Abstract
Chronic venous insufficiency is a common problem leading to varicose veins of lower limbs which was traditionally being treated with ligation and stripping. Endovenous ablation is an attractive alternative minimally invasive technique to treat such patients. We analysed the results of 100 consecutive patients treated with Radiofrequency based endovenous ablation using Closure Fast Catheter. Retrospective analysis of 100 consecutive patients with chronic venous insufficiency treated at our institution was done. All patients were classified pre and post procedure based on clinical, etiologic, anatomic and pathophyslogical classification, Venous clinical severity and Venous disablitity scores alongwith color doppler examination with follow up done at 2 weeks, 3 months and one year for any disease recurrence or residual symptoms. 97 of the 100 patients treated at 3 months and at 1 year showed good reduction of venous clinical severity and Venous disability scores to 0. Doppler showed complete closure of saphenofemoral junction and long saphenous vein at 2 weeks with no recanalisation at one year. No thrombus formation was observed. Minor complications like ecchymosis was seen in 9 patients and thrombophlebitis in 4 patients. Endovenous ablation using radiofrequency with Closure Fast technique showed improved short and long term results in patients with venous insufficiency with 100% closure seen on doppler studies along with lesser complications and no thrombus formation due shortened procedure time and improved catheter design.
Keywords: Varicose veins, Endovenous ablation
Introduction
Chronic venous insufficiency of the lower limbs is a common condition afflicting 25% of women and 15% men with the venous reflux at the the saphenofemoral junction(SFJ) being the most common cause leading to varicose veins [1]. The traditional treatment of venous insufficiency has been ligation and stripping of the long saphenous vein (LSV) followed by removal of varicose veins. Endovenous ablation (EVA) using radiofrequency (RF) was introduced as an alternative to the traditional surgery in clinical practice world wide in 1998-1999 [2, 3, 4] and since then has been a established procedure. Since the last two years there have been changes in the technology related to the use of RF catheter and has led to the introduction of one such catheter by the name of Closure Fast TM.
We retrospectively analysed the data of 100 consecutive patients of Chronic saphenofemoral insufficiency treated at our institution along with one year follow up details to determine the efficacy of the use of new RF catheter system and determined both short term and long term outcome alongwith its complications to determine the success this technique.
Patient and Methods
We retrospectively analysed the records of 100 consecutive patients of chronic saphenofemoral insufficiency who underwent EVA using RF with Closure Fast catheter between 2007-2008. Details of follow up done 2 weeks, 3 months and 1 year were also analysed. All patients had symptomatic varicose veins and the inclusion criteria for the study was based on the CEAP(clinical, etiologic, anatomical, pathophysiology) classification. All patients with C1-C4 disease ie C1: spider veins, C2, varicose veins, C3 ankle edema and C4 lipodermatitis, C5 with old healed ulcer were included in the study. The diagnosis was based on both clinical and color Doppler examination. Doppler was done on Acuson Cyprus ( Siemens, Erlangen Germany AG) system. Patients which showed a venous reflux of duration of 0.5 seconds in the long saphenous vein were included in the study. All patients in C6 category of CEAP i.e with active venous ulcer , patients with post thrombotic etiology Pr or O + R were excluded . VCSS and VDS scores were then determined for each patient. For VCSS 10 characteristic features were determined on a scale of 1–3 i.e mild, moderate and severe and the score added with maximum being 30. There characteristics were: pain, varicose veins, venous edema, pigmentation,inflammation, induration, fatigue, cramps, compression use and overall response. The VDS 3 characteristics were determined on a scale of 0–3 with 0 being asymptomatic, 1 symptomatic but able to carry usual activity, 2 carrying activity but with compression and 3 , unable to carry activity with compression. Follow up clinical and Doppler examination was done at 2 weeks, 3 months and 12 months to determine both short and long term outcome and the final VCSS and VDS scores estimated at the end of one year. Any patient with recanalisation of closed vein, recurrent reflux or neovascularisation was particularly recorded.]
Procedure: Was done on Vnus RF system using Closure Fast TM catheter( San Jose, California, USA) using 6-7 F catheters of 80 cm length. Patient was made to lie supine and the lower limb prepared and draped under aseptic conditions. The LSV and the SFJ were mapped under US guidance and the point of venous access determined around the knee joint. Access was obtained with 18 G puncture needle using 1% Xylocaine as local anesthetic. A 7-8 F venous catheter sheath was introduced over a 0.18 guidewire. Under ultrasound (US) guidance the Closure catheter was then inserted through the sheath and parked 1–3 cm proximal to SFJ. Tumescence anesthetic saline was infiltrated around the vein in the saphenous fascial compartment. The RF ablation was then started and in incremental steps of 7 cm with tip temperature of 120°C at 15 KW till the total length of LSV was closed till the knee joint . The catheter and the sheath were then withdrawn and the access site closed with a steristrip and compression bandage applied alongwith a compression stocking for a period of 2 weeks. The patient was made ambulatory immediately and discharged.
Follow up examination was done at 2 weeks, 3 months and 1 year with clinical and Doppler along with a 15 point questionare filled by the patient as to how he felt, his ability to carry on his daily routine and symptoms if any. Ambulatory phlebectomy if required was used as adjunctive procedure at 2 weeks if there were any residual varicosities which were deemed as unacceptable to the patient on cosmetic grounds.
Results
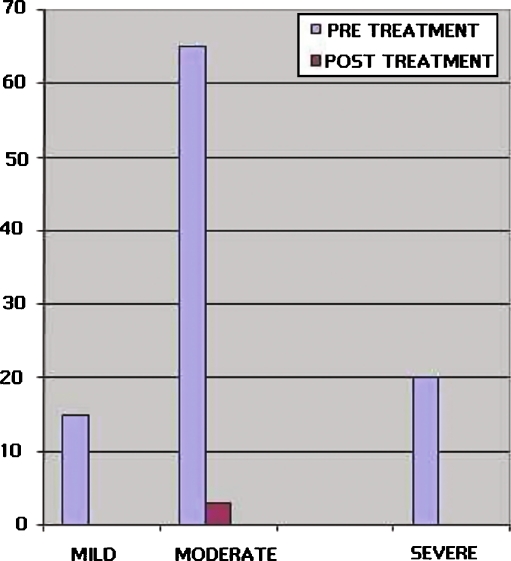
Retrospective analysis of data of 100 consecutive patients with SFJ incompetence who underwent RF ablation was done. Out of these, 68 patients were females and 32 males between the age group of 28 to 79 years with mean age group of 42 +/- 10.5 years for males and 41.4 +/- . 9.5 years for females. All patients were symptomatic for their venous problems with or without skin changes with the majority in the C2 group of CEAP i.e 48 patients, followed by C3 and C4-5 group 28 and 24 respectively (Table 1). The mean length of the treated LSV segment was 40 + - 5 cm( range 20 to 60 cm ). Branch reflux was seen in 12 patients and these were treated separately. The venous clinical severity scores are enumerated in Chart 1 with the largest number of patients seen in the moderate group with mean score of 16 in 65 patients followed by 20 patients in severe group with score 26 and 15 patients in the mild group with score of 7. Post treatment VCSS assessment was done at 3 months and showed significant reduced scores to 0 in 97 patients with only 3 patients having a score of 11( Chart 1, Figs. 1a, b, 2a, b). The third classification used was of Venous disability score (Chart 2) which showed that the maximum number of patients ie 53 patients had a moderate disability score of 2 followed by 34 patients in group 3 and 11 patients had a score 1. Post treatment at 3 months showed 95 patients were having VDS 0 and 5 had score 1 (Fig. 3a, b) , with only 3 patients out of these 5 patients having mild paresthesias, intermittent swelling and spider veins at 1 year follow up. The complications observed at 2 weeks follow up are enlisted in (Table 2). the most common being paraesthesia in saphenous distribution in 9 patients followed by ecchymosis , bruising in 7 (Fig. 4a) and thrombophlebitis in distal varicosities in 4 patients (Fig. 4b). Doppler examinations done at 2 weeks, at 3 months and at 1 year showed complete vein closure in 97% patients (Fig. 5a, b) while in 3 patients there was some flow seen across SFJ for a distance of 1-2 cm with no reflux. 1 patient showed neovacularisation and in another patient a denovo reflux was seen in the anterolateral vein which opened separately into the common femoral vein.
Table 1.
Demographic data of closure fast patients
| S.NO. | Variable | Male | Female |
|---|---|---|---|
| 1 | Number | 32 | 68 |
| 2 | Mean age | 42 | 41.4 |
| 3 | Mean weight | 78 kg | 65 kg |
| 4 | C2(CEAP) | 8 | 40 |
| 5 | C3 | 10 | 18 |
| 6 | C4-5 | 14 | 10 |
| 7 | Mean length of LSV treated | 40 cm | 40 cm |
Chart 1.
Chart showing Pre and post treatment VCSS scales
Fig. 1.
a Patient in C2 (CEAP) group I VCSS 4, VDS 1 showing multiple varicose veins. b Post EVA showing resolution of varicosities with C0, VCSS and VDS 0 status
Fig. 2.
a A pretreatment C3, patient Group II VCSS 12 and VDS 2 with Chronic venous insufficiency. b Post treatment status at 2 weeks with C0, VCSS and VDS o status
Chart 2.
Chart showing pretreatment and post treatment VDS scales
Fig. 3.
a, b Pre and post treatment improvement from VDS3 to VDS o
Table 2.
Table of complications in patients with EVA using closure fast
| S.NO. | Complications | Number |
|---|---|---|
| 1 | Saphenous paraesthesias | 9 |
| 2 | Ecchymosis | 7 |
| 3 | Thrombophlebitis | 4 |
| 4 | Thermal injury | 0 |
| 5 | Hematoma | 0 |
| 6 | Vein perforation | 0 |
| 7 | Thrombus formation | 0 |
Fig. 4.
a Post EVA treatment ecchymosis in the mid thigh. b Post EVA patient showing thrombophlebitis in the 2nd week
Fig. 5.
a, b Color Doppler study showing pretreatment reflux and post treatment complete closure at the SFJ
Ambulatory phlebectomy was done in 18 patients at 2 weeks and in 9 patients concomitant with LSV closure RFA was done for incompetent perforators.
Discussion
EVA of SFJ and LSV has been shown to be an alternative treatment option to venous stripping which leads to a painful and prolonged post operative recovery with high incidence of hematoma formation, nerve injury and infection [4, 5]. EVA is a minimally invasive procedure and can be done using a Laser or RF. Earlier studies using RF comprised of slow incremental pull back catheter technique which had a higher incidence of clot formation, early vessel recanalisation and thermal injury and the overall reported success in different studies was between 83–100% [6] which was similar or slightly less than laser technique. The present study shows improved results leading to good venous closure with minimal complications using the new closure fast technique which offset the limitations of previous RF technique alongwith improved patient comfort. The present technique did not require the use of any post procedure analgesics with the patient being ambulatory the same day which was a great advantage for early patient recovery. Merchant et al. [6] suggested that the pull back speed in the older RF technique was a strong determinant in the success of the venous closure as it determined the amount of thermal dose received by the vessel wall. We suggest that there are two more factors which lead to improved vein closure with Closure fast and these are increased thermal dose from 90 C to 120 C and secondly improved segmental contact with vessel wall of the FAST catheter compared to conventional Closure catheter. VCSS and VDS scores at 12 days, 3 months and 1 year also showed a significant reduction in scores from 7,16,26 to 0 in 97 patients (p < 0.001) for VCSS and for VDS from 3,2 in 95 patients to 0 thus showing an excellent symptomatic recovery in the present study. These results are quite similar to those shown in RECOVERY trial [7] completed on 65 patients in 2009. The latter study also showed superior results of the new technique over EVA using Laser with reduced rate of minor complications and improved VCSS and QOL scores at 2 weeks and at 23 days. Our study did not observe any thrombus formation formation in the LSV nor any projecting thrombus in common femoral vein the cause being significantly reduced procedure time, less duration of catheter insertion and improved collagen shrinkage of vessel wall resulting in 100% closure rate of the vessel. Similar results have also been recently reported by Markovic etal [8] with a closure rate of 100%. Our study shows a 1% neovascularisation rate and 0% recanalisation at one year follow up while the results by open surgical technique have shown to have a higher recurrence rates varying from 10–48% and in a recently published Indian study done by Kompally et al. 2009 [9] they were 12.9% which are significantly higher than the results of present study. EVOLEeS [2] trial showed a neovascularisation rate of 3% with conventional closure technique and 17% with stripping. The present technique also has a positive potential on the overall cost of treatment because of the immediate ambulation compared to more than 2 weeks of no work and hospitalisation by doing a traditional surgery [10]. 95% patients in the present study returned to normal activities within one day of the closure fast procedure; this outcome was observed to be even better than that shown by EVOLVeS [2] using the conventional closure technique where 80% patients resumed their activity after 24 hours of procedure compared to only 47% by stripping.
To conclude RFA with Closure Fast technique is a safe promising tool in the treatment of SFJ and LSV insufficiency and one year follow up results show high efficacy of its use in treating such patients with 100% closure of venous incompetence with good relief of symptoms with correction of VCSS and VDS scores at 3 months with no recurrence of reflux or symptoms at one year followup alongwith quick resumption of daily activities within one day of procedure.
References
- 1.Callan MJ. Epidemology of varicose veins. Br Journal of Surgery. 1994;81:167–173. doi: 10.1002/bjs.1800810204. [DOI] [PubMed] [Google Scholar]
- 2.Lurie F, Creton D, Elkof B, Kabnick, et al. Prospective Randomised study of endovenous radiofrequency obliteration(Closure procedure) versus ligation and stripping in a selected population (EVOLVeS study) J Vas Surg. 2003;88:207–214. doi: 10.1016/S0741-5214(03)00228-3. [DOI] [PubMed] [Google Scholar]
- 3.Wagner WH, Levin PM, Cosman V, Lauterbach SR, Jl C, Farher A. Early experience with radiofrequency ablation of the greater saphenous vein. Ann Vasc Surg. 2004;18:42–47. doi: 10.1007/s10016-003-0095-x. [DOI] [PubMed] [Google Scholar]
- 4.Dietzek AM. Endovenous radiofrquencly ablation for treatment of varicose veins. Vascular. 2007;15(5):255–61. doi: 10.2310/6670.2007.00062. [DOI] [PubMed] [Google Scholar]
- 5.Leopardi D, Hoggan BL, Fitridge RA, Woodruff PW, Maddern GJ. Systematic review of treatments for varicose veins. Ann Vasc Surg. 2009;23(2):264–76. doi: 10.1016/j.avsg.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Merchant RF, Pcihot O. Endovenous radiofrequency ablation of superficial and perforator veins. Vasc Surg. 2005;42(3):502–9. doi: 10.1016/j.jvs.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Almeida JA, Kaufman JA, Galckeritz OA, Chopra PA, Evans MT, Daniel F, et al. Radiofrequency endovenous ClosureFAST versus laser ablation for the treatment of great saphenous reflux: a multicenter, single-blinded, randomized study (recovery study) JVIR. 2009;20(6):752–759. doi: 10.1016/j.jvir.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Markovic JN, Shortell CK. Update on radiofrequency ablation. Vasc Surg Endovasc Ther. 2009;21(2):82–90. doi: 10.1177/1531003509335156. [DOI] [PubMed] [Google Scholar]
- 9.Kompally GR, Bhardwaj S, Singh G. Varicose veins clinical presentation and surgical management. Ind J Surgery. 2009;71:117–120. doi: 10.1007/s12262-009-0034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roth SM. Endovenous radiofrequency ablation of superficial and perforator veins. Surg Clin North Am. 2007;87(5):1267–84. doi: 10.1016/j.suc.2007.07.009. [DOI] [PubMed] [Google Scholar]