Abstract
Objectives
This study examined predictors of treatment expectation among osteoarthritis (OA) patients in a multi-site clinical trial of pain coping strategies training (CST).
Methods
Patients (N=171) completed a pre-treatment assessment battery that asked questions about treatment expectations, pain coping variables, pain, physical function, psychological distress, quality of life, and depression as well as background demographic and medical variables.
Results
Regression analyses indicated that several variables accounted for 21% of the variance in treatment expectations (p < .0001). Patients who were classified as adaptive copers, reported higher self efficacy and social interaction, had higher quality of life, and who had lower levels of affective distress and depression had more positive expectations about engaging in pain coping skills training. Variables that were not associated with treatment expectation were level of pain and physical dysfunction, duration of disease, and disability status as well as demographic variables.
Discussion
Thus, while many OA patients will approach pain coping skills training with positive expectations, others have lower expectations. This study suggests that a multidimensional assessment of OA patients with chronic pain can identify those who have higher expectations versus lower expectations. The results suggest that patients who are psychologically distressed are less optimistic about engaging in treatment and that these patients, in particular, may benefit from and need pre-treatment motivational interviewing to enhance their uptake of pain coping skills
Keywords: pain, osteoarthritis, treatment expectancy, self-efficacy, cognitive behavior therapy
Introduction
The literature describes patients’ attitude about treatment outcome as “expectancies of improvement or expectancies of usefulness/helpfulness” of the treatment.1 2 Whether it is direct clinical care or participating in a clinical trial, patients make choices about what treatment they engage in. Thus, when starting treatment, most patients are likely to have some degree of expectation. Treatment expectation is especially important for psychosocial interventions that are based on cognitive behavioral therapy (CBT) principles compared with more passive interventions like medication. CBT interventions, such as pain coping skills training (CST), require active patient engagement and patient practice of learned coping skills between sessions.
Clinical observations and research studies suggest that patients vary in their expectation for CBT-based interventions. Some patients report high expectation, whereas others report very low expectation.3 There is growing agreement that we need to learn more about the factors that explain these variations in expectation, since they have an influence on patient involvement with treatment and drop-out.4
Despite the recognized importance of the construct, surprisingly few studies have examined predictors of treatment expectation in the context of CBT-based interventions for chronic pain. Goossens et al. pooled the data from two studies of 121 fibromyalgia patients and lower back pain patients and examined how a number of pain and psychological variables collected prior to treatment related to treatment expectation.3 At baseline, patients with higher treatment expectation for CBT-based interventions were more likely to report better pain control, using positive reinterpretation of pain strategies to cope with pain, less fear of movement, and were less likely to be receiving disability payments for the pain disorder. Of equal interest are patient characteristics that were not significantly associated with treatment expectation: pain duration, catastrophizing, and depression. A second trial of 223 low back pain patients entering a randomized trial of physical exercise and/or CBT found that less pain-related fear and more internal control of pain was associated with higher treatment expectations.5 Each of these studies explained 10–12% of treatment expectation. Taken together, these findings suggest that patients who believed they could control their pain, used positive coping strategies, who were less fearful of pain (suggesting a more adaptive approach to pain), and were not receiving disability had higher expectation for CBT-based pain management interventions.
Identifying characteristics that predict osteoarthritis (OA) patients’ expectation for CBT-based interventions such as CST is important for several reasons. First, by understanding which patients are likely to have higher expectation for CBT-based interventions, we may be able to identify those patients who are most amenable to referral for treatment. Second, improving our ability to pinpoint patients with lower expectation may better enable us to engage a larger percentage of them in treatment by increasing their motivation through motivational interviewing efforts.6 This approach, for example, has been used successfully to increase the number of chronic pain patients who participate in a CBT-based pain management program.7
The purpose of this study was to examine how baseline psychosocial, demographic, and medical variables were concurrently related to treatment expectation in OA patients participating in a multi-site clinical trial of pain coping skills training. To our knowledge this is the first study to address this specifically in OA. Since there was very limited research to guide hypotheses, the study was designed as exploratory research with a set of 35 relevant variables and demographic characteristics. Related literature provided the basis for hypotheses for several variables. Overall, we hypothesized that patients with more positive baseline coping would have higher treatment expectation. Specifically, patients with a classification as “Adaptive” on the Multidimensional Pain Inventory (MPI), higher Pain Coping Attempts and Pain Control scores on the Coping Skills Questionnaire (CSQ), and higher self-efficacy would report higher treatment expectation for pain coping skills training. We hypothesized that pain catastrophizing (as assessed by the catastrophizing scale of the CSQ), depression (Beck Depression Inventory), and pain severity ratings would not be related to treatment expectation. We made no a priori hypothesis regarding differences in treatment expectation based on patients’ physical functioning, social functioning, and demographic characteristics.
Materials and Methods
Procedure
The data were from baseline assessments of an on-going randomized controlled clinical trial examining the effectiveness of nurse-delivered pain coping skills training (CST) for patients with persistent knee and/or hip pain due to osteoarthritis (10 individual sessions). Recruitment was conducted at three community clinical sites, one located in the New York area, one in Virginia, and one in North Carolina. The study protocol was approved by the relevant Institutional Review Boards for each site. Flyers and informational brochures were displayed in the exam and waiting rooms of the clinics advertising the study. In addition, clinic physicians and staff referred patients. The research team telephoned interested patients and provided them with a description of the study and the CST treatment. During the phone contact, patients were also screened for eligibility for the trial. Eligibility criteria were (1) being a patient at one of the designated recruitment clinics, (2) age 21 years and older, (3) physician-confirmed diagnosis of osteoarthritis of the hip or knee, (3) usual pain ≥ 4 (on a 10 point scale) for a duration of ≥ 6 months to qualify as “chronic pain”, (4) the ability to read, write, and understand English, (5) the ability to attend 10 treatment sessions within 20 consecutive weeks if randomized to treatment, (6) access to a telephone to complete daily automated telephone ratings and occasional phone sessions with the nurse, and (7) no hip or knee joint replacement surgery scheduled in the next 18 months or during the last 12 months.
Eligible patients were seen at their clinic by a research assistant for the baseline assessment. As part of the consent process, patients again were provided with a description of the CST intervention. Patients then completed a pre-treatment assessment battery that asked questions about treatment expectation, pain coping variables, pain, physical function, psychological distress, quality of life, and depression as well as background demographic and medical variables.
Measures
Treatment Expectation
A five-item treatment credibility/expectation questionnaire was modified for this study based on the Credibility/Expectation Questionnaire (Devilly & Borkovec, 2000). This scale uses items with face validity, and has also demonstrated construct validity and relationships with clinical outcomes.2 This type of measure has been used in clinical trials since the early 1970’s as a means for comparing patients’ baseline view of treatment.8 On a 10-point scale, patients were asked to rate whether CST seems logical, if they feel confident about the training, whether the training will help to control their pain, if they expect the nurse delivering the training to be helpful, and if they would recommend this training to others. The psychometric characteristics of this scale are reported for this study.
Pain Coping Measures
The Multidimensional Pain Inventory (MPI) is a 61-item instrument that evaluates the impact of and adaptation to chronic pain. It is comprised of 13 subscales that measure pain intensity, interference of pain with everyday activities, perceived life control, affective distress, and social support.9 Several studies report adequate to high internal consistency (Cronbach alpha 0.61–0.92).10–12 In the present sample, Cronbach alphas for the subscales ranged from .71 to .92. The computer scoring system (MAP)13 uses 9 of the 13 scales to classify each patient into one of three main adaptational styles: Adaptive (AC) patients with low pain impact and high levels of functional activity; Dysfunctional (DYS) patients with high pain impact, affective distress, and severe functional limitations; and Interpersonally Distressed (ID) patients with poor social support from their significant others in response to pain.14 The program uses multivariate classification procedures and a goodness-of-fit approach to determine if an individual’s MPI scale scores are sufficiently similar to any of the three prototypic profiles. For the present analyses we compared patients with an adaptive coping style (AC) to patients classified as having a maladaptive coping style (DYS and ID).
The Coping Strategies Questionnaire (CSQ) was used to measure patients’ pain coping strategies. This instrument has demonstrated sensitivity to change in several types of chronic pain patients and good construct validity. Test-retest reliabilities and internal consistency for the different subscales have been reported to range between r=.60 and r=.93 for the former and r=.74 to r=.89 for the latter.15, 16
Scores on the Coping Attempts factor of the CSQ were calculated by averaging the scores on six subscales that load on this factor: coping self-statements, praying or hoping, ignoring pain sensations, reinterpreting pain sensations, increasing behavioral activities, and diverting attention.17 In addition, we examined scores on the catastrophizing subscale and a rating of the overall effectiveness of coping strategies in decreasing and controlling pain. Cronbach alphas for the subscales ranged from .74 to .87 in this sample.
The Arthritis Self-Efficacy Scale (ASES) was used to measure patients’ perceived ability to perform specific behaviors aimed at controlling arthritis pain and disability.18 We used the 8-item version of the original 20-item instrument. The scale meets standards for validity and reliability estimates.19, 20 Cronbach alpha was .90 in the present sample.
Measures of Pain, Physical Function, Psychological Distress, and Quality of Life
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) is the most widely used outcome measure in hip and knee arthritis pharmaceutical and surgical studies.21 It includes 24 items covering: pain, stiffness, and physical function. Internal consistency and test-retest reliability for the subscales have been established previously.22, 23 In this sample, Cronbach alphas were .79 (pain), .69 (stiffness), and .95 (physical function).
The Arthritis Impact Measurement Scale (AIMS2) a 78-item questionnaire, specifically assesses the health status of patients with arthritis and has been used extensively in survey and treatment outcomes research.24 The AIMS2 consists of 12 subscales that capture 5 health status components: pain, physical functioning, affective functioning, social functioning, and role functioning. Reliability and validity of the measure have been demonstrated.25–27 Cronbach alphas for the subscales ranged from .71 to .90 in this sample.
The Quality of Life Scale (QOL) is a 16-item instrument designed to measure quality of life across a broad array of life domains in patients with chronic illness. 28 It has been shown that the instrument is conceptually clear, reliable (with a 6-week test-retest reliability of .76) and content-valid among medical patients. The measure showed good internal consistency (Chronbach alpha of .91) in this sample.
Depression Measure
The Beck Depression Inventory (BDI) was used to measure depressed mood.29 Alpha coefficients for the BDI in psychiatric and non-psychiatric populations range from .73 to .95.30 This 21-item instrument is widely used as a treatment outcome measure and is sensitive to the range of depressed mood in chronic pain patients.31 In a recent review of evidence-based assessment of depression, the BDI was judged to be the premier instrument for tracking changes in depressed mood in outpatient settings.32 Internal consistency was adequate (Chronbach alpha of .88) in this sample.
Analytic strategy
Frequency distributions, means, and standard deviations were examined for each of the treatment expectation items. Principal component analysis was then performed to examine the factorial structure of the items. Relationships between treatment expectation scale scores and patient characteristics were then examined with Pearson correlations (for continuous characteristics) and Spearman correlations (for rank-ordered characteristics). Finally, multiple regression analysis with forced entry was used to identify unique predictors of treatment expectation: the set of patient characteristics showing a significant zero-order association with treatment expectation was entered in the multiple regression. To correct for the large number of analyses conducted, the significance level was set at p < .005.
Results
Sample
A total of 393 patients were screened for eligibility to participate in the clinical trial. Of those, 160 patients (41%) did not meet the inclusion criteria. The most common reasons for ineligibility were average pain <4 (n = 50, 31%) and no diagnosis of hip/knee OA (n = 37, 23%). Patients could have multiple reasons for ineligibility. Sixty-one patients (16%) were eligible but declined to participate in the trial. Common reasons for not wanting to participate were too much time commitment (e.g. engage in the 10 sessions, length of the study, etc.) and lack of interest in the CST training. The remaining 171 patients (44%) enrolled in the clinical trial, completed the baseline questionnaire battery and were available for these analyses.
Patients had a mean age of 66 years (range 36 – 88, SD = 9.5), and were predominantly female (75%), married (60%), and White (86%). Most were high school graduates (94%), and 38% graduated college. The average self-reported duration of osteoarthritis was 13 years (range 1 – 55, SD = 9.9). One-sixth (16%) of the patients were receiving full time (14%) or part time (2%) disability; the average self-reported duration of disability was 10 years (range 1 – 26, SD = 7.3). Twenty-seven percent of the patients scored in the mild to severe range of depression on the BDI29 (see Table 1).
Table 1.
Demographic and illness characteristics of the sample (N = 150 – 171)
| Age (Mean, SD) | 66.3 (9.5) |
| Female | 75% |
| Race (White) | 86% |
| Married | 60% |
| Education | |
| Did not finish high school | 6% |
| High school graduate | 25% |
| Some college | 31% |
| College graduate or more | 38% |
| Employed | 30% |
| Disability benefits | 16% |
| Duration of osteoarthritis in years (Mean, SD) | 13.1 (9.9) |
| BDI Depression | |
| Minimal (0–13) | 73% |
| Mild (14–19) | 15% |
| Moderate (20–28) | 11% |
| Severe (29–63) | 1% |
Descriptive characteristics of treatment expectation scores
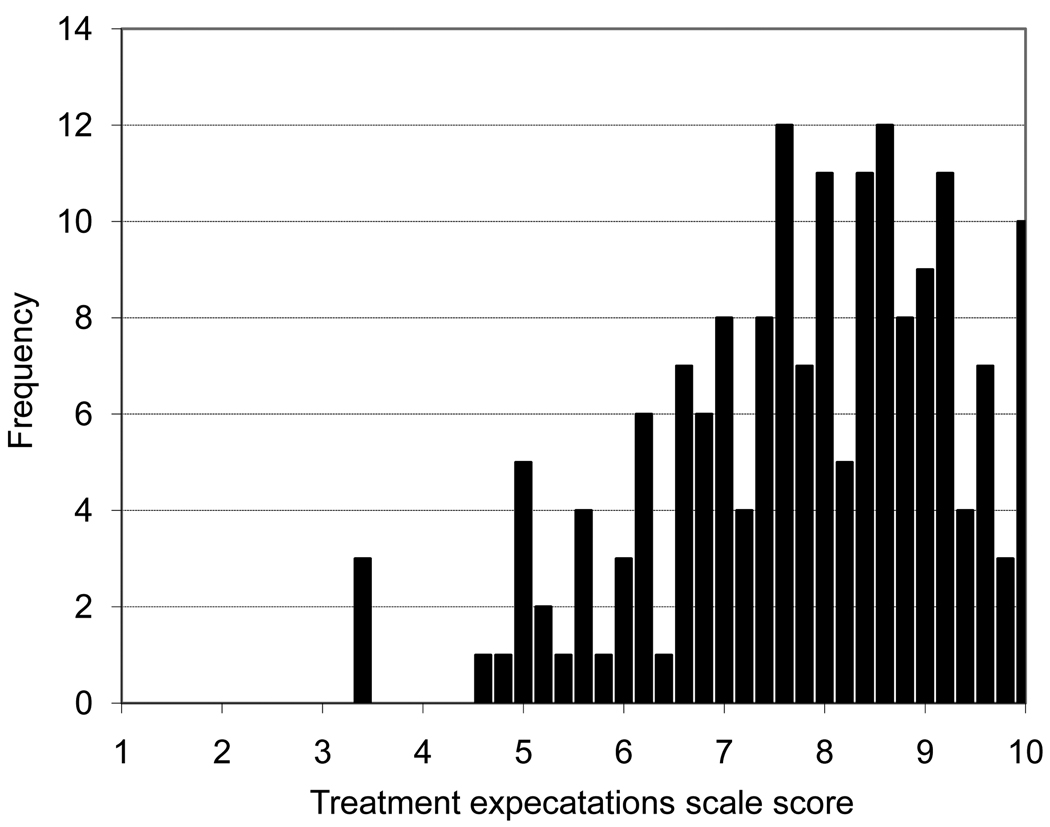
Descriptive statistics for the treatment expectation items are shown in Table 2. For each of the five items, the average response was above the scale midpoint of 5.5 on the 10-point scale (item means ranging from 7.11 to 8.39), suggesting that patients entering the trial generally held relatively favorable expectation about CST treatment. However, item response distributions showed considerable variability (i.e., standard deviations exceeding 1.5 scale points in all instances), and covered almost the full possible range of responses for all items. Principal components analysis suggested a single factor underlying the responses to the five items: only the first factor had an Eigen value greater than one (Eigen value = 3.27), explaining 65% of the variance of the responses. All items loaded substantially (≥ .73) on this factor. Thus, an overall treatment expectation scale score was created by averaging responses to the five items; this scale score demonstrated adequate internal consistency (Cronbach alpha = .87). The frequency distribution of the treatment expectation scale scores is shown in Figure 1.
Table 2.
Descriptive statistics of treatment expectation items and scale scores (N = 171)
| M | SD | Range | rit | |
|---|---|---|---|---|
| How logical does this treatment seem to you? | 8.22 | 1.78 | 2–10 | .59 |
| How confident are you that this treatment will help you manage your osteoarthritis? | 7.29 | 1.83 | 2–10 | .79 |
| How successful do you think the treatment will be in helping you to control and decrease your osteoarthritis pain? | 7.11 | 1.85 | 2–10 | .76 |
| How helpful do you think the nurse will be? | 8.39 | 1.62 | 2–10 | .66 |
| How confident would you be in recommending this treatment to a friend who has arthritis? | 8.18 | 1.83 | 1–10 | .65 |
| Overall scale scores | 7.84 | 1.44 | 3.4–10 |
Note: rit = item-total correlation. Overall scale scores were created by averaging the responses to the five items.
Figure 1.
Frequency distribution of treatment expectation scale scores.
Correlations between patient characteristics at baseline and treatment expectation
Correlations between the treatment expectation scale score and measures of pain, coping with pain, physical function, affective distress, quality of life, and depression are shown in Table 3. Also shown are correlations between treatment expectation and demographic and medical variables. As can be seen, while the associations were generally low to moderate in magnitude, several statistically significant relationships emerged.
Table 3.
Correlations of treatment expectation with patient characteristics
| R | p | n | |
|---|---|---|---|
| MPI – Adaptive coping style (vs. dysfunctional/interpersonally distressed) a | .29 | .0006 | 137 |
| Self-efficacy | .33 | <.0001 | 170 |
| CSQ - coping attempts | .21 | .0048 | 171 |
| diverting attention | .15 | .056 | 171 |
| reinterpreting pain | .11 | .14 | 171 |
| coping self statements | .11 | .16 | 171 |
| ignoring sensations | .04 | .62 | 171 |
| praying/hoping | .30 | .0001 | 171 |
| behavioral activities | .21 | .006 | 171 |
| CSQ - catastrophizing | −.12 | .11 | 171 |
| CSQ – pain control | .07 | .36 | 169 |
| BDI – total score | −.25 | .0008 | 171 |
| cognitive-affective sub-score | −.29 | .0001 | 171 |
| somatic sub-score | −.10 | .18 | 171 |
| Quality of life | .35 | <.0001 | 170 |
| WOMAC – global | .03 | .74 | 171 |
| pain | .06 | .42 | 171 |
| stiffness | .06 | .41 | 170 |
| physical | .01 | .93 | 171 |
| AIMS2 – physical component | −.08 | .33 | 170 |
| mobility | −.01 | .91 | 170 |
| walking & bending | −.11 | .16 | 170 |
| hand & finger | −.04 | .59 | 171 |
| arm function | −.11 | .16 | 171 |
| self-care | −.03 | .67 | 171 |
| household tasks | −.02 | .77 | 171 |
| AIMS2 – affect component | −.27 | .0005 | 168 |
| tension | −.20 | .009 | 168 |
| mood | −.30 | .0001 | 169 |
| AIMS2 - social interaction component | −.30 | .0001 | 169 |
| social activity | −.28 | .0002 | 169 |
| support from family | −.22 | .004 | 169 |
| AIMS2 - arthritis pain | −.09 | .23 | 171 |
| AIMS2 – work b | −.19 | .10 | 73 |
| AIMS2 - satisfaction | −.15 | .046 | 170 |
| AIMS2 - health perception | −.08 | .33 | 170 |
| AIMS2 - arthritis impact | −.12 | .11 | 170 |
| Age | .07 | .35 | 169 |
| Gender (female) | .14 | .09 | 150 |
| Race (white) | −.03 | .66 | 171 |
| Married | .10 | .20 | 164 |
| Education c | −.004 | .96 | 170 |
| Employed | .05 | .52 | 167 |
| Disability | .04 | .62 | 168 |
| Duration of osteoarthritis | .09 | .23 | 165 |
Note:
Excludes patients classified as “anomalous” or “hybrid” on the MPI;
excludes unemployed, disabled, and retired patients;
Spearman rank-order correlation. Results for subscales are in italics.
Relationships of pain coping variables with treatment expectation
As hypothesized, at baseline patients reporting a more adaptive coping style on the MPI had higher treatment expectation than those with a dysfunctional or interpersonally distressed coping style (p < .001). Second, patients with higher levels of self-efficacy were more likely to report higher treatment expectation (p < .0001), and patients who reported more frequent coping attempts (CSQ) also reported higher treatment expectation (p < .005). However, examination of the individual CSQ subscales making up the coping attempts factor revealed that this relationship met the study significance threshold for only the praying/hoping subscale (p = .0001).
Relationship of pain and physical function to treatment expectation
Consistent with our hypotheses, baseline pain and physical function variables (as assessed by the WOMAC and AIMS) were not significantly related to treatment expectation (ps ≥ .16).
Relationship of depression, affective distress, social function, and quality of life to treatment expectation
Contrary to our hypothesis, depression was related to treatment expectation, in that higher BDI total depression scores were associated with lower treatment expectation (p < .001). Consistent with this was the significant relationship observed for the affective distress component of the AIMS2 (p < .001). Specifically, patients scoring higher on mood disturbance (p < .0001) on the AIMS2 reported lower treatment expectation, whereas the association was only marginally significant for the tension subscale (p = .009) of the AIMS2. The AIMS2 social interaction component was also significantly associated with treatment expectation (p = .0001): patients reporting lower levels of social activity (p < .001) and less social support (p = .004) reported lower treatment expectation. Finally, patients with lower quality of life reported lower treatment expectation (p < .0001).
Relationship of demographic and medical variables with treatment expectation
No significant relationships were observed between treatment expectation and demographic or medical variables (i.e. age, gender, race, marital status, education, employment, disability, and illness duration (ps ≥ .09)).
Multiple regression predicting treatment expectation from patient characteristics
Variables that showed a significant zero-order association (p < .005) with treatment expectation were subsequently entered in a multiple regression analysis predicting treatment expectation. As shown in Table 4, most predictor variables were significantly intercorrelated, but the magnitude of these correlations was generally moderate. Variance inflation factors (VIFs) were within an acceptable range (VIFs < 2.5), suggesting no serious problem of multicollinearity. In combination, the predictor variables explained 21% of the variance in treatment expectation (p < .0001); however, none of the variables emerged as a unique predictor in the multiple regression (all ps > .05) (see Table 4).
Table 4.
Results of multiple regression analysis
| Multiple regression predicting treatment expectation |
Correlations among predictor variables | |||||||
|---|---|---|---|---|---|---|---|---|
| R2 = .21 | MPI | CSQ | BDI | QOL | ASES | AIMS2 affect | ||
| Std. beta | rpart | |||||||
| MPI adaptive style | .11 | .10 | ||||||
| CSQ coping attempts | .14 | .13 | .17 | |||||
| BDI depression | .02 | .01 | −.42* | −.07 | ||||
| QOL quality of life | .18 | .15 | .28* | .10 | −.54* | |||
| ASES self-efficacy | .15 | .12 | .34* | .14 | −.48* | .53* | ||
| AIMS2 affect | −.01 | .00 | −.40* | −.12 | .74* | −.47* | −.46* | |
| AIMS2 social | −.12 | −.10 | −.37* | −.19 | .39* | −.40* | −.33* | .49* |
Note:
p < .005.
rpart = semipartial correlation. MPI = Adaptive coping style (vs. dysfunctional/interpersonally distressed
Discussion
To our knowledge, this is the first study to specifically examine how OA patient characteristics relate to treatment expectation for 10-session pain coping skills training (CST), an empirically-validated CBT-based treatment for OA pain.33 One of the most interesting findings of this study was the substantial variation in treatment expectation among the OA patients participating in this clinical trial where scale scores ranged from 3.4 to 10 on the 10-point scale. Thus, although all of the patients volunteered for the clinical trial, some patients clearly had high expectation for this treatment, whereas others had lower expectation. One implication of this finding is that clinicians and researchers should not assume that OA patients are a homogeneous group with regard to their treatment expectation for CBT-based pain management and should be aware that patients may differ substantially in expectations when entering treatment.
This study found that pre-treatment levels of pain coping variables were meaningfully related to variations in patients' treatment expectation. OA patients who were classified on the MPI as adaptive copers were more likely to report higher treatment expectation for CST. In prior studies, adaptive copers have been described as better able to accept and live with persistent pain and as having lower levels of pain and pain-related disability.34 Self-efficacy was also significantly correlated with treatment expectations. Specifically, patients who reported higher confidence in their ability to manage arthritis pain and symptoms had higher treatment expectations. Thus, it is likely that CST is a treatment that is compatible with such patients’ positive view of disease management through self-management and active coping. Patients with a greater focus on surgical, pharmaceutical, or passive medical treatments (e.g. physical therapy sessions focusing on moist heat or ultrasound treatments) may not approach CST with as much enthusiasm.
This study also found that OA patients who reported higher affective distress and depression were more likely to have lower expectations regarding CST. This is interesting for several reasons. First, it suggests that OA patients who are psychologically distressed may have more difficulty engaging in CST treatment. These patients, in particular, may need and benefit from motivational interviewing to enhance their interest in learning pain coping skills. Second, given that a major target of CST involves reducing pain-related psychological distress, these patients - if they can become fully involved in treatment - may benefit substantially. These results suggest that health providers and researchers working with OA patients who are psychologically distressed should be aware that these patients may have lower expectation for CBT-based treatments and take this into account in treatment planning. Finally, it was interesting to see that the CSQ subscale, catastrophizing, which is typically correlated with pain-specific emotional distress, was not associated with expectations. Patients who respond to pain by catastrophizing often report difficulty making use of cognitive and behavioral coping strategies on their own.35 Because of this, these patients are particularly likely to need and potentially benefit from systematic training in pain coping skills.36
The AIMS2 social interaction measure was also found to relate to treatment expectation. Patients with lower levels of social interactions were more likely to have low expectation regarding CST. The social interaction variable shows correlations in expected directions with measures indicating more psychological distress, less self-efficacy and less quality of life. Thus, these results are consistent with the overall picture of the patient with lower treatment expectations as being more psychologically distressed and interpersonally isolated. Patients, who have positive interpersonal interactions and are more socially involved, may also feel more optimistic about establishing a one-on-one relationship with the nurse practitioner delivering the CST training.
Notably, this study did not find that demographics, medical variables or measures of pain or physical function were related to OA patients’ expectation about CST within the participating sample. This is encouraging, since it is often assumed that patients with certain demographic characteristics (e.g. older patients, male patients), very high levels of pain, or those who are very physically disabled by arthritis pain will have low interest in treatments based on self-management approaches such as CST. However, it is certainly possible that some of these characteristics could be related to patients’ decision to decline the invitation to participate in the trial.
Of the psychosocial variables that were found to be significantly related to treatment expectation, which one is most important? We conducted a multivariate regression analysis to address this question. This analysis showed that the set of psychosocial variables we identified as significantly related to treatment expectation in the correlational analyses (i.e. measures of pain coping, affect, depression and quality of life) explained a significant proportion of the variance (21%) in treatment expectation. Interestingly, none of the individual variables in this set emerged as a unique correlate of treatment expectation. Thus, patients’ expectations of the helpfulness of CST for OA pain appear to be related to a combination of variables, and may not be accurately assessed by focusing on any one of these variables.
One concern that arises in this regression approach is potential multicollinearity (i.e., the predictor variables might be highly intercorrelated) and confounding effects may be operating. As can be seen in Table 4, a number of the correlations among the predictor variables are in the .30s to .50s, suggesting only moderate redundancy among these variables, and the correlations do not form a pattern that would indicate underlying super ordinate factors. The one exception is a relatively high correlation between BDI and AIMS-affect scores (r = .74). Yet, when these two variables were collapsed into a single score for the multiple regression analysis, the results remained basically unchanged (data not shown). Thus, the unique variance explained by each of these affective variables was not due to the high degree of shared variance between them.
This study identified several psychosocial variables as significant correlates of treatment expectation for patients enrolling in a trial for CST. Patients who reported already engaging in a more adaptive approach to managing their chronic pain and who were not emotionally distressed as indexed by anxiety, depression, and who reported lower quality of life had more positive expectations about engaging in a 10-session treatment that guides patients toward more positive pain coping strategies. This study also found that no one pre-treatment patient characteristic was a unique correlate of patient treatment expectation. Just as important are the variables that were not associated with treatment expectation: level of pain and physical dysfunction, duration of OA, and disability status as well as standard demographic variables.
These observations are encouraging and also challenging for pain clinicians and researchers. They suggest that a multidimensional assessment of OA patients with chronic pain is necessary, and those who are psychologically distressed may have difficulty engaging in treatment. These patients, in particular, may benefit from and need motivational interviewing to enhance their uptake of pain coping skills.
Motivational interviewing (MI) approaches to pain are based on a theoretical model that maintains that the readiness to use pain coping skills is based on two factors: 1) the perceived importance of pain coping skills, and 2) the confidence (self-efficacy) that one has the ability to engage in these behaviors in a way that achieves desired outcomes (e.g. pain relief). 37 When working with a patient who has low expectations of CST, two MI approaches might be particularly useful.38 One approach is designed to enhance the patient's motivation for change, e.g. to move the patient from contemplating the use of coping skills toward preparing for or actually engaging in the use of pain coping skills. For example, during a therapeutic encounter with a patient with low expectations of CST, the clinician can listen empathically to the patient and affirm and acknowledge their concerns about using CST and use questioning to elicit the patient’s concerns about how he/she is currently coping and highlight statements that reflect a desire or intention to change how they are coping. The second approach is designed to strengthen patients’ belief that they can change how they are coping with pain. During a therapeutic encounter with a patient with low expectations, the clinician can observe instances of effective coping reported by the patient and reinforce the idea that the patient does make choices that yield either more helpful or more negative outcomes thereby highlighting the available control. Thus, these MI approaches may be particularly useful for enhancing patient's self-efficacy with regard to pain coping skills, a factor that we found was strongly related to higher treatment expectations.
The findings of this study partly replicate and expand upon two other studies that examined correlates of treatment expectation in pain patients. These studies also found that more adaptive coping with pain at baseline was associated with more positive treatment expectation.3, 5 However, the results differ in that we found a significant negative association with level of depression and did not find that disability status was related to treatment expectation. Differences between the studies could be due to many factors including different disease groups, variations in recruitment methods, and different treatment settings. Importantly, the variables in this study were able to account for 21% variance which is double that found in these two earlier studies.
This study had several limitations. First, the study sample is made up of predominantly older, female, and White patients. Replication of these findings is needed to determine whether they hold up in samples of OA patients that are more diverse especially with regard to sex and racial/ethnic background. Second, all patients in this study volunteered to participate in a clinical trial of CST. As might be expected on the basis of their volunteering, the mean level of their pre-treatment expectation was somewhat high (7/10). However, there was considerable variation in expectations with some patients having much higher treatment expectations than others. The situation in this clinical trial is likely similar to that which occurs when patients present for any new clinical pain treatment. One would anticipate that most patients would have somewhat high expectations, but that there would be variations with some patients reporting higher expectations than others. Third, future research may benefit from examining a more diverse set of patient characteristics to identify potentially unique correlates of treatment expectation. Fourth, we do not have data on the patients who declined the invitation to enter the clinical trial. Given their decision not to participate, these patients are likely to have lower treatment expectations and higher degrees of affective distress and poor coping. We have initiated a study to test this supposition.
In summary, this study was the first to examine correlates of treatment expectations for CST in OA patients with chronic pain. We found that patient expectations varied considerably. Patients, who were classified as adaptive copers, reported higher self efficacy and social interaction, had higher quality of life, and who had lower levels of affective distress and depression had more positive expectations about engaging in pain coping skills training. Variables that were not associated were level of pain and physical dysfunction, duration of disease, and disability status as well as demographic variables. Taken together, these findings underscore the notion that treatment expectation for CBT-based pain treatments can vary considerably and highlight the potential importance of psychosocial characteristics in understanding treatment expectations.
Acknowledgements
This research was supported by grants from the National Institutes of Health (AR054626 Joan E. Broderick, principal investigator) and Stony Brook University GCRC (Grant M01-RR10710) from the National Center for Research Resources. We would like to thank Amy Stein, John Pilosi, Anna Edwards, and Sarah Rowe for their assistance in collecting data and to Rebecca Shelby for her comments on this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Delsignore A, Schnyder U. Control expectancies as predictors of psychotherapy outcome: a systematic review. Br J Clin Psychol. 2007;46:467–483. doi: 10.1348/014466507X226953. [DOI] [PubMed] [Google Scholar]
- 2.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 3.Goossens ME, Vlaeyen JW, Hidding A, et al. Treatment expectancy affects the outcome of cognitive-behavioral interventions in chronic pain. Clin J Pain. 2005;21:18–26. doi: 10.1097/00002508-200501000-00003. discussion 69–72. [DOI] [PubMed] [Google Scholar]
- 4.Turk DC, Rudy TE. Neglected factors in chronic pain treatment outcome studies--referral patterns, failure to enter treatment, and attrition. Pain. 1990;43:7–25. doi: 10.1016/0304-3959(90)90046-G. [DOI] [PubMed] [Google Scholar]
- 5.Smeets RJ, Beelen S, Goossens ME, et al. Treatment expectancy and credibility are associated with the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. Clin J Pain. 2008;24:305–315. doi: 10.1097/AJP.0b013e318164aa75. [DOI] [PubMed] [Google Scholar]
- 6.Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 7.Habib S, Morrissey S, Helmes E. Preparing for pain management: a pilot study to enhance engagement. Journal of Pain. 2005;6:48–54. doi: 10.1016/j.jpain.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Borkovec TD, Nau CD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3:257–260. [Google Scholar]
- 9.Kerns R, Turk D, Rudy T. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 10.Wittink H, Turk DC, Carr DB, et al. Comparison of the Redundancy, Reliability, and Responsiveness to Change Among SF-36, Oswestry Disability Index, and Multidimensional Pain Inventory. Clin J Pain. 2004;20:133–142. doi: 10.1097/00002508-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Jakobsson U, Horstmann V. Psychometric evaluation of multidimensional pain inventory (Swedish version) in a sample of elderly people. European Journal of Pain. 2006;10:645–651. doi: 10.1016/j.ejpain.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Broderick J, Junghaenel D, Turk D. Stability of patient adaptation classifications on the Multidimensional Pain Inventory. Pain. 2004;109:94–102. doi: 10.1016/j.pain.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Multiaxial assessment of pain: Multidimensional Pain Inventory Computer Program. Pittsburgh: University of Pittsburgh; 1989. [computer program]. Version 2.1. [Google Scholar]
- 14.Turk D, Rudy T. Toward an empirically derived taxonomy of chronic pain patients: integration of psychological assessment data. J Consult Clin Psychol. 1988;56:233–238. doi: 10.1037//0022-006x.56.2.233. [DOI] [PubMed] [Google Scholar]
- 15.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 16.Keefe F, Brown G, Wallston K, et al. Coping with rheumatoid arthritis pain: catastrophizing as a maladaptive strategy. Pain. 1989;37:51–56. doi: 10.1016/0304-3959(89)90152-8. [DOI] [PubMed] [Google Scholar]
- 17.Keefe F, Caldwell D, Queen K, et al. Pain coping strategies in osteoarthritis patients. J Consult Clin Psychol. 1987;55:208–212. doi: 10.1037//0022-006x.55.2.208. [DOI] [PubMed] [Google Scholar]
- 18.Lorig K, Chastain R, Ung E, et al. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32:37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 19.Lorig K, Gonzalez V, Laurent D, et al. Arthritis self-management program variations: three studies. Arthritis Care Res. 1998;11:448–454. doi: 10.1002/art.1790110604. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez VM, Stewart A, Ritter PL, et al. Translation and validation of arthritis outcome measures into Spanish. Arthritis Rheum. 1995;38:1429–1446. doi: 10.1002/art.1780381010. [DOI] [PubMed] [Google Scholar]
- 21.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 22.Dunbar MJ, Robertsson O, Ryd L, et al. Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br. 2001;83:339–344. doi: 10.1302/0301-620x.83b3.11134. [DOI] [PubMed] [Google Scholar]
- 23.Basaran S, Guzel R, Seydaoglu G, et al. Validity, reliability, and comparison of the WOMAC osteoarthritis index and Lequesne algofunctional index in Turkish patients with hip or knee osteoarthritis. Clin Rheumatol. 29:749–756. doi: 10.1007/s10067-010-1398-2. [DOI] [PubMed] [Google Scholar]
- 24.Meenan RF, Mason JH, Anderson JJ, et al. AIMS2. The content and properties of a revised and expanded Arthritis Impact Measurement Scales Health Status Questionnaire. Arthritis Rheum. 1992;35:1–10. doi: 10.1002/art.1780350102. [DOI] [PubMed] [Google Scholar]
- 25.Ren XS, Kazis L, Meenan RF. Short-form Arthritis Impact Measurement Scales 2: tests of reliability and validity among patients with osteoarthritis. Arthritis Care Res. 1999;12:163–171. doi: 10.1002/1529-0131(199906)12:3<163::aid-art3>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 26.Merkel PA, Herlyn K, Martin RW, et al. Measuring disease activity and functional status in patients with scleroderma and Raynaud's phenomenon. Arthritis Rheum. 2002;46:2410–2420. doi: 10.1002/art.10486. [DOI] [PubMed] [Google Scholar]
- 27.Somers TJ, Shelby RA, Keefe FJ, et al. Disease severity and domain-specific arthritis self-efficacy: relationships to pain and functioning in patients with rheumatoid arthritis. Arthritis Care Res. 62:848–856. doi: 10.1002/acr.20127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burckhardt C, Woods S, Schultz A, et al. Quality of life of adults with chronic illness: A psychometric study. Res Nurs Health. 1989;12:347–354. doi: 10.1002/nur.4770120604. [DOI] [PubMed] [Google Scholar]
- 29.Beck A, Steer R, Brown G. Beck Depression Inventory®—II Manual. San Antonio, Texas: Harcourt Assessment, Inc; 1996. [Google Scholar]
- 30.Beck A, Steer R, Garbin M. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 31.Poole H, Bramwell R, Murphy P. Factor Structure of the Beck Depression Inventory-II in patients With chronic pain. Clin J Pain. 2006;22:790–798. doi: 10.1097/01.ajp.0000210930.20322.93. [DOI] [PubMed] [Google Scholar]
- 32.Thombs BD, Bass EB, Ford DE, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21:30–38. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999;80:1–13. doi: 10.1016/s0304-3959(98)00255-3. [DOI] [PubMed] [Google Scholar]
- 34.Turk DC. The potential of treatment matching for subgroups of patients with chronic pain: lumping versus splitting. Clin J Pain. 2005;21:44–55. doi: 10.1097/00002508-200501000-00006. discussion 69–72. [DOI] [PubMed] [Google Scholar]
- 35.Keefe FJ, Shelby RA, Somers TJ. Catastrophizing and pain coping: Moving forward. Pain. 2010;149:165–166. doi: 10.1016/j.pain.2010.02.030. [DOI] [PubMed] [Google Scholar]
- 36.Sullivan MJ, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Jensen MP, Nielson WR, Kerns RD. Toward the development of a motivational model of pain self-management. J Pain. 2003;4:477–492. doi: 10.1016/s1526-5900(03)00779-x. [DOI] [PubMed] [Google Scholar]
- 38.Jensen MP. Enhancing motivation to change in pain treatment. In: Turk DC, Gatchel RJ, editors. Psychological treatment for pain: A practitioner's handbook. New York: Guilford; 1996. pp. 78–111. [Google Scholar]