Abstract
Laparoscopic CBD exploration (LCBDE) is a cost effective, efficient and minimally invasive method of treating choledocholithiasis. Laparoscopic Surgery for common bile duct stones (CBDS) was first described in 1991, Petelin (Surg Endosc 17:1705–1715, 2003). The surgical technique has evolved since then and several studies have concluded that Laparoscopic common bile duct exploration(LCBDE) procedures are superior to sequential endolaparoscopic treatment in terms of both clinical and economical outcomes, Cuschieri et al. (Surg Endosc 13:952–957, 1999), Rhodes et al. (Lancet 351:159–161, 1998). We started doing LCBDE in 1998.Our experience with LCBDE from 1998 to 2004 has been published, Gupta and Bhartia (Indian J Surg 67:94–99, 2005). Here we present our series from January 2005 to March 2009. In a retrospective study from January 2005 to March 2009, we performed 3060 laparoscopic cholecystectomies, out of which 342 patients underwent intraoperative cholangiogram and 158 patients eventually had CBD exploration. 6 patients were converted to open due to presence of multiple stones and 2 patients were converted because of difficulty in defining Calots triangle; 42 patients underwent transcystic clearance, 106 patients had choledochotomy, 20 patients had primary closure of CBD whereas in 86 patients CBD was closed over T-tube; 2 patients had incomplete stone clearance and underwent postoperative ERCP. Choledochoduodenosotomy was done in 2 patients. Patients were followed regularly at six monthly intervals with a range of six months to three years of follow-up. There were no major complications like bile leak or pancreatitis. 8 patients had port—site minor infection which settled with conservative treatment. There were no cases of retained stones or intraabdominal infection. The mean length of hospital stay was 3 days (range 2–8 days). LCBDE remains an efficient, safe, cost-effective method of treating CBDS. Primary closure of choledochotomy in select patients is a viable & safe option with shorter operative time and length of stay. LCBDE can be performed successfully with minimal morbidity & mortality.
Keywords: Laparoscopy, CBD, T-tube
Laparoscopic Common Bile Duct Exploration
Introduction In the era of open cholecystectomy, open common bile duct(CBD) exploration was the procedure of choice for CBD stones. However, with laparoscopic cholecystectomy (LC) becoming the gold standard for cholelithiasis, the treatment for CBD stone has changed and various options are now available. These include Endoscopic Retrograde Cholangiopancreatography(ERCP), laparoscopic CBD exploration(LCBDE) or open CBD exploration. Laparoscopic CBD exploration has all the advantages of minimal access and is also most cost effective compared to the other options [1–3]. However, advanced surgical skills are required for the performance of the procedure. Here we present our experience of LCBDE.
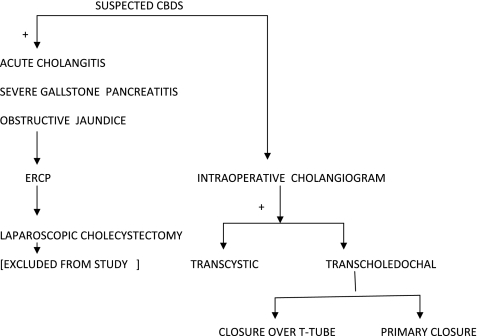
Materials and Methods From January 2005 to March 2009, 3060 laparoscopic cholecystectomies were performed. Intraoperative cholangiogram was done in 342 patients, CBD stones were present in 157 patients and 1 patient had a laparoscopically visible CBD stone so he did not undergo intraoperative cholangiogram. These 158 patients were analyzed with respect to their demographics, case records, operation notes and follow-up data. All significant complications were recorded . Complications looked for included bile leak, pancreatitis, cholangitis, T-tube problems, retained stones, urinary retention and wound infection. Our management protocol for suspected CBDS is given in Fig. 1. Intraoperative cholangiogram was performed selectively in patients with cholelithiasis as per criteria in Table 1. CBD exploration was performed either by a Transcystic approach or by a choledochotomy based on criteria in enumerated in Table 2.
Fig. 1.
Management protocol for suspected CBD stones
Table 1.
Predictors of cbd stone
| History/clinical | • Jaundice within 6 months |
| • Pancreatitis within 6 months | |
| Biochemical | • Bilirubin >10% of the normal at the higher side |
| • One or more liver function enzymes (Alkaline Phosphatase aspartate aminotransferase, alanine aminotransferase) >10% of the normal at the higher side. | |
| • Amylase >10% of the normal at the higher side | |
| Ultrasound | • Dilated CBD >7 mm |
| • CBD stone |
Table 2.
Cystic duct versus cbd approach
| Factors | Transcystic approach | Transcholedochal approach | |
|---|---|---|---|
| 1. | Number of stones | <3 | >3 |
| 2. | Stone size | <5 mm | >5 mm |
| 3. | CBD size | Any | >7 mm |
| 4. | Stone location | Distal CBD | Proximal CBD |
| 5. | Size of cystic duct | >4 mm | <4 mm |
| Failed transcystic approach |
Operative Technique
Intraoperative Cholangiogram
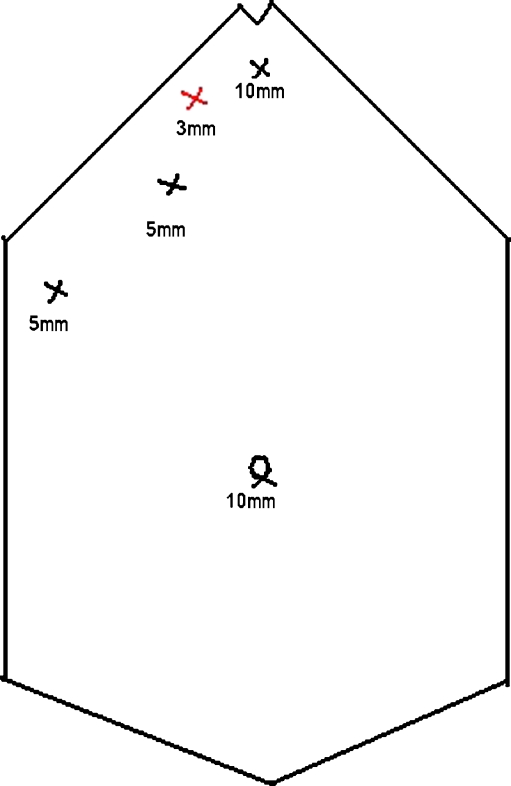
The standard 4-port configuration for LC was used. A fifth port was made, in between the right midclavicular and epigastric port just below the subcostal margin for inserting the choledochoscope if LCBDE was indicated (Fig. 2). The procedure was begun as for a standard LC. The fundus of the gall bladder was retracted towards the right shoulder and the Hartmanns pouch was retracted downwards and outwards toward the right hip. Calot’s triangle was dissected and ‘critical view of safety’ obtained. The cystic artery was clipped and divided. Then the cystic duct was milked towards the gall bladder to dislodge any cystic duct stone into the gall bladder. A clip was applied on the gall bladder side to prevent any back slippage of gallstone into the CBD and to prevent biliary spillage into the operative field. After making a small nick in the cystic duct, a ureteric catheter (4–5 Fr) or an infant feeding tube (no 5–6) after excluding air from it, was passed through the cystic duct into the CBD and a clip was applied snugly to prevent any back leakage of the contrast medium and slippage of the catheter. Dye was injected and Digital C-arm fluoroscopy provided the real time imaging of the biliary tree. In cases where the cystic duct could not be cannulated, contrast was directly injected into the CBD through a lumbar puncture needle (Fr 24) percutaneuosly. On cholangiogram, we looked for any filling defect—‘meniscus sign’, it’s size, site, number of bile duct stones, and free passage of contrast into the duodenum and for any anatomical variation of the biliary tree.
Fig. 2.
Port position for LCBDE
Transcystic Approach The catheter was removed. A guidewire was placed through the guidewire director, the director was removed and the remaining procedure was done over the guidewire. A balloon dilator was introduced to dilate the cystic duct. Then CBD stones were extracted by irrigation/suctioning, or with the help of Dormia basket/balloon catheter. A completion cholangiogram was done to confirm complete stone clearance. The cystic duct stump was closed with clips or suture ligature and the gall bladder was removed in the usual manner.
Transcholedochal Approach After opening up of the Calot’s triangle, the anterior surface of the CBD was dissected carefully and choledochotomy was performed by a longitudinal incision of 1 cm or more depending on the size of the stone with the help of endoscopic knife just below the insertion of the cystic duct into the bile duct. The stones were retrieved by spontaneous evacuation while incising the bile duct, blunt instrumental pressure with atraumatic forceps and milking, Dormia basket, Fogarty balloon catheter or irrigation and suction. Completion choledochoscopy (Fr 3.8, Olympus)was performed to assess the completeness of the procedure. Choledochotomy was closed over a t-tube with continuous 3-0 vicryl suture. Primary closure of CBD was done in cases were the ampulla was not violated and complete stone clearance was confirmed by choledochoscopy.Postoperative ERCP was done in 2 patients due to failure of transcystic approach in a non–dilated CBD. Where T-tube was placed, it was clamped on 3rd POD and patient discharged home. The tube was removed between 10th to 14th POD without a cholangiogram provided the patient had no pain abdomen,fever, nausea and vomiting and or jaundice. If the patient had any such symptom, a T-tube cholangiogram was done prior to T-tube removal. Choledochoduodenostomy was done in 2 patients as they had dilated CBD >2 cm with intrahepatic stones.A sub hepatic drain was placed in all cases which was removed on 2nd postoperative day if drain was <30 ml/ day.Patients were discharged home on the 3rd or 4th postoperative day.
Results
IOC was performed in 342 patients (11.18%) out of 3060 laparoscopic cholecystectomies. There were114 male patients and 228 patients were female. The mean age of the patient was 41 years.Of the 342 patients 157(45.9%) were detected to have CBD stones on IOC.Out of the 158 patients, USG was suggestive of CBD calculus in 74. Stones were removed either by transcystic or by choledochotomy approach as shown in Table 3. The mean duration of the procedure was 65 min (range 50–80 min).
Table 3.
Our experience
| Procedure | No. of patients |
|---|---|
| Laparoscopic cholecystectomy | 3060 |
| Intraoperative cholangiogram | 342 |
| Laparoscopic CBD exploration | 158 |
| Converted to open | 8 |
| Transcystic approach | 42 |
| Transcholedochal approach | 106 |
| Primary closure | 20 |
| T-tube | 86 |
| Post-operative ERCP | 2 |
| Choledochoduodenostomy | 2 |
We had no mortality in our series. Morbidity was 2.66%. There were no cases of pancreatitis or bile leak. 4 patients developed port site infection which settled with conservative treatment but required 2–3 days extra inpatient stay. There were no cases of retained stone on average 6 months follow up.(range 1 month–36 months). (Table 4) The mean length of hospital stay was 3 days (range 2–8 days). We encountered no major complications or mortality in our study.
Table 4.
Our complications
| Converted to open in 8 patients (5.33%) |
| Wound infection in 4 patients (2.66%) |
| No ileus |
| No pancreatitis |
| No bile leak |
| No retained stones |
Discussion
Laparoscopic cholecystectomy currently is accepted as the gold standard for surgical treatment of gallbladder disease. Open CBD exploration was the preferred approach for BDS. ERCP came & quickly established itself as a preferred method of treatment for CBD stones. But the quest for a single stage treatment and the improving skills of Laparoscopic surgeons has put LCBDE in to the reckoning and LCBDE is now one of the preferred treatment options for patients with cholecystocholedocholithiasis, when adequate expertise is available.
Choledocholithiasis is found in 10% of patients who present for cholecystectomy [1]. The various interventional options available for treatment of CBDS are pre-,intra- or post operative ERCP with/without endoscopic sphincterotomy(ES), LCBDE and open CBD exploration.
Preoperative ERCP The success rate for stone clearance is 87% to 97% but upto 25% of patients require two or more ERCP treatment [5]. The associated morbidity and mortality rates are 5% to 11% and 0.7% to 1.2% respectively.Complications of ERCP include bleeding, duodenal perforation, cholangitis, pancreatitis and bile duct injury [6].Intraoperative ERCP ± ES is another option for removal of CBDS, particularly stones in the common hepatic duct or intrahepatic system. The use of intraoperative ERCP is effective but it requires additional equipment and additional personnel [7].Postoperative ERCP is useful in patients with incomplete stone clearance or retained stones [8].
LCBDE The successful laparoscopic management of CBDS is dependent on several factors including surgical expertise , adequate equipment, the biliary anatomy and the number and size of CBD stones. Successful stone clearance rates for LCBDE range from 85% to 95% with a morbidity rate of 4% to 16% and mortality of 0% to 2% [9].Complications include bile leak and CBD stricture.A metanalysis of 1762 patients who underwent LCBDE from 19 studies worldwide showed a mean duct clearance of 80% with average morbidity of <10% (4–16%) and mortality of <1% (0–2.7%) [10].Also, Transcystic stone clearance may have a recovery very similar to laparoscopic cholecystectomy alone [11, 12] as it is a more anatomical approach. A meta analysis by Guruswamy K.S , Samraj K. in 2007 showed no statistically significant difference in any of the out comes between T-tube and primary closure of choledochotomy, apart from the hospital stay which was significantly lower in the primary closure group [10].An alternative to T-Tube is antegrade stent placement and primary closure [13]. We did antegrade stent placement in a few cases as published earlier [4]. In one patient we had an unexpected bile leak postoperatively. This and the additional cost of an upper endoscopy for stent removal after four weeks , stopped us from doing any further stenting. A recently described option to T-Tube is placement of ureteric Catheter through cystic duct which is brought out through the abdominal wall with primary closure of CBD [14].Our successful duct clearance rate is 92% with average morbidity of 2.66% and mortality 0%. This is comparable to the data seen in the meta analysis [9].Other options such as extracorporeal shockwave lithotripsy(ESWL), Laser lithotripsy and dissolving solutions such as ursodeoxycholic acid(UDCA) and methyl- tert- butyl ether(MTBE) have not gained acceptance. They have especial indications and more clinical trials in this area are required [5].
Conclusion
There are numerous options for the management of CBDS. Laparoscopic CBD exploration requires advanced surgical skills specially endosuturing. A skilled surgeon can handle most of the CBDS laparoscopically. There are specific indications for ERCP and open approaches. Ultimately the operating surgeon should decide on the appropriate approach and treatment based on his own skills, the patient condition and the availability and expertise of the endoscopist. In skilled hands, LCBDE is a safe and feasible option with the advantages of minimal access and early recovery.
References
- 1.Petelin J. Laparoscopic approach to common bile duct exploration. Surg Endosc. 2003;17:1705–1715. doi: 10.1007/s00464-002-8917-4. [DOI] [PubMed] [Google Scholar]
- 2.Cuschieri A, Lezoche C, Morino M, Croce E, et al. E.A.E.S. multicenter prospective randomized trial comparing two stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13:952–957. doi: 10.1007/s004649901145. [DOI] [PubMed] [Google Scholar]
- 3.Rhodes M, Susmon L, Cohen L, Lewis MP. Randomized trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159–161. doi: 10.1016/S0140-6736(97)09175-7. [DOI] [PubMed] [Google Scholar]
- 4.Gupta P, Bhartia VK. Laparoscopic management of common bile duct stones: our experience. Indian J Surg. 2005;67:94–99. [Google Scholar]
- 5.Shojaiefard A, Esmaeilzadeh M, Ghafouri A, Mehrabi A (2009) Various techniques for the surgical treatment of common bile duct stones: a meta review. Gasteroenterol Res Pract :1–12 [DOI] [PMC free article] [PubMed]
- 6.Tai CK, Tang CN, Ha JPY, Chau CH, Siu WT, Li MKW. Laparoscopic exploration of common bile duct in difficult choledocholithiasis. Surg Endosc. 2004;18(6):910–914. doi: 10.1007/s00464-003-8216-8. [DOI] [PubMed] [Google Scholar]
- 7.Assalia A, Gagner M, Schein M (2006) Controversies in surgery. pp 261–272
- 8.Nathanson L, O’Rourke N, Martin I, et al. Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trial. Ann Surg. 2005;242:188–192. doi: 10.1097/01.sla.0000171035.57236.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson MH, Tranter SE. All-comers policy for laparoscopic exploration of the common bile duct. Br J Surg. 2002;89(12):1608–1612. doi: 10.1046/j.1365-2168.2002.02298.x. [DOI] [PubMed] [Google Scholar]
- 10.Guruswamy KS, Samraj K. Primary closure versus T-tube drainage after laparoscopic common bile duct exploration. Cochrane Database Syst Rev. 2007;1:CD005641. doi: 10.1002/14651858.CD005641.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Meman MA, Meman MI. Laparoscopic common bile duct exploration: the past, the present and the future. Am J Surg. 2000;179:309–315. doi: 10.1016/S0002-9610(00)00346-9. [DOI] [PubMed] [Google Scholar]
- 12.Lezoche E, Pagani A, Carlei F, Felicioth F, Lomanto D, Guerrie M. Laparoscopic treatment of gallbladder and common bile duct stones: a prospective study. World J Surg. 1996;20:535–542. doi: 10.1007/s002689900083. [DOI] [PubMed] [Google Scholar]
- 13.Isla AM, Griniatsos J, Karvounis E, Arbuckle JD. Advantages of laparoscopic stented choledochography over T-tube placement. Br J Surg. 2004;91:862–866. doi: 10.1002/bjs.4571. [DOI] [PubMed] [Google Scholar]
- 14.Wei Q, Hu HJ, Cai XY, et al. Biliary drainage after laparoscopic cholecystectomy. World J Gastroenterol. 2004;10:3175–3178. doi: 10.3748/wjg.v10.i21.3175. [DOI] [PMC free article] [PubMed] [Google Scholar]