Abstract
In Buerger’s disease conservative treatment is questionable. Arterial reconstructive surgery is not feasible and sympathectomy has limited role. Progression of the disease invariably leads to amputation. Ilizarov’s method increases the vascularity of the ischaemic limb. Retrospective analysis of Ilizarov’s technique in 60 patients was done. Immediate results took into account rest pain, colour of skin, venous return, temperature, pulse oxymeter measured oxygen saturation and ulcer/amputation stump wound healing. Early and late results took into account rest pain, healing of ulcers/amputation stump with or without plastic coverage, claudication distance, resumption of previous occupation and domestic ambulation. The mean follow up of patients was 63 months. Immediate results were promising except two amputations. Early result were excellent to good in 56 and late results were excellent to good in 48 patients. Deterioration had significant correlation with smoking. Ilizarov’s method is an excellent and cheap procedure in treatment of Buerger’s disease.
Keywords: Thromboangiitis obliterans, Buerger’s disease, Ilizarov, Fixator, Neo-angiogenesis, Lateral distraction
Introduction
Buerger’s disease / Thromboangiitis obliterans (TAO) is an inflammatory disorder affecting small and medium sized arteries with unknown etiology and strong association with smoking [1]. It is a difficult disease to treat and abstinence from smoking is must to arrest the progress. Conservative treatments like vasodilators, anti- coagulants, prostaglandin therapy etc. have questionable role. Arterial reconstructive surgery is not feasible usually. Sympathectomy, though widely used works partially or not at all. Progression of the disease invariably leads to amputation [2].
In 1951, Ilizarov began to use distraction osteogenesis to treat acute fractures. Over the years, the methods and devices have evolved and its indications have been extended to treat fractures and associated complications: nonunion, chronic osteomyelitis, shortened extremity, joint contracture, and deformity [3]. In TAO affecting lower limbs a vertical osteotomised bone fragment of tibia is slowly distracted horizontally to induce neo-angiogenesis which develops an effective collateral circulation to salvage the limb [3–6]. Only osteotomy with periosteal stripping [7], revascularising osteotrepanation [8, 9] and vascular gene therapy [10, 11] are alternative promising methods.
This is a retrospective analysis of 60 patients of TAO with grade III & IV ischemia treated by Ilizarov’s technique.
Materials & Methods
From 1989 to 2006, 77 male patients with TAO grade III and IV ischemia were treated with Ilizarov’s technique. There was a loss of follow up of 17 patients who were not included in the study. The mean age of the patients at presentation was 43.22 ± 5.03( range 29–56 years). The age of disease onset was a mean of 39.37 ± 3.87 ( range 27–48 years) All were heavy smokers smoking a mean of 24.83 ± 5.37(range 15–35 bidi/cigarette) daily for more than a mean of 21.57 ± 4.35 years (range 12–35 years). 10 patients were also chewing tobacco.All patients had rest pain and intermittent claudication (claudication distance : <10 meters in 08 patients, 11–50 meters in 34 patients, 51–100 meters in 10 patients , and >100 meters in 08 patients). Non healing ulcer & varying degree of gangrene were present in 26 & 14 patients. Trophic changes were present in all.
All patients had palpable femoral pulsation and absent dorsalis pedis and posterior tibial pulsations. Popliteal pulsation were absent in 15 patients. 53 patients had some surgery earlier(below knee amputation in contralateral limb in 24, sympathectomy ipsilateral in 24, ipsilateral vascular bypass in 14, omentoplexy in one, contralateral amputation and ipsilateral sympathectomy in one, contralateral amputation and ipsilateral bypass in 8, ipsilateral sympathectomy and bypass in 2 patients). All were treated conservatively also. Inclusion criterion in the study were diagnosed cases of TAO with grade III & IV ischemia. Patients with diabetes mellitus, immuno- compromised state & on long term steroid therapy were excluded. Routine blood investigations, radiographs and femoral arteriogram done pre-operatively. Femoral arteriogram confirmed complete blocks at lower femoral in 6, upper popliteal in 4, lower popliteal in 32 and anterior / posterior tibial in 18 patients. All were counselled to give up tobacco.
Operative Technique
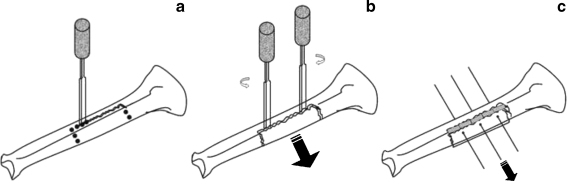
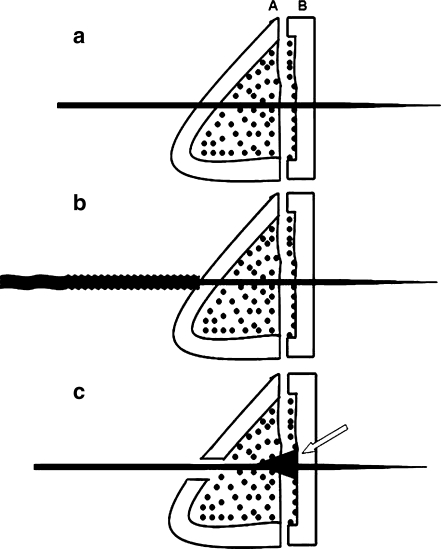
Pre-constructed Ilizarov’s frame with two full rings and lateral distraction assembly were made according to size and side of the leg.All were operated under spinal or general anaesthesia in supine position without tourniquet. The pre-constructed frame was fixed with two olive wires in each upper and lower ring in such a way that they rest just below tibial tuberosity and at supramalleolar level respectively. The olive wires inserted as per goniometric atlas, following the safe zones. 120 pounds of tension applied to each wire before fixing. Through an anterior approach to tibia the skin & periosteum is incised and periosteum stripped. Multiple drill holes are made with a drill hole zig, 0.5 cm medial to the anterior margin of the tibia. Both anterior and posterior cortex are drilled and holes are also made on the lateral surface of tibia at ends of the corticotomy. A 5 mm osteotome/corticotome is used to complete the osteotomy(Fig. 1a, b). Care is taken to prevent fracture. Three parallel k-wires are passed through the tibia and osteotomised fragment and then replaced by olive wires sequentially after overdrilling (Fig. 2). These wires are fixed to the lateral distraction device. After 7 days of waiting period, lateral distraction (Fig. 1c)at the rate of 0.25 mm 6 hourly is done for 20 days to achieve a distraction of 2 cm. Regular dressing is done and stitches removed at 10 days. If the gangrene is not infected then we wait till demarcation is complete before doing an amputation and if infected then guillotine amputation is done primarily. With index surgery 10 forefoot & 04 hindfoot amputations and after one week 8 forefoot and 4 hindfoot amputations done. Debridement of ulcers done regularly and raw area grafted later.
Fig. 1.
a Drill holes made with zig is connected with osteotome to complete the osteotomy anteriorly and laterally. b Twisting of the osteotomes in opposite direction to complete the osteotomy posteriorly. c The osteotomised fragment laterally pulled with neo-histeogenesis inbetween and around it
Fig. 2.
a K wire passed from medial to lateral side in the middle of tibia (through the parent tibia[A] and the osteotomised fragment [B]) parallel to floor. b Over drilling over the K wire, medial cortex only,with a cannulated cancellous drill bit to make way for the bulbous olive of the olive wire. c Olive wire replaces k wire. The olive bulb of the olive wire rests at the endosteal surface(block arrow) of osteotomised fragment of tibia
Physiotherapy and full weight bearing with stick support was advised. Radiographs taken postoperatively and every 6 weeks till removal of frame. Femoral arteriogram was done in few cases at 4th week postoperatively as per the monetory status of the patient. After 2.5 to 3 months the Ilizarov assembly is loosened and patient allowed to walk for 2 weeks to check the consolidated tibial strength. Fixator assembly then removed without anaesthesia. A patellar tendon bearing brace / cast is given for 4 weeks.
Antibiotics were given and analgesics like paracetamol & Tramadol were used and avoiding NSAID’s because of their anti-inflammatory action, which hampers neovascularisation.
Statistics
Descriptive statistics( mean,range,standard deviation ) were calculated for different values. Chi-square test for checking significance of association between attributes with p value for smoking.
Results were assessed as immediately (within 4 wks) ,early (at 6 months)and late (at final follow up). Immediate results took into account rest pain, colour of toe pulp/nailbed, temperature, pulse oxymeter measured oxygen saturation and ulcer/amputation stump wound healing. Early and late results were assessed by taking into account rest pain, healing of ulcers/amputation stump with or without plastic coverage, claudication distance,resumption of previous occupation and domestic ambulation.
Excellent
No rest pain, healed ulcers or amputation stump ,no claudication, resumption of previous occupation and unaffected domestic ambulation.
Good
Absence of rest pain, healed ulcers or amputation stump, claudication distance of 1–2 kms, but able to continue previous occupation and domestic ambulation affected sometime.
Fair
Absence of rest pain, persisting / recurrent ulcers, claudication distance of < 1 km, change to alternative occupation and affection of routine domestic ambulation.
Poor
Major amputation was necessitated.
Results
The mean follow up of patients was 5.4 (range 2–11 years). Early results showed rest pain disappearance by 2nd week in 45 and by 4th week in 13. The need for analgesia in all reduced after 2 days. Skin warmth , colour of toe pulp/ nailbed improved in all by 10 days. All patients with ulcer / gangrene showed signs of healing by 2 weeks. Oxygen saturation also improved in all. Early results were excellent in 42, good in 14 , fair in 2 and poor in 2 and late results were excellent in 34 (Figs. 3 and 4.), good in 14 , fair in 6 and poor in 6 patients.
Fig. 3.
a Operated sympathectomy patient (black arrow). b Infected gangrene of toes operated amputation. c Absent flow in femoral arteriogram beyond mid femoral artery. d Operated with Ilizarov technique. e Healed amputation stump. f, g, h Developed extensive collateral circulation(white arrows)beyond obstruction with consolidating osteotomy of tibia(black arrow) at 4 months
Fig. 4.
a Developing dry gangrene of great toe. b, c, d Femoral arteriogram showing no flow beyond popliteal artery. e, f With Ilizarov frame healing raw area, no gangrene progression and establishing collateral circulation that has reached upto ankle (white arrow) with distraction at corticotomy site (black arrow) seen in femoral arteriogram done at three weeks post operative. g healed amputed great toe stump at final follow up
Complication of pin tract infection (superficial 14 / deep 4 ) cleared with dressing and antibiotics . Stitch necrosis occurred in 10 patients healed eventually. Protruded bone block in 4 patients necessitated removal (Fig. 5). Peroperative fracture in tibia in 2 united by adding another ring and keeping the frame for 6 weeks more. Two patients showed progressive infection and gangrene leading to amputation.
Fig. 5.
a Consolidated excess new bone that formed in a patient because he continued distraction for 35 days instead of 20 days. b Infection with bone block protrusion c Managed with debridement and “shaving off” of the block that healed eventually
Discussion
TAO is a segmental, inflammatory, nonatherosclerotic occlusive disease of small and medium arteries described by Felix Von Winiwarter (1879) and Leo Buerger (1908), there after commonly called Buerger’s disease [1, 2].
It is common in asia, the middle east and eastern europe, but rare in north america and western europe [2, 12]. Though, frequently reported from India, no statistics are available [2].
The etiology is unknown but strongly associated with tobacco. Nearly 40% who continue smoking need amputation as opposed to 5% who abstain. Female affections is increasing with smoking [2, 12–15].
All our patients were heavy smokers.Genetic factors, Cell mediated immunity, HLA predisposition, autoantibodies, low socioeconomic status and poor work environment have been incriminated in etiology [2, 15].
Histopathological findings vary according to the duration [2, 13]. There are interposed segments of affected veins and arteries with normal segments. In acute phase a pan vasculitis develops with occlusive highly cellular thrombus with microabscesses and multinucleated giant cells. In intermediate phase progressive organization occurs. In end-stage there is fibrosis and recanalisation [2, 13, 14].
Diagnostic criterion is mainly clinical. Shionoya’s criterion for diagnosis includes a smoking history, onset before the age of 50 years, infrapopliteal arterial occlusions, either upper limb involvement or phlebitis migrans and absence of atherosclerotic risk factors other than smoking. Arteriographic findings are supportive and histopathological finding corroborate its existence [2].
All our patients were already diagnosed as TAO and were transferred from surgical departments and fitted into Shionoya’s criterion.
Olin’s criteria includes additionally exclusion of other vascular disease [15].
Onset is around 40 years with ischaemia developing distally and progressing proximally. Patients present with claudication, rest pain, ulcer, gangrene, cyanosis or Raynauds phenomena. Mesentric, coronary, cerebral arterial involvements have been reported. Trophic changes like thickened nails, shrunken digits, loss of hairs and inter digital fungal infection may be present. Edema is usually present to get relief of pain by dependency. Differential diagnosis from atherosclerotic obliterans is clinical. There are periods of exacerbations and remissions related to smoking [2, 12, 15].
Segmental arterial pressure measurements are normal above and markedly reduced distally. Monitoring of ankle and toe pressures, plethysmography and digital artery flow velocity may have practical value. Thallium 201 perfusion scan are helpful in determining healing potential of ulcers and in documenting the response to therapeutic intervention [2, 15].
Colour doppler is a noninvasive method for assessment of distal flow. Echocardiography and ultrasonography of aorta can rule out proximal source of emboli. ESR, CRP, antivascular antibody, rheumatoid factor, complement levels etc. are helpful to exclude other causes of vasculities. CBC, antithrombin III, antiphospholipid antibodies, factor assays, PT and aPTT can exclude hyper coagulopathies [2, 15].
Characteristic arteriographic findings in TAO shows skip lesions with normal proximal arteries, “corks screw” collaterals following the course of thrombosed vessel (martorell’s sign) [16].
Treatment of TAO needs a thorough understanding of the pathogenesis, and has remained enigmatic. Complete abstinence from smoking is critical for success of available therapy [2, 12]. Early treatment is also important to avoid social problems and improve quality of life [17].
The treatment goals include improving arterial flow, alleviating rest pain and improving claudication distance, healing of ulcers/ wounds and limiting the level of amputation in developing gangrenes.
Medical therapy is questionable [2]. Vasodilator therapy is not effective because of non selective vasodilatation, though intravenous ilioprost has been claimed to be effective [18]. Intra-arterial thrombolytic therapy has been tested in acute exacerbation with some success [19].
Despite the clear presence of inflammation, NSAID’s or steroids have no role. Counselling is must for stopping tobacco use, protection of foot from thermal chemical and mechanical trauma [2].
Sympathectomy removes the vasoconstrictor tone improving blood flow and promoting ulcer healing and improving pain [2, 12, 15, 20]. But,it does not increase flow to ischemic muscles and thus no improvements occur in claudication distance. Its long term role in chronically dilated ischaemic vessls is also questionable [2, 20].
Direct revascularization surgeries are not possible due to diffuse involvement and absence of distal target vessel [2, 12, 15, 21]. Graft failure is high [22] but can be attempted with impending gangrene and a target vessel [23]. Profoundoplasty has been done with some success especially with adequate ankle flow [24].
Revascularizing osteotrepanation is a newer method with promising results in grade II b ischemia [8, 9]. Its long term results are awaited.
Omentopexy is an attractive option [25]. But, it needs proper mobilization of omentum by experts and more surgical time, increasing complications. Prolonged ileus, wound infection, closure difficulties and hernia have been reported [25].
Vascular gene therapy may be useful by inducing angiogenesis using vascular endothelial growth factor or basic fibroblast growth factor [10, 11]. But its cost and availability to commonly affected poor patients remains to be seen.
Ilizavor’s technique is very effective to induce neoangiogenesis in TAO [3–6]. According to Ilizarov, gradual traction on living tissues can stimulate and maintain regeneration and active growth of tissues (bone, muscle, fascia, nerve, vessels, skin, and its appendages). This is called the “law of tension stress”. The quality and quantity of histiogenesis depends upon : 1) the rigidity of bone fixation , 2 ) the degree of damage at the time of corticotomy , 3) the rate of distraction [3]. Ilizarov’s apparatus should be stable which can be achieved with two full rings tightly connected to each other with threaded rods and to the tibia with tensioned olive wires. By increasing or decreasing the rate, poor response is expected-a non union or early consolidated union may occur. By following all these principles and techniques, patients can be mobilized weight bearing from the next postoperative day. A latent period of 7–10 days is the period given before starting the distraction and during this period an organized inflammation sets in [3].
In a series of 28 patients [4] of operated Ilizarov technique, immediate and late good results were noted in 20 and 18 patients. 2 patients had fractures of tibia during operative intervention and 4 had purulent infection or skin necrosis complication. In another long term result follow up Fokin et al. [5] reported 94.2% positive result out of 125 patients treated. They also used additionally lumbar sympathectomy and arterial reconstruction in 41 and 16 patients. Fokin et al conveyed that in grade IV ischaemia, late appearance of revascularization and possibility of temporary deterioration should be kept in mind. With this method aggravation of necrotic process, postoperative arterial spasm and thrombosis, excess rate of bone split distraction and wrong choice of level of osteotomy were the main cause of unsatisfactory outcomes. Chaudhary et al. [6] operated 31 patients, 27 had prolonged and dramatic relief. 2 patients had failure and needed major amputation and 2 had partial relief. They used modified crossed wire technique for pulling of osteotomy fragment instead of olive wire which are more easily removed than olive wires.
In our series of 60 patient with follow-up the immediate results were very encouraging (58) 96% of patients showed disappearance of rest pain (Fig. 6), improved skin warmth, colour and wound / ulcer healing. 2 patients with uncontrolled infection and progressive gangrene ended up with BK amputations. Claudication distance was not taken into account in early results because, with the fixator patients have some pain in walking so, correct assessment cannot be done. Early and late results took into account rest pain amputation stump / ulcer healing, claudication distance, resumption of previous occupation and domestic ambulation. 56 (93.6%) patients showed excellent to good result. Only 2 (3.3%) patients had fair result and 2 patients (3.3%) had failure of treatment. Pin tract infection epidermal edge necrosis were minor complication that responded to conservative approach. Protruded bone block in 4 patients needed surgical removal. Fracture tibia can be avoided by sound technique. Two of our initial patients(during early learning curve) developed fracture that remained stable with an additional full ring and healed adequately in due course of treatment. The frame was left for another 6 weeks to allow consolidation. Following these we started using a special drill guide zig for controlled planned osteotomy. The calculated p-value by chi-square test less than 0.01 suggests highly significant association between smoking and deterioration of results.
Fig. 6.
Operated patients have dramatic pain relief of rest pain as evident in these smiling patients operated in a fortnight
Corticotomy near major neurovascular bundle only without fixation/distraction, with whole length tibial periosteal stripping has also promised good results using the principles of inflammation. It was used in TAO, ASO and diabetes [7].
Conclusion
TAO is grave problem faced by poor patients of developing and underdeveloped countries, with diagnosis and treatment still obscure. Ilizarov’s method is a low cost technically simple procedure, with excellent results in grade III and IV limb ischaemia and can be done in small operative setups in our country. Long term prospective randomized controlled trials are needed to establish this procedure as the first line treatment. Results of newer promising modalities are awaited. Till then, the quest for an ideal treatment of this enigmatic limb threatening condition will continue.
References
- 1.Buerger L. Thromboangiitis obliterans: a study of the vascular lesions leading to pre-senile spontaneous gangrene. Am J Med Sci. 1908;136:567–580. doi: 10.1097/00000441-190810000-00011. [DOI] [Google Scholar]
- 2.Shionoya S. Buerger’s disease (Thromboangiitis Obliterans). Vascular surgery, vol I. 4. Philadelphia: RB Rutherford, WB Saunders; 2010. pp. 235–245. [Google Scholar]
- 3.Illzarov GA. The tension—stress effect on the genesis and growth of tissues. Transosseous osteosynthesis: theoretical and clinical aspects of the regeneration and growth of tissue. Berlin: Springer; 1992. pp. 137–256. [Google Scholar]
- 4.Fokin AA, Verbovetskii LP, Fokin AA, Kulak AN (1990) The effectiveness of G.A. Ilizarov’s method in treating patients with III – and IV – stage chronic ischemia of the lower extremities [Article in Russian]. Vestn Khir Im I I Grek Nov (11):15–20 [PubMed]
- 5.Fokin AA, Fokin AA Jr, Verbovetskii LP (1993) Short and long – term results of non – standard revascularization of the lower extremities [Article in Russian] Grud Serdechnososudistaia Khir, Jul–Aug; (4):23–28 [PubMed]
- 6.Chaudhary M, Chaudhary P, Chaudhary MR (2006) Buerger’s disease—its management by bone widening technique of Ilizarov. Recent advances in surgery, Roshan Lal Gupta, Jaypee Brothers, New Delhi (8) 259–271
- 7.Bharat R, Kelkar BR. Induced angiogenesis for limb ischemia. Clin Orthop. 2003;412:234–240. doi: 10.1097/01.blo.0000072461.53786.4d. [DOI] [PubMed] [Google Scholar]
- 8.Zusmanovich FN (1996) The Treatment of Obliterans arterial diseases of the extremities by a revascularizing osteotrepanation method [Article in Russian] Khirurgila (Mosk) (6):34–36 [PubMed]
- 9.Obraztsov AV, Kokhan YP, Zavarina IK, Mitroshin GY, Kozyavkin VV, Rzyanin AV. The pathogenetic aspects of revascularization osteotrepanation. J Ang Vasc Sug. 2000;6(1):21. [Google Scholar]
- 10.Chelboun JO, Martins RN. The development and enhancement of the collateral circulation in an animal model of lower leg ischaemia. Aust N Z J Surg. 1994;64(3):202–207. doi: 10.1111/j.1445-2197.1994.tb02179.x. [DOI] [PubMed] [Google Scholar]
- 11.Isner JM, Pieczek A, Schainfeld R, Blair R, Haley L, Asahara T, et al. Clinical evidence of angiogenesis after arterial gene transfer of phVEGF165 in patient with ischaemic limb. Lancet. 1996;348:370–374. doi: 10.1016/S0140-6736(96)03361-2. [DOI] [PubMed] [Google Scholar]
- 12.Olin JW, Young JR, Graor RA, Ruschhaupt WF, Bartholomew JR. The changing clinical spectrum of thromboangiitis obliterans (Buerger’s disease) Circulation. 1990;82(IV):3–8. [PubMed] [Google Scholar]
- 13.Kurata A, Franke FE, Machinami R, Schulz A. Thromboangiitis obliterans: classic and new morphological feature. Virchows Arch. 2000;436:59–67. doi: 10.1007/PL00008199. [DOI] [PubMed] [Google Scholar]
- 14.Shionoya S, Leu HJ, Lie JT. Buerger’s disease(Thromboangiitis obliterans) In: Sstehbens W, Lie J, editors. Vascular pathology. London: Champan & Hall Medical; 1995. pp. 657–678. [Google Scholar]
- 15.Olin JW. Thromboangiitis obliterans (Buerger’s disease) N Engl J Med. 2000;343:864–869. doi: 10.1056/NEJM200009213431207. [DOI] [PubMed] [Google Scholar]
- 16.Suzuki S, Mine H, Umehara I, Yoshida T, Okada Y. Buerger’s disease (Thromboangiitis obliterans): an analysis of the arteriograms of 119 cases. Clin Radiol. 1982;33(2):235–240. doi: 10.1016/S0009-9260(82)80068-8. [DOI] [PubMed] [Google Scholar]
- 17.Ohta T, Ishioashi H, Hosaka M, Sugimoto I. Clinical and social consequences of Buerger disease. J Vasc Surg. 2004;39(1):176–180. doi: 10.1016/j.jvs.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Fiessinger JN, Schafer M. Trial of Ilioprost versus aspirin treatment for critical limb ischaemia of thromboangiitis obliterans. The TAO study. Lancet. 1990;10:555–557. doi: 10.1016/0140-6736(90)90346-7. [DOI] [PubMed] [Google Scholar]
- 19.Hussein EA, Dorri A. Intra-arterial streptokinase as adjuvant therapy for complicated Buerger’s disease: early trials. Int Surg. 1993;78:54–58. [PubMed] [Google Scholar]
- 20.Chander J, Singh L, Lal P, Jain A, Lal P, Ramteke VK. Retroperitoneoscopic lumbar sypathectomy for buerger’s disease: a novel technique. J Soc Laproendosc Surg. 2004;8(3):291–296. [PMC free article] [PubMed] [Google Scholar]
- 21.Lazarides MK, Georgiadis GS, Papas TT, Nikolopoulos ES. Diagnostic criteria and treatment of Buerger’s disease: a review. Int J Low Extrem Wounds. 2006;5(2):89–95. doi: 10.1177/1534734606288817. [DOI] [PubMed] [Google Scholar]
- 22.Sasajima T, Kubo Y, Inaba M, Goh K, Azuma N. Role of infrainguinal bypass in Buerger’s disease: an eighteen – year experience. Eur J Vasc Endovasc Surg. 1997;13(2):186–192. doi: 10.1016/S1078-5884(97)80017-2. [DOI] [PubMed] [Google Scholar]
- 23.Izumi Y, Sasajima T, Inaba M, Morimoto N, Goh K, Kubo Y. Results of arterial reconstruction in Buerger’s disease. Nippon Geka Gakkai Zasshi. 1993;94:751–754. [PubMed] [Google Scholar]
- 24.Talwar S, Jain S, Porwal R, Laddha BL, Prasad P. Pedicled omental transfer for limb salvage in Buerger’s disease. Int J Cardiol. 2000;72:127–132. doi: 10.1016/S0167-5273(99)00179-5. [DOI] [PubMed] [Google Scholar]
- 25.Hoshino S, Nakayama K, Igari T, Honda K. Long term results of omental transplantation for chronic occlusive arterial diseases. Int Surg. 1983;68(1):47–50. [PubMed] [Google Scholar]