Report of a Case
A 67-year-old man with a long-standing history of snoring noted that, in recent years, the snoring had worsened so much that his wife banned him from their bedroom. Since his retirement, he gained 20 pounds, and knee problems reduced his physical activity. His nasal allergies also had worsened. He noted increased fatigue, daytime sleepiness, and some trouble concentrating. He reported following a medication regimen as treatment for hypertension, but he otherwise denied having any medical problems. He had a tonsillectomy and adenoidectomy as a child and had no history of thyroid disease.
Physical examination showed nasal congestion with moderately swollen, pale turbinates and no purulent discharge. The septum was midline. Oropharyngeal examination showed no tonsils and a low soft palate with elongated uvula that tended to collapse against the posterior aspect of the pharynx and abutted the base of tongue. Fiberoptic laryngeal examination showed a normal larynx with moderate collapse of the lateral pharyngeal walls in “blocked” inspiration (a reverse Müller's maneuver whereby the patient holds his nose, closes his mouth, and attempts to breathe inward). He had a short, thick neck and was overweight.
The working diagnosis was obstructive sleep apnea.
Diagnosis of Obstructive Sleep Apnea
The reference standard for diagnosis of sleep disorders is to perform polysomnography (a sleep study), during which the sleeping patient is observed for oxygen saturation level, amount of oral and nasal airflow, degree of respiratory effort, electrocardiographic measurements, body position, and overall body movement. This examination can be done both “inhouse” in a sleep laboratory and with home sleep studies for which the patient is connected to monitors and observed in the patient's natural sleep environment.
On the basis of the apnea-hypopnea index, the severity of sleep apnea is categorized as mild, moderate, or severe. Mild sleep apnea is defined by an apnea-hypopnea index score anywhere from 5 to 14, oxygen saturation level of at least 86%, and minimal daytime disability. Moderate sleep apnea is defined by an index score anywhere from 15 to 30 or an oxygen saturation level of 80% to 85% and clinically significant dysfunction at work or socially because of daytime somnolence and loss of concentration. Severe sleep apnea is defined by an index score >30 or an oxygen saturation level of ≤79% and incapacitation caused by the sleep disorder.
Common causes of obstructive sleep apnea include obesity or excessive weight gain (fatty tissue in the throat tissue narrows and blocks the airway when the muscles relax), age (loss of muscle mass and tone in the upper airway), gender (men tend to have narrower airways than women), irregular sleep hours, anatomic abnormality (nasal obstruction, enlarged tongue, elongated soft palate, large tonsils and adenoids), use of alcohol and sedatives (relaxes the musculature), smoking (causes inflammation and swelling of the upper airway), and severe reflux (gastroesophageal reflux disease). Snoring is a common symptom of sleep apnea and results from obstruction, usually by the soft palate and uvula (Figure 1).1 However, snoring itself does not involve cessation of breathing, and many “snorers” have normal results of sleep studies.
Figure 1.
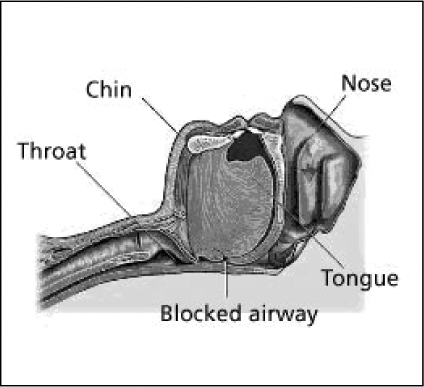
Diagram shows anatomic structures involved in snoring.
Adapted and reproduced by permission from: Abeloff D. Medical art: graphics for use. Baltimore: Williams & Wilkins; 1982.1
Treatment of Obstructive Sleep Apnea
Where “sleep classes” are available, most patients are referred to these classes, group appointments at which patients receive educational material on snoring and sleep apnea. This material advises patients to eliminate their use of alcohol, tobacco, and sedatives, to sleep on their side instead of their back, and to regularize their sleep hours. Overweight patients receive a plan for weight reduction and appropriate exercise to maintain mobility. Physicians prescribe intranasal steroid medication and nonsedating antihistamine drugs for nasal allergies.
Patients with moderate to severe sleep apnea are treated with continuous positive airway pressure (CPAP). This therapy requires the patient to wear a mask over their nose during sleep, when the pressure is adjusted to keep the airway open at night. Although CPAP therapy is the most effective treatment for obstructive sleep apnea, this therapy is often unsuccessful because of patient noncompliance: Some studies have reported compliance rates lower than 70%.2 The patient described in the present case report was treated with CPAP and noted substantial reduction in both fatigue and daytime somnolence.
Obstructive sleep apnea has been treated with many surgical procedures: uvulopalatopharyngoplasty (UPPP), a procedure which removes soft tissue at the back of the throat—uvula, tonsils (if present), and part of the redundant soft palate—but does not address problems originating at the base of tongue or hypopharynx; tonsillectomy and adenoidectomy (effective in some children); mandibular and hyoid advancement procedures (operations which are difficult, risky, and inconsistently successful); and radiofrequency ablation procedures (effective treatment for snoring but inconsistently successful for treating sleep apnea). All of these treatments have substantial risks and are only moderately successful. Tracheostomy is the most effective treatment because it bypasses the upper airway completely; however, this procedure is also the least popular and is technically challenging in the morbidly obese patient. For most patients, the postoperative care necessitated by tracheostomy makes this option untenable as an elective procedure.
Conclusion
Snoring is part of the spectrum of sleep-disordered breathing that may be a symptom of obstructive sleep apnea, but not all patients who snore have clinically significant sleep apnea. Snoring may be present in 30% to 50% of the general adult population, whereas 2% of women and 4% of men have clinically significant (moderate to severe) obstructive sleep apnea.3
Complications of untreated obstructive sleep apnea can include cardiovascular changes such as hypertension, ventricular dysfunction, or pulmonary hypertension. To determine the proper intervention required to reduce these complications, patients should receive a polysomnogram, either on an outpatient (“home” study) basis or in a sleep laboratory with a technician in attendance. Severity of sleep apnea does not always correlate with anatomic findings or with medical history; therefore, patients who snore should receive at least a nocturnal screening test measuring oxygen saturation and airflow, and patients with daytime somnolence or symptoms suggestive of sleep apnea should receive a full sleep study.
Patients with sleep apnea have an increased risk of airway problems after general anesthesia and should be observed carefully during the perioperative period. In addition, use of opioid and sedative drugs should be minimized for these patients to prevent airway compromise and desaturation.
To splint and keep the upper airway patent during sleep, the most effective treatment for sleep apnea is CPAP given at a level determined by results of a titration study; variations of this treatment include bi-level positive air pressure (BIPAP, a procedure in which expiratory pressure is lower than prescribed inspiratory pressure if high pressure is required) or auto titration (self-adjusting pressure).
Treatment for snoring may include weight loss, avoidance of supine sleeping position, sleeping with head elevated, avoidance of alcohol or sedatives at night, and treatment of nasal symptoms.
Treatment for snoring may include weight loss, avoidance of supine sleeping position, sleeping with head elevated, avoidance of alcohol or sedatives at night, and treatment of nasal symptoms. Patients who snore may opt to use a dental appliance at night or may consider various procedures for treating snoring—eg, radiofrequency ablation of the palate (somnoplasty), a procedure designed to stiffen the soft palate or to increase airway patency. These procedures are considered cosmetic and thus are not covered either by the Kaiser Foundation Health Plan or by other insurance providers, but many Head and Neck Surgery Departments will soon offer snoring treatment procedures on a fee-for-service basis.
References
- Abeloff D. Baltimore: Williams & Wilkins; 1982. Medical art: graphics for use. [Google Scholar]
- Flemons WW. Clinical practice. Ostructive sleep apnea. N Engl J Med. 2002 Aug 15;347(7):498–504. doi: 10.1056/NEJMcp012849. [DOI] [PubMed] [Google Scholar]
- Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993 Apr 29;328(17):1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
Recommended Reading
- Dart RA, Gregoire JR, Gutterman DD, Woolf SH. The association of hypertension and secondary cardiovascular disease with sleep-disordered breathing. Chest. 2003 Jan;123(1):244–60. doi: 10.1378/chest.123.1.244. [DOI] [PubMed] [Google Scholar]
- Dreher A, de la Chaux R, Klemens C, et al. Correlation between otorhinolaryngologic evaluation and severity of obstructive sleep apnea syndrome in snorers. Arch Otolaryngol Head Neck Surg. 2005 Feb;131(2):95–8. doi: 10.1001/archotol.131.2.95. [DOI] [PubMed] [Google Scholar]
- Iseri M, Balcioglu O. Radiofrequency versus injection snoreplasty in simple snoring. Otolaryngol Head Neck Surg. 2005 Aug;133(2):224–8. doi: 10.1016/j.otohns.2005.04.018. [DOI] [PubMed] [Google Scholar]
- Riley RW, Powell NB, Li KK, Troell RJ, Guilleminault C. Surgery and obstructive sleep apnea: long-term clinical outcomes. Otolaryngol Head Neck Surg. 2000 Mar;122(3):415–21. doi: 10.1016/S0194-5998(00)70058-1. [DOI] [PubMed] [Google Scholar]
- Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996 Feb;19(2):156–77. doi: 10.1093/sleep/19.2.156. [DOI] [PubMed] [Google Scholar]


