1. Introduction
Depression is widely studied among adolescents due to its potential negative impact on future life choices and experiences (Lewinsohn, Hops, Roberts, Seeley, & Andrews, 1993), correlation to future depression (Canals, Domènech-Llaberia, Fernández-Ballart, & Martí-Henneberg, 2002; Monroe, Rohde, Seeley, & Lewinsohn, 1999), co-occurrence with other disorders such as anxiety and substance abuse (Hjemdal, Aune, Reinfjell, Stiles, & Friborg, 2007; Petersen et al., 1993), connection to suicide attempts in adolescents (Joe, Baser, Neighbors, Caldwell, & Jackson, 2009; Petersen et al., 1993), and its contribution to the global disease burden (Merry, McDowell, Wild, Bir, & Cunliffe, 2004). Extant research suggests that by the age of 18, up to 24% of adolescents will have experienced at least one incident of major depressive disorder (Kowalenko et al., 2002). Though mental disorders are evident in adolescents in general, Black adolescents have been characterized as a particularly vulnerable group especially regarding the occurrence of depression (Gibbs, 1990; Myers, 1989; Rosella & Albrecht, 1993). Indeed, studies indicate that Black adolescents experience depression at disproportionately higher levels than adolescents from other racial/ethnic groups (Roberts, Roberts, & Chen, 1997; Wu et al., 1999).
1.1 Mental health service use among adolescents
Numerous alternatives for the treatment of depression exist; however, service use among the adolescent population remains low (SAMHSA, 2009a). In general, approximately 80% of young people that need mental health treatment are not accessing suitable, appropriate care (National Advisory Mental Health Council, 1990; US Department of Health and Human Services [USDHHS], 1999). Moreover, ethnic minority youth represent a notably susceptible group regarding the lack of treatment for depression. According to the U.S. Surgeon General's report on mental health, ethnic minority children are less likely than white children to receive mental health services (USDHHS, 2001), and this disparity is particularly pronounced for black children and adolescents (Flisher et al., 1997). SAMHSA reported that 9.5% and 9.7% of Black and Hispanic adolescents, respectively, as compared to 12.7% of white adolescents utilized outpatient mental health services in 2008 (SAMHSA, 2009b). Similarly, Kodjo and Auinger (2004) found that emotionally distressed Black adolescents received mental health counseling significantly less than their white or Hispanic counterparts.
1.2 Stigma, mental health service use, and mental disorders
Stigma is one of the main patient level deterrents to mental health service utilization, and may take various forms (e.g., public stigma, self-stigma) (Moses, 2009). Perceived public stigma is defined as the anticipation of negative attitudes and possible prejudice from others based on having a mental disorder or using treatment services (Link, Cullen, Struening, Shrout, & Dohrenwend, 1989; Sirey et al., 2001). Conversely, self-stigma is an individual's negative concept of self, based on their internalization of society's view of their condition (Barney, Griffiths, Jorm, & Christensen, 2006; Corrigan & Watson, 2002).
The stigmatization of people with mental disorders remains a key obstacle to the advancement of prevention, treatment, and illness recovery efforts (Corrigan, 2007; Mann & Himelein, 2004; Pescosolido, Perry, Martin, McLeod, & Jensen, 2007; USDHHS, 1999). Stigma is negatively associated with seeking, using, and complying with treatment for mental health issues (Sirey et al., 2001). Elsewhere, Perry, Pescosolido, Martin, McLeod, and Jensen (2007) found that depressed children and adolescents may be more susceptible to mental illness stigma than adults. Stigmatizing responses and subsequent social distance have also been reported to be strongest towards adolescents (Martin, Pescosolido, Olafsdottir, & McLeod, 2007).
Corrigan (2007) proposed that clinical diagnoses labels and their associated criteria can increase public stigma by prompting stereotypes about, and promoting prejudice and discrimination against, people dealing with mental illnesses. Prior research, on mostly adult populations, reveals that specific types of a disorder or greater levels of a disorder also impact stigma. Dinos, Stevens, Serfaty, Weich, and King (2004) reported that psychiatric outpatients with anxiety, depression, and personality disorders were more impacted by subjective feelings of stigma even without the experience of obvious prejudice. In addition, Yen et al. (2005) reported that Taiwanese outpatients with more severe depression reported greater levels of self-stigma. Furthermore, Raguram, Weiss, Channabasavanna, and Devins (1996) and Pyne et al. (2004) found that higher levels of depressive symptoms and greater depression severity, respectively, were significantly related to greater perceived stigma in psychiatric outpatients.
1.3 The present study
Stigma adversely impacts mental health service utilization and recovery for those suffering from mental disorders (Perlick, 2001). However, scant scientific attention has been given to exploring factors that may contribute to increased stigma, especially among adolescents who may be more susceptible to mental illness stigma. The previous findings regarding depression and stigma in adults, along with the high prevalence rates and low service usage in adolescent populations, particularly among Black adolescents, signify the importance of exploring the relationship within this population. As such, the purpose of this study was to explore the relationship between Black adolescents' perceived stigma and their current level of depression severity in an outpatient sample. We hypothesized that depression severity will be positively associated with greater perceived stigma. Examining this relationship will improve our understanding of factors that underlie the process of mental health service utilization in this population.
2. Method
2.1 Participants
Participants were recruited from a community mental health agency in a metropolitan, Midwestern city. The agency has provided services for low-income and at-risk children and families for over 80 years. Services include an education program for teenage parents, a support program for incarcerated women and their children, a support program for high risk infants, and a family bereavement program for families whose sons or daughters have been killed, and for children who witness violent crimes. Outpatient programs include child, adolescent, and family counseling, an adolescent sexual abusers program, and chemical dependency treatment and services for youth who are both emotionally and mentally impaired. Special outpatient psychiatric services, residential treatment, and case management are also offered. The agency receives formal client referrals from local schools, hospitals, and the juvenile justice system. A sample of 108 adolescents and their caregivers participated in the study. Of the 108 adolescents, 102 identified as African American, two identified as mixed race, two identified as Latino, and two identified as American Indian. Approximately 54% of the sample was female.
2.2 Procedure
During an initial intake and assessment session, agency staff presented an explanation of the study to eligible participants (ages 12-17) and invited adolescent and caregiver dyads to participate. Invitations to participate were presented separately to caregivers and adolescents to reduce any semblance of coercion. Each caregiver provided written consent to allow the adolescent to participate in the research study, while adolescents provided written assent. Study eligible participants who declined invitation to participate in the study were asked to complete a refusal form, which enabled them to indicate a reason for refusal. Information regarding the demographics of the participants who refused to be in the study was not obtained. There is no suggested difference between those who refused and those who consented as the main reasons given for refusal were “not enough time” and “not interested.” Any adolescent who, in the opinion of the professional staff, was unstable or unfit to participate in the study due to their mental or physical status was to be excluded from the study. No one was refused for this reason.
The study protocol was approved by the Institutional Review Board at the University of Michigan and the agency's Board on Evaluation and Quality. Agency staff at the community mental health agency received a detailed training regarding study rationale, goals, data collection, HIPAA compliance, and recruitment procedures. A follow-up training was held eight months post study initiation to provide a review of important study procedures, introduce procedural changes, and address recruitment challenges being faced by agency staff.
2.3 Measures
2.3.1 Depression severity
Depression severity was measured by the 30-item Reynolds Adolescent Depression Scale 2nd edition (RADS-2) (Reynolds, 2002) which was developed to evaluate the severity of depressive symptoms in adolescents, ages 11-20. The RADS-2 was designed for individuals with at least third grade reading ability. Adolescents answered 30 items on a 4-point likert scale that requires a response of whether a symptom-related item occurred: almost never, hardly ever, sometimes, or most of the time. These items are framed in the present tense which requires the adolescent to respond based on how they currently feel. The 30 items provide scores on four factorally derived subscales and a total raw score. The subscales assessed symptoms of (1) Dysphoric Mood (e.g., sadness and crying behavior) (2) Anhedonia/Negative Affect (e.g., disinterest in having fun, and engaging in pleasant activities with other students (3) Negative Self-Evaluation (e.g., negative feelings about oneself such as low self worth, and self-denigration) and (4) Somatic Complaints (e.g., somatic or vegetative complaints such as stomachaches, feeling ill, fatigue, and sleep disturbance). The RADS-2 total raw score provides the clinical severity of depressive symptomatology in adolescents, but does not provide a formal DSM-IV diagnosis for Major Depressive Disorder. Of the 30 items, 7 items are scored in reverse order. These items are phrased in a positive manner so that reversing the scoring key represents greater depression. Adolescents' responses are weighted 1 to 4 points, so that the RADS-2 total raw score ranges from 30-120. Adolescents who scored within the range of 30-75 were considered to be in the normal clinical depression range, 76-81 in the mild clinical depression range, 82-88 in the moderate clinical depression range, and 83-120 in the severe clinically depressed range. For the purpose of the current study, the total raw score was used for analysis and scores were calculated into two categories: normal (30-75) and mild to severe (76-120).
2.3.2 Perceived stigma
Perceived stigma was measured using the 5-item Attitudes toward Psychological Help (ATPH) scale. This scale was adapted from the perceived stigma scale (Pyne et al., 2004), which was modified from the Stigma Scale for Receiving Psychological Help (SSRPH) (Komiya, Good, & Sherrod, 2000), developed to assess individuals' awareness of social stigma associated with receiving psychological services. Validation studies of the SSRPH indicated a reliability coefficient of α= 0.72. The ATPH scale used in this study was adapted to reflect attitudes toward mental health treatment services. For example, the first item in the perceived stigma scale “Receiving treatment for depression carries social stigma,” was changed to “Receiving mental health services is something people look down upon.” Similar to the perceived stigma scale and the Stigma Scale for Receiving Psychological Help, there were 4 Likert-type responses (“strongly disagree”, “disagree”, “agree”, and “strongly agree”) with scores from each item ranging from 0 to 3. The total raw score range was 0 to 15 with higher scores indicating greater perceived stigma. The average raw score for each participant was calculated and categorized into low (0-3), medium (4-6), and high (7-13) stigma for the purpose of bivariate analyses. The scores were further categorized into low (0-3) and high (4-15) stigma for multivariate analysis. The reliability coefficient for the modified scale was determined to be ∝ = .67.
2.3.3 Perceived need for mental health services
Perceived need for mental health services was measured by two questions asking the adolescent to respond to whether they have needed an emotional counselor or a psychiatrist within the last six months. Participants answered either yes (1) or no (0) to both questions. The variable was then recoded into three categories: none, psychiatrist or counselor, and both.
2.4 Analysis
Bivariate analyses were conducted to examine the associations between the clinical, socio-demographic, and stigma variables. Logistic regression analysis was used to measure the effect of depression severity on perceived stigma. Statistical significance was determined at the p < .05 level. All analyses were conducted using PASW Statistics version 18 (formerly SPSS) (SPSS, 2009).
3. Results
3.1 Bivariate analyses
Two separate chi-square analyses were conducted. The first analysis (Table1), examined the associations between depression severity (RADS-2) and all the socio-demographic variables in the study. Results indicate that gender (χ2 = 9.75; p <.01) was significantly associated with depression severity, with females having higher depressive symptom levels than males. Approximately 77% of the adolescents categorized as mild to severely depressed were girls. In contrast, 56% of the adolescents reporting in the normal range for depression were boys.
Table 1. Clinical and socio-demographic characteristics of subjects.
| Depression Severity | |||
|---|---|---|---|
| Normal (n=77) | Mild/Severe (n=31) | pValue | |
| N (%) | N (%) | ||
| Age | |||
| Child (0-12) | 19 (90.48) | 2 (9.52) | |
| Early Adolescence (13-14) | 27 (65.85) | 14 (34.15) | |
| Late Adolescence (15-17) | 29(69.05) | 13 (30.95) | |
| x22 | 2.22; 0.14 | ||
| Gender | |||
| Male | 43 (86.00) | 7 (14.00) | |
| Female | 34 (58.62) | 24 (41.38) | |
| x21 | 9.75; 0.002** | ||
| Grade | |||
| Elementary (1-6) | 10 (100.00) | 0 (0.00) | |
| Intermediate (7-8) | 26 (70.27) | 11 (29.73) | |
| High School (9-12) | 36(66.67) | 18 (33.33) | |
| x22 | 3.12; 0.08 | ||
| Perceived Service Need | |||
| None | 38 (84.44) | 7 (15.56) | |
| Psychiatrist or Counselor | 26 (76.47) | 8 (23.53) | |
| Both | 13 (44.83) | 16 (55.17) | |
| x22 | 12.49; 0.0004*** | ||
p < .05;
p < .01;
p < .001
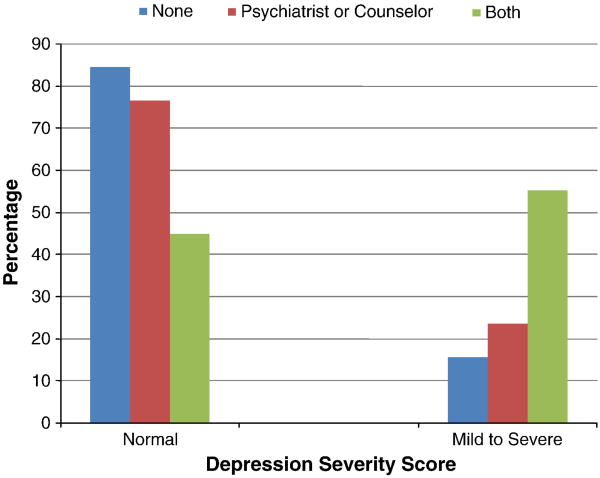
Findings also indicate a statistically significant relationship between perceived service need and depression severity (χ2 = 12.49; p <.001). Approximately 77% of the adolescents who reported mild to severe depressive symptoms perceived a need for treatment from a psychiatrist, counselor, or both. Surprisingly, within the group categorized as normal based on their depression severity scores, approximately 51% of adolescents reported a need for treatment from one or both types of mental health providers (Table 1). Among adolescents indicating no perceived need for treatment, 84% were in the normal range for depression severity, which suggests an appropriate level of self-assessment (Figure 1).
Figure 1. Perceived service need and depression severity.
The second chi-square analysis explored the associations between perceived stigma and depression severity along with the socio-demographic characteristics of the sample. The results indicate a statistically significant association between perceived stigma and depression severity (χ2 = 7.86; p <.01) (Table 2). Approximately 48% of adolescents with mild to severe depressive symptoms, as compared to 29% of those in the normal depressive symptom range, exhibited the greatest level of perceived stigma.
Table 2. Perceived stigma, depression severity, and socio-demographic characteristics.
| Perceived Stigma | |||||
|---|---|---|---|---|---|
| Total | 0-3 Low |
4 to 6 Medium |
7 to 15 High |
pValue | |
| N (%) | N (%) | N (%) | |||
| Age | |||||
| Child (0-12) | 21 | 6 (28.57) | 8 (38.10) | 7 (33.33) | |
| Early Adolescence (13-14) | 41 | 12 (29.27) | 15 (36.59) | 14 (34.15) | |
| Late Adolescence (15-17) | 42 | 13 (30.95) | 14 (33.33) | 15 (35.71) | |
| x22 | 0.0000; 1.00 | ||||
| Gender | |||||
| Male | 50 | 15 (30.00) | 21 (42.00) | 14 (28.00) | |
| Female | 58 | 17 (29.31) | 18 (31.03) | 23 (39.66) | |
| x21 | 0.64; 0.42 | ||||
| Grade | |||||
| Elementary (1-6) | 10 | 3 (30.00) | 5 (50.00) | 2 (20.00) | |
| Intermediate (7-8) | 37 | 10 (27.03) | 12 (32.43) | 15 (40.54) | |
| High School (9-12) | 54 | 18(33.33) | 20 (37.04) | 16 (29.63) | |
| x22 | 0.12; 0.73 | ||||
| Perceived Service Need | |||||
| None | 45 | 16 (35.56) | 12 (26.67) | 17 (37.78) | |
| Psychiatrist or Counselor | 34 | 12 (35.29) | 16 (47.06) | 6 (17.65) | |
| Both | 29 | 4 (13.79) | 11 (37.93) | 14 (48.28) | |
| x22 | 2.06; 0.15 | ||||
| Depression Severity | |||||
| Normal (30-75) | 77 | 29 (37.66) | 26 (33.77) | 22 (28.57) | |
| Mild to Severe (76-120) | 31 | 3 (9.68) | 13 (41.94) | 15 (48.39) | |
| x21 | 7.86; 0.005** | ||||
p < .05;
p < .01;
p < .001
3.2 Multivariate analysis
Logistic regression was conducted to further examine the relationship between depression severity and stigma, in particular, whether depression severity predicted low or high perceived stigma. Findings show that depression severity was significantly related to an increase in perceived stigma (p<.05) (Table 3). Controlling for relevant socio-demographic variables, results indicate that adolescents who were mild to severely depressed were 4.8 times more likely than those in the normal range for depression severity to perceive stigma related to the use of mental health services.
Table 3. Logistic regression of the effect of depression severity on perceived stigma.
| Perceived Stigma | |||
|---|---|---|---|
| ODD Ratio | 95% CI | pValue | |
| Age | |||
| Child (0-12) | 1.00 | ||
| Early Adolescence (13-14) | 0.92 | 0.25 – 3.33 | 0.88 |
| Late Adolescence (15-17) | 0.98 | 0.18 – 5.19 | 0.98 |
| Gender | |||
| Male | 1.00 | ||
| Female | 0.83 | 0.32 – 2.15 | 0.70 |
| Grade | |||
| Elem/Intermed (1-8) | 1.00 | ||
| High School (9-12) | 0.62 | 0.17 – 2.23 | 0.46 |
| Perceived Service Need | |||
| None | 1.00 | ||
| Psychiatrist or Counselor | 0.84 | 0.31 – 2.29 | 0.29 |
| Both | 2.07 | 0.54 – 7.90 | 0.21 |
| RADS-2 Score | |||
| Normal (30-75) | 1.00 | ||
| Mild to Severe (76-120) | 4.80 | 1.17 – 19.69 | 0.03* |
p < .05;
p < .01;
p < .001
4. Discussion
This study examined the relationship between depression severity and perceived stigma regarding mental health treatment. Results support a statistically significant association between depression severity and perceived stigma. Approximately half of the adolescents classified as being mild to severely depressed experienced higher perceived stigma associated with receiving mental health treatment. This is a noteworthy contribution to the mental health service use literature because this phenomenon has been rarely examined among Black adolescents, a population with disproportionately higher vulnerability to depression. Our findings, however, are consistent with prior research on adults (e.g., Pyne et al., 2004), which found that depression severity was a predictor of greater perceived stigma.
The results also indicate that gender and depression severity were significantly associated. More Black female adolescents were mild and severely depressed than their male counterparts. This finding is consistent with much of the literature on gender differences in adolescent depression (e.g., Peterson et al., 1993).
Concomitantly, results revealed a significant association between perceived need for treatment and depression severity, an indication that this sample of Black adolescents was able to aptly identify their need for mental health services. Approximately 77% of adolescents characterized as mild or severely depressed perceived a need for treatment from a psychiatrist, counselor, or both. More surprising, and somewhat unexpected, was that 51% of adolescents characterized as normal, based on their depression severity score, perceived a need for treatment from one or both mental health service providers. It is possible that those adolescents considered below the cut-off for clinical endorsement of depression, according to the RADS-2, have other unmet mental health or psychosocial needs that they believe necessitate formal treatment.
Other research has reported a relationship between perceived need, mental health status, and service use. Wu et al. (1999) found that children with depressive disorders (with or without disruptive disorders) were more likely to report a need for services than those who reported a disruptive disorder only. Additionally, the same study reported that child perceived service need significantly predicted their use of mental health services, school based mental health services, and any service. Correspondingly, in a Dutch adolescent sample, Zwaanswijk and colleagues (2004) reported that only 6.4% of adolescents who perceived an emotional or behavioral problem (425; 10.9% of total sample) were referred for mental health services. The current research supports the need to continue to explore adolescents' perceptions of their own need for mental health services in a Black adolescent population, as perceived need may significantly impact their service utilization.
This study has several limitations. First, the data were collected using cross-sectional survey design methods, limiting any ability to infer causality or directionality. For example, a recent study among Black adolescents found that higher levels of public stigma increased depressive symptoms, but that having higher levels of social support moderated this relationship (Lindsey, Joe, & Nebbitt, in press). Thus, longitudinal research may be required to show causality or determine directionality among these constructs. Second, the small sample size and non-probability sample limits generalizability. Therefore, we are unable to determine whether our findings are consistent with the general population of Black adolescents. Finally, although the findings explicated an association between perceived service need and depression severity, the study did not measure factors that may account for the adolescent's underlying reason for identifying or perceiving that need. This is important to consider as many of the adolescents in the normal range for depression severity identified a need for service.
Though exploratory, this study has important practice and research implications for mental health service delivery targeting Black adolescents. As stigma has been related to seeking, utilizing, and maintaining mental health services (Sirey et al., 2001), Black adolescents in outpatient treatment may benefit from interventions that integrate stigma reduction techniques in order to decrease anticipation of negative treatment by others. Additionally, Black adolescents in both groups (normal and mild to severe) were able to recognize their need for services. From a practice standpoint, referrals to treatment services may need to consider the adolescents own acknowledgment of need along with clinical diagnoses. Furthermore, results from this study could inform the development of services appropriate for adolescents who may not meet the criteria for a clinical diagnosis of depression, but have identified mental health or other psychosocial needs.
The study should be replicated to further examine stigma as a barrier to mental health service use among depressed Black adolescents based on their susceptibility to negative mental health outcomes and their level of unmet need. Future research can explore depression severity and stigma through longitudinal study to further understand the relationship between the variables over time and with larger samples of adolescents. Additionally, studies are needed that examine the role of perceived service need in determining Black adolescents access to and use of mental health services.
Acknowledgments
We appreciate the assistance of Katie Taylor, Ajabeyeng Amin, and Lili Deng from the Research Lab on Race and Self Destructive Behavior on all aspects of the Adolescent Mental Health Service Use Project.
Funding/Support: Dr. Joe's time on this project was supported by a grant (R01-MH82807) from the National Institute of Mental Health. Dr. Lindsey was supported for his time in preparation of this manuscript by the University of Maryland Multidisciplinary Research Career Development Program - MCRDP (NIH K12RR023250; PI: Alan R. Shuldiner). Dr. Lindsey was awarded a personal competitive 5-year K12 scholar career development award as allocated under the institutional MCRDP K12 grant awarded to the University of Maryland. Neither funding source had any role in the writing of this report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Theda Rose, Email: 27rose@cardinalmail.cua.edu.
Sean Joe, Email: sjoe@umich.edu.
Michael Lindsey, Email: mlindsey@ssw.umaryland.edu.
References
- Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Australian and New Zealand Journal of Psychiatry. 2006;40(1):51–54. doi: 10.1080/j.1440-1614.2006.01741.x. [DOI] [PubMed] [Google Scholar]
- Canals J, Domènech-Llaberia E, Fernández-Ballart J, Martí-Henneberg C. Predictors of depression at eighteen. European Child & Adolescent Psychiatry. 2002;11(5):226–233. doi: 10.1007/s00787-002-0286-y. [DOI] [PubMed] [Google Scholar]
- Corrigan PW. How clinical diagnosis might exacerbate the stigma of mental illness. Social Work. 2007;52(1):31–39. doi: 10.1093/sw/52.1.31. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology Science and Practice. 2002;9(1):35–53. [Google Scholar]
- Dinos S, Stevens S, Serfaty M, Weich S, King M. Stigma: The feelings and experiences of 46 people with mental illness: Qualitative study. The British Journal of Psychiatry. 2004;184(2):176–181. doi: 10.1192/bjp.184.2.176. [DOI] [PubMed] [Google Scholar]
- Flisher AJ, Kramer RA, Grosser RC, Alegria M, Bird HR, Bourdon KH, Moore RE, et al. Correlates of unmet need for mental health services by children and adolescents. Psychological Medicine. 1997;27(5):1145–1154. doi: 10.1017/s0033291797005412. [DOI] [PubMed] [Google Scholar]
- Gibbs JT. Mental health issues of black adolescents: Implications for policy and practice. In: Stiffman A, Davis L, editors. Ethnic issues in adolescent mental health. Newbury Park: CA: Sage Publications, Inc; 1990. pp. 21–52. [Google Scholar]
- Hjemdal O, Aune T, Reinfjell T, Stiles TC, Friborg O. Resilience as a predictor of depressive symptoms: A correlational study with young adolescents. Clinical Child Psychology and Psychiatry. 2007;12(1):91–104. doi: 10.1177/1359104507071062. [DOI] [PubMed] [Google Scholar]
- Joe S, Baser RS, Neighbors HW, Caldwell CH, Jackson JS. 12-month and lifetime prevalence of suicide attempts among black adolescents in the national survey of American life. Journal of American Academy of Child & Adolescent Psychiatry. 2009;48(3):271–283. doi: 10.1097/CHI.0b013e318195bccf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodjo CM, Auinger P. Predictors for emotionally distressed adolescents to receive mental health care. Journal of Adolescent Health. 2004;35(5):368–373. doi: 10.1016/j.jadohealth.2003.12.005. [DOI] [PubMed] [Google Scholar]
- Kowalenko N, Wignall A, Rapee R, Simmons J, Whitefield K, Stonehouse R. The ACE program: Working with schools to promote emotional health and prevent depression. Youth Studies Australia. 2002;21(2):23–30. [Google Scholar]
- Komiya N, Good GE, Sherrod ND. Emotional openness as a predictor of college students' attitudes toward seeking psychological help. Journal of Counseling Psychology. 2000;47(1):138–143. [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102(1):133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lindsey MA, Joe S, Nebbitt V. Family matters: The role of mental health stigma and social support on depressive symptoms and subsequent help-seeking among African-American boys. Advance online publication. The Journal of Black Psychology. doi: 10.1177/0095798409355796. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review. 1989;54(3):400–423. [Google Scholar]
- Mann CE, Himelein MJ. Factors associated with stigmatization of persons with mental illness. Psychiatric Services. 2004;55(2):185–187. doi: 10.1176/appi.ps.55.2.185. [DOI] [PubMed] [Google Scholar]
- Martin JK, Pescosolido BA, Olafsdottir S, McLeod JD. The construction of fear: Americans' preferences for social distance from children and adolescents with mental health problems. Journal of Health and Social Behavior. 2007;48(1):50–67. doi: 10.1177/002214650704800104. [DOI] [PubMed] [Google Scholar]
- Merry S, McDowell H, Wild CJ, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based depression prevention program. Journal of American Academy of Child & Adolescent Psychiatry. 2004;43(5):538–547. doi: 10.1097/00004583-200405000-00007. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Rohde P, Seeley JR, Lewinsohn PM. Life events and depression in adolescence: Relationship loss as a prospective risk factor for first onset of major depressive disorder. Journal of Abnormal Psychology. 1999;108(4):606–614. doi: 10.1037//0021-843x.108.4.606. [DOI] [PubMed] [Google Scholar]
- Moses T. Stigma and self-concept among adolescents receiving mental health treatment. American Journal of Orthopsychiatry. 2009;79(2):261–274. doi: 10.1037/a0015696. [DOI] [PubMed] [Google Scholar]
- Myers HF. Urban stress and mental health in black youth: An epidemiologic and conceptual update. In: Jones RL, editor. Black adolescents. Berkeley, CA: Cobb & Henry; 1989. pp. 123–152. [Google Scholar]
- National Advisory Mental Health Council. National plan for research on child and adolescent mental disorders. Rockville, MD: National Institute of Mental Health; 1990. [Google Scholar]
- Perlick DA. Special section on stigma as a barrier to recovery: Introduction. Psychiatric Services. 2001;52(12):1613–1614. doi: 10.1176/appi.ps.52.12.1613. [DOI] [PubMed] [Google Scholar]
- Perry BL, Pescosolido BA, Martin JK, McLeod JD, Jensen PS. Comparison of public attributions, attitudes, and stigma in regard to depression among children and adults. Psychiatric Services. 2007;58(5):632–635. doi: 10.1176/ps.2007.58.5.632. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Perry BL, Martin JK, McLeod JD, Jensen PS. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatric Services. 2007;58(5):613–618. doi: 10.1176/ps.2007.58.5.613. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Compas BE, Brooks-Gunn J, Stemmler M, Ey S, Grant KE. Depression in adolescence. American Psychologist. 1993;48(2):155–168. doi: 10.1037//0003-066x.48.2.155. [DOI] [PubMed] [Google Scholar]
- Pyne JM, Kuc EJ, Schroeder PJ, Fortney JC, Edlund M, Sullivan G. Relationship between perceived stigma and depression severity. The Journal of Nervous and Mental Disease. 2004;192(4):278–283. doi: 10.1097/01.nmd.0000120886.39886.a3. [DOI] [PubMed] [Google Scholar]
- Raguram R, Weiss MG, Channabasavanna SM, Devins GM. Stigma, depression, and somatization in south India. American Journal of Psychiatry. 1996;153(8):1043–1049. doi: 10.1176/ajp.153.8.1043. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Reynolds adolescent depression scale-2nd edition (RADS-2): Professional manual. 2nd. Lutz, FL: Psychological Assessment Resources; 2002. [Google Scholar]
- Roberts RE, Roberts CR, Chen YR. Ethnocultural differences in prevalence of adolescent depression. American Journal of Community Psychology. 1997;25(1):95–110. doi: 10.1023/a:1024649925737. [DOI] [PubMed] [Google Scholar]
- Rosella JD, Albrecht SA. Toward an understanding of the health status of black adolescents: An application of the stress-coping framework. Issues in Comprehensive Pediatric Nursing. 1993;16(4):193–205. doi: 10.3109/01460869309078277. [DOI] [PubMed] [Google Scholar]
- Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Raue P, Friedman SJ, Meyers BS. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. American Journal of Psychiatry. 2001;158(3):479–481. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]
- Statistical Package for the Social Sciences. Predictive analytics software. Chicago: Author; 2009. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH report: Major depressive episode and treatment among adolescents. Rockville, MD: Office of Applied Studies; 2009a. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2008 national survey on drug use and health: National findings (NSDUH Series H-36 No SMA 09-4434) Rockville, MD: Office of Applied Studies; 2009b. [Google Scholar]
- US Department of Health and Human Services. Mental health: A report of the surgeon general. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. Retrieved from http://mentalhealth.samhsa.gov/features/surgeongeneralreport/home.asp. [Google Scholar]
- US Department of Health and Human Services. Mental health: Culture, race, and ethnicity—a supplement to mental health: A report of the surgeon general. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. Retrieved from http://www.surgeongeneral.gov/library/mentalhealth/cre/sma-01-3613.pdf. [PubMed] [Google Scholar]
- Wu P, Hoven CW, Bird HR, Moore RE, Cohen P, Alegria M, Roper MT, et al. Depressive and disruptive disorders and mental health service utilization in children and adolescents. Journal of American Academy of Child & Adolescent Psychiatry. 2004;38(9):1081–1090. doi: 10.1097/00004583-199909000-00010. [DOI] [PubMed] [Google Scholar]
- Yen CF, Chen CC, Lee Y, Tang TC, Yen JY, Ko CH. Self-stigma and its correlates among outpatients with depressive disorders. Psychiatric Services. 2005;56(5):599–601. doi: 10.1176/appi.ps.56.5.599. [DOI] [PubMed] [Google Scholar]
- Zwaanswijk M, Van der Ende J, Verhaak PF, Bensing JM, Verhulst FC. Factors associated with adolescent mental health service need and utilization. Journal of American Academy of Child & Adolescent Psychiatry. 2003;42(6):692–700. doi: 10.1097/01.CHI.0000046862.56865.B7. [DOI] [PubMed] [Google Scholar]