Frank Brennan, MD, a primary care physician, arrives at work at 7:00 am, to get a head start on the day. It's a Monday and he knows his schedule will be full of patients wanting his care and attention. He enjoys being with his patients, but always needs more time. He diligently works through his schedule, focusing on one patient at a time. Dr Brennan worries about all the patients on his panel who need to come in but haven't. He would like to get back to why he became a physician in the first place: to be with, talk to, and care for his patients in a personal way. But by the end of the day he is exhausted trying to stay on schedule. It's only Monday. Simply running faster will not work. Dr Brennan thinks there's got to be a better way.
Rob Unitan, MD, a pulmonologist from the NW Region, Samir Patel, MD, a family practitioner, and Gerard Livaudais, MD, an internist, both from the Hawaii Region, wondered about that “better way” and developed bold visions of how a new approach would work. Through a chance meeting in 2005 at the Institute for Healthcare Improvement (IHI) Summit on Clinic Redesign in Washington, DC, they discovered their common interests. Dr Unitan, Dr Patel, and Dr Livaudais created a new program to dramatically change the way they work that changed forever how they view “care delivery.”
“Our work is not the schedule” Dr Livaudais quoted Doug Eby, MD, whom he met at the Washington, DC, conference. “The work should really be our panel, not just those who come in sick.”1,2 Dr Livaudais knew that seeing one patient at a time didn't work and that incremental refinement of our existing system would not get us there. “What we need,” Dr Livaudais continued, “is to totally rethink our methods of delivering care. We should redesign our system with a forward-looking concept that anticipates what we need to succeed to improve the health of the entire population we serve.”
What resulted was Total Panel Ownership and an easy-to-use Web-based member database called the Panel Support Tool.
—Tom Janisse, Editor-In-Chief
Total Panel Ownership
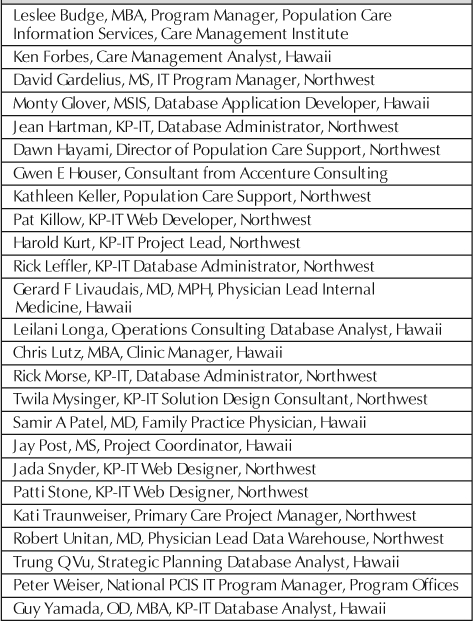
Responding to the challenges of the existing system, the Northwest and Hawaii Regions (Table 1) embarked on the transformation of the Care Delivery System, referred to as Total Panel Ownership. Beginning with Primary Care, this implementation began in 2005 with two pilot sites in the Hawaii Region; widespread implementation will continue in 2006 for both Regions.
Table 1.
Total Panel Ownership and Panel Support Tool team
Opening Day Congratulations.
December 9, 2005
Dear Panel Support Tool Team,
On behalf of the Hawaii Region's executive team, chiefs, PIC's, and Board of Directors, please accept our heart felt “mahalo nui loa” for your astounding collaboration, expertise, and will to succeed that allowed for the Panel Support Tool to be piloted this week. It's fast, beautiful, and useful!!
It was my privilege to attend the Nanaikeola Clinic's “day 1” experience and I am reassured that you have given our physicians, practitioners, and staff an outstanding tool to identify and treat “care gaps,” engage our members in the context “we know you and care about you,” and demonstrate improved evidence-based clinical outcomes.
I am flat out amazed and grateful. When KP talks about our “integration advantage,” I've always envisioned miraculous productivity. Your diverse expertise, passionate, synergistic design and product implementation is so appreciated. In Hawaii, “no ka oi” signals the very best. Congratulations all, no ka oi.
— Geoff Galbraith, Vice President, Quality Improvement, Hawaii Permanente Medical Group
Although there is no single definition of Total Panel Ownership, the following are its main elements:
The focus is on relationship. This includes the relationship with the members of the panel as well as among members of the core team. It has been statistically demonstrated that members who have a close relationship with their Primary Care Physician (PCP) are more satisfied.3 A strong relationship generates trust with the physician and other team members. In this environment, team members are able to function to the best of their ability.
The needs of the panel are met in the most efficient and convenient way. In addition to the face-to-face office visit, a resource-intensive option, panel members are given more flexible access options: phone consults, phone advice, phone and e-mail-based care management, self care, group appointments and more.
A dedicated core team owns the care of the panel. With “ownership,” the core team has the autonomy and freedom to innovate how care is delivered with an emphasis on being proactive, not reactive. Ownership means the team is responsible for the delivery of care, reaping the benefits or accepting the consequences. There is a strong personal incentive to care for the panel in the most effective and efficient manner.
The team has tools to support the care of the panel. The primary tool is the Panel Support Tool, which graphically displays “care gaps” for each member of the panel. The care gaps are based on the latest evidence of recommended care for members with various conditions and recommended preventive care on the basis of gender and age. The team works to close the gaps for all members of the panel. The team is encouraged to be creative in how the gaps are closed, including addressing the maximum number of nonacute needs during an acute visit.
The team is proactive in meeting the needs of the entire panel. Each member should be afforded value in return for his/her dues. One objective is to have an “annual touch” with each member of the panel. Offerings are customized on the basis of each member's needs. A member with diabetes and heart disease may need intensive RN-based care management; a young member with no illnesses may need only basic information on maintaining a healthy lifestyle. The team tailors resources to meet individual needs and preferences.
Innovators are allowed to emerge and try new experiments. Total Panel Ownership needs a nurturing environment in which “independent agents” move quickly and freely to explore new ground and try new “rapid-cycle” experiments that may lead to new solutions. An evolving concept, Total Panel Ownership is a flexible and open program that allows solutions to arise out of practice.
The natural “power” of the team is unleashed. Total Panel Ownership's intrinsic “attractors” make it inviting for teams. It thus becomes a self-sustaining change program generating its own power to continue, rather than relying on an external force-feed to keep it going.4
Total care is coordinated. Total care means that primary care and specialty care should be seamless in providing services. Using the Panel Support Tool as the common ground for coordination, specialty and primary care can each identify the intersection where primary care and specialty care services meet.
There is accountability for resources. Panel ownership includes the responsibility to manage panel resources and their associated costs. It is our cost structure that puts us at risk in the health care marketplace and presents the greatest challenge to the organization. Rather than implementing a straight percentage reduction in the budget, our chosen method is waste elimination. Waste adds cost without adding value; therefore waste elimination does not compromise care. The Panel Support Tool is a natural place to reveal cost information and potential waste and make this information available for teams to use.
These are the core building blocks that the teams in Hawaii and the Northwest will use to help create the new care delivery system. Each clinic/team is self-governing and therefore free to create/design an improvement effort that supports one or more of these elements. Ideally, all of the above elements will be covered in the process and the best aspects of each will be combined to create the new, transformed care delivery system. Most of these teams will begin with the adoption and implementation of the Panel Support Tool.
A Historic Moment Now Realized.
One can envision a new health care system of the future, which will begin with a basic comprehensive health evaluation for each individual …. The result of that evaluation will chart each individual's personal pathway through our health care resources toward optimal health. Periodic updating of health evaluation profiles will monitor the homeostasis of vital body systems and significant deviations will trigger computerized warnings and corrective instructions. Health evaluations will alert and advise measures to be taken against individual predictive risks be they lifestyle, hereditary, environmental or age/sex linked through time. Such individualized continuing health care would greatly reduce patient uncertainty and could, in large part, replace today's chaotic random-entry demand with a smooth regulated use of appropriate resources that would not only be cost effective, but also would optimize the health of each individual through his lifetime. It should be clear this new medical care delivery system in this health care of the future could never be fully achieved without the large amount of individual information, cybernetic data feedback, protocols, advice rules, monitoring and surveillance that systematized health evaluation and computerization makes possible. That is the great promise of this new delivery system for medicine of the future.
— Sidney R Garfield, MD, 1975, co-founder of Permanente Health Plan, in a talk to medical students at the University of Southern California
The Panel-Support Tool
A Case of Then and Now:
Then: James is a 39-year-old diabetic patient last seen by Dr Frank Brennan two years ago. Quiet and reserved, he recently quit his job and withdrew from all social interaction. Although his wife orders his medicine regularly, he throws it away. He hasn't been monitoring his glucose for many months now. James is aware of a ‘nick’ on his shin that is looking angry but he remains impassive to his wife's concerns. Unfortunately, no one at the clinic knew about this, nor had they picked up on his depression, brought on by the anniversary of his father's death five years ago. There simply hadn't been enough time in the rushed visits to do more than a brief physical and a review and ordering of labs and medications. With an overloaded schedule every day, it's not clear when anyone will notice that he hasn't had his labs drawn, until his leg becomes serious enough to force him to come in for debridement and antibiotics.
Now: James is a 39-year-old diabetic patient of Dr Frank Brennan who saw him one year ago. He's in good control of his diabetes and though naturally reserved, has a good relationship with his physician and has great rapport with his physician's medical assistant. He receives an e-mail from his team every three months, and expects a phone call every three to six months, as well. His progress, and that of every patient on the panel, is monitored by the team via the Panel Support Tool. Last week, while reviewing the diabetic portion of the total panel, the team was surprised that James was on the list. When they called him they recognized his remarkable lassitude, and encouraged James to come in. During the call, the team used the Panel Support Tool to uncover his overdue labs and medications, which had been ordered. Behavioral health, copied on the telephone encounter with a request, prepared to meet with James on the day of his visit. All in all, the combination of an existing relationship and a tool that prevents patients from “falling through the cracks” proactively averted a disaster with remarkable efficiency.
The primary difference between these then-and-now case vignettes is the Panel Support Tool. As shown in these vignettes, the Panel Support Tool gives providers the capability to quickly and easily assess the health needs of any single member or any cross-section of the physician's panel without awaiting the availability of analytic resources. The tool then helps providers take the needed action with the support of evidence-based systems of care.
The Panel Support Tool was created through a collaboration between clinicians and Kaiser Permanente Information Technology (KP-IT) from the Northwest and Hawaii Regions with support from the Care Management Institute's Population Care Information System (PCIS) workgroup. Web-based, the Panel Support Tool was designed to compliment KP HealthConnect by giving us efficient and effective summary information at the PCP's panel level rather than at the patient level. This required that the Panel Support Tool be developed so that it: 1) is easily available online, 2) needs little or no training to use, 3) is powerful enough to do Standard-of-Care type screening, 4) provides instant analysis, and 5) enables immediate patient intervention. Significant support is also being received from the Institute for Healthcare Improvement (IHI) and the 21st Century Care Redesign, which is contributing ways to quickly develop, test, and implement ideas using PDSA improvement cycles.
The “Care Gap”—The Total Panel Ownership Measure of Quality
Care gap identification and calculation is a primary feature of the Panel Support Tool. The care gap is a numerical score representing the difference (or “gap”) between needed care and provided care. For example, patients with a history of diabetes, coronary artery disease, peripheral vascular disease, or cerebrovascular disease who have not filled a prescription for a statin or an ACE inhibitor in the past six months, or have no documentation of aspirin use, receive four points for each deficiency (ie, 12 points if they are missing all three drugs). If they are found to have poorly controlled hypertension, another two points are added. If they haven't had their LDL checked in the past 12 months, this earns one more point.
Each night the Panel Support Tool extracts a set of specific data elements from KP HealthConnect and the regional data warehouse and displays the information on a dynamic spreadsheet with various color and numeric coding for easy reading (Figure 1). For example, the tool automatically sorts members with the highest calculated care gap to the top of the list for quick identification and action. The clinician and/or their support staff can sort for any number of conditions or parameters to identify common or prevalent health needs that may be addressed many-at-a-time instead of one-at-a-time. Total or composite care gaps can also be calculated for each panel and thus the net improvement in the health of the panel can be measured over time.
Figure 1.

The Complete Panel View.
Navigating Through The Panel Support Tool
The Panel Support Tool is designed to be intuitive enough to require little or no training. The following describes the ease by which a user can navigate the tool and exercise its basic features:
After entering an ID and password, the tool opens to a list of all of the primary care providers in the Region. Clicking on a clinician's name brings up the Complete Panel View (Figure 1), which is a grid that stratifies the panel members according to their individual weighted care gap scores and disease severity classification, graphically displayed for diabetes mellitus, cardiovascular disease, congestive heart failure, renal insufficiency, hypertension, primary prevention screening (breast, cervical, and colorectal cancer screening, immunizations, blood pressure and lipid), and risk factors such as hyperlipidemia, obesity, and smoking.
From the Complete Panel View spreadsheet, clicking on the member's name takes the user to a Patient Detail Screen (Figure 2), which, in addition to care gaps, displays their most recent vitals, relevant medications, and core laboratory values. Hovering over the result displays the trend. Clicking on a member's medical record number, however, takes the user to a Patient Snapshot Screen, which lists each care gap contributing to the score. Hovering over most gaps with the cursor brings up a small window, which further defines the criteria for that specific deficiency.
Figure 2.

Patient Detail Screen.
The Complete Panel View grid is configured with each disease in a single column. The presence and severity of each disease, together with monitoring/guideline compliance is indicated by the color coding of each cell (or square) formed by the intersection of the disease column and the patient's row. For example, in a patient with diabetes and a glycosylated hemoglobin (HgbA1c) less than 7% in the past six months the diabetes cell will be green. An HgbA1c between 7–9% turns the cell yellow, and >9% turns it red. A diabetic without an HgbA1c result in the past 6–12 months will be identified with a yellow square, and >12 months since the last HgbA1c earns a red square. Detailed descriptions listing the parameters used in determining the color coding for all diseases are found in the Glossary (Figure 3).
Figure 3.
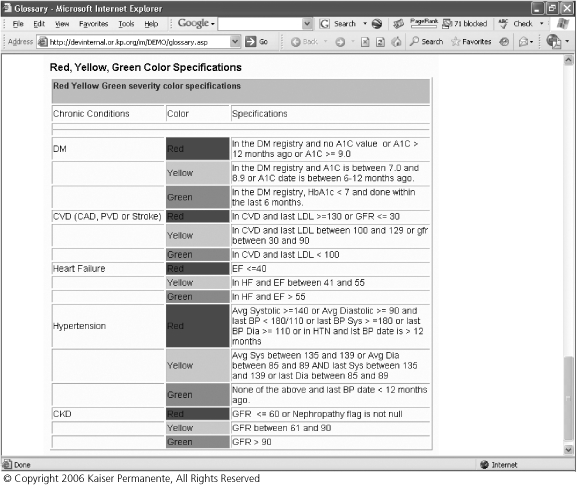
Glossary: Red, Yellow, Green Color Specifications.
While designed for the primary care provider, the Tool also supports users focusing on a specific disease, such as case/care managers. Clicking on the disease name at the top of each column stratifies all members of the panel in descending severity for that disease. Red indicators are found at the top of the grid, followed by yellow, then green. Patients identified in a specific disease registry are designated with a ‘Y’ in that cell. Panel members not identified as having that specific disease fall to the bottom of the grid.
Although the Panel Support Tool runs on the desktop outside KP HealthConnect, the user can easily toggle to and from the medical record for documentation and ordering. Work is ongoing to embed the tool within the HealthConnect home-space to facilitate greater integration with the medical record. The goal is to be able to launch Review or an Encounter for a specific member in HealthConnect directly from the tool.
Patient Activity Tracking
An important and useful feature of the Panel Support Tool is its ability to track panel activity by the PCP, specialist, or other caregiver on each member. These “ticklers” help the provider remember where s/he last worked on the panel. For example, the tool keeps track of which patients were “touched” within the last year and which ones weren't. The tool can also identify all members of a panel seen in the Emergency Department in the past week, and displays each member's most recent hospitalization information. It also lists the date of their last primary care visit and can easily identify all not seen in the past year.
A Cross-Functional Team-Based Approach
The Panel Support Tool is designed to allow teams to maximize their support of the PCP. The team closest to the PCP is the Core Team: In Total Panel Ownership, a core team typically consists of a PCP and a dedicated support team, which includes: a Registered Nurse (RN), a Medical Assistant (MA), a Nurse Practitioner (NP), and a receptionist, although the exact composition is still in flux (for example one core team may have one PCP, one MA, and a .5 RN and another core team may have one PCP, .5 MA, and one RN.) Team members are empowered to self-organize and find creative ways to meet the needs of their panel.4 Over time, the core team will develop close-knit relationships among the members of the core team as well as between the core team and the panel of members. These relationships will lead to trust.
Future Directions: Specialty Care/Primary Care Integration
The Panel Support Tool has great potential to promote better integration and care coordination between specialty and primary care. Work is in process to provide views that can cut across panels and display data on all patients with a given disease. Its potential to support proactive coordinated care programs that can be led or managed by various teams who have access to the tool is tremendous. A fully functional demonstration version of the tool is available at: http://devinternal.or.kp.org/im/demo/login.cfm.
Potential Benefits and Savings.
The benefits and savings from Total Panel Ownership and the Panel Support Tool are significant. They include:
Avoidance of expensive acute care. This is possible by allowing a competent analysis of the panel for developing needs.
Elimination of costly waste. Large benefits are possible from improved coordination between primary care and specialty physicians working on the panel in an aligned, coordinated way.
More effective use of staff time. By working more efficiently at the panel level rather than the one-member-at a-time level staff can be more productive.
Increased member retention. By better targeting and promoting programs, low-utilizing or healthier members will get more value for their paid dues and will be more inclined to renew. This obviously maintains/increases our market share.
Increased physician retention. As the various PCP support teams join in, assess the PCP's panel and do additional corrective or preventive care under the PCP's general direction, the PCP receives a greater feeling of support in the workplace. This helps to avoid physician burnout and attrition.
Improved staff retention. Staff are happier when given more sustainable and fulfilling work.
Better use of less expensive associate and support providers. This can occur with better review of panel needs for identification of appropriate opportunities.
Less reliance on the resource-intensive clinic visit. By giving the patient a greater range of options for access, they will naturally select those that are more efficient for themselves and the organization.
Greater involvement of staff on managing resource costs. This capability begins with the provider level cost data.
Better overall delivery of quality care due to all of the above.
It's All About The Relationship
A core value to absolutely maintain is the time-honored “relationship” with the patient. Why is relationship important? Relationship is the hidden link between the member, staff, and PCP. Its power and presence is always there and exists in many ways, but isn't necessarily noticed, appreciated, or understood. Although quality health care is delivered, the member cannot always judge that; however, the member does judge the quality of the relationship. That is what is valued. If the relationship isn't good, the patient feels it. The member's self worth is reflected in the relationship, eg, how the PCP values what the patient says. Patients with low self worth feel less empowered to change. Relationship is the “magic” element that can make operations special. Behind what is said and done, the patient notices the deep heart-based feeling that only comes from relationship. What ultimately lies at the core of operations, principles, and strategies, is the personal and professional relationship between members and physicians, team, and staff.
Grounded with a relationship focus, the team channels all interactions toward the PCP team. This requires patient education, external and internal marketing, agreements with the other PCP teams, and receptionist and scheduling support. Over time, systems such as scheduling have unintentionally evolved to obstruct panel ownership and relationship by appointing patients into the next available slot. The result has been that patients of Dr Jones saw Dr Smith even though Dr Jones was in clinic that day and vice versa (because Dr Jones' appointments were filled with Dr Smith's patients). Similarly, centralized call centers, disease management programs, mass mailings from “Kaiser” or “your doctor” all subtly replace the patient's primary relationship with their PCP team. This does not diminish the merit of call centers, but simply points out the missed opportunities of more efficient, effective, and personal interactions occurring through an existing, trusting relationship.
How does Total Panel Ownership support “the relationship”? Relationship is intrinsic to the design in many ways:
Flexible modes of access—relating to patients in ways other than the clinic visit
Annual touches—maintain regular contact
Personal health agreements—built on trust from an effective working relationship
Panel support specialists—staff empowered and encouraged to establish a relationship with each member
PCP team support—through team relationship
Personal change—relating to the individuality of each patient
Education and self-care—not as teacher but as partner in their health
Panel database—through the panel database, we KNOW each patient better. To know each patient better is to relate to each patient better.
How Provider “Sustainability” Is Supported.
Total Panel Ownership ensures provider sustainability in many ways:
Work efficiencies—the Panel Support Tool provides an easy, satisfying way to work.
Efficient access—less intensive use of appointment provides more breathing room in schedule.
Work enrichment—the variety of access types makes work more interesting.
PCP team support—team support is the highest physician satisfier.5
Quality of work-life—physicians can do what they became physicians to do.
Enjoyment of relationships—physicians have more opportunity to enjoy patients, team members, and colleagues.
Energy generation—Total Panel Ownership encourages a culture of support for our providers that continuously recharges their battery.
Implementation to Date
As of February 2006, two clinics in Hawaii have gone live on the Panel Support Tool with about 100 users (half physicians and half support staff) signed up. The Northwest will begin rolling out its version of the Panel Support Tool in early March 2006, and has identified nearly 50 clinicians to pilot the tool by late April. The Hawaii Region is basing its 2006 Strategic Plan on Total Panel Ownership and the Panel Support Tool, with all clinics developing innovative plans to support its implementation. For example, the Hawaii Region is now planning a new “21st Century” Clinic on Windward Oahu, whose bold design will promote superior communication and relationships within the core team and between the core team and the patients. Fredrick Sands, MD, an internist at the Maui-Lani clinic, says, “The Panel Support Tool is great! It helps me track and manage my patients with chronic diseases, and it gives me a quick and efficient assessment of my patient's preventive care needs. Now I feel much more confident that I'm taking care of all my panel patients.”
Summary
Total Panel Ownership and the Panel Support Tool is a promising answer to the serious challenges of escalating costs, competition, and member demands. Under Total Panel Ownership, physicians and staff can become an integrated network of dedicated professionals, empowered to make changes they control, supported by efficient programs that take care of all their patients, with relationship-based care at the core. The Panel Support Tool is the breakthrough that allows us to look at all members and relate to them in an efficient, value-added way. By moving away from the one-patient-at-a-time concept, allowing more effective and efficient use of our resources and managing them in ways that add the greatest perceived value to each of our members, we will have greater capacity and capability to compete and thrive in the health care marketplace (and Dr Brennan, our PCP, will then have a sustainable and enjoyable practice within reach).
Conclusion
The intent of Total Panel Ownership goes beyond operational improvement—it's really about creating an environment where the organization's power can be focused on supporting true member needs. We want to do more than just focus on those who come to see us for their physical health issues. We want to know and satisfy the needs of each of our members—the high-utilizing members with multiple medical conditions and the low-utilizing, healthy members—and then foster those behavior patterns that will keep them healthy and happy. This will allow those low-utilizing, healthy members, most at risk of leaving KP, to see value for their premium dollar. These outcomes are most possible when we are able to develop trusting relationships. That is the goal of Total Panel Ownership. Enabled by the Panel Support Tool, Total Panel Ownership makes it possible for us to know each and every one of our members and achieve a unique relationship with each. When it comes to care transformation, we believe it's all about the relationship.
References
- Eby D. “Alaska Native Medical Center: Values-Driven System Design,”. 2005. Patient-Centered Care Improvement Stories, IHI.org.
- Eby D. “Building Healthy Relationships at Alaska Native Medical Center,”. 2005. Patient-Centered Care Improvement Stories, IHI.org.
- Care Experience Council, To see or not to see – Improving PCP access [monograph on the Internet] Oakland (CA): 2004 Mar. [cited 2006 Jan 25]. (about 20 pages). Available from: www.cl.kp.org/pkc/national/operations/cec/content/Primary_Care_Conference/Workshops/PCA_CONF_Carlton_etal_ToSeeorNottoSee_ImprovingPCPAccess_3_04.ppt. [Google Scholar]
- McDaniel RR., Jr. Complexity Science and Health Care Management, Advances in Health Care Management. Volume 2. Elsevier Science Ltd; 2001. pp. 11–36. pages. [Google Scholar]
- Care Experience Council. Successful practices in physician work environment—Summary report [monograph on the Internet] 2003 May. [cited 2006 Jan 25]; [p 11]. Available from: http://cscrdpkct001.crdc.kp.org:7800/search?q=successful+practices+in+the+physician+work+environment++summary+report&site=cec&getfields=url&client=cec&proxystylesheet=cec&output=xml_no_dtd&filter=0.


