Abstract
Objective
Socioeconomic disparities in pain may be attributable both greater frequency in stressful financial events, as well as greater vulnerability to economic hardship, for those at the lower end of the socioeconomic spectrum. This study investigated the effects of economic hardship and daily financial worry on daily pain among women with a chronic musculoskeletal condition.
Design
The sample consisted of 250 women with osteoarthritis (N=105), Fibromyalgia (N=46), or both (N=99). During an initial assessment, participants’ chronic pain diagnosis, level of economic hardship, and demographic information were ascertained. Over 30 days, daily diary assessments recorded daily financial worries and daily pain severity. Hypotheses were tested using multilevel modeling for repeated measures in SAS PROC MIXED.
Main Outcome Measure
Daily pain severity.
Results
Results indicated that both conditions of economic hardship and daily ratings of financial worry had significant detrimental effects on daily pain. Participants with greater levels of financial stress had greater pain in response to daily financial worries than their counterparts with little or no financial stress. Further, participants in the sample who were not employed and who reported higher levels of financial stress exhibited the most pain reactivity in response to daily financial worries.
Conclusion
Financial stress was associated not only with greater exposure to daily financial worries, but also with greater vulnerability to pain on days when daily financial worries were experienced.
Keywords: economic hardship, chronic pain, socioeconomic disparities, women
Individuals at lower socioeconomic levels have demonstrated greater morbidity and mortality across a broad array of diseases when compared to individuals at higher socioeconomic levels (Adler, Boyce, Chesney, Cohen, Folkman, Kahn, & Syme, 1994; Gallo, Bogart, Vranceanu, & Matthews, 2005; Marmot, 2004), including heart disease, stroke, lung disease, HIV-related disease, tuberculosis, suicide, accidents, and arthritis (Adler & Ostrove, 1999; Marmot, 2004). Investigators have begun to articulate what characterizes the everyday processes and experiences in daily life that would help to explain these social class disparities (Almeida, Neupert, Banks, & Serido 2005; Baum, Garofalo, & Yali, 1999; Gallo & Matthews, 2003; Zautra, Murray, & Parish, 2005).
There is ample evidence that individuals at lower levels of SES experience more stressful life events (Almeida et al., 2005; Baum et al., 1999; Dohrenwend & Dohrenwend, 1970; Gallo & Matthews, 2003; Matthews, Raikkonen, Everson, Flory, Marco, Owens et al., 2000) and live in environments that expose them to more chronic stressors (Gee & Payne-Sturges, 2004) than their higher SES counterparts. In addition to experiencing a greater frequency of chronic environmental stressors, there is evidence that people at lower socioeconomic levels have comparatively fewer psychosocial resources, which results in a decreased ability to manage stressful experiences (Adler et al., 1994; Gallo & Matthews, 2003). Over time, not only increased exposure to stressors, but also increased vulnerability to those stressors, lead to poorer health for those at the lower end of the socioeconomic spectrum (Almeida et al., 2005; Gallo & Matthews, 2005; Grzywacz, Almeida, Neupert, & Ettner, 2004; Matthews et al., 2000).
The stress associated with lower socioeconomic status (SES), compounded by stress associated with chronic pain, renders chronic pain sufferers particularly vulnerable to the adverse effects of stress on health and physical functioning. In fact, some of the greatest socioeconomic inequalities are found for arthritis and related conditions (Callahan, 2003; Dalstra, Kunst, Borrell, Breeze, Cambois, Costa, et al., 2005; Ward, 2001), including increased prevalence, morbidity and mortality among people with arthritis and other musculoskeletal disorders (Callahan, 2003). Among rheumatic disease samples, socioeconomic disparities are documented for the prevalence of rheumatoid arthritis (ERAS Study Group, 2000; Maiden, et al., 1999), chronic generalized musculoskeletal pain and fibromyalgia (Gran, 2003), systemic lupus erythematosus (Ward, 2001) and in disease severity among hip pain sufferers (Eachus, Chan, Pearson, Propper, & Smith, 1999). Among general population samples, lower SES is associated with more frequent reports of musculoskeletal pain (Jablonska, Soares, & Sundin, 2006; Urwin, Symmons, Allison, Brammah, Busby, & Roxby 1998), and pain intensity and physical disability (Brekke, Hjortdahl, & Kvien, 2002). Due to the potential for chronic pain and pain-related disability to influence social standing (Callahan, 2003), and the higher prevalence of arthritis among women (Arber, 1997; Gran, 2003; Jablonska et al., 2006; Katz, 2002), there is a strong need to better understand the influence of SES among women with chronic pain.
Economic hardship is closely linked to measures of SES but has distinct characteristics. Self-ratings of economic hardship involve a subjective appraisal of one’s objective economic resources. There is some evidence that this subjective dimension adds predictive value to the study of health-related outcomes. A measure of subjective SES, developed to assess one’s perceived social standing in relation to others, was compared to a composite of traditional SES indicators – education level, occupational status, and income – and was found to be more predictive of both psychological functioning and health-related outcomes (Adler, Epel, Castellazzo, & Ickovics, 2000; Ostrove, Adler, Kupperman, & Washington, 2000). The present study utilizes a conceptualization of economic hardship that encompasses both objective and subjective experiences related to one’s economic circumstances. Economic hardship, therefore, is a common form of stress (Fox & Chancey, 1998), rooted in objective economic resources, that is understudied in the context of chronic pain. Beyond individual differences in economic hardship, there is a strong rationale to understand the daily processes related to financial worries and pain. Through daily diary methodology (Affleck, Zautra, Tennen, & Armeli, 1999), repeated daily measure over time allow us to model dynamic day-to-day stress processes that contribute to differences in pain due to increased exposure (to economic hardship) and vulnerability (to daily financial worries), which may further our understanding of processes leading to socioeconomic disparities in pain.
A review of the literature pertaining to economic hardship, daily financial worry, and pain revealed that few existing studies have investigated the influence of economic hardship on pain, and none have examined the effects of repeated measures of daily financial worry on pain. Due to the scarcity of existing data, we included relevant studies of constructs similar to economic hardship under different variable names. The review included studies that measured perceived hardship or stress due to economic conditions such as difficulty with personal finances, paying bills, or affording everyday necessities for oneself or one’s family, and that tested their associations with pain, pain-related outcomes, or health-related outcomes.
Economic hardship has demonstrated wide-ranging negative effects on health and adaptation in both chronic pain (Jackson, Iezzi, & Lefreniere, 1997; Soares, Sundin, & Grossi, 2003) and population samples (Conger, Conger, Matthews, & Elder, 1999; Creed, Muller, & Machin, 2001; Fox & Chancey, 1998). More severe functional limitations due to long-term illnesses were associated with financial strain, which was measured as difficulty paying for or managing expenses (Blank & Burstrom, 2002). Those who faced unemployment or low SES were particularly vulnerable to experiencing financial strain (Blank & Burstrom, 2002). Economic pressure, which refers to perceived stress due to difficulty meeting material needs and paying debts, was found to predict self-rated health among single mothers (Wickrama, Lorenz, Conger, Elder, Abraham, & Fang, 2006). Another study found that within families, economic stress was a significant predictor of poor self-rated physical health (Fox & Chancey, 1998). Among pain patients, financial strain (defined as difficulty with living expenses, earning money, and worry about one’s financial situation) was found to be a significant determinant of self-reported disability (Soares et al., 2003). Economic stress has also been linked to psychological distress among groups with and without chronic pain (Jackson et al., 1997; Jackson, Iezzi, Lefreniere, & Narduzze, 1998), and among an unemployed sample (Creed et al., 2000).
Empirical evidence for the influence of economic hardship on pain and pain severity among chronic pain sufferers is relatively sparse; however, one European study examined the effects of financial strain (measured as self-reported difficulty with making ends meet) both in a female community sample and within a subsample of women with prolonged pain (Jablonska et al., 2006). The study found that in the general population, financial strain distinguished between women with self-reported pain and women without pain. Further, among women with chronic pain, financial strain was associated with pain complexity, frequency, intensity, and disability (Jablonska, et al., 2006). In sum, economic hardship, even when broadly defined, is commonly experienced (Fox & Chancey, 1998) and understudied in the context of chronic pain and adaptation.
To our knowledge, the effects of daily financial worries among chronic pain patients have not been previously investigated; however, Skinner and colleagues (2004) used weekly observations (gathered over 12 weeks) to investigate the effects of negative financial events and interpersonal stressors among arthritis patients. Weekly changes in financial and interpersonal stressors were found to contribute to declines in both emotional and physical health among arthritis sufferers (Skinner, Zautra, & Reich, 2004). A growing number of studies have investigated models of stress exposure and vulnerability to explain health disparities using daily diary methodology (Grzywacz et al., 2004; Almeida et al., 2005; Fifield, McQuillan, Armeli, Tennen, Reisne, & Affleck, 2004; Zautra et al., & Parish, 2005) and ecological momentary assessment (Gallo et al., 2005; Matthews et al., 2000). Because day-to-day stress processes are of paramount importance in the experience of pain, and because changes in economic conditions may be particularly relevant in the context of chronic pain, the day-to-day associations between financial worries and pain may reveal important pathways that would further our understanding of socioeconomic disparities in pain.
The current study examined the effects of economic hardship and daily financial worry among women with chronic musculoskeletal pain conditions. We conceptualized economic hardship as a relatively stable measure of perceived hardship due to personal economic conditions, which may develop over time as difficulties accumulate. In contrast, daily financial worry refers to day-to-day worry about finances, and is more likely to fluctuate depending on daily circumstances. We tested pathways involving daily financial worry, economic hardship, and pain to address whether greater exposure to financial worries, and vulnerability due to economic hardship, contribute to greater daily pain. In order to rule out the contribution of individual differences in personality on daily pain ratings, we controlled for several individual characteristics. The personality trait neuroticism is associated with increased vulnerability to stress among arthritis patients (Fifield et al., 2004; Smith & Zautra, 2002) as well as fibromyalgia patients (Charles, Gatz, Pedersen, & Dahlberg, 1999; Netter & Hennig, 1998). Therefore, individual differences in neuroticism, as well as pain diagnosis, age, and working status were statistically controlled.
Hypotheses
Three hypotheses were explored:
On days when financial worries were high, participants would report higher levels of musculoskeletal pain.
Greater economic hardship would be associated with higher average daily pain ratings.
For those participants who reported higher levels of economic hardship, the impact of daily financial worry on daily pain would be greater than for those who reported lower levels of economic hardship.
Method
Participants
The sample consisted of 250 middle aged adult women with a diagnosis of osteoarthritis (OA; N=105), Fibromyalgia (FM; N=46), or both (OA/FM; N=99). Participants were recruited directly from the community through direct mailing to members of the local chapter of the Arthritis Foundation, and through physician’s offices, senior citizen groups, and advertisements posted in local newspapers and neighborhood circulars. Participants included in the study met criteria of having received a diagnosis of OA and/or FM less than five years prior to entry into the study, and confirmation of the diagnosis(es) by a physician. A telephone screening assessment for FM and OA symptoms (White, Speechly, Harth, & Ostbye, 1999) followed by an in-home interview and assessment were used to identify possible co-morbid conditions. Those with co-morbid autoimmune conditions or injury-related chronic pain, and those involved in legal litigation, were excluded from the study. Participants were also required to have a Functional Disability Index score greater than .5 on the Health Assessment Questionnaire (Fries, Spitz, & Young, 1982) and had average pain levels greater than 35 on a 0–100 numeric scale.
After the screening procedure, 263 female participants who returned completed consent forms were enrolled. Data for the 250 participants for whom both diary and initial interview data were available are included in the present study. Participants were between the ages of 37 and 72, (M = 57.3, SD = 8.4). The majority of participants were Caucasian (88.5%). 44.8% of the sample were not working at the time of the initial assessment. Participants reported having had symptoms of FM or OA for an average of 5.2 years (SD = 4.4). Descriptive statistics for socio-demographic variables are listed in Table 1.
Table 1.
Descriptive Statistics of Demographic and Key Study Variables
| N (%) | M (SD) | Skewness | Kurtosis | |
|---|---|---|---|---|
|
Demographic Variable | ||||
| Age | 249 | 57.3 (8.4) | −.26 | −.68 |
| Family Annual Income | 240 | 12.9 (4.2) | −.89 | .00 |
| under $3,000–$18,999 | 50 (20.8%) | |||
| $19,000–$39,999 | 64 (26.7%) | |||
| $40,000–$69,999 | 70 (29.2%) | |||
| $70,000 and over | 56 (23.3%) | |||
| Education | 247 | 5.1 (1.4) | −.24 | −.68 |
| Less than high school | 4 (1.6%) | |||
| Completed high school | 37 (15.0%) | |||
| Vocation or trade school | 35 (14.2%) | |||
| 1–3 years college | 81 (32.8%) | |||
| 4-year college | 31 (12.6%) | |||
| Post-grad college | 59 (23.9%) | |||
|
Key Study Variable | ||||
| Daily Pain | 7256 | 54.1 (23.6) | −.22 | −.68 |
| Daily Financial Worry | 7211 | 1.8 (.9) | .78 | −.43 |
| Economic hardship | 249 | 2.89 (1.81) | .75 | −.69 |
| Neuroticism | 250 | 2.5 (.8) | .36 | .15 |
| Diagnosis | 250 | |||
| Fibromyalgia (FM) | 46 (18.4%) | |||
| Osteoarthritis (OA) | 105 (42.0%) | |||
| Both FM and OA | 99 (39.6%) | |||
| Work Status | 250 | |||
| Not working | 112 (44.8%) | |||
| Working or volunteering | 138 (55.2%) | |||
Procedure
Initial assessment
Upon consent to participate in the study, participants were mailed the initial interview, which included items assessing demographic information, personality, disease activity, and economic hardship. Participants were instructed to complete initial questionnaires on their own. During an in-home visit, trained clinicians reconfirmed diagnoses by tender point examinations. Questionnaires were subsequently collected and reviewed for completeness by staff. Participants were paid $25 upon completion of the initial assessment.
Daily diaries
Participants were trained to complete daily assessments for 30 days using laptop computers. They were instructed to complete the diary before going to sleep each night and were phoned twice in the first week and once each week thereafter to review any problems with the diary completion. The mean number of diaries completed was 28.0 and the modal number was 30. Participants were paid $3 for each diary they completed, totaling up to $90.
Daily Diary Measures
Daily pain
Pain was measured using a 0 to 100-point numerical rating of the average level of pain that day where 0 is “no pain” and 100 is “pain as bad as it can be” (Jensen, Karoly, & Braver, 1986).
Daily financial worry
Participants were asked to rate “Overall, how much have you worried about finances today?” on a 4-point scale from “not at all” to “extremely,” in order to assess perceived stress due to finances. Deviation scores for daily financial worry were calculated by subtracting each individual’s mean score across all days from the individual’s daily score for each variable. The distribution of daily financial worry ratings was somewhat positively skewed, with few daily reports of moderate or extreme worry about finances (1699 days, 23.6%) compared to the number of reports of none or little worry about finances (5497 days, 76.4%).
Individual Measures
Diagnostic group
Diagnosis was assessed using a dichotomous variable that categorized participants as having OA only (dx = 1) or not (dx = 0). The comparison group (dx = 0) contained participants who had FM alone or FM and OA. This way of categorizing participants was reflective of group differences in pain. One-way ANOVAS with Tukey HSD post-hoc tests indicated that the OA group reported significantly lower pain levels than both FM groups, but FM and OA/FM groups were not significantly different from each other in average pain level (mean difference= −2.1, SE=2.8, p=.73). Mean scores on daily pain in each diagnostic category and differences according to diagnosis on other key variables are presented in Table 2.
Table 2.
Means of Key Variables across Diagnostic Groups
| Variable | OA | FM | FM/OA | |
|---|---|---|---|---|
| Individual Mean Daily Pain** | Mean | 46.96a | 58.40 b | 60.62b |
| SD | 17.22 | 15.86 | 13.54 | |
| N | 105 | 46 | 99 | |
| Individual Mean Daily Financial Worry | Mean | 1.78a | 1.87 a | 1.94a |
| SD | .73 | .72 | .74 | |
| N | 105 | 46 | 99 | |
| Neuroticism** | Mean | 2.31ac | 2.63bc | 2.71b |
| SD | .70 | .79 | .77 | |
| N | 103 | 46 | 96 | |
| Age** | Mean | 60.07c | 52.20a | 57.27b |
| SD | 7.74 | 7.76 | 8.37 | |
| N | 103 | 46 | 99 | |
| Economic hardship* | Mean | 2.52a | 2.82ac | 3.23bc |
| SD | 1.75 | 1.82 | 1.83 | |
| N | 105 | 46 | 97 | |
| Income* | Mean | 12.91ab | 14.30 b | 12.23 a |
| SD | 3.85 | 3.69 | 4.63 | |
| N | 102 | 46 | 92 | |
| Education | Mean | 5.14a | 5.44a | 4.91a |
| SD | 1.45 | 1.31 | 1.42 | |
| N | 104 | 45 | 98 |
ANOVA test of group means yielded p<.05.
ANOVA test of group means yielded p<.01.
Notate similarities and differences between group means. Superscripts with the same letter are statistically equivalent.
Economic hardship
Economic hardship was assessed during the initial interview using seven items regarding respondents’ ability to afford basic necessities (Feather, 1989). Responses were measured on a scale ranging from 1= “Definitely not” to 7= “Yes, definitely.” Examples of items included: “Are you able to afford a home suitable for yourself/your family?”, “Do you have enough money for the kind of food you/your family should have?”, “Are you able to afford furniture or household equipment that needs to be replaced?”, and “Do you have enough money for the leisure activities you/your family want?” Construct validity was previously demonstrated through its association with an existing measure of financial strain (r = .69, p<.001; Warr & Jackson, 1985). In the present study economic hardship was significantly related to average individual daily financial worry (r = .49, p<.01), providing further evidence for construct validity. All items were reverse keyed, so that higher scores indicate greater economic hardship. Scale scores were created by computing mean scores across items. In the present study Cronbach’s alpha was .96.
Neuroticism
Neuroticism was assessed in the initial questionnaire using 12 items making up the neuroticism subscale of the Big Five personality inventory (Costa & McCrae, 1992). Participants rated their agreement with items beginning with the root “I see myself as someone who. . . .” on a 5-point scale from 1 = disagree strongly, 3 = neither agree nor disagree, 5 = agree strongly. Items included “I can be moody,” “I can be tense,” and “I get nervous easily.” Four of the 12 items were reverse coded, and mean scores across items were used to create scale scores. Cronbach alpha reliability was .88 in the present study.
Socioeconomic status
Education level was the main SES indicator utilized. Education may be a more stable SES indicator among older adults than income level and is therefore less susceptible to problems of reverse causality (Almeida et al, 2005; Braveman et al., 2005; Grzywacz et al., 2004). Seven ordinal categories coded 1 to 7 were used to represent the highest level of education attained – less than high school, completed high school, completed some college, completed college, and completed some graduate school. Annual family income was measured on an ordinal scale. Participants were asked to choose one of 19 categories representing total family annual income. In our sample, complex SES profiles were expected because participants were in an age range characterized by frequent transition to retirement, and because pain conditions may affect one’s employment status and economic situation.
Work Status
One item assessed whether participants were working, and whether they worked part-time or full-time. This item included both paid and voluntary work. We used a dichotomous variable to represent work status. Those who were working full- or part-time were assigned code 1, and zero was assigned to those who were not working at the time of the initial assessment.
Data Analysis
The data for these analyses are hierarchical, consisting of up to 30 daily observations nested within the 250 participants, a structure best addressed using multilevel modeling (MLM; Affleck, Zautra, Tennen, & Armeli, 1999). MLM procedures may be particularly helpful for the investigation of within-person processes leading to socioeconomic disparities in health outcomes because of its ability to combine the investigation of relations between variables within individuals over time with an investigation of how the relations generalize across individuals or relate to socioeconomic differences between individuals (Affeck et al., 1999).
In the current analyses, Level 1 represented daily measurements of pain and daily financial worry. Daily financial worry ratings were person-centered, in order to partial out between-person differences in ratings. Level 2 measures included economic hardship and several control variables measured at the individual level. – age, neuroticism, diagnostic group, and working status. Each level 2 variable was sample-centered. An autoregressive parameter was included in the analyses in order to remove variance due to the previous day’s score on daily variables. Multilevel models were specified to test hypotheses using SAS PROC MIXED software (Littel, Milliken, Stroup, & Wolfinger, 1996).
Results
Descriptive statistics for demographic and key study variables are displayed in Table 1. All variables were within normal limits on skewness and kurtosis. In preliminary analyses, correlations and one-way ANOVAs among key and demographic variables were computed. The intraclass correlation (ρ = .496) for daily pain (Singer, 1998) indicated that a considerable portion of total variance was accounted for by within-person variance. Economic hardship was correlated with both income (r = −.60, df = 238, p<.001) and, to a lesser extent, education (r = −.15, df = 244, p= .02). The correlation between education and family income was small but statistically significant (r = 0.18, df = 235, p = .005). Differences in correlations suggest that each SES variable and economic hardship captured distinct aspects of social status and material resources.
Mean differences in key variables according to diagnosis and working status were investigated using a series of one-way ANOVAs. Tukey HSD post-hoc comparisons were computed where significant group differences were found. Statistical differences across diagnostic groups are detailed in Table 2. The OA/FM group had the highest mean economic hardship and lowest mean family income and education level. The OA group had the lowest economic hardship and highest level of educational achievement, and the FM group had the highest mean family income. Participants with FM or FM with OA had higher average pain than those with OA only. There were no significant differences in average pain level between working and non-working participants (F(2,247) = 2.3, p=.10). However, those working full-time had higher mean income (F(2,236) = 20.1, p<.001), higher mean educational achievement level (F(2,243) =8.5, p< .001), and lower mean economic hardship (F(2,245) = 4.9, p=.008) than those who were not working.
The results of the preliminary analyses demonstrated important differences on key variables across diagnostic and work status groups. We concluded that these group differences were important to consider, and we examined them in subsequent analyses both as control variables and as interaction terms in exploratory analyses to investigate their moderating effects.
Inferential Analyses
Main effects of economic hardship and daily financial worry on daily pain
First, multilevel equations were specified to compare random intercepts-only with random intercepts-and-slopes models for the main effect of daily financial worry on pain. By comparing these models, fit statistics were used to determine whether the data were best fit to a model where slope representing the relation between daily financial worry and pain were fixed across all participants in the sample, or allowed to differ for each individual. A comparison of fit indices indicated that the best-fit model included random slopes. In addition, a test of the covariance parameter estimate representing random slopes was statistically significant (τ11 = 10.3, SE = 3.7, p= .003), providing further evidence that slopes varied across participants. The main effect of deviation in daily financial worry on pain was significant (β = .94, SE = .44, df = 6564, p= .032). Individual level control variables (neuroticism, age, diagnostic group, working status group) were included in the model. In order to rule out non-linear effects, a quadratic term representing daily financial worry on daily pain was tested but was not statistically significant (β = .18, SE = .37, df = 6939, p = .63).
A second set of multilevel equations were specified in order to test the effect of economic hardship on daily pain. The main effect of economic hardship on daily pain was statistically significant (β = 1.31, SE = .57, df = 234, p=.023), over and above individual differences on control variables.
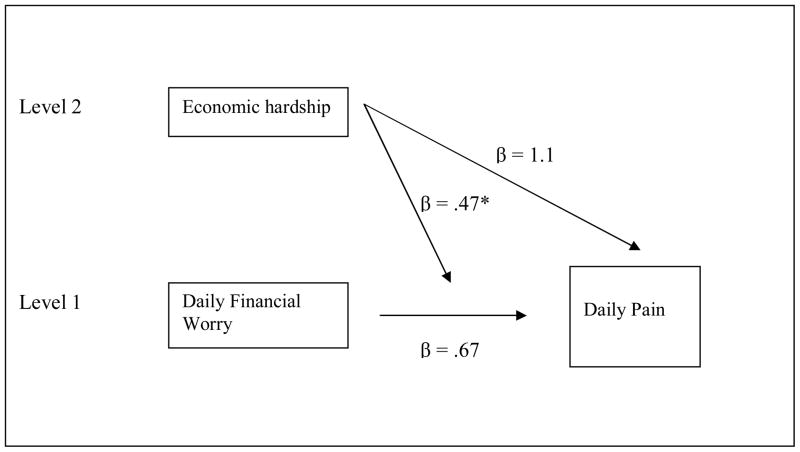
Effects of economic hardship by daily financial worry on pain
Finally, multilevel regression equations were specified to test the hypothesis that individuals with greater economic hardship levels exhibit increased stress reactivity in the face of financial worries than their counterparts with lower economic hardship. The interaction between daily financial worry and economic hardship was significant (β = .47, SE = .23, p = .04). This effect was statistically significant after controlling for the influence of level 2 control variables. Estimates of conditional covariance components indicated significant variation among slopes (τ1,1 = 8.9, SE = 2.5, p < .01) as well as intercepts (τ00 1 = 214.0, SE = 21.4, p < .001). Results of the multilevel regression model are listed in Table 3. Figure 1 graphically depicts the results of hypothesis testing.
Table 3.
Multilevel Regressions Predicting Daily Pain
| Random Effects | |||||
|---|---|---|---|---|---|
| Covariance Parameter Estimates | Subject | β | SEβ | Z | p |
| UN (1,1) | ID | 213.98** | 21.40 | 10.00 | <.0001 |
| UN (2,1) | ID | −7.63 | 7.50 | −1.02 | 0.31 |
| UN (2,2) | ID | 8.95** | 3.59 | 2.49 | 0.01 |
| AR (1) | ID | 0.28** | 0.01 | 21.50 | <.0001 |
| Residual | . | 271.95** | 5.42 | 50.17 | <.0001 |
| Fixed Effects | |||||
| Predictor Variables | β | SE β | df | t | p |
| Level 1 | |||||
| Δ Daily Financial Worry | 0.68 | 0.44 | 6507 | 1.54 | 0.12 |
| Level 2 | |||||
| Economic hardship | 1.31 | 0.57 | 234 | 2.29 | 0.02 |
| Diagnostic Group | 10.68** | 2.14 | 234 | 5.00 | <.0001 |
| Age | −0.06 | 0.13 | 234 | −0.45 | .65 |
| Neuroticism | 1.68 | 1.37 | 234 | 1.23 | .22 |
| Working Status | −3.21 | 2.08 | 234 | −1.54 | .12 |
| Level 1 X Level 2 | |||||
| Δ Daily Financial Worry X Economic hardship | 0.47* | 0.23 | 6507 | 2.02 | 0.04 |
Notes. Diagnostic Group, Age, Neuroticism, and Working Status are control variables. All independent variables are sample-centered, except daily financial worry, which is person-centered. Degrees of freedom reflect listwise deletion of level 2 variables.
UN refers to unstructured model specification.
AR refers to specification of an autoregressive parameter.
p<.01.
p<.05.
Figure 1.
Final multilevel model illustrating the moderation of economic hardship on the effect of daily financial worry on daily pain.
Note. Values are multilevel regression coefficients predicting daily pain. Control variables are not depicted.
*p<.05.
Supplemental Analyses
Because this study pertained to socioeconomic disparities in pain, the authors were interested in comparing economic hardship with SES measures of educational attainment and family income within the context of the present study. Direct effects of SES indicators on daily pain were tested separately in multilevel regression models. Family income was not a significant predictor of daily pain (β = −0.41, SE = .26, df = 238, p = .12), and educational attainment demonstrated a marginally significant relationship with daily pain (β = −1.39, SE = .75, df = 245, p = .07).
In order to test whether our central finding was moderated according to diagnostic group or working status, we entered these categorical variables into three-way interaction terms with economic hardship and daily financial worry, and tested their effects on daily pain. The triple interaction with diagnostic group was not significant (β = −0.50, SE = 0.48, df = 6660, p=.30), suggesting there were no differences in the interaction effect between economic hardship and daily financial worry on pain across diagnostic groups. A triple interaction with working status yielded a significant effect on pain (β = −0.56, SE = .28, df = 6653, p = .048), indicating that the interaction varied across working status groups. In order to further understand these differences, we tested the interaction model in each group. Daily financial worry had a significant effect on daily pain among the non-working group (β = 1.70, SE = 0.64, df = 3071, p=.01), but not among those who were working (β = 0.44, SE = 0.58, df = 3640, p=.45).
To display the effects of working status, we plotted the two-way interaction of daily financial worry and economic hardship in separate plots for each working group. Figure 2 shows the relation between daily financial worry and pain at low (1SD below), mean, and high (1SD above) values of economic hardship (EH in figure). High and low levels of daily financial worry depicted in the figure were designated using values at 1 SD below and 1SD above the mean. The working group plot shows a main effect of economic hardship, however the flat slopes and parallel lines demonstrate that there was no main effect of daily financial worry, and no interaction between economic hardship and daily financial worry on pain in this subgroup. In contrast, the non-working group plot illustrates main effects of economic hardship and daily financial worry, as well as their interaction. Those with high economic hardship experienced the most pain on days with high financial worry, those with a mid-range level of economic hardship experienced more moderate effects of daily financial worry on pain, and those with low economic hardship appeared not to experience any impact of daily financial worry on pain.
Figure 2.
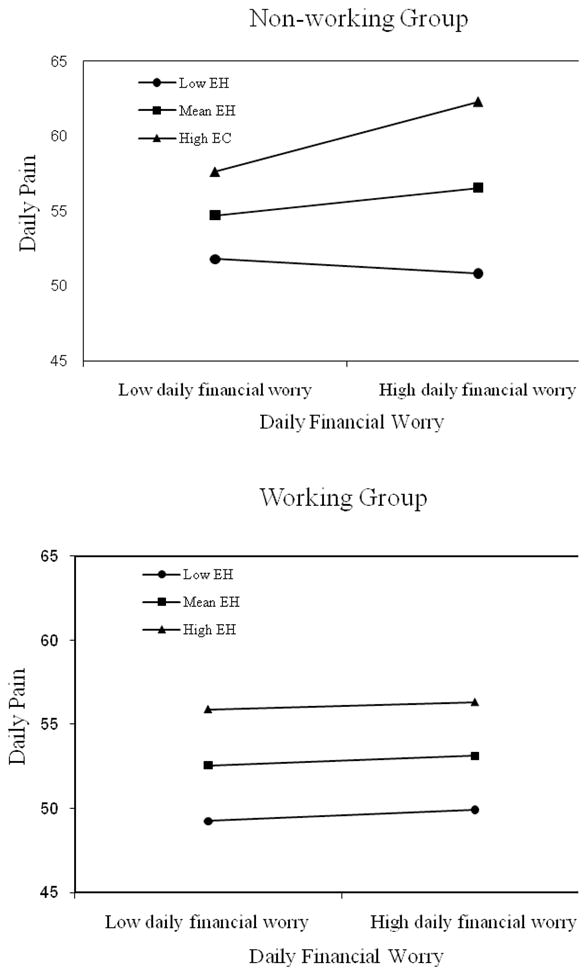
Interaction between daily financial worry and financial stress in working and non-working groups.
Discussion
The major aim of this study was to investigate whether economic hardship and daily financial worry predict musculoskeletal pain among women. Overall, daily financial worry was associated with daily pain, a finding that supported the first hypothesis. The second hypothesis of the study, that economic hardship would moderate the effects of daily financial worry on daily pain, was also supported. Day-to-day financial worry led to significantly more pain among those who rated their financial situations as more stressful. Greater economic hardship appears to render pain sufferers more vulnerable to daily financial worries than those less financially compromised. There was evidence of considerable variation between individuals in pain levels and in the slope of the relation between daily financial worry and pain across individuals.
Prior studies have linked economic hardship to emotional and physical health outcomes such as self-reported disability among pain patients (Soares et al., 2003), increased vulnerability to impairment from long-term illness (Blank & Burstrom, 2002), psychological distress among an unemployed sample (Creed et al., Machin, 2001), and emotional distress in healthy and chronic pain samples (Jackson et al., 1997, Jackson et al., 1998). The present study links economic hardship to daily ratings of pain severity. The findings also support previous research that found weekly levels of financial and interpersonal stress were associated with differences in arthritis pain among people with rheumatoid arthritis (Skinner et al., 2004). In the present study, the effects of economic hardship and daily financial worry were consistent across diagnostic groups who have different types of pain, providing evidence of the generalizability of the findings. The requirement for a physician’s verification of diagnosis also strengthens the validity of our results.
A review of disparities in rheumatic diseases concluded that socioeconomic disparities in the occurrence and outcomes of rheumatic disease have not been adequately studied in the U.S. (Odutola & Ward, 2005). The current study links daily financial worries with daily pain, a finding that may illustrate how a day-to-day process may contribute to health inequalities as they unfold over time. These findings parallel previous work to suggest that an accumulation of stressful conditions over the lifespan leads to health disparities. From a developmental perspective, the effects of childhood as well as adult socioeconomic status can be viewed as trajectories that develop over the life course and influence health in both positive and negative ways (O’Rand & Hamil-Luker, 2005). In the current study, the effects of daily financial worry may present an example of micro trajectories with effects that accumulate over time. Further prospective studies are needed to investigate the processes whereby daily financial worries develop into chronic economic hardship over time.
Consistent with other contemporary measures that emphasize the psychological appraisal component associated with SES (Conger et al., 1999; Ostrove et al., 2000), the current findings further support the utility of a socioeconomic variable that reflects both economic conditions and cognitive appraisal. This link between material and psychological components may provide key insight into understanding paths linking SES to health. Two indicators of SES were compared to economic hardship for their relation to pain – family annual income and educational attainment. Economic hardship proved to be the most robust measure relating socioeconomic standing to pain, though educational attainment also marginally predicted daily pain. Family annual income was significantly correlated with economic hardship, but did not predict daily pain. Family annual income may not have been an adequate indicator of social standing among this aging sample because many participants were likely to be retired. Educational attainment may have proven to be a better SES indicator because it reflects a dimension of social standing that is related to greater resources including health literacy and problem solving skills (Braveman, Cubbin, Egerter, Chideya, Marchi, & Metzler, et al., 2005).
Although the main effect of economic hardship on pain was consistent across the entire sample, the detrimental effects of day-to-day financial worries were limited to those who were not working. Those working part- or full-time were unaffected by those worries. This finding is relevant to literature that addresses the effects of unemployment and financial strain on health. Existing evidence suggests an increased vulnerability to financial strain among the unemployed (Blank & Burstrom, 2002; Creed et al., 2001). Through post-hoc testing of work status differences we were able to offer an interpretation of our results that relates to this literature. However, the number of post-hoc tests may have led to increased threat of Type I error. In addition, the measures utilized in the current study were not able to distinguish whether participants in the non-working group were unemployed, retired, or not working due to disability. Future investigation into these differences would be useful.
Participation in the world of work, even a part-time or volunteer job, was a psychological resource. Those who worked were less vulnerable to the relation between worry about finances and pain. Investigators of work and well-being have hypothesized that the detrimental effects of unemployment or low income may be explained through their effects on personal agency. Strained financial resources restrict personal control over one’s ability to plan and realize the personally satisfying lifestyles necessary to experience and maintain well-being (Marmot, 2004; Marmot, Fuhrer, Ettner, Marks, Bumpass, & Ryff, 1998; Matthews et al., 2000). Perhaps among chronic pain populations, the lack of personal control over life situations posed by financial hardship encompasses a lack of control over one’s pain condition. Further investigation into the mediating influence of personal control in the context of chronic pain is warranted. The role of other psychological variables, such as the role of negative and positive emotions in response to financial conditions (Gallo et al., 2005), may also prove to be a promising future area for inquiry.
The study also has implications for the use of daily process methods in the study of socioeconomic disparities in chronic musculoskeletal pain. There are now a number of studies that have documented socioeconomic inequalities the in the prevalence of musculoskeletal pain conditions (Callahan, 2003; Eachus et al., 1999), in mortality due to musculoskeletal pain (Callahan, 2003), and in longitudinal functional outcomes (Maiden et al., 1999). However, most have used cross-sectional data. This study is the first to investigate pain disparities among Fibromyalgia and osteoarthritis pain sufferers using daily process observations. Although our data are based on self-reports, a necessity in examination of pain severity, the diary design with many repeated measures provided a multi-level data structure. The level 1 (within-person) analyses essentially controlled for stable individual (between-person) differences in pain reports. The current study demonstrated that incorporating daily process variables in the investigation of socioeconomic disparities in pain can contribute important information about pain due to daily stress associated with finances. Daily process methodology may be an essential tool in elucidating the pathways leading to SES disparities in musculoskeletal pain.
Inquiries aimed at assessing different types of financial stressors may add depth to the study of health consequences of daily financial events. Qualitative descriptions of stressful financial events provided by participants in the current study ranged from home and auto repairs, to health expenses, to child expenses, to interpersonal arguments concerning expenses. Analyses of specific types of financial stressors would provide data addressing which kinds of financial stressors are the most common, which are rated as the most stressful, and which are most related to pain outcomes. Investigation of the impact of varied types of financial events could also contribute to a nuanced understanding of the effects of economic hardship by illuminating processes by which the accumulation of negative financial events over time develops into chronic economic hardship. Anecdotally, responses from the current study seemed to indicate that financial stressors often occurred in clusters. A stressor such as being unable to pay a bill on one day was often followed by not being able to pay bills on subsequent days. Further investigation may address the ways in which responses to financial stressors in day-to-day life play out over time and lead to pain and other health outcomes.
In addition to pain, future studies on the effects of economic hardship or day-to-day financial worry on health outcomes such as physical functioning, mental health measures, fatigue, and sleep could yield important new information on the range and boundaries of adverse effects. Further research to identify psychological, social, and physiological mediators of the effects of economic hardship on pain and pain-related outcomes would also lend greater insight into the causal pathways that lead to socioeconomic inequalities in pain and may improve our ability to reduce them. Recent times have enjoyed greater recognition of health disparities as a central contemporary public health and social justice concern. The current economic and employment climate make the potential health consequences of economic stress and hardship even more critical. A thorough understanding of the real impact of chronic economic hardship on pain and other related outcomes could serve an important role to inform new health care policies as they develop.
Acknowledgments
This study was supported by a grant from NIAMS (R01 AR046034). The authors would like to thank Manuel Barrera, Jr., and Morris Okun, for their valuable early feedback on this manuscript.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea
References
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme L. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physical functioning: preliminary data in healthy White women. Health Psychology. 2000;19(6):586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: What we know and what we don’t. Annals of the New York Academy of Sciences. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Affleck G, Zautra AJ, Tennen H, Armeli S. Multilevel daily process designs for consulting and clinical psychology: A preface for the perplexed. Journal of Consulting and Clinical Psychology. 1999;67(5):746–754. doi: 10.1037//0022-006x.67.5.746. [DOI] [PubMed] [Google Scholar]
- Almeida DM, Neupert SD, Banks SR, Serido J. Do daily stress processes account for socioeconomic health disparities? Journals of Gerontology: Series B. 2005;60B(Special Issue II):34–39. doi: 10.1093/geronb/60.special_issue_2.s34. [DOI] [PubMed] [Google Scholar]
- Arber S. Comparing inequalities in women’s and men’s health: Britain in the 1990s. Social Science and Medicine. 1997;44(6):773–787. doi: 10.1016/s0277-9536(96)00185-2. [DOI] [PubMed] [Google Scholar]
- Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress: Does stress account for SES effects on health? Annals of the New York Academy of Sciences. 1999;896:130–143. doi: 10.1111/j.1749-6632.1999.tb08111.x. [DOI] [PubMed] [Google Scholar]
- Blank N, Burstrom B. Limiting long-term illness and the experience of financial strain in Sweden. Scandinavian Journal of Public Health. 2002;30:41–46. [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: One size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Brekke M, Hjortdahl P, Kvien TK. Severity of musculoskeletal pain: relations to socioeconomic inequality. Social Science & Medicine. 2002;54:221–228. doi: 10.1016/s0277-9536(01)00018-1. [DOI] [PubMed] [Google Scholar]
- Callahan LF. Social epidemiology and rheumatic disease. Current Opinion in Rheumatology. 2003;15:110–115. doi: 10.1097/00002281-200303000-00004. [DOI] [PubMed] [Google Scholar]
- Charles ST, Gatz M, Pedersen NL, Dahlberg L. Genetic and behavioral risk factors for self-reported joint pain among a population-based sample of Swedish twins. Health Psychology. 1999;18(6):644–654. doi: 10.1037//0278-6133.18.6.644. [DOI] [PubMed] [Google Scholar]
- Conger RD, Conger KJ. Resilience in Midwestern families: Selected findings from the first decade of a prospective, longitudinal study. Journal of Marriage and Family. 2002;64(2):361–373. [Google Scholar]
- Conger RD, Conger KJ, Matthews LS, Elder GH. Pathways of economic influence on adolescent adjustment. American Journal of Community Psychology. 1999;27(4):519–541. doi: 10.1023/A:1022133228206. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and the NEO Five-Factor Inventory (NEO-FFI): Professional manual. Odessa, FL: Psychological Assessment Resources, Inc; 1992. [Google Scholar]
- Creed PA, Muller J, Machin MA. The role of satisfaction with occupational status, neuroticism, financial strain and categories of experience in predicting mental health in the unemployed. Personality and Individual Differences. 2001;30:435–447. [Google Scholar]
- Dalstra JAA, Kunst AE, Borrell C, Breeze E, Cambois E, Costa G, Geurts JJM, Lahelma E, Van Oyen H, Rasmussen NK, Regidor E, Spadea T, Mackenbach JP. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. International Journal of Epidemiology. 2005;34:316–324. doi: 10.1093/ije/dyh386. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Dohrenwend BS. Class and race as status-related sources of stress. In: Levine S, Scotch NA, editors. Social Stress. Chicago: Aldine; 1970. [Google Scholar]
- Eachus J, Chan P, Pearson N, Propper C, Smith GD. An additional dimension to health inequalities: disease severity and economic position. Journal of Epidemiology and Community Health. 1999;53:603–611. doi: 10.1136/jech.53.10.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ERAS Study Group. Socioeconomic deprivation and rheumatic disease? What lessons for the health service? Annals of Rheumatological Disease. 2000;59:794–799. doi: 10.1136/ard.59.10.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feather NT. Reported changes in behaviour after job loss in a sample of older unemployed men. Australian Journal of Psychology. 1989;41(2):175–185. [Google Scholar]
- Fifield J, McQuillan J, Armeli S, Tennen H, Reisne S, Affleck G. Chronic strain, daily work stress and pain among workers with rheumatoid arthritis: Does job stress make a bad day worse? Work & Stress. 2004;18(4):275–291. [Google Scholar]
- Fox GL, Chancey D. Sources of economic distress: Individual and family outcomes. Journal of Family Issues. 1998;19(6):725–749. [Google Scholar]
- Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the Health Assessment Questionnaire, disability and pain scales. Journal of Rheumatology. 1982;9(5):789–793. [PubMed] [Google Scholar]
- Gallo LC, Bogart LM, Vranceanu A, Matthews KA. Socioeconomic status, resources, psychological experiences, and emotional responses: A test of the Reserve Capacity Model. Journal of Personality and Social Psychology. 2005;88(2):386–399. doi: 10.1037/0022-3514.88.2.386. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129(1):10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gee GC, Payne-Sturges DC. Environmental health disparities: A framework integrating psychosocial and environmental concepts. Environmental Health Perspectives. 2004;112(17):1645–1653. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gran JT. The epidemiology of chronic generalized musculoskeletal pain. Best Practice & Research Clinical Rheumatology. 2003;17(4):547–561. doi: 10.1016/s1521-6942(03)00042-1. [DOI] [PubMed] [Google Scholar]
- Grzywacz JG, Almeida DM, Neupert SD, Ettner S. Socioeconomic status and health: A micro-level analysis of exposure and vulnerability to daily stressors. Journal of Health and Social Behavior. 2004;45:1–16. doi: 10.1177/002214650404500101. [DOI] [PubMed] [Google Scholar]
- Jablonska B, Soares JJF, Sundin O. Pain among women: Associations with socioeconomic and work conditions. European Journal of Pain. 2006;10:435–447. doi: 10.1016/j.ejpain.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Jackon T, Iezzi A, Lefreniere K. The impact of psychosocial features of employment status on emotional distress in chronic pain and health comparison samples. Journal of Behavioral Medicine. 1997;20(3):241–256. doi: 10.1023/a:1025552710949. [DOI] [PubMed] [Google Scholar]
- Jackon T, Iezzi A, Lafreniere K, Narduzzi K. Relations of employment status to emotional distress among chronic pain patients: A path analysis. The Clinical Journal of Pain. 1998;14(1):55–60. doi: 10.1097/00002508-199803000-00008. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- Katz WA. Musculoskeletal pain and its socioeconomic implications. Clinical Rheumatology, Suppl. 2002;1:S2–S4. doi: 10.1007/s100670200028. [DOI] [PubMed] [Google Scholar]
- Little RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for linear mixed models. Cary, NC: SAS Institute; 1996. [Google Scholar]
- Maiden N, Capell HA, Madhok R, Hampson R, Thomson EA. Does social disadvantage contribute to the excess mortality in rheumatoid arthritis patients? Annals of Rheumatological Disease. 1999;58:525–529. doi: 10.1136/ard.58.9.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot MG. The Status Syndrome: How social standing affects our health and longevity. New York: Henry Holt & Co., Inc; 2004. [Google Scholar]
- Marmot MG, Fuhrer R, Ettner SL, Marks NF, Bumpass LL, Ryff CD. Contribution of psychosocial factors to socioeconomic differences in health. The Milbank Quarterly. 1998;76:403–440. doi: 10.1111/1468-0009.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Raikkonen K, Everson SA, Flory JD, Marco CA, Owens JF, Lloyd CE. Do the daily experiences of healthy men and women vary according to occupational prestige and work strain? Psychosomatic Medicine. 2000;62:346–353. doi: 10.1097/00006842-200005000-00008. [DOI] [PubMed] [Google Scholar]
- Netter P, Hennig J. The fibromyalgia syndrome as a manifestation of neuroticism? Z Rheumatol Suppl. 1998;57(Suppl2):105–108. doi: 10.1007/s003930050248. [DOI] [PubMed] [Google Scholar]
- Odutola J, Ward MM. Ethnic and socioeconomic disparities in health among patients with rheumatic disease. Current Opinion in Rheumatology. 2005;17:147–152. doi: 10.1097/01.bor.0000151403.18651.de. [DOI] [PubMed] [Google Scholar]
- O’Rand AM, Hamil-Luker J. Processes of cumulative adversity: childhood disadvantage and increased risk of heart attack across the life course. Journal of Gerontology: Series B. 2005;60B(Special Issue II):117–124. doi: 10.1093/geronb/60.special_issue_2.s117. [DOI] [PubMed] [Google Scholar]
- Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychology. 2000;19:613–618. doi: 10.1037//0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Education and Behavioral Statistics. 1998;24(4):323–355. [Google Scholar]
- Skinner MA, Zautra AJ, Reich JW. Financial stress predictors and the emotional and physical health of chronic pain patients. Cognitive Therapy Research. 2004;28(5):695–713. [Google Scholar]
- Smith BW, Zautra AJ. The role of personality in exposure and reactivity to interpersonal stress in relation to arthritis disease activity and negative affect in women. Health Psychology. 2002;21(1):81–88. [PubMed] [Google Scholar]
- Soares JJF, Sundin O, Grossi G. Age and musculoskeletal pain. International Journal of Behavioral Medicine. 2003;10(2):181–190. doi: 10.1207/s15327558ijbm1002_07. [DOI] [PubMed] [Google Scholar]
- Urwin M, Symmons D, Allison T, Brammah T, Busby H, Roxby M, Simmons A, Williams G. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Annals of Rheumatological Disease. 1998;57:649–655. doi: 10.1136/ard.57.11.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward MM. Examining health disparities in systemic lupus erythematosus. Arthritis & Rheumatism. 2001;44(12):2711–2714. doi: 10.1002/1529-0131(200112)44:12<2711::aid-art457>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Warr PB, Jackson PR. Factors influencing the psychological impact of prolonged unemployment and re-employment. Psychological Medicine. 1985;15:795–807. doi: 10.1017/s003329170000502x. [DOI] [PubMed] [Google Scholar]
- White KPl, Speechly M, Harth M, Ostbye T. Comparing self-reported function and work disability in 100 community cases of fibromyalgia syndrome versus controls in London, Ontario: the London Fibromyalgia Epidemiology Study. Arthritis & Rheumatism. 1999;42(1):76–83. doi: 10.1002/1529-0131(199901)42:1<76::AID-ANR10>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Wickrama KAS, Lorenz FO, Conger RD, Elder GH, Jr, Abraham WT, Fang SA. Changes in family financial circumstances and the physical health of married and recently divorced mothers. Social Science & Medicine. 2006;63(2006):123–136. doi: 10.1016/j.socscimed.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Murray K, Parish B. Adding paths to resilience and daily accounts to an already rich field of inquiry: A brief commentary on James Jackson’s “Social structure and health disparities”. In: Schaie KW, Carstensen L, editors. Social structures, aging and self-regulation. New York: Springer; 2005. [Google Scholar]