Abstract
Laparoscopic cholecystectomy is the standard procedure for symptomatic gall stone disease. Situs inversus is a condition where the visceral anatomy is reversed. Laparoscopic cholecystectomy in a patient of situs inversus is a technically difficult procedure. Six patients of situs inversus underwent laparoscopic cholecystectomy from January 2003 to December 2009. In the first patient of situs inversus, we operated by placing the ports in mirror image fashion as that of standard laparoscopic cholecystectomy. However in next five patients we modified the technique by interchanging the epigastric and left mid clavicular line ports to overcome the problem of handedness. The procedure was successfully completed in all six patients. No intraoperative or postoperative complications occurred. The mean operating time was 65 mins (45–85 mins). Laparoscopic cholecystectomy is safe in patients of situs inversus. However, extreme care and skill is required to identify the reversed anatomy and to overcome the problem of handedness. Interchanging the epigastric and left mid clavicular line ports makes the procedure easier.
Keywords: Situs inversus, Laparoscopic cholecystectomy
Introduction
Prof. Med Erich Muhe performed first laparoscopic cholecystectomy on September 12, 1985. Phillipe Mouret performed laparoscopic cholecystectomy in March 1987. Since then, it has become the gold standard technique for removal of pathological gall bladder. Performing laparoscopic cholecystectomy in a patient of situs inversus poses great challenges right from diagnosis, investigating the patient to the most important aspect i.e. performing the procedure itself. The reason is obviously the reversed anatomical orientation of the visceral organs, whereby the liver and gall bladder are situated on the left side of the abdominal cavity and stomach and spleen are on the right side. Inspite of these difficulties, laparoscopic cholecystectomy has been performed in patients of situs inversus and its safety established. Here, we share our experience of laparoscopic cholecystectomy in 6 patients of situs inversus and discuss the technical challenges encountered during the procedure as well as suggest the solutions to overcome those difficulties.
Patients & Methods
This study is retrospective data analysis of patients who underwent laparoscopic cholecystectomy during the period from January 2003 to December 2009. All patients diagnosed to have symptomatic gall stone disease and situs inversus were included in the study.
Patients presenting with upper abdominal or left upper quadrant pain were evaluated by ultrasound study of abdomen. Those patients diagnosed to have situs inversus and cholelithiasis were further investigated to rule out cardiac anomalies by echocardiogram. Electrocardiogram, chest X-ray and upper GI endoscopy were routinely performed in all patients.
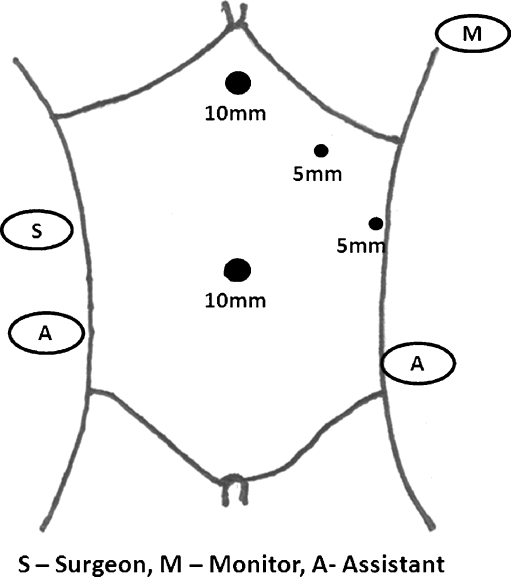
After thorough hematological and biochemical investigations, the patients were operated under general anaesthesia. In the first case, we operated in a position where the primary surgeon and first assistant stood on the right side of the patient while the second assistant and the monitor were on left side of the patient. The ports were positioned in mirror image fashion as that of standard laparoscopic cholecystectomy with 10 mm umbilical and epigastric ports and 5 mm left mid clavicular line and left anterior axilliary line subcostal ports [Fig. 1]. However the primary surgeon, being right handed, faced difficulty in dissection with the left hand through the epigastric port while the right hand was used for traction on Hartman’s pouch. However, the procedure was completed safely.
Fig. 1.
OT set up and port position in first case
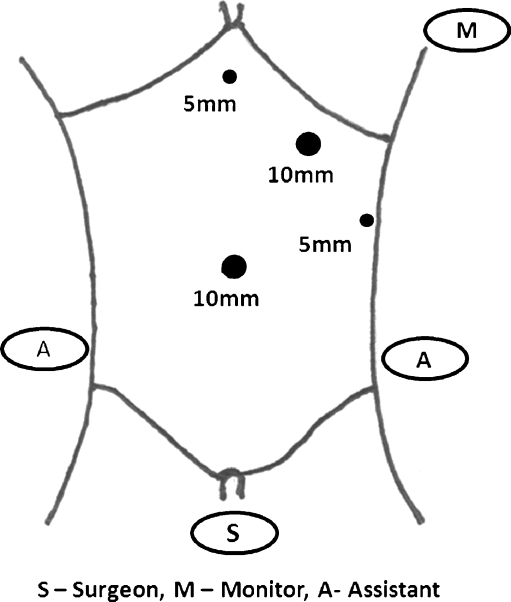
Learning from the first experience we adopted certain modifications in the next patient. The primary surgeon stood in between the legs of the patient and the monitor was put at the left shoulder. The camera assistant stood at the right flank while the second assistant stood on left side of the patient. Pneumoperitoneum was created by closed technique using a veress needle. 10 mm optical port was inserted at umbilicus. 5 mm epigastric and left anterior axilliary line subcostal ports were made. Another 10 mm subcostal right hand working port was made at left mid clavicular line [Fig. 2]. Liver and gall bladder were visualized on left side of the peritoneal cavity [Fig. 3] while stomach and spleen were seen on right side. The surgeon dissected through the 10 mm left mid clavicular line port using his right hand while holding the Hartman’s pouch with the left hand through the 5 mm epigastric port. Left anterior axilliary line port was used for holding the fundus of gall bladder. Calot’s traingle dissection, clipping of cystic duct and cystic artery and raising the gall bladder from its bed were done from the left mid clavicular line port [Fig. 4]. Gall bladder was put into an endobag and extracted via the umbilical port. This technique was adopted in all the subsequent cases. Drain was kept in one patient who had acute cholecystitis.
Fig. 2.
OT set up and port position in later five cases
Fig. 3.
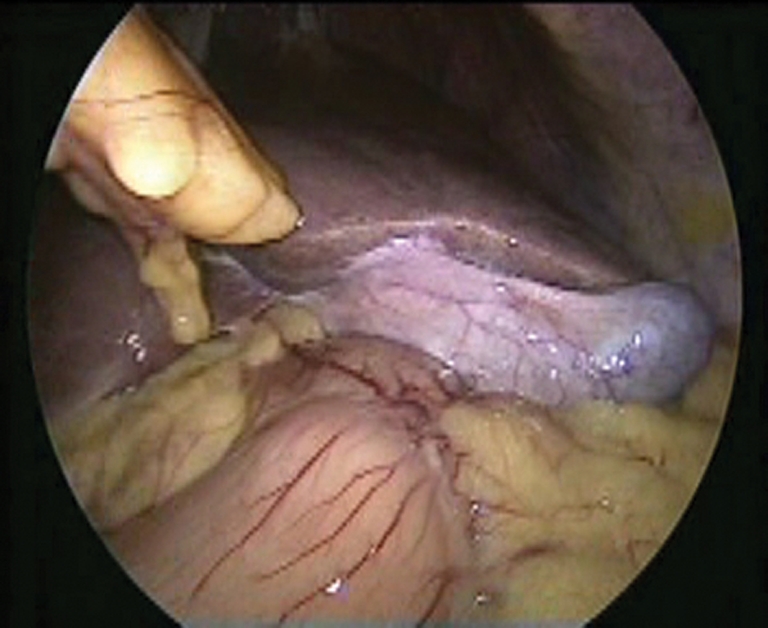
Laparoscopic view of gall bladder in situs inversus
Fig. 4.
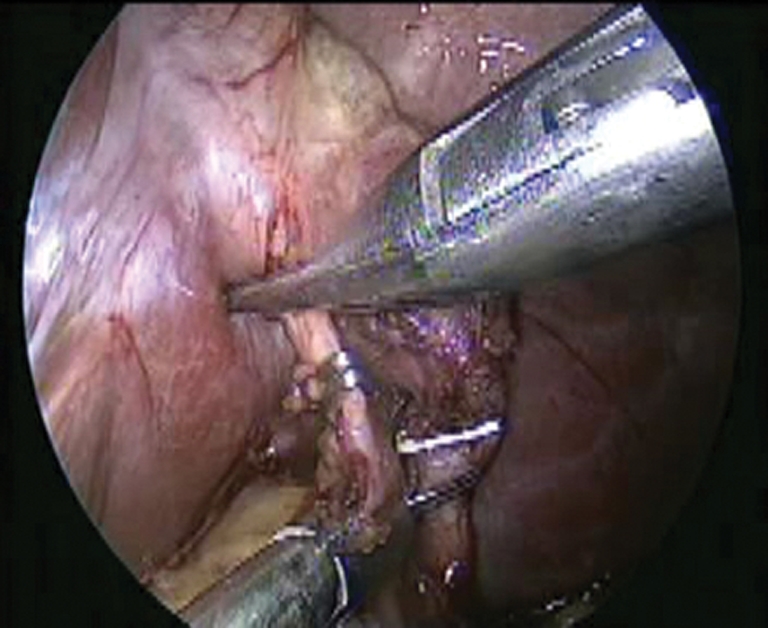
Clipping of inferior cystic artery and cystic duct
Results
During January 2003 to December 2009, 7131 patients underwent laparoscopic cholecystectomy at ILS Hospital, Kolkata. Out of these, six patients, including five females and 1 male, were diagnosed to have situs inversus totalis. The incidence of situs inversus cannot be derived from this data as the centre is a high volume referral centre for laparoscopic procedures and patients of situs inversus diagnosed elsewhere were referred for laparoscopic cholecystectomy. The patient demographic data is as per Table 1. None of the patients had choledocholithiasis or pancreatitis.
Table 1.
Demographic data of patients of situs inversus and clinical details
| S. No | Age/Sex | Presenting complaints | Previous surgery | Diagnosis | Complication | 7 day F/U | Histopathology |
|---|---|---|---|---|---|---|---|
| 1 | 36/F | Dull ache LHQ pain | – | Cholelithiasis | – | OK | Cholecystitis |
| 2 | 43/F | LHQ pain | LUCS | Cholelithiasis | – | OK | Cholecystitis |
| 3 | 27/F | LHQ pain | – | Cholelithiasis | – | OK | Cholecystitis |
| 4 | 48/M | Epigastric pain, dyspepsia | – | Cholelithiasis | – | OK | Cholecystitis |
| 5 | 59/F | Acute LHQ pain | – | Acute Cholecystitis | – | OK | Cholecystitis |
| 6 | 33/F | LHQ dull ache | TOF | Cholelithiasis | – | OK | Cholecystitis |
All the patients underwent laparoscopic cholecystectomy by a surgical team headed by the second author. The first patient was operated by placing ports in mirror-image fashion. But it was found to be difficult due to problems of ‘handedness’. Hence the later 5 cases were operated with the primary surgeon standing in between the legs of the patient and interchanging the epigastric and left mid clavicular line ports. This technique was found to be more comfortable. The mean operating time was 65 mins (45–85 mins). There were no major vascular or bile duct injuries during the procedure. One patient had inferior cystic artery. No other obvious vascular or ductal anomalies were encountered. Five patients who were electively operated were discharged on the next day while the patient operated for acute cholecystitis was discharged after 48 hrs. There were no post-operative complications. Histopathological reports came as cholecystitis in all patients.
Discussion
Situs inversus is a morphological anomaly of positioning of internal viscera wherein there is reversal of the usual ‘handedness’ of visceral topography [1]. It is a rare autosomal recessive disorder occurring in 1:5000 to 1:20,000 [2–4]. The first human case of situs inversus was reported by Fabricius in 1600 [5]. The reversal may be thoracic, abdominal or both. The normal development requires a 270 degree counter clock wise rotation that yields the normal anatomy of the visceral structures. In situs inversus the 270 degree rotation occurs in the clock wise direction [6]. Depending on the degree of malrotation situs inversus may be total, including abdominal and thoracic organs (situs inversus totalis) or more rarely, partial (situs inversus partialis) [2]. It may be associated with other congenital anomalies, such as renal dysplasia, biliary atresia, congenital heart disease or pancreatic fibrosis [2]. Situs inversus associated with bronchiectasis and sinusitis is known as Kartagener’s syndrome. The incidence of cholelithiasis in situs inversus is believed to be same as in general population. However, the presentation of patients of situs inversus having gall stone disease is different as they have left upper quadrant pain or epigastric discomfort causing delay in diagnosis and about 10% patients have right upper quadrant pain also [7]. The proposed explanation for this is that the central nervous system may not share in the general transposition [3].
Laparoscopic cholecystectomy is the gold standard treatment for symptomatic gall stone disease in normal population. However, its application in situs inversus has been viewed with skepticism for obvious reasons. The first known report on laparoscopic cholecystectomy in a patient with situs inversus was by Campos and Sipes in 1991 [8]. Since then, various case reports have confirmed the safety of laparoscopic cholecystectomy in situs inversus. The procedure is however, more difficult and precautions must be taken to modify the technique and understand the reversed anatomy.
For overt reasons, surgeons performing laparoscopic cholecystectomy in situs inversus patients face difficulties. Not only the orientation of the visceral anatomy is reserved, the problem of ‘handedness’ also needs to be overcome. Most of the reports on laparoscopic cholecystectomy in situs inversus mention operative technique where the operating surgeon stands on the right side, monitor is placed on left side and the ports are placed in the mirror image position as that of standard laparoscopic cholecystectomy. We also performed the first case of the present series in the same fashion. However the problem of handedness posed difficulties in dissecting with the left hand. Few reports mention overcoming this problem by having the assistant to hold the Hartman’s pouch while the primary surgeon does the dissection through the epigastric port with his right hand [3, 9]. However, this requires better co-ordination between two different surgeons which is more difficult than achieving co-ordination between two hands of the same surgeon. Hence we changed the technique by altering the 10 mm right hand working port to left mid clavicular line while retracting the gall bladder neck through the 5 mm epigastric left hand working port. This technical modification is also described in literature [10]. We share the same experience as that of these authors. There was some difficulty due to crossing of the instruments but this was easily overcome. The procedure could be completed safely in all the patients with no complications even in one case of acute cholecystitis.
Conclusion
Laparoscopic cholecystectomy in patients of situs inversus, although a difficult proposition, is feasible and safe. The presentation of gall stone disease in the patients is often atypical. These patients must be carefully investigated to rule out associated congenital anomalies. While operating on these patients, extreme care is required for proper recognition of the reversed anatomy. The technique of operating with the primary surgeon standing in between the patient’s leg and interchanging the epigastric and left subcostal midclavicular ports is easier than the more commonly described ‘mirror-image’ technique.
Disclosure of Statement
The authors do not have any commercial associations that might create a conflict of interest in connection with the submitted manuscript.
References
- 1.Kumar S, Fusai G (2007) Laparoscopic cholecystectomy in situs inversus totalis with left-sided gall bladder. Ann R Coll Surg Engl 89 [DOI] [PMC free article] [PubMed]
- 2.Pitiakoudis M, Tsaroucha AK, Kototomichelakis M, Polychronidis A, Simopoulos C. Laparoscopic cholecystectomy in a patient with Situs Inversus using ultrasonically activated coagulating scissors. Report of a case and review of the literature. Acta chir belg. 2005;105:114–117. [PubMed] [Google Scholar]
- 3.McKay D, Blake G. Laparoscopic cholecystectomy in situs inversus totalis: a case report. BMC Surgery. 2005;5:5. doi: 10.1186/1471-2482-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah AY, Patel BC, Panchal BA. Laparoscopic cholecystectomy in-patient with situs inversus. JMAS March. 2006;2:1. doi: 10.4103/0972-9941.25674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yaghan RJ, Gharaibeh KI, Hammori S. Feasibility of laparoscopic cholecystectomy in situs inversus. J Laparoendosc Adv Surg Tech. 2001;11:233–237. doi: 10.1089/109264201750539763. [DOI] [PubMed] [Google Scholar]
- 6.Song JY, Rana N, Rottman CA. Laparoscopic appendicectomy in a female patient with situs inversus: case report and literature review. JSLS. 2004;8:175–177. [PMC free article] [PubMed] [Google Scholar]
- 7.Rao PG, Katariya RN, Sood S, Rao PLNG. Situs inversus totalis with calculus cholecystitis and mucinous cystadenomas of ovaries. J Postgrad Med. 1977;23:89–90. [PubMed] [Google Scholar]
- 8.Campos L, Sipes E. Laparoscopic cholecystectomy in a 39 years old female with situs inversus. J Laparoendosc Surg. 1991;1:123–126. doi: 10.1089/lps.1991.1.123. [DOI] [PubMed] [Google Scholar]
- 9.Hamdi J, Hamdan OA. Laparoscopic cholecystectomy in situs inversus totalis. Saudi J Gastroenterol. 2008;14(1):31–32. doi: 10.4103/1319-3767.37803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghosh N, Roy A, Bhattacharya SK, Mukherjee S, Saha M (2009) Laparoscopic cholecystectomy in situs inversus, a modified approach. Internet J Surg 19(2)