Abstract
The appearance of subcapsular liver hematoma after a laparoscopic cholecystectomy (LC) is an infrequent complication and seldom studied. Some cases have been connected to ketorolac given during surgery and after surgery. Other described causes are : hemangiomas or small iatrogenic lesions that could be aggravated by administration of ketorolac. Coagulation dysfunction like circulating heparin as seen in hemathological diseases is cause of bleeding after aggressive procedures. We describe two cases of subcapsular liver hematoma after LC, both of them have been given intravenous ketorolac and one of them had multiple myeloma. We discuss the causes and treatment of it.
Keywords: Laparoscopic cholecystectomy, Spontaneous subcapsular liver hematoma, Complications of laparoscopic cholecystectomy, Ketorolac and surgery, Circulanting heparin-like anticoagulants
Introduction
The appearance of subcapsular liver hematoma after a laparoscopic cholecystectomy (LC) is an infrequent complication and seldom studied. Some cases have been connected to ketorolac given during surgery and after surgery. Other described causes are: hemangiomas or small iatrogenic lesions that could be aggravated by administration of ketorolac. Coagulation dysfunction like circulating heparin as seen in hemathological diseases is cause of bleeding after aggressive procedures. We describe two cases of subcapsular liver hematoma after LC, both of them have been given intravenous ketorolac and one of them had multiple myeloma. We discuss the causes and treatment of it.
Case 1
A 69 years old woman with medical history of multiple myeloma and Pott’s disease was admitted for elective laparoscopic cholecystectomy (LC). An ultrasound previous to surgery showed cholelitiasis without signs of cholecystitis. Blood tests were normal (haemoglobin 13.5 g/L; INR: 1.1; prothrombin time: 13 seconds).
LC was performed using four trocars: two 10 mm trocars and two 5 mm trocars. The dissection was accomplished without difficulty. Neither wounds nor lacerations were observed during surgery. The patient was administered 30 mg of intravenous ketorolac at the end of the surgery and the three days following surgery: 30 mg every 8 hours. The postoperative period was a bit slow due to pyrexia and inspecific gastrointestinal symptoms.
On the fifth day after surgery, the patient had right upper quadrant pain, nauseas and vomits. Blood test showed a light decrease of haemoglobin: 9.6 g/L. An ultrasound was made and no lesions were revealed.
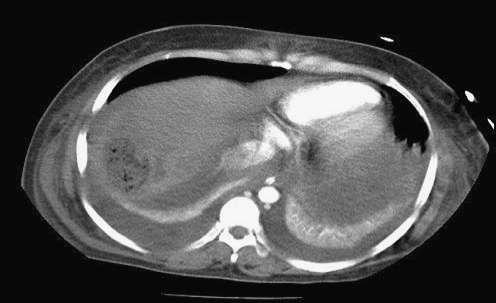
After 24 hours, the patient showed hemodynamic instability, hypotension, tachycardia , and blood test: haemoglobin of 4.5 g/L, INR 0.9, and increase of liver enzymes: GOT 5782, GPT 367 and FA 146. A CT (Figs. 1 and 2) revealed an intrahepatic subcapsular collection in V, VI and VII hepatic segments (size: 16 × 5 cm). The patient was admitted in the ICU. An arteriography was performed but no signs of active bleeding were observed.
Fig. 1.
Intrahepatic subcapsular collection in V, VI and VII hepatic segments
Fig. 2.
Intrahepatic subcapsular collection in V, VI and VII hepatic segments (16 × 5 cm)
So, an exploratory laparotomy was made due to hemodynamic instability, despite blood and plasma support. An important hematoma in the right lobe hepatic was observed; it was drained and packed, a hepatic biopsy was taken. Neither parenchymal injury of the gallbladder bed nor iatrogenic lesions were seen. After 48 hours, the packing was reviewed and no signs of bleeding were seen.
The patient recovered uneventfully. Control CT was performed 20 days after surgery and it revealed avascular areas in V, VI and VII hepatic segments. Rest of liver was normal.
She was also followed up by Hematology Department, and they suggested that the “heparin like anticoagulant factor” associated to haematology diseases (in this case multiple myeloma) could have triggered the bleeding and so, the subcapsular hematoma liver. Though, they did not find “heparin like anticoagulant factor” in her blood, and coagulation tests were normal: INT 1.0; thrombin time: 13 seconds; reptilase time: 16 seconds; activated partial thromboplastin time: 30 seconds.
The patient was discharged 37 days after the elective LC.
The biopsy revealed ischemia and necrosis.
A new control CT was made after 5 months: small hypocaptant areas in the highest zone of right lobe liver.
Case 2
A 29 years old woman was admitted for elective LC because of cholelitiasis. Medical history was insignificant. Ultrasound previous to surgery revealed cholelitiasis without signs of cholecystitis. Blood tests were normal: INR 1.0; prothrombin time 14 seconds.
She underwent LC using four trocars: two 10 mm trocars and two 5 mm trocars. The dissection of the gallbladder from the liver bed was accomplished easily. There were no incidents during surgery. She was administered ketorolac 30 mg intravenous at the end of the surgery and 30 mg every 8 hours for 24 hours.
After 24 hours, the patient had an episode of perspiration and hypotension which did not improve with support measures. Blood test showed haemoglobin of 6 gr/L, INR 0.8 and liver dysfunction. A CT was made and showed a subcapsular hematoma of the right lobe liver (Fig. 3). So, she underwent exploratory laparotomy and we found a massive subcapsular hematoma of the right liver lobe. No iatrogenic lesions were found. The bed gallbladder did not present lesions. The hematoma was drained and we performed a packing. After 24 hours, we reviewed the patient and did not find signs of bleeding. A liver biopsy was taken and reported like hematic material.
Fig. 3.
Subcapsular hematoma in right lobe liver
After surgery the patient had pleural spillage, auricular fibrillation and polyneuropathy.
She was discharged after 30 days and remains well and asymptomatic nowadays.
Discussion
The LC is the choice for the treatment of symptomatic uncomplicated cholelithiasis [9]. The mortality rate is around 0.66% [9] and morbidity of 7% [4]. The appearance of postoperative haemorrhage is rare ( 0.08–0–2% of all cases ) [2], and the places where more often occur are: gallbladder bed, abdominal wall, cystic artery and falciform ligament [2].
Ketorolac is the first injectable nonsteroidal antiinflammatory drug used as an analgesic in the perioperative period [1, 3, 8], it is also used by anestesists like part of the standardized, evidence-based regime [11]. Between all of the NSAIDs, ketorolac is associated with the highest risk estimate of bleeding [10]. It has an antiplatelet activity and its activity could last as long as 24 hours after its administration [3]. Ketorolac could cause bleeding and hematoma, or aggravate any small hepatic injury during surgery [1].
The presence of circulating heparin like anticoagulant is observed in haematological diseases such as multiple myeloma, T-prolymphocytyc leukaemia..., so it has been described that these patients could bleed after small aggressive procedures [12] such as brown bone aspiration, cutaneous bleeding [14], epistaxis [13] or deep site hematoma [13].
So, there are several theories about the cause of subcapsular liver hematoma in these patients. Traction of the lower hepatic surface made for irrigating and draining the subhepatic space would produce bleeding and hematoma ; in addition to, hepatic hemangiomas were found in some cases, so the traction over the liver could break these hemangiomas, so this with administration of ketorolac would cause a liver subcapsular hematoma, like Pietra et all. support[2]. Some surgeons support the study of the hepatic parenchymal previous to surgery.
Three clear causes have been described like cause of liver hematoma: small tears of the hepatic capsule after traction on the gallbladder, puncture of the liver with the trocar when introducing the trocar and parenchymal injury while excision of the gallbladder [15].
Others back up that this kind of complication is inherent to the method of surgery itself [5].
The diagnostic can be difficult till symptoms appear: pain, fever, vomits or hypovolemic shock.
About the management: if the patient is stable, asymptomatic and the hematoma is small a conservative therapy is the choice. But if the hematoma has an important size so it is unlikely that it can be reabsorbed, a percutaneous drain can be performed using under ultrasound guidance [7]. If the patient is unstable a laparotomy is mandatory [6].
We report about two cases: The first one was a woman with multiple myeloma (Ig A), who was given 30 mg intravenous ketorolac during and after surgery . There were no incidents during surgery and no lesions were seen. The postoperative period was slow with non-specific symptoms. She went under laparotomy because of hemodynamic instability. We did not find iatrogenic lesions, just an important hematoma in the right hepatic lobe. It was drained and a packing made. The cause about this intrahepatic hematoma is not clear. We think that ketorolac could have had a role, or have aggravated some small lesions caused during surgery and not seen. In addition to, the patient had a multiple myeloma; the role of this is not clear because it was studied by hemathologists and until now they have not been able to demonstrated alteration in coagulation tests. We think that more studies about this condition are needed because of there are some cases, in the literature, about bleeding in this patients. We cannot discard the possibility of breaking some hemangioma during surgery, though no hemangiomas were seen on ultrasound performed previous to surgery.
In the second case, ketorolac was also administrated during and after surgery, 30 mg every 8 hours, intravenous. There were no incidents during surgery. Laparotomy was needed because of hemodynamic instability But in this case, the cause seems to clearer : a imagen of 2 cm of size compatible with a hemangioma was found in an ultrasound during the follow up. We think that the hemangioma could have been broken fortuitously during surgery and not seen, and the ketorolac given would have aggravated the lesion, like Pietra et al. supports in his work [2].
We conclude, the LC is a safe method and the choice for symptomatic uncomplicated cholelithiasis, with low mortality and morbidity. The presence of an subcapsular liver hematoma after a LC is a rare complication few studied. Till now only 10 cases haven been reported. It has been connected to administration of ketorolac, which would aggravate small iatrogenic lesions occurring during surgery and that would go unnoticed. But others factors could have an important role, like the presence of hemangiomas that would be ruptured by chance during surgery or causes that would produce bleeding such as circulating heparin like associated to haematological disease such multiple myeloma or leukaemia. About the management: if the patient is stable the hematoma can be observed or drained percutanously with ultrasound guidance, and if instable laparotomy is mandatory. More studies are needed to clear these causes and determinate is some kind of study should be accomplished in patient with risk of bleeding, as though the role of the ketorolac in perioperative-postoperative period.
References
- 1.Ertad BL, Rapapport WD. Subcapsular hematoma alter laparoscopic cholecystectomy, associated with ketorolac administration. Pharmacotherapy. 1994;14:613–615. [PubMed] [Google Scholar]
- 2.Pietra N, Sarli L, Costi R, Violi V. Intrahepatic subcapsular hematoma: a rare postoperative complication of laparoscopic cholecystectomy. Surg Laparosc Endosc. 1998;8:304–307. doi: 10.1097/00019509-199808000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Vuilleumier H, Halkic N. Ruptured subcapsular hematoma after laparoscopic cholecystectomy attributed to ketorolaco induced coagulopathy. Surg Endosc. 2003;17:659. doi: 10.1007/s00464-002-4255-9. [DOI] [PubMed] [Google Scholar]
- 4.Nathason LK, Shimi S, Cuscgieri A. Laparoscopic cholecystectomy: the Dundee thecnique. Br J Surg. 1991;78:155–159. doi: 10.1002/bjs.1800780208. [DOI] [PubMed] [Google Scholar]
- 5.Alexander HC. Two unusual hemorrhagic complications during laparoscopic cholecystectomy. Surg Laparosc Endosc. 1993;3:346–348. [PubMed] [Google Scholar]
- 6.Obara K, Imai S, Uchiyama S, Uchiyama K, Moriyama Y. A case with subcapsular hematoma of the liver following laparoscopic cholecystectomy. Nippon Ika Daigaku Zasshi. 1998;65:478–480. doi: 10.1272/jnms1923.65.478. [DOI] [PubMed] [Google Scholar]
- 7.Bhandakar DS, Katara AN, Shah RS. Intrahepatic subcapsular hematoma complicating laparoscopic cholecystectomy. Sug Laparosc Endosc. 2004;18(5):868–870. doi: 10.1007/s00464-003-4540-2. [DOI] [PubMed] [Google Scholar]
- 8.Shetty GS, Stuart Falconer J, Benyounes H. Subcapsular hematoma of the liver fater laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech. 2005;15(1):48–50. doi: 10.1089/lap.2005.15.48. [DOI] [PubMed] [Google Scholar]
- 9.Navez B, Mutter D, Russier Y, Vix M, Jamali F, Lipski D, et al. Safety of laparoscopic approach for acute cholecystitis: retrospective study of 609 cases. World J Surg. 2001;25(10):1352–1356. doi: 10.1007/s00268-001-0122-4. [DOI] [PubMed] [Google Scholar]
- 10.Laporte JR, Ibanez L, Vidal X, Vendrell L, Leone R. Upper gastrointestinal bleeding associated with the use of NSAIDs: newer versus older agents. Drug Saf. 2004;27(6):41120. doi: 10.2165/00002018-200427060-00005. [DOI] [PubMed] [Google Scholar]
- 11.Jensen K, Kehlet H, Lund CM. Post-operative recovery profile after laparoscopic cholecystectomy: a prospective observational study of a multimodal anaesthetic regime. Acta Anaesthesiol Scand. 2007;51(4):464–71. doi: 10.1111/j.1399-6576.2006.01251.x. [DOI] [PubMed] [Google Scholar]
- 12.Shetty GS, Falconer JS, Benyounes H. Subcapsular hematoma of the liver after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2005;15(1):48–50. doi: 10.1089/lap.2005.15.48. [DOI] [PubMed] [Google Scholar]
- 13.Llamas P, Outeirino J, Espinoza J, Santos AB, Roman A, Tomas JF. Report of three cases of circulating heparin-like anticoagulants. Am J Hematol. 2001;67(4):256–258. doi: 10.1002/ajh.1126. [DOI] [PubMed] [Google Scholar]
- 14.Torjemane L, Guermazi S, Ladeb S, Romdhane NB, Lakhal A, Abdelkefi A, et al. Blood Coagul Fibrinolysis. 2007;18(3):279–281. doi: 10.1097/MBC.0b013e32809cc946. [DOI] [PubMed] [Google Scholar]
- 15.Fusco MA, Scout TE, Pauluzzi MW. Traction injury to the liver during laparoscopic cholecystectomy. Surg Laparosc Endosc. 1994;6:454–456. [PubMed] [Google Scholar]