Abstract
Background
Plasma antibody measurements of antibody levels to periodontal pathogens may be used to support diagnosis, disease activity, classification, and prognosis of periodontitis.
Objective
The aim of this study was to investigate the long-term stability of plasma antibody levels against Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis.
Design
Plasma immunoglobulin G (IgG) antibody levels against the pathogens were analyzed annually during 15 years from 21 voluntary subjects, whose periodontal status was not known at the point of selection. The total number of plasma samples was 315. In connection of the last sampling, the clinical and radiographic periodontal status was examined. Pooled bacterial samples from periodontal pockets, as well as salivary samples were collected for A. actinomycetemcomitans and P. gingivalis detection, and antibody determinations, respectively. According to the clinical status, six subjects had periodontitis, whereas 15 did not.
Results
Plasma IgG-class antibody levels to periodontal pathogens remained extremely stable during the 15-year period and no significant (p>0.05) intra-individual variations were observed. Retrospectively, the average plasma IgG antibody levels against A. actinomycetemcomitans and P. gingivalis were 1.6–2.3 (p<0.05) and 1.4–1.7 (p<0.05) fold higher in the subjects with periodontitis than those without, respectively, during the whole 15-year tracking. As expected, at the time of the periodontal examination the plasma and salivary IgG antibody levels were associated both with periodontitis and bacterium-positivity.
Conclusions
Plasma IgG levels against A. actinomycetemcomitans and P. gingivalis are extremely stable during 15 years both in subjects with and without periodontitis.
Keywords: Aggregatibacter actinomycetemcomitans, longitudinal studies, periodontitis, plasma, oral infections, Porphyromonas gingivalis, saliva
Major periodontal pathogens include Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis. The association between P. gingivalis and periodontitis is stronger even though a carrier-state of the species may exist (1). A. actinomycetemcomitans has a dual role in the oral flora: it has been associated with aggressive forms of periodontitis (2), but the bacterium can also be found in the oral cavity of healthy individuals (3). The bacterial load in periodontal pockets leads to the activation of host-bacterial interactions. To establish an infection, the pathogen must overcome numerous surface barriers, such as epithelium and mucus, and also the innate immunity and adaptive immunity (4). Periodontal pathogens stimulate B cell activation mainly through classical antigen-specific immune response. A. actinomycetemcomitans and P. gingivalis are capable of inducing high antibody response that can in fact exceed those found in many other pathological bacterial infections (5).
Plasma and saliva antibody measurements have been used to diagnose periodontitis, estimate its activity, classification and prognosis, and success of treatment (5). Several studies have reported elevated levels of plasma immunoglobulin G (IgG) against periodontal pathogens especially in patients with aggressive periodontitis (6–9). Immunoglobulin A (IgA) is the predominant immunoglobulin in saliva, and salivary IgA plays a role in the local immune defense system. In addition to the plasma-derived IgG and IgA, certain subclasses of IgG and IgA can be produced locally in the periodontal pockets (10). Antibody production, especially that of IgG and IgA, is considered to have a protective role in the pathogenesis of periodontitis (11, 12). It has also been suggested that antibodies may not necessarily need to decrease periodontal pathogen loads in order to exert a protective effect, but they may neutralize toxins and proteolytic enzymes as well as promote opsonization, and complement activation (11).
The stability of IgG-class antibody levels has been investigated in a few follow-up studies. The follow-up time in those studies has varied from two to three years (13, 14). IgG-class antibody levels showed long-term stability; no decrease has been reported after periodontal treatment (6, 14) or treatment has lowered the IgG levels only temporarily (15).
Earlier studies have mainly focused on the relationship between antibody levels and severity of periodontitis or between bacterial presence and their homologous antibodies. The aim in this study was therefore to investigate the long-term stability of plasma antibody levels against A. actinomycetemcomitans and P. gingivalis in plasma samples analyzed annually from the same individuals during 15 years.
Material and methods
Subject sample
This report is based on the 15-year collection of blood samples from a rural population in Leppävirta, Savolax, Finland, whose selenium status was followed by annual blood sampling. The original sample included 26 men and 19 women in 1985 (16). The local public health-care center recruited subjects. Volunteers for the periodontal examination were recruited by a questionnaire, and 9 men and 12 women participated. During the 15 years, the subjects had had dental check-ups by their general practitioners and none of them had previously been treated by a periodontologist. However, they were instructed to seek periodontal treatment after the examination if necessary. The characteristics of the participants at the end of the study are shown in Table 1. All the participating subjects gave their informed consent.
Table 1.
Clinical characteristics in periodontitis (n=6) and periodontally healthy (n=15) subjects in the end of the study
| Periodontitis | Periodontally healthy | ||
|---|---|---|---|
| Variable | n (%) | n (%) | p-Valuea |
| Gender | |||
| Men | 1 (17) | 8 (53) | ns |
| Women | 5 (83) | 7 (47) | ns |
| General health | |||
| Elevated blood pressure | 3 (50) | 2 (13) | ns |
| Cardiovascular diseases | 2 (33) | 0 | ns |
| Diabetes (type II) | 0 | 1 (7) | ns |
| Osteoporosis | 0 | 1 (7) | ns |
| Current smoking | 0 | 3 (20) | ns |
| Mean±SD | Mean±SD | ||
| Age | 66±5 | 59±13 | 0.302 |
| Periodontal examination | |||
| Total number of teeth | 19.5±4.1 | 15.7±10.8 | 0.569 |
| Visible plaque (% of sites) | 13.33±9.2 | 11.2±9.6 | 0.558 |
| Bleeding on probing (% of sites) | 36.8±9.5 | 24.6±17.2 | 0.112 |
| Number of teeth with periodontal pockets (≥5 mm) | 2.0±2.5 | 0 | 0.000 |
| Periodontal pockets (% of sites) | 1.8±2.3 | 0 | 0.000 |
| Clinical attachment loss (mm) | 4.17±4.54 | 0 | 0.000 |
| Highest CPITN valueb | 3.8±0.4 | 2.4±0.5 | 0.000 |
| Total number of angular bony defectsc | 1.5±2.0 | 0.3±0.5 | 0.213 |
Mann–Whitney test or Chi-square test.
CPITN=community periodontal index of treatment needs. Tracking of plasma antibodies against Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis during 15 years.
Radiological analyses.
Note: ns=non-significant.
Clinical and radiographic examination
The subjects were examined with respect to visible plaque and bleeding on probing (17), probing depth (periodontal pockets ≥5 mm), and clinical attachment loss at six sites per tooth, at all present teeth (Table 1). One dentist (JA) performed all the clinical examinations. WHO probe (LM Dental LM 550B Si, LM-instruments Oy/Ab, Pargas, Finland) was used in the examinations. Subjects were categorized into those with and without periodontitis according to the following criteria: subjects with periodontitis had at least one site with a periodontal pocket deeper than 5 mm and clinical attachment loss (see Table 1).
Periodontal status and possible infectious foci of periodontium and/or alveolar bone were detected from analog panoramic tomographs. The number of peri-apical lesions, angular bony defects (they were at least to the middle third of the root length), furcation lesions in molars, and pericoronitis in third molars were recorded.
Plasma and salivary samples
Plasma samples were collected once a year for 15 years from the 21 participants and stored at −20°C. The following samples were collected at the end of the 15-year period.
Paraffin-stimulated salivary samples were collected for five minutes. The salivary sample was divided into two aliquots, of which 2 ml was centrifuged immediately at 12,000 rpm for five minutes and frozen on dry ice. The frozen samples were brought to the research laboratory at the Institute of Dentistry, University of Helsinki, Helsinki, within 48 hours and stored at −70°C.
Bacterial samples and antibody measurements
From the 21 participants in the study, pooled bacterial samples from the 14 most inflamed periodontal pockets in each subject were collected with sterile curettes at the end of the study. The samples were transported to the laboratory in vials containing 2 ml of viability preserving medium no. III (VMGA III) medium, and cultured. A. actinomycetemcomitans and P. gingivalis were identified as previously described (18, 19). Briefly, for A. actinomycetemcomitans, 100-µl aliquots of undiluted and 10−2 dilutions of samples were inoculated on Trypic soy bacitracin vancomycin (TSBV)-agar plates and incubated in 5% CO2 in air at 36°C for three days. A. actinomycetemcomitans grew as typical adherent colonies, which were catalase-positive. For P. gingivalis, 100-µl aliquots of 10−4 and 10−5 were inoculated on Brucella agar plates and incubated in anaerobic jars at 37°C for 10 days. P. gingivalis grew as dark-pigmented colonies, which had positive trypsin-like enzyme activity as detected with carbo-benzoxy-L-arginine-7-amino-4-methylcoumarin amide HCl (CAAM)-reagent.
Bacterial DNA was isolated from the VMGA III medium according to the manufacturer's instructions using Chelex 100 resin, and A. actinomycetemcomitans and P. gingivalis were detected by PCR as reported earlier (20, 21). In every series of PCR, chromosomal DNA extracted from A. actinomycetemcomitans (ATCC43718) and P. gingivalis (W50) strains served as positive controls, and water served as a negative control.
Plasma IgG and salivary IgG and IgA antibodies against A. actinomycetemcomitans and P. gingivalis were detected by multiserotype-ELISA as previously described (6). The strains used as formalin-killed whole cell antigens were ATCC29523, ATCC43781, ATCC33384, IDH781, IDH1708, and C59 representing A. actinomycetemcomitans serotypes a, b, c, d, e, and a non-serotypeable strain, respectively, and ATCC33277, W50, and OMGS434 representing P. gingivalis serotypes a, b, and c, respectively. Plasma or saliva diluted in antibody buffer (PBS containing 0.05% Tween 20 and 0.5% bovine plasma albumin) was incubated at room temperature for two hours. For the determinations, four dilutions of each sample were used in duplicate. The dilutions were as follows: plasma samples for the detection of A. actinomycetemcomitans IgG 1:500, 1:1,500, 1:4,500, and 1:13,500 and for the detection of P. gingivalis IgG 1:100, 1:400, 1:1,600, and 1:6,400, and salivary samples for the detection of either A. actinomycetemcomitans or P. gingivalis IgG and IgA were 1:3.3, 1:10, 1:30, and 1:90. The results were calculated as Area under the plasma concentration time curve (AUC) from the dilution curves. The inter-assay coefficients for variation as calculated from values of the reference serum applied on each plate were 6.3 and 5.5% for A. actinomycetemcomitans and 5.1 and 4.7% for P. gingivalis IgA and IgG, respectively.
Statistical analysis
Data analysis was performed using the SPSS for Windows, version 13.0 (SPSS Inc, Chicago, IL, USA). Differences in the clinical characteristics and antibody levels between the two study groups were analyzed by the Mann−Whitney U test or Chi-square test. Interactions between parameters were examined using Pearson Correlation. The statistical significance of the intra-individual differences in annual plasma IgG levels was analyzed by the Kruskall–Wallis test. P-values ≤0.05 were considered as statistically significant.
Results
Demographic and clinical data
Table 1 provides a summary of the demographic and clinical data of the subject sample. According to our classification criteria, the subjects with periodontitis at the time of the clinical examination had higher number of deep (≥5 mm) periodontal pockets, attachment loss levels, and community periodontal index of treatment needs (CPITN) value compared to those without periodontitis. No differences were found in the bleeding on probing and visible plaque or in the number of angular bony defects detected from the radiographic pictures between the two groups. There were no statistical differences in the general health and current smoking between the subjects with (n=6) and without (n=15) periodontitis.
Antibody levels at the end of the study
Mean plasma and salivary IgG antibody and salivary IgA antibody levels against A. actinomycetemcomitans and P. gingivalis in the periodontitis and non-periodontitis groups at the end of the study are shown in Table 2. Mean salivary IgG antibody levels against A. actinomycetemcomitans and both salivary and plasma IgG levels against P. gingivalis were significantly higher in subjects with periodontitis compared to the levels in the periodontally healthy subjects. There were no differences in the salivary IgA antibody levels against A. actinomycetemcomitans and P. gingivalis between the groups.
Table 2.
Antibody levels in periodontitis and periodontally healthy subjects in the end of the study
| Variable | Periodontitis | Periodontally healthy | p-Valuea |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Plasma antibody levels (EU)b | |||
| A. actinomycetemcomitans IgG | 20.51±12.76 | 11.06±5.70 | 0.066 |
| P. gingivalis IgG | 20.35±6.76 | 11.94±4.26 | 0.008 |
| Salivary antibody levels (EU) | |||
| A. actinomycetemcomitans IgG | 0.63±0.58 | 0.14±0.16 | 0.045 |
| A. actinomycetemcomitans IgA | 1.11±0.88 | 0.59±0.50 | 0.205 |
| P. gingivalis IgG | 0.44±0.39 | 0.03±0.02 | 0.001 |
| P. gingivalis IgA | 0.85±0.76 | 0.46±0.37 | 0.235 |
Mann–Whitney test.
EU=ELISA units.
Long-term inter and intra-individual antibody variations
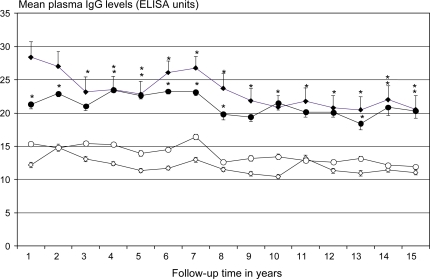
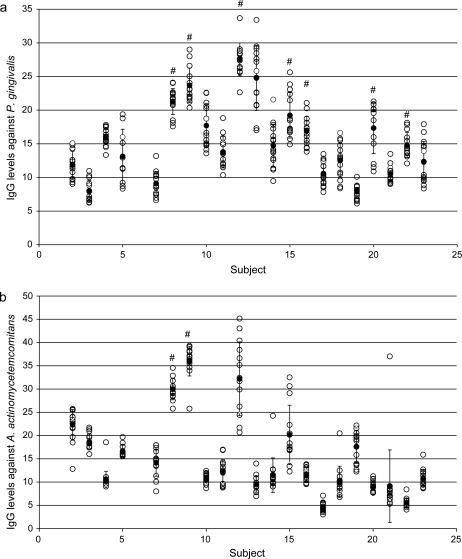
The mean annual plasma antibody IgG levels against A. actinomycetemcomitans and P. gingivalis during the 15-year period in subjects with and without periodontitis are shown in Fig. 1. Plasma IgG levels against A. actinomycetemcomitans were 1.6–2.3 fold higher in subjects with periodontitis than in those without (p<0.05). Mean IgG levels against P. gingivalis were 1.4–1.7 fold higher in subjects with periodontitis than in periodontally healthy subjects (p<0.05). The intra-individual variation in plasma IgG antibodies against P. gingivalis (Fig. 2a) and A. actinomycetemcomitans (Fig. 2b) during the 15 years are shown for all subjects. The individual variation during the study was not statistically significant in any of the subjects.
Fig. 1.
Plasma immunoglobulin G (IgG) levels against A. actinomycetemcomitans and P. gingivalis levels during 15 years. The classification into those with and without periodontitis was done in the connection of the last sampling. The A. actinomycetemcomitans levels (ELISA units, mean±SEM) of periodontitis subjects (n=6) (♦) and periodontally healthy subjects (n=15) (⋄), P. gingivalis levels (ELISA units, mean±SEM) in periodontitis subjects (•) and periodontally healthy subjects (○). Statistically significant differences are marked with asterisk (p<0.05).
Fig. 2.
Individual variation in plasma immunoglobulin G (IgG) levels (ELISA units) against P. gingivalis (a) and A. actinomycetemcomitans (b) during 15 years. The box plot columns show antibody levels in each year (○), mean antibody levels (•), and standard deviation (vertical lines). One box plot column represents one subject. Subjects marked with # are those who were PCR-positive for P. gingivalis (a) and A. actinomycetemcomitans (b) at the end of the study.
Detection of bacteria
Mean plasma and salivary IgG levels were associated with the bacteria detected by PCR (Table 3). IgG levels against A. actinomycetemcomitans and P. gingivalis in both plasma and saliva were significantly higher in subjects positive for A. actinomycetemcomitans and P. gingivalis compared to the subjects negative for the bacteria, respectively. Salivary IgA levels against A. actinomycetemcomitans and P. gingivalis were not significantly elevated in PCR-positive subjects for either of the bacteria. Of the two A. actinomycetemcomitans PCR-positive subjects one was culture-positive. Seven subjects were PCR-positive for P. gingivalis, and five of them were culture-positive.
Table 3.
Antibody levels in subjects positive and negative for PCR-detected A. actinomycetemcomitans and P. gingivalis in the end of the study
| PCR negative Mean±SD | PCR-positive Mean±SD | p-Valuea | |
|---|---|---|---|
| Antibodies against A. actinomycetemcomitans | Negative for A. actinomycetemcomitans | Positive for A. actinomycetemcomitans | |
| n=19b | n=2c | ||
| IgG in plasma | 11.45±5.70 | 35.72±1.65 | 0.023 |
| IgG in saliva | 5.05±5.59 | 21.29±1.84 | 0.023 |
| IgA in saliva | 16.72±10.05 | 27.73±6.47 | 0.093 |
| Antibodies against P. gingivalis | Negative for P. gingivalis | Positive for P. gingivalis | |
| n=14d | n=7e | ||
| IgG in plasma | 11.89±4.24 | 19.24±7.06 | 0.014 |
| IgG in saliva | 0.03±0.02 | 0.38±0.39 | 0.007 |
| IgA in saliva | 0.48±0.38 | 0.76±0.72 | 0.456 |
Mann–Whitney U test.
Subjects negative for PCR detection of. A. actinomycetemcomitans.
Subjects positive for PCR detection of A. actinomycetemcomitans.
Subjects negative for PCR detection of P. gingivalis.
Subjects positive for PCR detection of P. gingivalis.
Correlation analyses
Correlation coefficients between the periodontal status and plasma, and salivary IgG and IgA antibody levels against A. actinomycetemcomitans and P. gingivalis at the end of the study are shown in Table 4. The number of angular bony defects correlated with IgG antibody levels against P. gingivalis in plasma and saliva and IgA antibody levels against A. actinomycetemcomitans in saliva. The number of deepened periodontal pockets (≥5 mm) correlated with IgG antibody levels against P. gingivalis in both plasma and saliva, IgA antibody levels against P. gingivalis in saliva, and IgG and IgA antibody levels against A. actinomycetemcomitans in saliva. Mean clinical attachment loss correlated with IgG and IgA antibody levels against P. gingivalis and A. actinomycetemcomitans in both plasma and saliva. The highest CPITN value correlated with IgG levels against P. gingivalis and A. actinomycetemcomitans in both plasma and saliva.
Table 4.
Correlation coefficients between plasma IgG levels to A. actinomycetemcomitans and P. gingivalis and periodontal status at the time of periodontal examination
| Pg IgG in plasma | Aa IgG in plasma | Pg IgA in saliva | Pg IgG in saliva | Aa IgA in saliva | Aa IgG in saliva | Highest CPI value | Mean attachment loss (mm) | Periodontal pocketsa | Vertical bone loss (number of pockets) | Bleeding on probing (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bleeding on probing (%) | 0.164 | 0.225 | 0.064 | 0.262 | 0.125 | 0.210 | 0.233 | 0.258 | 0.170 | 0.050 | 1 |
| Vertical bone loss (number of pockets) | 0.589* | 0.264 | 0.660* | 0.623* | 0.633* | 0.432 | 0.381 | 0.451 | 0.901 | 1 | |
| Periodontal pocketsa | 0.564* | 0.315 | 0.515* | 0.642* | 0.548* | 0.438* | 0.535* | 0.380 | 1 | ||
| Mean attachment loss (mm) | 0.637* | 0.637* | 0.660* | 0.895* | 0.581* | 0.798* | 0.598* | 1 | |||
| Highest CPIb value | 0.628* | 0.526* | 0.224 | 0.663* | 0.236 | 0.498* | 1 | ||||
| Aa IgGcin saliva | 0.664* | 0.881* | 0.719* | 0.895* | 0.713* | 1 | |||||
| Aa IgAcin saliva | 0.513* | 0.497* | 0.938* | 0.706* | 1 | ||||||
| Pg IgGcin saliva | 0.783* | 0.729* | 0.732* | 1 | |||||||
| Pg IgAcin saliva | 0.452* | 0.504* | 1 | ||||||||
| Aa IgGcin plasma | 0.493* | 1 | |||||||||
| Pg IgGcin plasma | 1 |
Number of sites with deepened (≥5 mm) periodontal pockets.
CPI = clinical plaque index.
ELISA units per stimulated salivary flow rate.
Statistically significant (p<0.05).
Discussion
Tracking of plasma antibodies
The present study is a retrospective 15-year tracking of plasma antibody levels against A. actinomycetemcomitans and P. gingivalis. Throughout the whole time frame, the mean plasma antibody levels remained extremely stable, and only minor, non-significant individual variation was seen. Furthermore, our data showed elevated mean antibody levels against both A. actinomycetemcomitans and P. gingivalis in subjects, who were diagnosed as having periodontitis at the end of the 15-year time period, compared to the periodontally healthy.
The main result in the present study was the remarkable stability of plasma IgG levels in both the periodontitis and periodontally healthy subjects, even though the periodontal classification was done at the end of the study. The limitation of the study is that we did not have the dental history of the subjects who participated in the study, and it is possible that they had had active periodontitis at some point during the 15 years. This is, however, not likely since at the time of the dental examination, none of them were currently in periodontal treatment or in the maintenance care. The subjects had got occasional periodontal treatment by their general practitioners, but none of them had sought for treatment by a specialized periodontologist.
The antibody detection method we use in our laboratory has been published earlier (22). Antigens in the assay represent A. actinomycetemcomitans serotypes a–e and a non-serotypeable strain, and P. gingivalis serotypes a–c (6). When the IgG-class antibody levels to pathogens are summed up, the assay has a specificity and sensitivity of 90 and 71%, respectively, for finding periodontitis by measuring antibody levels from plasma samples (6). Since the aim of the present study, however, was not to validate further the multiserotype-ELISA, the antibody levels were not summed up.
Our findings are consistent with previous studies. Papapanou and co-workers demonstrated an overall stability of plasma IgG-class antibody titers to 19 periodontal bacteria over a 30-month period for both periodontitis patients and periodontally intact control subjects (14). Periodontal treatment among those with the disease did not affect the plasma antibody levels. Furthermore, Dye and co-workers (2009) reported that serum IgG titers to selected periodontal species are feasible in epidemiologic studies using a combined serologic/demographic approach (23). Several other studies have shown higher plasma IgG levels against specific periodontal pathogens in patients with periodontitis than in periodontally healthy individuals (5, 9, 24, 25). It has been suggested that elevated antibody levels against A. actinomycetemcomitans and P. gingivalis exert a protective role in the progression of periodontitis (11). In a 36-month follow-up study, the patients who had low homologous plasma antibody levels together with cultivable A. actinomycetemcomitans and P. gingivalis, showed a positive predictive value for periodontitis disease recurrence (11). Our retrospective study, however, does not suggest a protective role for the plasma IgG-class antibody levels.
Cultivable A. actinomycetemcomitans and P. gingivalis can serve as markers for destructive periodontal disease in adult subjects (26). In the present study, we were able to detect two A. actinomycetemcomitans-positive subjects and seven P. gingivalis-positive subjects by PCR. From those subjects, bacteria could be cultivated in one and five cases, respectively. Plasma and salivary IgG levels were elevated in the P. gingivalis-positive subjects as detected with both PCR method and cultivation. In the A. actinomycetemcomitans-positive subjects, the plasma and salivary IgG levels were elevated in the PCR-positive group. This can be explained by the small number of A. actinomycetemcomitans-positive subjects in the population.
Plasma and salivary IgG levels correlated with each other. At the year of periodontal examination, both plasma and salivary antibody levels against P. gingivalis were significantly higher in the periodontitis group than in the periodontally healthy group. Concerning A. actinomycetemcomitans only the salivary IgG levels were elevated in the periodontitis group. A trend was seen also for plasma IgG against A. actinomycetemcomitans to be elevated in the periodontitis group even though not statistically significant. The small study population may explain this; from 28 subjects participating originally in the study annually during the 15 years, only 21 attended the clinical examination. In addition, all affected subjects had chronic periodontitis, that is more commonly associated with the presence of P. gingivalis than A. actinomycetemcomitans (27). Although IgA is the predominant immunoglobulin in saliva, our study showed elevated salivary IgG levels against both A. actinomycetemcomitans and P. gingivalis in periodontitis. In the whole saliva samples, the total immunoglobulin originates both from crevicular fluid and exocrine secretion. Therefore, there is some discrepancy compared to previous studies, in which salivary IgA have been measured in subjects with periodontitis.
Hägewald and co-workers reported that a group of patients with aggressive periodontitis had lower total IgA levels than periodontally healthy subjects (28), whereas Henskens and associates found no difference in saliva IgA concentrations between patients with chronic periodontitis and periodontally healthy subjects (29). The present study supports the latter observation showing no differences in the IgA levels of periodontitis and periodontally healthy groups.
Overall, plasma and salivary IgG and IgA levels against A. actinomycetemcomitans and P. gingivalis correlated significantly with periodontal status. There was a positive correlation with the number of sites with deepened periodontal pockets, mean attachment loss, and angular bony defects detected from the radiographic pictures. Only three of the 21 participants in the present study were current smokers, and all of them belonged to the periodontally healthy group. Smoking is a strong risk factor for periodontal diseases and may have an impact also on immunoglobulin levels (8, 12, 30), but in this study the number of current smokers was too small to study the effect of smoking on the antibody production.
In conclusion, the mean plasma IgG levels against A. actinomycetemcomitans and P. gingivalis were stable during the entire 15-year period. The mean plasma antibody levels were also correlated with the periodontal status, the levels were significantly higher in subjects with periodontitis compared to the periodontally healthy. In this study population, periodontitis was moderate and the number of subjects with periodontitis was small. Therefore, further studies are needed to confirm the observations among patients with severe periodontitis.
Acknowledgements
Ms Tiina Karvonen is acknowledged for excellent technical assistance. The study was financially supported by the Academy of Finland (#118391 for PJP) and Finnish dental society Apollonia (for LL).
Conflict of interest and funding
The authors declare that they have no conflict of interest. This study was supported by the Academy of Finland (#118391 for PJP).
References
- 1.Könönen E, Paju S, Pussinen PJ, Hyvönen M, Di Tella P, Suominen-Taipale L, et al. Population-based study of salivary carriage of periodontal pathogens in adults. J Clin Microbiol. 2007;8:2446–51. doi: 10.1128/JCM.02560-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Slots J, Reynolds HS, Genco RJ. Actinobacillus actinomycetemcomitans in human periodontal disease: a cross-sectional microbiological investigation. Infect Immun. 1980;29:1013–20. doi: 10.1128/iai.29.3.1013-1020.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zambon JJ. Actinobacillus actinomycetemcomitans in human periodontal disease. J Clin Periodontol. 1985;12:1–20. doi: 10.1111/j.1600-051x.1985.tb01348.x. [DOI] [PubMed] [Google Scholar]
- 4.Delves PJ, Roitt IM. The immune system. Second of two parts. New Engl J Med. 2000;343:108–17. doi: 10.1056/NEJM200007133430207. [DOI] [PubMed] [Google Scholar]
- 5.Kinane DF, Mooney J, Ebersole JL. Humoral immune response to Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis in periodontal disease. Periodontol 2000. 1999;20:289–340. doi: 10.1111/j.1600-0757.1999.tb00164.x. [DOI] [PubMed] [Google Scholar]
- 6.Pussinen PJ, Vilkuna-Rautiainen T, Alfthan G, Mattila K, Asikainen S. Multiserotype enzyme-linked immunosorbent assay as a diagnostic aid for periodontitis in large-scale studies. J Clin Microbiol. 2002;40:512–8. doi: 10.1128/JCM.40.2.512-518.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung HY, Lu HC, Chen WL, Lu CT, Yang YH, Tsai CC. Immunoglobulin G profiles in different forms of periodontitis. J Periodontal Res. 2003;38:471–6. doi: 10.1034/j.1600-0765.2003.00675.x. [DOI] [PubMed] [Google Scholar]
- 8.Graswinckel JE, van der Velden U, van Winkelhoff AJ, Hoek FJ, Loos BG. Plasma antibody levels in periodontitis patients and controls. J Clin Periodontol. 2004;31:562–8. doi: 10.1111/j.1600-051X.2004.00522.x. [DOI] [PubMed] [Google Scholar]
- 9.Wang D, Kawashima Y, Nagasawa T, Takeuchi Y, Kojima T, Umeda M, et al. Elevated serum IgG titer and avidity to Actinobacillus actinomycetemcomitans serotype c in Japanese periodontitis patients. Oral Microbiol Immunol. 2005;20:172–9. doi: 10.1111/j.1399-302X.2005.00208.x. [DOI] [PubMed] [Google Scholar]
- 10.Lundqvist C, Baranov V, Teglund S, Hammarström S, Hammarström ML. Cytokine profile and ultrastructure of intraepithelial gamma delta T cells in chronically inflamed human gingiva suggest a cytotoxic effector function. J Immunol. 1994;153:2302–12. [PubMed] [Google Scholar]
- 11.Rams TE, Listgarten MA, Slots J. Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis subgingival presence, species-specific serum immunoglobulin G antibody levels, and periodontitis disease recurrence. J Periodontal Res. 2006;41:228–34. doi: 10.1111/j.1600-0765.2005.00860.x. [DOI] [PubMed] [Google Scholar]
- 12.Kinane DF, Mark Bartold P. Clinical relevance of the host responses of periodontitis. Periodontol 2000. 2007;43:278–93. doi: 10.1111/j.1600-0757.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 13.Ehmke B, Beikler T, Haubitz I, Karch H, Flemmig TF. Multifactorial assessment of predictors for prevention of periodontal disease progression. Clin Oral Investig. 2003;7:217–21. doi: 10.1007/s00784-003-0227-2. [DOI] [PubMed] [Google Scholar]
- 14.Papapanou PN, Neiderud AM, Disick E, Lalla E, Miller GC, Dahlén G. Longitudinal stability of serum immunoglobulin G responses to periodontal bacteria. J Clin Periodontol. 2004;31:985–90. doi: 10.1111/j.1600-051X.2004.00599.x. [DOI] [PubMed] [Google Scholar]
- 15.Ebersole JL, Cappelli D, Steffen MJ, Willmann DE, O'Dell DS. Host response assessment in recurring periodontitis. J Clin Periodontol. 1996;23:258–62. doi: 10.1111/j.1600-051x.1996.tb02085.x. [DOI] [PubMed] [Google Scholar]
- 16.Varo P, Alfthan G, Ekholm P, Aro A, Koivistoinen P. Selenium intake and serum selenium in Finland: effects of soil fertilization with selenium. Am J Clin Nut. 1988;48:324–9. doi: 10.1093/ajcn/48.2.324. [DOI] [PubMed] [Google Scholar]
- 17.Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25:229–35. [PubMed] [Google Scholar]
- 18.Asikainen S, Alaluusua S, Kari K, Kleemola-Kujala E. Subgingival microflora and periodontal conditions in healthy teenagers. J Periodontol. 1986;57:505–9. doi: 10.1902/jop.1986.57.8.505. [DOI] [PubMed] [Google Scholar]
- 19.Saarela M, Stucki AM, von Troil-Lindén B, Alaluusua S, Jousimies-Somer H, Asikainen S. Intra- and inter-individual comparison of Porphyromonas gingivalis genotypes. FEMS Immunol Med Microbiol. 1993;6:99–102. doi: 10.1111/j.1574-695X.1993.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 20.Ashimoto A, Chen C, Bakker I, Slots J. Polymerase chain reaction detection of 8 putative periodontal pathogens in subgingival plaque of gingivitis and advanced periodontitis lesions. Oral Microbiol Immunol. 1996;11:266–73. doi: 10.1111/j.1399-302x.1996.tb00180.x. [DOI] [PubMed] [Google Scholar]
- 21.Mättö J, Saarela M, Alaluusua S, Oja V, Jousimies-Somer H, Asikainen S. Detection of Porphyromonas gingivalis from saliva by PCR by using a simple sample-processing method. J Clin Microbiol. 1998;36:157–60. doi: 10.1128/jcm.36.1.157-160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vilkuna-Rautiainen T, Pussinen PJ, Mattila K, Vesanen M, Ahman H, Dogan B, et al. Antigenically diverse reference strains and autologous strains of Actinobacillus actinomycetemcomitans are equally efficient antigens in enzyme-linked immunosorbent assay analysis. J Clin Microbiol. 2002;40:4640–5. doi: 10.1128/JCM.40.12.4640-4645.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dye BA, Herrera-Abreu M, Lerche-Sehm J, Vlachojannis C, Pikdoken L, Pretzl B, et al. Serum antibodies to periodontal bacteria as diagnostic markers of periodontitis. J Periodontol. 2009;80:634–47. doi: 10.1902/jop.2009.080474. [DOI] [PubMed] [Google Scholar]
- 24.Naito Y, Okuda K, Takazoe I. Immunoglobulin G response to subgingival gram-negative bacteria in human subjects. Infect Immun. 1984;45:47–51. doi: 10.1128/iai.45.1.47-51.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Craig RG, Boylan R, Yip J, Mijares D, Imam M, Socransky SS, et al. Serum IgG antibody response to periodontal pathogens in minority populations: relationship to periodontal disease status and progression. J Periodontal Res. 2002;37:132–46. doi: 10.1034/j.1600-0765.2002.00031.x. [DOI] [PubMed] [Google Scholar]
- 26.van Winkelhoff AJ, Loos BG, van der Reijden WA, van der Velden U. Porphyromonas gingivalis, Bacteroides forsythus and other putative periodontal pathogens in subjects with and without periodontal destruction. J Clin Periodontol. 2002;29:1023–8. doi: 10.1034/j.1600-051x.2002.291107.x. [DOI] [PubMed] [Google Scholar]
- 27.Haffajee AD, Socransky SS. Microbial etiological agents of destructive periodontal diseases. Periodontol 2000. 1994;5:78–111. doi: 10.1111/j.1600-0757.1994.tb00020.x. [DOI] [PubMed] [Google Scholar]
- 28.Hägewald S, Bernimoulin JP, Köttgen E, Kage A. Salivary IgA subclasses and bacteria-reactive IgA in patients with aggressive periodontitis. J Periodontal Res. 2002;37:333–9. doi: 10.1034/j.1600-0765.2002.00337.x. [DOI] [PubMed] [Google Scholar]
- 29.Henskens YM, van den Keijbus PA, Veerman EC, Van der Weijden GA, Timmerman MF, Snoek CM, et al. Protein composition of whole and parotid saliva in healthy and periodontitis subjects. Determination of cystatins, albumin, amylase and IgA. J Periodontal Res. 1996;31:57–65. doi: 10.1111/j.1600-0765.1996.tb00464.x. [DOI] [PubMed] [Google Scholar]
- 30.Apatzidou DA, Riggio MP, Kinane DF. Impact of smoking on the clinical, microbiological and immunological parameters of adult patients with periodontitis. J Clin Periodontol. 2005;32:973–83. doi: 10.1111/j.1600-051X.2005.00788.x. [DOI] [PubMed] [Google Scholar]