Abstract
Poor survival in pulmonary hypertension is known to be associated with unfavorable hemodynamic variables, including elevated right atrial pressure, elevated mean pulmonary artery pressure, and low cardiac index. However, the effect of plasma volume on outcome has not been evaluated. Our goal was to study the spectrum of plasma volume distribution in patients with pulmonary hypertension and to determine whether plasma volume could provide any prognostic insight in these patients.
Our pilot study comprised 11 patients (aged 46 ± 16 years; 7 women) who were undergoing pulmonary artery catheterization before vasodilator therapy. In all 11 patients, plasma volume was measured, with use of <25 μCi 131I-radioiodinated serum albumin. Patient follow-up averaged 19 months.
There were 2 deaths. The 2 patients who died had the highest right atrial pressures in the group: ≥17 mmHg. Those 2 patients also had 2 of the 3 highest plasma volumes at ≥8.4%. None of the patients underwent lung transplantation.
The propensity for elevated plasma volume and right atrial pressure in patients who died in this pilot study is consistent with the advanced right-sided heart failure that oc curs in the terminal stages of pulmonary hypertension. Elevated plasma volume may be a useful prognosticator; further studies are needed to assess whether manipulation of plasma volume affects prognosis. (Tex Heart Inst J 2003;30:305–7)
Key words: Outcome, plasma volume, pulmonary hypertension/mortality
In the course of pulmonary hypertension, there is a gradual deterioration in hemodynamics over time, and a gradual onset of right-sided heart failure with volume overload. Investigators 1 have described the hemodynamics in pulmonary hypertension and its relation to outcome. Elevated right atrial pressures have been shown to predict poor outcome in patients with pulmonary hypertension. 1 We postulated that, pathophysiologically, elevated plasma volume might also be found in those pulmonary hypertension patients who had advanced right heart failure and the poorest prognosis. Accordingly, the goal of this small pilot study was to examine the feasibility of performing plasma volume studies using iodine-labeled albumin on patients undergoing pulmonary artery catheterization, and to perform follow-up of patient outcome. Atrial natriuretic peptide (ANP), arginine vasopressin (AVP), aldosterone (PA), and plasma renin (PRA) levels were sampled at the same time.
Patients and Methods
Patients with pulmonary hypertension who were undergoing standard clinical and right heart hemodynamic evaluation of their condition were offered inclusion in this study. Exclusion criteria were lack of consent, allergy to iodine or albumin, pregnancy or lactation, and religious constraints. The study group consisted of 7 women and 4 men with a mean age of 46 ± 16 (SD) years. Six patients had primary pulmonary hypertension, 2 had scleroderma, one had sarcoidosis, one had sleep apnea with pulmonary hypertension, and one had pulmonary hypertension secondary to congenital heart disease. The duration of patient follow-up averaged 19 months. All patients gave consent in accordance with requirements of the Institutional Review Board at the Cleveland Clinic.
Venous samplings of ANP, PRA, AVP, and PA were drawn from each patient. Plasma volume, red cell mass, and hematocrit were measured at the same time. All patients were on low-sodium (2 g per day) diets.
A full hemodynamic profile was obtained for each patient with use of a pulmonary artery catheter inserted via the internal jugular vein. Right atrial, right ventricular, pulmonary artery, and pulmonary capillary wedge pressures were recorded. Cardiac output was determined by the Fick method.
Of the 11 patients, 6 were taking a diuretic and 6 were on warfarin (which was withheld before the procedure); one was on digitalis. Four were on a calcium channel blocker, 2 were on an angiotensin-converting enzyme inhibitor, one was on an angio-tensin receptor blocker, and one was on an oral nitrate.
Plasma volume was measured with <25 μCi 131I-radioiodinated serum albumin intravenously with an 11-minute equilibration period. Total blood volume was calculated from plasma volume and simulta-neously measured venous hematocrit. Values were cal culated as percentage of normal for sex to allow averaging of data obtained from men and women. Normal values for our laboratory for men are 29.4 ± 0.8 mL/cm height and for women are 23.7 ± 0.5 mL/cm height.
A short, 18- or 20-gauge intravenous cannula connected to a 3-way stopcock was used to obtain plasma venous sampling. The catheter was filled with a saline solution, with samplings performed after the patient had rested for 30 minutes in a supine position. A total of 20 mL blood was drawn from each patient and was separated into 5 plastic tubes. Plasma AVP and ANP samples were placed in pre-chilled ethyleneglycotetra-acetic acid (EGTA) tubes. Ren-in and aldosterone were assayed at the Cleveland Clinic Foundation.
Plasma volume, hemodynamic variables, and neuro-hormone levels were assessed for relationship to poor outcome (death). Due to the small sample size of this pilot, only descriptive statistics using means, standard deviations, and ranges were performed. Trends were graphically depicted.
Results
Follow-up of the 11 patients took place over an average of 19 months. None of the patients underwent lung transplantation. Two patients were subsequently hospitalized and died. The other 9 remained alive and free from hospitalization.
The mean plasma volume was −25% ± 13% of normal, with a range of −23% to 13%. The mean ANP was 115 ± 81 pg/mL; AVP, 3 ± 3 fmol/mL; aldosterone, 12 ± 11 ng/dL; and plasma renin activity, 15 ± 25 ng/dL. The mean serum creatinine was 0.8 ± 0.2 mg/dL.
The mean right atrial pressure was 11 ± 6 mmHg; mean pulmonary artery pressure, 55 ± 13 mmHg; pulmonary capillary wedge pressure (PCWP), 19 ± 14 mmHg; and Fick cardiac index, 2.0 ± 0.4 L/min/m2. The elevated PCWP was likely skewed by 2 outlying values in the group: when they were excluded, the mean PCWP was 9 ± 5 mmHg. The pulmonary vascular resistance was 9 ± 4 Wood units.
Two patients died. These patients had the highest mean right atrial pressures in the group at 17 and 18 mmHg (Fig. 1), as well as 2 of the 3 most elevated plasma volumes at 8% and 12% (Fig. 2). No trends between neurohormones and death were observed.
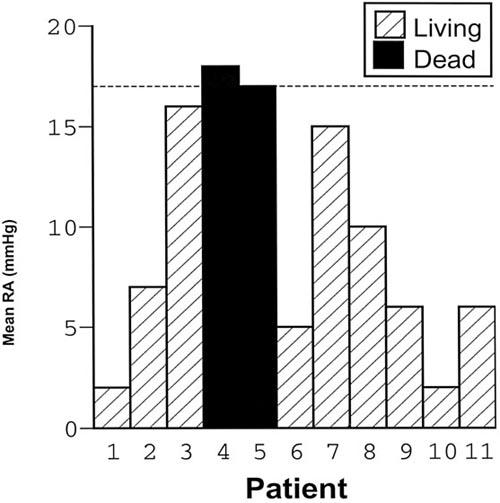
Fig. 1 Outcome and right atrial (RA) pressure.
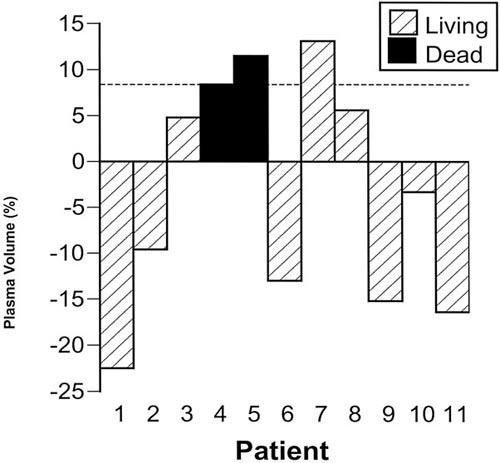
Fig. 2 Outcome and plasma volume.
Discussion
There are data from earlier investigations regarding the role of neurohormones in pulmonary hypertension. Nootens and colleagues 2 reported neurohumoral activation in right heart failure with elevated plasma norepinephrine and endothelin. Nagaya and co-authors 3 reported that, in pulmonary hypertension, plasma brain natriuretic peptide increases in proportion to the extent of right ventricular dysfunction.
Although there are data on fluid regulators in pulmonary hypertension, the actual plasma volume status in patients with pulmonary hypertension has not been well characterized. Of note, the only article pertaining to plasma volume status and pulmonary hypertension in the literature is a report on Pimelea spp. poisoning in cattle, which led to pulmonary hypertension and hypervolemia. 4 In that study, when cattle were infused with Pimelea spp., a marked expansion of plasma volume was observed, accompanied by pulmonary artery contraction.
In other cardiopulmonary conditions, more data exist with regard to volume status. In congestive heart failure, the traditional thinking has been that plasma volume is elevated due to stimulation of the renin– aldosterone system and arginine vasopressin. More recently, however, Feigenbaum and associates 5 reported that plasma and blood volumes are contracted in patients with chronic heart failure, which indicates excessive diuresis, deconditioning, or both. Plasma volume has also been studied 6 in the setting of end-stage heart failure treated by left ventricular assist devices (LVADs). After the implantation of LVADs, both plasma volume and its regulators (ANP, PA, PRA, and AVP) decreased. 6
The relationship of hemodynamic variables to outcome in pulmonary hypertension is better defined than is plasma volume to outcome. Sandoval and coworkers 1 found that increased right atrial pressure and low cardiac index are hemodynamic variables that predict poor outcome in patients with pulmonary hypertension. In our study, 2 of the 3 patients with the highest plasma volume levels died, and the 2 patients who died had the highest right atrial pressures, in keeping with earlier reports. The propensity for elevated plasma volume and right atrial pressures in pa tients with pulmonary hypertension who die is consistent with the advanced right-sided heart failure that occurs in the terminal stages of patients with pulmonary hypertension. This small pilot study is limited by sample size, but we hope that it will lead to further investigation. Elevated plasma volume may be a powerful prognostic indicator. Further studies are merited to determine whether manipulation of plasma volume affects the prognosis of patients with pulmonary hypertension.
Footnotes
Address for reprints: Karen B. James, MD, The Cleveland Clinic Foundation, Kaufman Center for Heart Failure, 9500 Euclid Avenue, Desk F25, Cleveland, OH 44195
E-mail: jamesk@ccf.org
References
- 1.Sandoval J, Bauerle O, Palomar A, Gomez A, Martinez-Guerra ML, Beltran M, Guerrero ML. Survival in primary pulmonary hypertension. Validation of a prognostic equation. Circulation 1994;89:1733–44. [DOI] [PubMed]
- 2.Nootens M, Kaufmann E, Rector T, Toher C, Judd D, Francis GS, Rich S. Neurohormonal activation in patients with right ventricular failure from pulmonary hypertension: relation to hemodynamic variables and endothelin levels. J Am Coll Cardiol 1995;26(7):1581–5. [DOI] [PubMed]
- 3.Nagaya N, Nishikimi T, Okano Y, Uematsu M, Satoh T, Kyotani S, et al. Plasma brain natriuretic peptide levels increase in proportion to the extent of right ventricular dysfunction in pulmonary hypertension. J Am Coll Cardiol 1998;31(1):202–8. [DOI] [PubMed]
- 4.Kelly WR. Pulmonary hypertension, hypervolaemia, and haemodilution in Primelea spp. poisoning of cattlea brief review. Clin Exper Pharmacol Physiol 1975;Suppl 2:163–6. [PubMed]
- 5.Feigenbaum MS, Welsch MA, Mitchell M, Vincent K, Braith RW, Pepine CJ. Contracted plasma and blood volume in chronic heart failure. J Am Coll Cardiol 2000;35:51–5. [DOI] [PubMed]
- 6.James KB, McCarthy PM, Jaalouk S, Bravo EL, Betkowski A, Thomas JD, et al. Plasma volume and its regulatory factors in congestive heart failure after implantation of long-term left ventricular assist devices. Circulation 1996;93:1515–9. [DOI] [PubMed]


