Ther. 1998;21:89–93. [PubMed] [Google Scholar]
- 10.Lavin RA, Pappagallo M, Kuhlemeier KV. Cervical pain: a comparison of three pillows. Arch Phys Med Rehabil. 1997;78:193–8. doi: 10.1016/s0003-9993(97)90263-x. doi: 10.1016/S0003-9993(97)90263-X. [DOI] [PubMed] [Google Scholar]
- 11.Ambrogio N, Cuttiford J, Lineker S, Li L. A comparison of three types of neck support in fibromyalgia patients. Arthrit Care Res. 1998;11:405–10. doi: 10.1002/art.1790110512. doi: 10.1002/art.1790110512. [DOI] [PubMed] [Google Scholar]
- 12.Persson L. Neck pain and pillows: a blinded study of the effect of pillows on non-specific neck pain, headache and sleep. Adv Physiother. 2006;8:122–7. doi: 10.1080/14038190600780239. [Google Scholar]
- 13.Miller R. The prone sleeper's spine. Brit Osteopath J. 1984;16:61–8. [Google Scholar]
- 14.McDonnell J. Sleep posture: its implications. Brit J Phys Med Indust Hyg. 1946;9:46–52. [PubMed] [Google Scholar]
- 15.Gordon S, Grimmer K, Trott P. Sleep position, age, gender, sleep quality and waking cervico-thoracic symptoms. Internet J Allied Health Sci Pract. 2007;5:1. Available from: http://ijahsp.nova.edu/articles/vol5num1/gordon2.htm. [Google Scholar]
- 16.Gordon SJ, Trott P, Grimmer KA. Waking cervical pain and stiffness, headache, scapula or arm pain: gender and age effects. Aust J Physiother. 2002;48:9–15. doi: 10.1016/s0004-9514(14)60277-4. [DOI] [PubMed] [Google Scholar]
- 17.Gordon S, Grimmer-Somers K. Consistency of reports of sleep quality, pillow comfort and cervico-thoracic waking symptoms on “own” pillow of known type and shape. J Musculoskelet Pain. Forthcoming 2010 [Google Scholar]
- 18.Gordon S, Grimmer-Somers K, Trott P. Pillow use: the behaviour of cervical pain, sleep quality and pillow comfort in side sleepers. Manual Ther. 2009;14:671–8. doi: 10.1016/j.math.2009.02.006. doi: 10.1016/j.math.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Australian Bureau of Statistics. 2001 census data [Internet] Canberra: The Bureau; c2001. [cited 2009 Mar 10]. Available from: http://www.abs.gov.au. [Google Scholar]
- 20.American Academy of Sleep Medicine. International classification of sleep disorders revised: diagnostic and coding manual. Chicago: The Academy; 2001. [Google Scholar]