Presented as a poster at the Kaiser Permanente Care Management Institute Conference, October 18, 2004, San Francisco, California; as a poster at the Kaiser Permanente National Quality Conference, June 27–July 1, 2005, Monterey, California; and at the Kaiser Permanente National Hypertension Implementation Committee teleconference, September 13, 2005.
Hypertension (HTN) or high blood pressure, is defined as consistently elevated systolic BP above 140 mmHg or diastolic above 90 mmHg. For certain groups of people, ideal blood pressure is even lower than this. Uncontrolled hypertension can lead to end organ damage, including heart failure, heart attacks, nephropathy, peripheral vascular disease, aortic dissection, blindness, or stroke. Because there are no symptoms of hypertension until organ damage occurs, hypertension is known as the “silent killer.”
The group identified the obstacles preventing KPMAS from providing the best possible care for members with hypertension …
Problem
Kaiser Permanente of the Mid-Atlantic States (KPMAS) serves approximately 500,000 people in Maryland, Virginia and Washington, DC. KPMAS is composed of Kaiser Foundation Health Plan of the Mid-Atlantic States, Inc, and the Mid-Atlantic Permanente Medical Group, PC, an independent medical group with more than 900 physicians providing care for members and the community throughout the area.
In 2001, KPMAS scored 49% in the “Controlling High Blood Pressure” measure for the Health Plan Employer Data and Information Set (HEDIS) and below the 25th percentile of performance for health plans nationwide. More importantly, these 2001 results meant fewer than half of KPMAS' members with documented hypertension had their blood pressure controlled (defined as <140/90). Approximately 50,000 members were at increased risk for complications of hypertension, damage that is entirely preventable with appropriate care.
Assessment
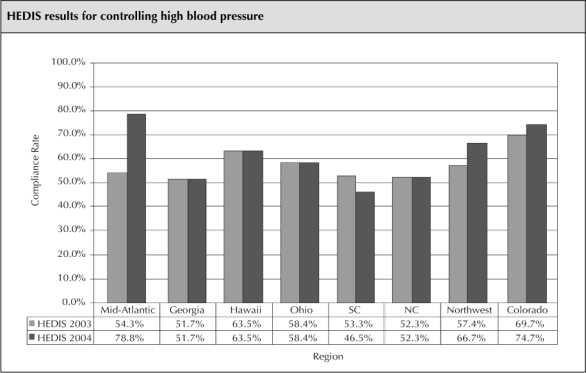
KPMAS leadership recognized the need for a quality improvement program to improve control of high blood pressure. A well-attended, multidisciplinary barrier analysis meeting was held in October 2001 to identify and discuss the barriers to providing the highest quality of care for patients with hypertension. Participants at the meeting included physicians from internal medicine, family practice, cardiology, neurology, nephrology, and urgent care. In addition, nursing, pharmacy, nutrition, behavioral health, case management, nurse advice, quality, measurement, health education, risk management, health information management services (HIMS), and information technology (IT) representatives fully participated. The group identified the obstacles preventing KPMAS from providing the best possible care for members with hypertension, including:
Poor ability to accurately measure, collect, and administratively record blood pressure values
Inconsistent messages and education to members and to staff related to evidence-based clinical practice guidelines
Inconsistent provider practice
Inadequate systems for follow-up
Systematically addressing these barriers formed the basis of whole system change to improve care.
Goal
From its inception, the HTN program was designed to serve not only patients with known hypertension, but also patients at risk (people with diabetes, chronic kidney disease [CKD], heart failure, and coronary artery disease). Using the HEDIS 2001 national 90th percentile for blood pressure control as a benchmark (62.3%), leadership decided that the program goal was 63% of adult members with a diagnosis of hypertension would have BP <140/90. Because the program also included patients with a chronic disease, our internal metric was consistent with the clinical practice guidelines, and more stringent than HEDIS control specifies. We defined BP control in members with diabetes and CKD as a BP <130/80. While a 14% improvement was a stretch as a goal, it was believed that once KPMAS could accurately identify and track blood pressures administratively, the Region would be able to lower blood pressure for the 14,000 additional patients' blood pressure that it would take to reach target.
… our internal metric was consistent with the clinical practice guidelines, and more stringent than HEDIS control specifies.
Interventions
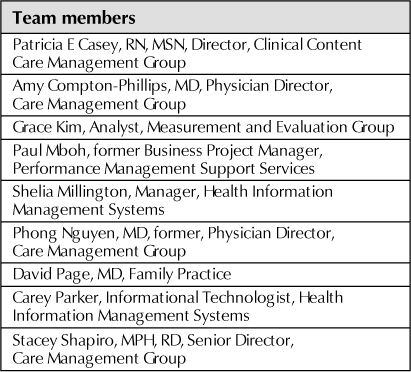
While many interventions were implemented over the following years (Figure 1), the most significant interventions included:
Implementation of a blood pressure measurement competency validation program for staff and clinicians, using a mannequin arm that simulated Korotkoff sounds. The competency draft was based on the information in Human Blood Pressure Determination by Sphygmomanometer (American Heart Association, 2001)1 and a BP competency program developed by the Virginia Department of Health. The BP measurement competency validation program was modeled after the American Heart Association training for cardiopulmonary resuscitation. The competency program was disseminated throughout the entire Region by the significant support of nursing practice consultants and the medical centers' nursing managers. The competency program not only reinforced the technical skills of measuring blood pressure, but reinforced with front-line staff (who convey important messages to patients) the critical importance of blood pressure being at goal, not “just a little high.”
- Dissemination of an education program targeting providers, health care teams and patients, to ensure consistent messages on blood pressure goals and treatment. This included:
- - Providing regional and medical center educational programs for providers, pharmacists, nurses, clinical assistants, IT, HIMS, and medical coders.
- - Developing and disseminating the Clinical Practice Guidelines2 along with Continuing Medical Education programs, pocket cards, memos, newsletter items, and Intranet articles to all providers.
- - Placing “Know what your blood pressure numbers mean” and “BP Tips” posters in all exam rooms, continually reinforcing goals and targets not only with patients, but staff and clinicians as well.
Adoption of mandatory blood pressure measurement at all primary care and specialty encounters.
- Placement of the BP on a preprinted member visit encounter form (VEF) and into an administrative database. This intervention served as a “band-aid” until the Region had a designated vital sign section in the electronic medical record. The VEF was particular to a member and the clinician associated with the visit and contained the patient's demographics. Completing the VEF was already established in the workflow of every outpatient visit. The IT and HIMS teams created an alert on the VEF for patients with HTN or a chronic disease: blank spaces for BP values preprinted on the form, which would be completed during the visit. At day's end, a clerical person entered the completed form, and the handwritten blood pressure measurement, into the mainframe system. The administrative database had two main benefits:
- Subsequent VEF forms for a patient would pre-print the last two historical blood pressure measurements. This allowed the treating clinician to trend the BP measurements and to tell if an elevated blood pressure at that visit was an isolated event, or a consistent finding, even if the member's chart was unavailable.
- The BP values in this database enabled the development of feedback reports with individual patient, treating physician, medical center, and regional data. Of note, most of KPMAS's improvements came in 2003 but the initial reports were not released until November of that year. Therefore, these reports were not the key drivers of improvement.
Figure 1.
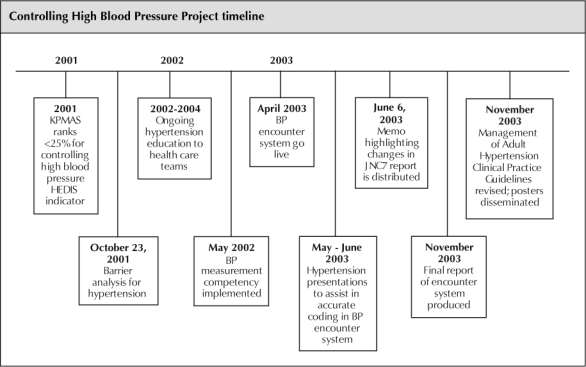
Chart shows timeline for project on controlling high blood pressure.
Each discipline brought an action-oriented passion for controlling hypertension that allowed for organizational agility …
In addition to addressing the barriers above, other systematic interventions, in keeping with the theory of the chronic care model that numerous influences (not just physician one-on-one time in the office) contribute to a patient's long-term outcome managing their chronic condition. These interventions are summarized in Figure 2.
Figure 2.
Implementation of the KPMAS Hypertension Program, based on the Chronic Care Model.
AHA, American Heart Association; BP, blood pressure; CA, clinical assistant, CME, continuing medical education; DM, diabetes; HEDIS, Health Plan Employer Data and Information Set; HIMS, Health Information Management Services; HBP, high blood pressure; MD, physician; RN, registered nurse.
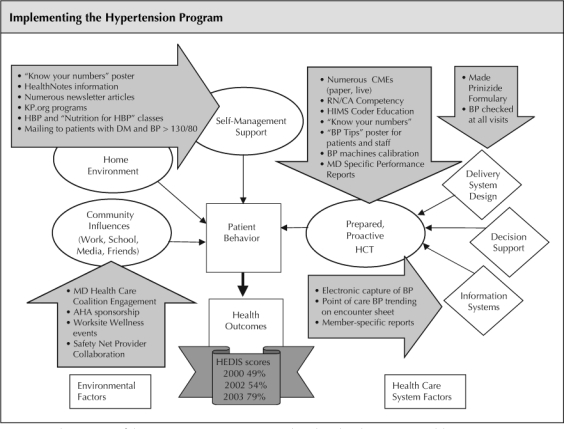
Results
With these multifaceted interventions, along with the high-level sponsorship of the importance of HTN control, KPMAS saw its HEDIS score for controlling high blood pressure jump to 78.8% in 2004 (Figure 3). Although the HEDIS score dipped to 73% in 2005, the variation is not statistically significant and KPMAS remains the leader in HTN control among all the KP Regions.
Figure 3.
Graph shows HEDIS results for controlling high blood pressure in hypertensive patients across KP Regions.
Discussion
The significant results of the project validate the published literature3 on process redesign employing quality improvement concepts: an involvement of the entire organization and information sharing are critical to controlling hypertension. It is important to note that this project was completed without added personnel or administrative or financial incentives. It used the existing electronic legacy medical record systems.
Involvement of KPMAS leadership, primary care and specialty physicians, nurses, nutritionists, pharmacists, clinical assistants, data entry personnel, medical coders, data analysts, health education specialists, quality experts, information technology specialists, health information personnel and members, all made this project successful. Each discipline brought an action-oriented passion for controlling hypertension that allowed for organizational agility in implementation perseverance and sustained clinical improvements.
References
- Perloff D, Grim C, Flack J, et al. Human blood pressure determination by sphygmomanometry. Dallas (TX): American Heart Association; 2001. [DOI] [PubMed] [Google Scholar]
- Kaiser Permanente. Mid-Atlantic States. Management of adult hypertension: clinical practice guideline [monograph on the Intranet] November 2003 [cited 2005 Dec 29]. Available from: http://cl/kp.org/portal/site/mid-atlantic/?epi_menultemID=7e85504896e476f8401fdf702a71eea0&epi_menuID=3c518a725d0366f8401fdf702a71eea0.
- ICIC: The Chronic Care Model: Model Elements [homepage on the Internet] Seattle (WA): Improving Chronic Illness Care, MacColl Institute for Healthcare Innovation, Group Health Cooperative Center for Health Studies; [cited 2006 Jan 6]. Available from: http.improvingchroniccare.org/change/model/components.html. [Google Scholar]


