Abstract
We prospectively compared, according to their preoperative clinical profiles, the in-hospital outcomes of patients operated on consecutively (but without randomization) for isolated coronary artery disease with on-pump or off-pump techniques.
During 2001, 324 patients underwent coronary artery bypass grafting: 216 patients (mean age, 66.7 ± 8.9 years; range, 41–85 years) underwent on-pump revascularization, and 108 patients (mean age, 67.6 ± 10 years; range, 37–90 years) underwent full-sternotomy off-pump revascularization. The 2 groups were homogeneous with regard to female sex (22.6% vs 26.8%), previous cardiac operation (2.8% vs 4.6%), cardiogenic shock (1.3% vs 1.9%), diabetes (30% vs 33%), and chronic renal failure that required hemodialysis (3% vs 3.5%).
Postoperative complications, including bleeding, myocardial infarction, acute renal failure, mediastinitis with sternal dehiscence, cerebrovascular events, and prolonged respiratory assistance were more frequent in on-pump patients (P = 0.004). The total number of grafts and the grafts per patient ratio were significantly higher in on-pump patients (P = 0.0001), whereas the total number of full arterial revascularizations was higher in off-pump patients (P = 0.0001). Off-pump patients showed a significantly shorter intensive care unit stay (P = 0.02), and less need for intra-aortic balloon pump insertion (P = 0.04). In-hospital mortality was 2.8% in on-pump patients and 2.7% in off-pump patients (P = NS).
Although the hospital mortality rate was comparable for the 2 techniques, the in-hospital comparison between the 2 groups showed how the avoidance of cardiopulmonary bypass can significantly reduce the cumulative postoperative incidence of complications in patients undergoing coronary artery bypass grafting. (Tex Heart Inst J 2003;30:261–7)
Key words: Cardiopulmonary bypass, myocardial revascularization/methods, postoperative complications
Cardiopulmonary bypass (CPB) and cardioplegia have been the mainstays of coronary artery bypass grafting (CABG) for a long time. However, CPB has been recognized as one of the major causes of postoperative complications and multiple organ failure, especially in elderly patients or in the presence of diffuse atherosclerotic disease. 1 It has been shown, in fact, that the avoidance of CPB is associated with lower morbidity rates, mainly in selected high-risk subgroups of patients undergoing CABG. 2,3
Due to great improvements in technology that yield an optimal operative field, the ability to perform coronary anastomoses on the beating heart has increased; many authors have shown how even patients with multivessel coronary artery disease can be successfully revascularized with use of off-pump techniques. 4,5 Therefore, off-pump coronary artery bypass grafting (OPCAB) has become a real alternative.
We studied the in-hospital morbidity and mortality rates of 324 patients who underwent CABG via the on-pump technique (216 patients; CPB group) or via the off-pump technique (108 patients; OPCAB group), with nonrandomized assignment but with prospective data collection and follow-up.
Patients and Methods
Data Recording. From 1 January 2001 through 31 December 2001, we performed 324 isolated consecutive coronary artery revascularizations. One third (n=108) of these patients were operated on with the OPCAB technique by 2 surgeons. The optimal surgical strategy for each patient was determined on an individual basis by the attending surgeon in consultation with the patient, and not randomly. All the data were prospectively collected and monitored for morbidity and mortality rates during the patients' hospital stay.
The following preoperative data were recorded: age, sex, cardiac catheterization results (total number of diseased vessels and left ventricular ejection fraction), previous cardiac operation, indication (emergent, urgent, and elective), and risk factors (diabetes, chronic renal failure with and without hemodialysis, dyslipidemia, chronic obstructive pulmonary disease [COPD], preoperative intra-aortic balloon pump [IABP], smoking, peripheral vascular disease, previous neurologic events, previous myocardial infarction [MI], history of cancer, chronic atrial fibrillation, and systemic hypertension).
For the purposes of this study, we defined chronic renal failure as persistent preoperative high urea and creatinine values or the necessity for hemodialysis, which conditions we considered 2 separate risk factors. We summarized coronary study results in accordance with National Heart, Lung, and Blood Institute Coronary Artery Surgery Study guidelines. 6
Primary end-points were operative mortality, in-cidence of postoperative complications (including bleeding, need for IABP, MI, acute renal failure, sternal dehiscence because of mediastinitis, neurologic events, de novo atrial fibrillation, and prolonged respiratory assistance), the mean length of stay in the intensive care unit, the number of grafts per patient, and full arterial revascularization.
Postoperative bleeding was defined as bleeding that required surgical revision; IABP insertion, as use of a balloon between the end of the CABG procedure and discharge from the intensive care unit; mediastinitis, as septic sternal dehiscence; cerebrovascular events, as all new cerebral events that persist longer than 24 hours; and prolonged respiratory assistance, as a need for mechanical ventilation that exceeds 24 hours. When 2 of the 3 following criteria were present, a myocardial infarction was recorded: new Q-waves on 12-lead electrocardiogram, significant increase in P-troponine I and P-creatine kinase myocardial band, and new regional abnormalities on 2-dimensional echocardiogram. Acute renal failure was defined as postoperative P-creatinine and urea values increased in relation to preoperative ones or the need of furo-semide infusion for longer than 72 hours or of hemodialysis, despite good hemodynamic status.
The indication for surgery was defined as emergent when the patient was in cardiogenic shock, urgent when the patient was operated on within 48 hours of admission or diagnosis, and elective when the patient was in stable clinical status and summoned from home on the day before the operation. Operative mortality was defined as in-hospital death or death within 30 days.
Most OPCAB patients underwent re-evaluation by coronary arteriography before discharge. The only exclusion criteria were critical renal failure and denied consent. Cardiopulmonary bypass patients did not undergo postoperative coronary angiography.
Surgical Technique
Anesthesia. All procedures were performed with the patients under general anesthesia; in addition, patients received oral lorazepam, 2 mg, 1 hour before the start of anesthesia. Monitoring catheters were inserted under local anesthesia in the left radial artery for continuous monitoring of blood pressure and in the right internal jugular vein for infusing drugs and monitoring central venous pressure. Monitoring was also performed via electrocardiographic leads II and V5 with automated ST-segment analysis and trending, via pulse oximetry, and via capnometry. After a 5-minute preoxygenation period, general anesthesia was induced with thiopental (2.5 mg/kg) followed by fentanyl (5 μg/kg) and vecuronium (0.1 mg/kg). Mechanical ventilation with a mixture of 60% oxygen and 40% room air was administered. Maintenance of anesthesia was achieved with fentanyl (up to 20 μg/kg before sternotomy) and with a continuous infusion of propofol (3 mg/kg per hour) and cisatracurium (1.5 μg/kg per min). Intravenous antibiotic prophylaxis (cephazolin, 30 mg/kg) was given. All patients were monitored during the entire procedure by means of transesophageal echocardiography.
All patients were operated on through a median sternotomy. The conduits of choice were the left and right internal thoracic arteries (LITA and RITA, respectively), the radial artery, and the saphenous vein. The thoracic arteries were harvested as pedicled vessels with satellite veins, fascia, and muscle.
Off-Pump Coronary Artery Bypass. When performing OPCAB surgery, we routinely used a Genzyme stabilizing system (Genzyme Corporation; Cam bridge, Mass), Silastic rubber sutures placed proximal and distal to the anastomotic site as coronary artery occluders, an intraluminal shunt in case of hemodynamic instability, and a custom-made blower insufflating humidified CO2 at a flow less than 5 L/min, to ensure a bloodless operative field.
Intravenous heparin (1 mg/kg) was given to maintain an activated clotting time longer than 400 seconds. Deep pericardial sutures were placed to keep the heart vertical to enable lateral vessel grafting, and the orientation of the operating table was modified to enable exposure of the right coronary artery territory.
After we performed the arteriotomy, we tightened the snares, avoiding excessive tension, just enough to obtain a bloodless operative field. We preferred to perform first the anastomosis on the vessel with the culprit stenosis or with a large dependent territory. When the radial artery, saphenous vein, and LITA or RITA grafts were performed in a free-graft or Y-graft configuration, the proximal anastomosis was fashioned first. The posterior descending coronary artery was preferred to the right coronary artery as the target vessel, to avoid arrhythmias and atrioventricular block.
Cardiopulmonary Bypass. When performing CABG surgery under CPB, we maintained the activated clotting time above 480 seconds. Cardiopulmonary bypass was instituted with a single right atrial cannula and ascending aortic cannulation. The flow was maintained at 2.4 L/min/m2 with a mean arterial blood pressure greater than 50 mmHg, at 32 °C; in the instance of a previous cerebrovascular event, the flow was pulsatile. Cardiac arrest was achieved by cold intermittent blood cardioplegia, antegrade and retrograde.
Statistics. The prevalence of risk factors and the 1-year cumulative incidence of perioperative (in-hospital) death and complications in the 2 groups were compared with the Fisher exact test for discrete variables and the t test for continuous variables.
Results
Demographics. All preoperative data and risk factors are detailed in Table I. The 2 patient populations, CPB and OPCAB, were comparable with regard to mean age and age distribution, female sex (22.6% vs 26.8%, respectively), previous cardiac operation, diabetes, cardiogenic shock, chronic renal failure, chronic renal failure treated with hemodialysis, dyslipidemia, surgical indications, preoperative IABP insertion, peripheral vascular disease, low ejection fraction, history of cancer, chronic atrial fibrillation, and hypertension. In CPB patients, there was a significant occurrence of smoking (18.5% vs 8.3%), previous neurologic events (7.8% vs 2.7%), and previous MI (21.3% vs 12%). Chronic obstructive pulmonary disease was more prevalent in OPCAB patients (9.2% CPB vs 21.3% OPCAB). The OPCAB patients were a little older, and that group had a slightly larger percentage of women. With regard to age distribution, the OPCAB patients had a larger distribution in the age group over 60 years, and the CPB patients were homogeneously distributed even in the younger age group. No patient selected for the OPCAB surgical technique was converted to CPB surgery during operation.
TABLE I. Demographics and Risk Factors

Patients with fewer diseased vessels, specifically single or double vessels, prevailed significantly in the OPCAB group (single vessel, P = 0.0001; double ves sel, P = 0.045). Multivessel disease prevailed in the CPB group (P = 0.0001). Left main disease was 19.2% in the CPB group and 14.3% in the OPCAB group (P = 0.36) (Table II).
TABLE II. Operative Data on 324 Patients
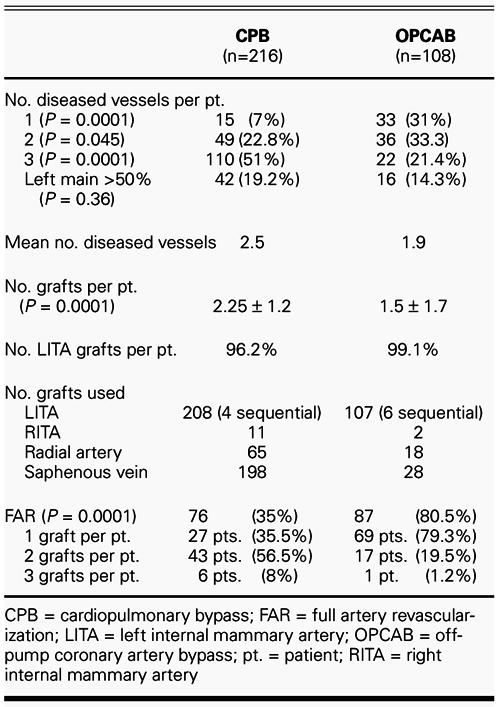
Full revascularization dominated in CPB patients (grafts per patient, 2.25 ± 1.2 CPB vs 1.5 ± 1.7 OPCAB; P = 0.0001), and full arterial revasculariza tion dominated in OPCAB patients (35% CPB vs 80.5% OPCAB; P = 0.0001). The LITA grafts were used in most patients in both groups (96.2% CPB vs 99.1% OPCAB). Four LITA grafts were performed in sequential fashion to the left anterior descending coronary artery (LAD) and diagonal branch in the CPB group, in comparison with 6 sequential grafts in the OPCAB patients. The RITA grafts were used in only 5% of CPB patients and in 1.8% of OPCAB patients, because we enlarged the use of the nondominant radial artery (13.4% of total grafts in CPB vs 11.2% in OPCAB) (Table II). When the ascending aorta was affected by atherosclerotic plaques, detected either by palpation or by epiaortic ultrasonography, we attempted to prevent perioperative stroke by avoiding partial aortic clamping; instead, we per formed the proximal anastomosis in the Y-graft fashion (6 CPB vs 4 OPCAB patients).
Postoperative Morbidity. Table III summarizes the in-hospital morbidity rates of all patients. The complication with the highest incidence rate was acute renal failure, which occurred mostly in CPB patients (10.2% CPB vs 5.5% OPCAB; P = 0.21). Among patients who had acute renal failure, 13.6% of CPB and 33% of OPCAB patients had chronic renal failure preoperatively.
TABLE III. Postoperative Morbidity
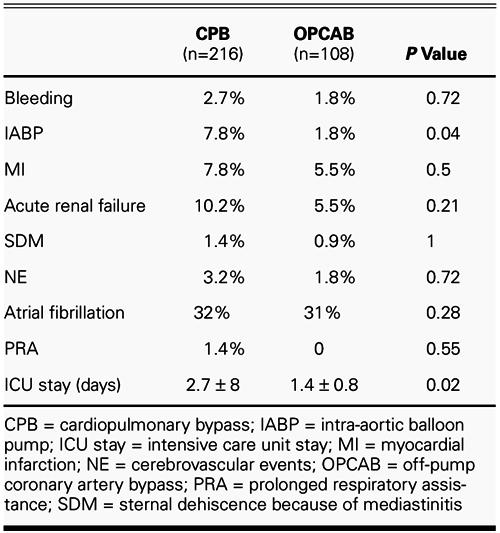
The use of the IABP was significantly higher in the CPB patients (7.8% vs 1.8%; P = 0.04), and MI was more frequent in the CPB patients, although not significantly so (7.8% CPB vs 5.5% OPCAB; P = 0.5).
In regard to all other complications, bleeding, sternal dehiscence due to mediastinitis, neurologic events, atrial fibrillation, and prolonged respiratory assistance were more frequent in CPB patients, although not significantly so. In all patients who sustained neurologic events, the proximal anastomoses were performed with partial ascending aortic clamping. When the cumulative postoperative incidence of all complications in patients undergoing CABG was compared, a statistically significant low occurrence (P = 0.004) was found in the OPCAB group.
The mean intensive care unit stay (in days) was significantly longer in the CPB than in the OPCAB patients (P = 0.02).
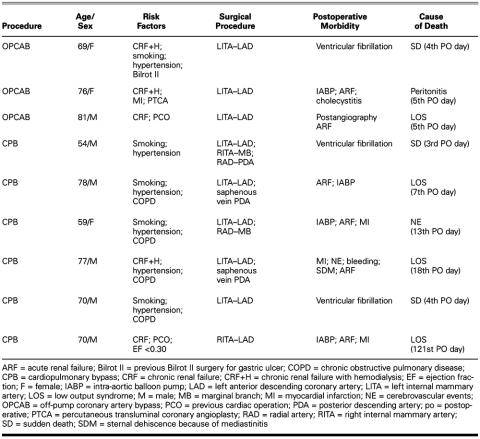
Postoperative Mortality. Six patients died in the CPB group and 3 in the OPCAB group, for operative mortality rates of 2.8% and 2.7%, respectively (Table IV). Among the 6 deaths in the CPB group, 2 patients died suddenly on the 3rd and 4th postoperative days, 3 died of low cardiac output syndrome and acute renal failure due to MI, and the last died because of a new neurologic event. Among the 3 OPCAB deaths, 1 patient died suddenly on the 4th postoperative day, the 2nd because of low cardiac output syndrome due to acute renal failure secondary to postoperative angiography, and the last because of cholecystitis. The patients who died had the following prevalent risk factors: chronic renal failure treated with hemodialysis (2 OPCAB and 1 CPB; 33.3% of the patients who died), previous cardiac surgery (the first was a CPB patient who 8 years before had undergone a LITA–LAD graft and marginal and posterior descending artery branch anastomoses with saphenous vein grafts; and the second was an OPCAB patient who 12 years before had undergone double saphenous vein anastomoses of the LAD and the marginal branch), and IABP insertion (4 CPB vs 1 OPCAB).
TABLE IV. Postoperative Mortality
The patients underwent autopsy, and the cause of death was discussed with the pathologist. All the anastomoses that had been performed in these patients were patent.
Postoperative Angiography. Angiography before discharge was performed in 86 OPCAB patients (79.6%). All 6 sequential grafts were patent. Among a total of 155 grafts performed in 108 OPCAB patients, 5 (3.2%) grafts showed a culprit stenosis in 3 patients (2.7%). Only in 1 patient, a 77-year-old man with a critical distal stenosis at the LITA–LAD anastomosis level, was a percutaneous transluminal coronary angioplasty procedure performed. In the other 2 patients, no adjunctive procedure was added.
Discussion
This study prospectively investigated the in-hospital mortality and morbidity rates of 2 groups of patients who were assigned to CPB or OPCAB techniques (but not at random), which were performed during a 1-year period in single university center.
Off-pump myocardial revascularization, which avoids tissue ischemia and systematic inflammatory response as well as less oxidative stress and myocardial injury, is gaining popularity as a feasible alternative to conventional CABG with CPB and is displaying a trend toward lower rates of morbidity and mortality, and lower cost. 7,8
Many reports confirm that single and multiple coronary revascularization can be performed safely in a beating heart, with good early and mid-term results: specifically, a lower incidence of neurologic deficit, renal failure, prolonged airway intubation, blood loss, and wound infections, compared with on-pump cases. 4,9,10
Nevertheless, some authors 11 have identified a large number of patients who experienced new-onset angina after undergoing off-pump procedures. Moreover, some of these patients had angiograms showing stenoses at or near the anastomotic sites. 11
It is clear that high-quality anastomoses are crucial for graft patency. It is therefore mandatory to obtain good intraoperative exposure and stabilization in order to achieve this goal. 12
In the present study, the 2 groups of patients were comparable in age and distribution of age, sex, previous cardiac operation, surgical indication, preoperative IABP insertion, low ejection fraction, chronic renal failure, diabetes, dyslipidemia, peripheral vascular disease, history of cancer, chronic atrial fibrillation, and hypertension. The only risk factors significantly different between the 2 groups were previous MI, previous neurologic event, and smoking, which were more frequent in CPB patients, and COPD, which was more frequent in OPCAB patients.
The CPB patients had significantly more complete revascularizations, with a mean of 2.25 ± 1.2 grafts and a mean of 2.5 diseased vessels, as opposed to a mean of 1.5 ± 1.7 grafts and 1.9 diseased vessels in OPCAB patients. Full arterial revascularization predominated in OPCAB patients (80.5% vs 35%) because of a significant prevalence of single- and double-vessel disease in this group. All the CABG patients who underwent full arterial revascularization received complete revascularization.
The concept that complete revascularization is associated with better long-term survival has been advanced by many authors. 13,14 Scott and associates 14 showed that the LITA–LAD graft is the most important bypass graft but that patients (2,067 patients; mean age, 54 ± 9 years) who underwent an incomplete revascularization were affected by a significantly lower survival rate, starting from the 2nd decade after surgery. Our current policy, to minimize complications, is to avoid full revascularization in the presence of small and greatly diseased vessels with poor run-off, fibrous or necrotic areas, or significant comorbid conditions that increase surgical risk. The single-vessel LITA–LAD patients in our study were older (mean age, 71 ± 9.7 years) than were Scott's patients, which in itself increased the morbidity and mortality risks. Moreover, these patients were severely affected by many comorbid conditions, such as chronic renal failure (14%), COPD (7%), peripheral vascular disease (7%), low ejection fraction (4.4%), previous MI (7%), and previous cardiac operation (4%), which in our judgment justified incomplete revascularization policy in this 70-year-old population.
The cumulative incidence rate of postoperative blood loss and bleeding that required surgical re-exploration was higher in CPB patients. De novo atrial fibrillation and sternal dehiscence due to mediastinitis were also more frequent in CPB patients. Acute renal failure was the most frequent complication, with an occurrence rate of 9% in the total population: in CPB patients it was almost double that in OPCAB patients (10.2% vs 5.5%; P = NS), despite the higher rate of chronic renal failure in the latter group.
According to our data and to other authors' findings in regard to elderly patients or to severe left ventricular dysfunction, 15–17 OPCAB results in better myocardial preservation with a lower need for IABP insertion and a lower occurrence of new MI. Our 2 groups were absolutely comparable in terms of surgical indication, low ejection fraction, need for preoperative IABP insertion, and previous cardiac operation.
The occurrence of a new neurologic event was higher in CPB patients, as expected, 18 but it is relevant to note that these patients were significantly more affected by cerebral complications preoperatively. All of the patients affected by neurologic events underwent partial aortic clamping for the proximal anastomosis, and no instance of significant atherosclerosis of the ascending aorta was detected at palpation. These data suggest the usefulness in this high-risk subgroup of patients of the no-touch aortic technique using sequential and Y-graft anastomoses, as described by other authors. 19
The stay in the intensive care unit was significantly shorter among OPCAB patients because of shorter time to extubation (despite a greater prevalence of COPD in these patients; P = 0.005), less occurrence of acute renal failure and less need of furosemide in-fusion, and shorter time for hemodynamic recovery.
The in-hospital mortality rate was similar with the 2 techniques; however, most deaths in OPCAB patients were noncardiac related. The anastomoses were all widely patent at autopsy. In this group, 1 patient died of low-output syndrome: he was an 81-year-old man with chronic renal failure and previous cardiac operation who was discharged from the intensive care unit on the 2nd postoperative day and died of acute renal failure consequent to follow-up coronary angiography. None of the patients who died experienced an acute MI. Three patients in the CPB group died of low-output syndrome, and in 2 of these an acute MI was discovered. Two patients died suddenly, and autopsy did not clarify the cause of these deaths, which occurred despite patent graft anastomoses. One young woman without a previous cerebral event died of a neurologic event; in this case, the patient had under gone double-vessel revascularization with a partial clamping technique for the proximal anastomosis.
The achievement of high-quality anastomosis is more difficult in the OPCAB technique but is of course critical to its success. We performed early pre-discharge angiography in 80% of OPCAB patients, the results of which showed a high patency rate and confirmed other authors' good results with beating-heart surgery. 20 Three patients were affected by critical graft stenosis, but in only 1 case did the cardiologist perform a percutaneous transluminal coronary angioplasty. When we weigh the benefits of optimal patency against the risks of invasive follow-up angiography (1 death due to acute renal failure and low-output syndrome), we think we should limit re-study to patients without comorbid conditions.
In conclusion, the patients who underwent CABG with the OPCAB technique showed a lower cumulative incidence of complications and a lower mortality rate than did the CPB patients, even in higher risk patients, although this difference was not significant if each complication was analyzed in isolation. The need for IABP intervention and the rate of myocardial infarction were less frequent during OPCAB surgery, and the OPCAB patients' recovery time in intensive care was shorter. The postoperative angiographic studies, consecutively performed, showed excellent quality and patency of anastomoses in the sequential and Y-grafts fashioned during use of the beating-heart technique. Reducing manipulation of the ascending aorta by avoiding cannulation and partial clamping contributes greatly to the reduction of cerebrovascular complications.
Footnotes
Address for reprints: Tomaso Bottio, MD, Istituto di Chirurgia Cardiovascolare, Via Giustiniani, 2, 35128 Padova, Italy
E-mail: tomaso.bottio@unipd.it
References
- 1.Edmunds LH Jr. Why cardiopulmonary bypass makes patients sick: strategies to control the blood-synthetic surface interface. In: Karp RB, Laks H, Wechsler AS, editors. Advances in cardiac surgery. Vol 6. St Louis: Mosby; 1995. p. 131–67. [PubMed]
- 2.Wan S, Izzat MB, Lee TW, Wan IY, Tang NL, Yim AP. Avoiding cardiopulmonary bypass in multivessel CABG reduces cytokine response and myocardial injury. Ann Thorac Surg 1999;68:52–7. [DOI] [PubMed]
- 3.Arom KV, Flavin TF, Emery RW, Kshettry VR, Janey PA, Petersen RJ. Safety and efficacy of off-pump coronary artery bypass grafting. Ann Thorac Surg 2000;69:704–10. [DOI] [PubMed]
- 4.Cartier R, Brann S, Dagenais F, Martineau R, Couturier A. Systematic off-pump coronary artery revascularization in multivessel disease: experience of three hundred cases. J Thorac Cardiovasc Surg 2000;119:221–9. [DOI] [PubMed]
- 5.Bull DA, Neumayer LA, Stringham JC, Meldrum P, Affleck DG, Karwande SV. Coronary artery bypass grafting with cardiopulmonary bypass versus off-pump cardiopulmonary bypass grafting: does eliminating the pump reduce morbidity and cost? Ann Thorac Surg 2001;71:170–5. [DOI] [PubMed]
- 6.The National Heart, Lung, and Blood Institute Coronary Artery Surgery Study. A multicenter comparison of the effects of randomized medical and surgical treatment of mildly symptomatic patients with coronary artery disease, and a registry of consecutive patients undergoing coronary angiography. Circulation 1981;63(6 Pt 2):I1–59. [PubMed]
- 7.Arom KV, Emery RW, Flavin TF, Peterson RJ. Cost-effectiveness of minimally invasive coronary artery bypass surgery. Ann Thorac Surg 1999;68:1562–6. [DOI] [PubMed]
- 8.Reichenspurner H, Boehm D, Detter C, Schiller W, Reichart B. Economic evaluation of different minimally invasive procedures for the treatment of coronary artery disease. Eur J Cardiothorac Surg 1999;16(Suppl 2):S76–9. [PubMed]
- 9.Hernandez F, Cohn WE, Baribeau YR, Tryzelaar JF, Charlesworth DC, Clough RA, et al. In-hospital outcomes of off-pump versus on-pump coronary artery bypass procedures: a multicenter experience. Ann Thorac Surg 2001;72:1528–34. [DOI] [PubMed]
- 10.Anyanwu AC, Al-Ruzzeh S, George SJ, Patel R, Yacoub MH, Amrani M. Conversion to off-pump coronary bypass without increased morbidity or change in practice. Ann Thorac Surg 2002;73:798–802. [DOI] [PubMed]
- 11.Gundry SR, Romano MA, Shattuck OH, Razzouk AJ, Bailey LL. Seven-year follow-up of coronary artery bypasses performed with and without cardiopulmonary bypass. J Thorac Cardiovasc Surg 1998;115:1273–8. [DOI] [PubMed]
- 12.Pirk J, Kellovsky P. An alternative to cardioplegia. Ann Thorac Surg 1995;60:464-5. [DOI] [PubMed]
- 13.Jones EL, Weintraub WS. The importance of completeness of revascularization during long-term follow-up after coronary artery operations. J Thorac Cardiovasc Surg 1996;112:227–37. [DOI] [PubMed]
- 14.Scott R, Blackstone EH, McCarthy PM, Lytle BW, Loop FD, White JA, Cosgrove DM. Isolated bypass grafting of the left internal thoracic artery to the left anterior descending coronary artery: late consequences of incomplete revascularization. J Thorac Cardiovasc Surg 2000;120:173–84. [DOI] [PubMed]
- 15.Demers P, Cartier R. Multivessel off-pump coronary artery bypass surgery in the elderly. Eur J Cardiothorac Surg 2001;20:908–12. [DOI] [PubMed]
- 16.Al-Ruzzeh S, George S, Yacoub M, Amrani M. The clinical outcome of off-pump coronary artery bypass surgery in the elderly patients. Eur J Cardiothorac Surg 2001;20:1152–6. [DOI] [PubMed]
- 17.Eryilmaz S, Corapcioglu T, Eren NT, Yazicioglu L, Kaya K, Akalin H. Off-pump coronary artery bypass surgery in the left ventricular dysfunction. Eur J Cardiothorac Surg 2002;21:36–40. [DOI] [PubMed]
- 18.van der Linden J, Hadjinikolaou L, Bergman P, Lindblom D. Postoperative stroke in cardiac surgery is related to the location and extent of atherosclerotic disease in the ascending aorta. J Am Coll Cardiol 2001;38:131–5. [DOI] [PubMed]
- 19.Al-Ruzzeh S, George S, Bustami M, Nakamura K, Khan S, Yacoub M, Amrani M. The early clinical and angiographic outcome of sequential coronary artery bypass grafting with the off-pump technique. J Thorac Cardiovasc Surg 2002;123:525–30. [DOI] [PubMed]
- 20.Lund O, Christensen J, Holme S, Fruergaard K, Olesen A, Kassis E, Abildgaard U. On-pump versus off-pump coronary artery bypass: independent risk factors and off-pump graft patency. Eur J Cardiothorac Surg 2001;20:901–7. [DOI] [PubMed]