Abstract
Clearance of apoptotic cells is necessary for tissue development, homeostasis and resolution of inflammation. The uptake of apoptotic cells is initiated by an ‘eat-me’ signal, such as phosphatidylserine, on the cell surface and phagocytes recognize the signal by using specific receptors. In this study, we show that the soluble form of the receptor for advanced glycation end products (RAGE) binds to phosphatidylserine as well as to the apoptotic thymocytes. RAGE-deficient (Rage−/−) alveolar macrophages showed impaired phagocytosis of apoptotic thymocytes and defective clearance of apoptotic neutrophils in Rage−/− mice. Our results indicate that RAGE functions as a phosphatidylserine receptor and assists in the clearance of apoptotic cells.
Keywords: macrophage, phagocytosis, phosphatidylserine, apoptosis, RAGE
Introduction
The receptor for advanced glycation end products (RAGE) is a member of the immunoglobulin superfamily of cell-surface molecules (Neeper et al, 1992); it is expressed in diverse cell types including endothelium, T-lymphocytes and monocytes/macrophages (Brett et al, 1993). RAGE recognizes a variety of ligands, such as high-mobility group protein-1 (HMGB1), and the binding of RAGE to such ligands has been linked to many diseases including diabetes, atherosclerosis, neurodegeneration, inflammation and tumours (Ramasamy et al, 2009). RAGE is expressed in both a full-length membrane-bound form (mRAGE) and various soluble forms lacking the transmembrane domain (sRAGE). sRAGE is produced by the proteolytic cleavage of mRAGE and alternative mRNA splicing (Raucci et al, 2008; Hudson et al, 2008a) and is a competitive inhibitor of RAGE by acting as a decoy for RAGE ligands (Santilli et al, 2009).
Rapid removal of apoptotic cells by phagocytes is crucial for the maintenance of tolerance and prevents inflammation and autoimmune responses against intracellular antigens released from the dying cells (Savill & Fadok, 2000). The uptake of apoptotic cells is initiated by an ‘eat-me’ signal, such as phosphatidylserine, on the cell surface and phagocytes recognize the signal by using specific receptors (Fadok et al, 1992; Verhoven et al, 1995). Several classes of receptors have been implicated in the recognition of apoptotic cells, possibly by means of direct binding to the exposed phosphatidylserine, including brain-specific angiogenesis inhibitor 1 (BAI1), T-cell immunoglobulin and mucin domains-containing protein 4 (Tim4) and stabilin-2 (Kobayashi et al, 2007; Miyanishi et al, 2007; Park et al, 2007, 2008), or indirect binding through bridging molecules (milk fat globule-EGF factor 8 protein (MFG-E8), growth arrest-specific 6 (Gas6); Scott et al, 2001; Hanayama et al, 2004). The engagement of the phosphatidylserine receptors initiates signalling events within the phagocytes that lead to activation of the small GTPase Rac and the subsequent cytoskeletal reorganization of the phagocyte membrane, to allow corpse internalization (Albert et al, 2000). Deficiencies of the receptors that participate in the recognition of phosphatidylserine on the surface of apoptotic cells lead to a failure to maintain self-tolerance and the development of autoimmunity (Cohen et al, 2002; Asano et al, 2004).
Although RAGE is a member of the pattern-recognition receptor family (Xie et al, 2008), whether it participates in the phagocytosis and clearance of apoptotic cells remains unknown. In this study, we present evidence that RAGE binds to phosphatidylserine and modulates apoptotic cell phagocytosis. Furthermore, we confirm the role of RAGE in apoptotic cell clearance in lipopolysaccharide (LPS)-induced acute lung injury in mice.
Results And Discussion
sRAGE binds to apoptotic thymocytes and phosphatidylserine
To determine whether RAGE identifies its functional ligands on apoptotic cells, we prepared thymocytes with a proportion of apoptotic cells by dexamethasone treatment and evaluated the binding capacity of RAGE to the apoptotic thymocytes by using Alexa Fluor 660 dye-labelled sRAGE and JC-1 dye (Petit et al, 1995). We found that sRAGE specifically bound to an apoptotic population of thymocytes (Fig 1A, black portion), indicating that RAGE binds to a structure highly expressed on the surface of apoptotic thymocytes. Advanced glycation end product, one of the main RAGE ligands, was not present on apoptotic thymocytes (supplementary Fig S2 online). Exposure of phosphatidylserine on the outer-membrane leaflet is an important indicator of the presence of apoptotic compared with live cells (Fadok et al, 1992); therefore, we tested whether RAGE can bind to phosphatidylserine. By using a protein–lipid overlay assay that used hydrophobicmembranes pre-spotted with a concentration gradient of eight different lipids found in cell membranes (PIP Strip), we found that sRAGE specifically bound to phosphatidylserine in a concentration-dependent manner, except for a slight binding to phosphatidylglycerol (Fig 1B). To determine the binding affinity of sRAGE to phosphatidylserine, we used a surface-plasmon resonance analysis (Biacore) using phosphatidylserine or phosphatidylcholine (as a reference) liposomes immobilized on the sensor chip and serial dilutions of sRAGE as soluble analytes. The sensorgrams showed an increase in response units that was reflective of phosphatidylserine binding, and the binding response was concentration dependent, with a KD of 0.563 μM (Fig 1C). These findings indicate that sRAGE specifically binds to phosphatidylserine.
Figure 1.
sRAGE binds to apoptotic cells and phosphatidylserine. (A) JC-1 dye detects mitochondrial membrane potential and red fluorescence decreases in apoptotic cells (black dots). sRAGE specifically bound to apoptotic cells (black), compared with a non-apoptotic population (grey). Data shown are representative of three experiments. (B) sRAGE bound to phosphatidylserine blotted on PIP Strip. Data shown are representative of two experiments. (C) SPR assays. A serial concentration of sRAGE (0, 4.32, 13.9, 117 and 350 μg/ml) was flowed over immobilized PS or PC liposomes on the Biacore sensor chip. Response to PC was used as a reference (left). The response curve of PS/sRAGE binding was obtained by subtracting the curve of PS from that of PC, as described in the Methods section (right). Data shown are representative of two experiments. BSA, bovine serum albumin; PC, phosphatidylcholine; PS, phosphatidylserine; RU, response units; SPR, surface-plasmon resonance; sRAGE, soluble receptor for advanced glycation end products.
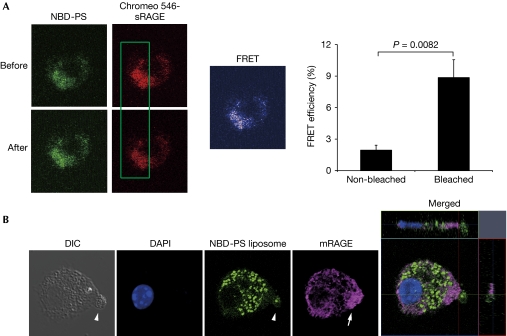
To investigate whether sRAGE can interact with phosphatidylserine on apoptotic cells, apoptotic thymocytes were incubated with NBD-phosphatidylserine (1,2-dioleoyl-sn-glycero-3-phospho-L-serine-N-(7-nitro-2-1,3-benzoxadiazol-4-yl)) and Chromeo 546-labelled sRAGE. The distribution of phosphatidylserine and sRAGE on the cell surface was determined by confocal imaging, and the interaction between sRAGE and NBD-phosphatidylserine was measured by fluorescence resonance energy transfer (FRET analysis). As shown in Fig 2A, both phosphatidylserine and sRAGE were localized to the surface of apoptotic thymocytes. FRET spots, indicating interactions between sRAGE and phosphatidylserine, appeared on the cell surface, with the acceptor (Chromeo 546–sRAGE, red fluorescence) being photobleached. By contrast, fewer FRET spots were observed on the cell surface of the same thymocytes that were not photobleached (Fig 2A). This indicates that RAGE and phosphatidylserine colocalize on the cell membrane.
Figure 2.
RAGE and phosphatidylserine bind to each other on the cell surface. (A) Images of the donor (NBD-PS, green) on apoptotic thymocytes, the acceptor (sRAGE, red), the bleached area and the FRET spots are shown. FRET efficiency was significantly increased by bleaching the fluorescence of the acceptor (sRAGE), demonstrating the direct binding between PS and RAGE (right graph). Data represent average values with s.e.m. Student's t-test was used to analyse the comparisons between two groups, and P values < 0.05 were considered significant. (B) A representative confocal microscopic image of a macrophage phagocytosing a PS liposome. Membrane-associated full-length RAGE expression on macrophages was concentrated in a pseudopod that was formed (arrow) towards a PS liposome (arrowhead). Phagocytosed NBD-PS was seen in the cytoplasm of the macrophage. DAPI, 4,6-diamidino-2-phenylindole; DIC, differential interference contrast; FRET, fluorescence resonance energy transfer; mRAGE, membrane receptor for advanced glycation end products; PS, phosphatidylserine; RAGE, receptor for advanced glycation end products; sRAGE, soluble receptor for advanced glycation end products.
Confocal images of alveolar macrophages cocultured with NBD-phosphatidylserine liposomes showed that mRAGE expression was concentrated in a pseudopod that formed towards a phosphatidylserine liposome (Fig 2B). Both FRET analysis and confocal images demonstrated that phosphatidylserine expressed on apoptotic cells binds to full-length mRAGE located in macrophages, and that this phosphatidylserine–RAGE binding might have a role in apoptosis recognition and phagocytosis.
RAGE deficiency or sRAGE impairs phagocytosis
As RAGE can bind to phosphatidylserine, we sought to determine the function of RAGE in the phagocytosis of apoptotic cells, examining the phagocytic capacity of both wild-type and Rage−/− alveolar macrophages (Fig 3A). Alveolar macrophages were cocultured with apoptotic thymocytes from wild-type mice. The phagocytic index of wild-type alveolar macrophages at 2 h was significantly higher than that of Rage−/− macrophages (P=0.013; Fig 3B), suggesting that alveolar macrophages can recognize and phagocytose apoptotic cells through the activity of RAGE on their cell surface. Because sRAGE functions as an endogenous competitive inhibitor of ligand engagement by cell-surface RAGE (Santilli et al, 2009), we then examined the effect of sRAGE on macrophage phagocytosis. sRAGE administration significantly impaired the phagocytosis of apoptotic thymocytes by wild-type alveolar macrophages, which confirms that RAGE contributes to the phagocytosis of apoptotic cells. Interestingly, sRAGE administration also induced a significant phagocytosis defect in Rage−/− alveolar macrophages; it is possible that sRAGE counteracts not only RAGE-mediated phagocytosis, but also other phosphatidylserine receptor-mediated phagocytosis, such as that mediated by BAI1 and Tim4. These results suggest that RAGE is one of the phosphatidylserine receptors that recognize apoptotic cells.
Figure 3.
Rage−/− alveolar macrophages impair the phagocytosis of apoptotic thymocytes in vitro and show reduced Rac1 activation in response to phosphatidylserine liposomes. (A) Representative microscopic images showing the phagocytosis of wild-type and Rage−/− alveolar macrophages with or without sRAGE (3 μg/ml) treatment. Arrowheads indicate phagocytized thymocyte fragments. (B) Wild-type alveolar macrophages or Rage−/− alveolar macrophages incubated with apoptotic thymocytes with or without sRAGE. The number of apoptotic cells per macrophage uptake was determined as the phagocytic index. Phagocytic indexes were significantly decreased in sRAGE-treated and RAGE-deficient macrophages. (C) PS, and not PC, activated Rac1 in wild-type macrophages. PS-induced Rac1 activation was not seen in RAGE-deficient macrophages. sRAGE significantly attenuated PS-induced Rac1 activation. White bars represent wild type; black bars represent Rage−/−. Data represent average values with s.e.m. The data were compared using analysis of variance with the Bonferroni adjustment, and P values <0.05 were considered significant. AM, alveolar macrophage; PC, phosphatidylcholine; PS, phosphatidylserine; RAGE, receptor for advanced glycation end products; Rage−/−, RAGE deficient; sRAGE, soluble receptor for advanced glycation end products; WT, wild type.
PS–RAGE binding is crucial for Rac1 activation
Intracellular RAGE signalling pathways involve Rho GTPases (Hudson et al, 2008b) and Rac1, activation of one of Rho GTPases is essential in the phosphatidylserine-recognition system that is involved in apoptotic cell removal (Albert et al, 2000). We therefore prepared phosphatidylserine liposomes to mimic apoptotic cells and tested whether phosphatidylserine–RAGE binding could alter the level of activated Rac1 during uptake by alveolar macrophages. Wild-type alveolar macrophages showed greater phosphatidylserine liposome-induced Rac1 activation; by contrast, phosphatidylserine liposomes did not activate Rac1 in Rage−/− alveolar macrophages. Phosphatidylcholine liposomes were tested as a negative control, and did not activate Rac1 in either the wild-type or Rage−/− alveolar macrophages (Fig 3C). These data demonstrate that inducible Rac1 activation is due to phosphatidylserine recognition through RAGE in alveolar macrophages. The level of Rac1 remained at near-basal levels in both wild-type and Rage−/− macrophages when phosphatidylserine liposomes were supplied with sRAGE (Fig 3C). sRAGE competed with RAGE for phosphatidylserine binding and functioned as a decoy that abrogated Rac1 activation, supporting the assertion that phosphatidylserine–RAGE binding is a prerequisite for the induction of Rac1 activation in alveolar macrophages.
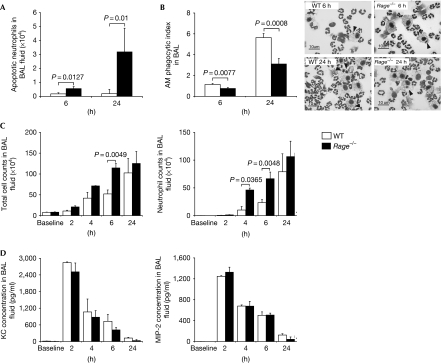
Defective clearance of apoptotic cells in Rage−/− mice
We next tested whether RAGE participates in apoptotic cell clearance in vivo. As RAGE is constitutively expressed at high levels in the lung (Brett et al, 1993), we induced lung injury in Rage−/− and wild-type mice by an intranasal insufflation of LPS (20 μg per mouse in 100 μl of PBS). Intranasal instillation of LPS induces extensive neutrophil migration within the airspace. Once neutrophils extravasate, they undergo programmed cell death (Watson et al, 1996) and are then removed from the airspace by phagocytosis of alveolar macrophages (Cox et al, 1995). This active programme of resolution starts in the first few hours after an inflammatory response begins (Serhan & Savill, 2005). We performed a bronchoalveolar lavage (BAL) at 0 (baseline), 2, 4, 6 and 24 h after LPS administration and examined the apoptotic cells recovered from the BAL fluid. More apoptotic neutrophils were found in Rage−/− mice at 6 and 24 h after LPS administration than in wild-type mice (Fig 4A). Further, we examined the phagocytosis of both wild-type and Rage−/− alveolar macrophages (Fig 4B, right). Rage−/− alveolar macrophages showed significantly decreased phagocytosis of apoptotic neutrophils at 6 and 24 h, compared with wild type (Fig 4B, left). Next, we checked whether this impaired clearance of apoptotic neutrophils would affect the accumulation of inflammatory cells within the airspace. We found that LPS administration resulted in a rapid increase of inflammatory cells in BAL fluid at 2, 4, 6 and 24 h in mice. The total number of cells in BAL fluid recovered from the Rage−/− mice was substantially greater than that recovered from the wild-type mice at 2, 4, 6 and 24 h, and there was a statistically significant difference at 6 h between the two groups (P=0.02; Fig 4C, left). The increased number of inflammatory cells was largely attributable to the increase in neutrophils (Fig 4C, right). We also checked keratinocyte-derived chemokine (KC) and macrophage inflammatory protein 2 (MIP-2), which are the key cytokines associated with neutrophil recruitment (Martin, 2002). The KC and MIP-2 levels in BAL fluid did not significantly differ between the two types of mice after LPS administration (Fig 4D). Taken together, these data show that deletion of RAGE in macrophages impairs the clearance of apoptotic cells, thereby leading to increased inflammatory cell accumulation within the airspace in the early phase of LPS-induced acute lung injury.
Figure 4.
Rage−/− alveolar macrophages impair apoptotic cell clearance in vivo. (A) Cells recovered from BAL fluid after LPS exposure were stained with FITC-conjugated annexin V and phycoerythrin-conjugated mouse Ly-6G (GR-1) antibody. Data show average counts of apoptotic neutrophils (GR-1+/annexin V+) in wild-type mice and Rage−/− mice (n=3–5). (B) Alveolar macrophage phagocytosis of apoptotic neutrophils in LPS-induced BAL was determined as the AM phagocytic index (n=6–9). The image indicates an AM with an ingested apoptotic neutrophil. (C) Changes in total cell counts in BAL fluid (left) and neutrophils (right) after LPS exposure in wild-type mice and Rage−/− mice, at each time point (n=5–9). (D) Changes in KC (left) and MIP-2 (right) levels in BAL fluid during the 24 h after LPS exposure (n=6–9). White bars represent wild type; black bars represent Rage−/−. Data represent average values with s.e.m. throughout. The data were compared using analysis of variance with the Bonferroni adjustment except neutrophil counts, KC and MIP-2. Neutrophil counts, KC and MIP-2 were analysed using non-parametric analysis of variance (Kruskal–Wallis test) with Dunn's Multiple Comparison Test. P values <0.05 were considered significant. AM, alveolar macrophage; BAL, bronchoalveolar lavage; FITC, fluorescein isothiocyanate; KC, keratinocyte-derived chemokine; LPS, lipopolysaccharide; MIP-2, macrophage inflammatory protein 2; Rage−/−, receptor for advanced glycation end products deficient; WT, wild type.
In LPS-induced lung injury, HMGB1 has a key role in the late phase of the injury (Wang et al, 1999). Liu et al (2008) reported that HMGB1 interacts with phosphatidylserine and diminishes the phagocytosis of apoptotic cells. We confirmed the binding of HMGB1 and phosphatidylserine by protein–lipid overlay assay (supplementary Fig S3A online) and surface-plasmon resonance analysis (Biacore; supplementary Fig S3B online). However, HMGB1 also bound to other lipids—namely, phosphatidylglycerol and phosphatidic acid—and its binding affinity to phosphatidylserine was lower than that of sRAGE (KD=3.08 μM in HMGB1, KD=0.563 μM in sRAGE), according to the Biacore analysis. Nevertheless, there remains the possibility of a multiprotein complex composed of sRAGE and HMGB1 that binds to phosphatidylserine in vivo; further work is needed to clarify this.
Apoptotic cell clearance is important for tissue development (Savill & Fadok, 2000), and inefficient phagocytosis of apoptotic cells could lead to the development of autoimmune disease (Zitvogel et al, 2010). However, Rage−/− mice that were kept in a sterile environment, were viable and did not show any overt phenotypes. The lack of both RAGE and sRAGE might keep the RAGE-null animals in a comparative balance in which no phenotype is expressed.
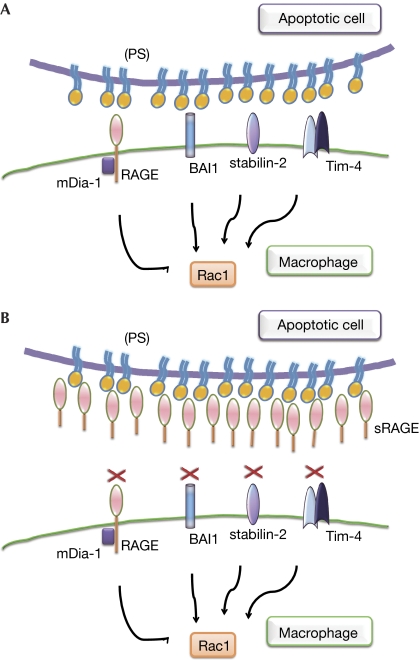
The data presented in this study provide new insights into the process of apoptotic cell clearance by RAGE. First, RAGE might function as one of the phosphatidylserine receptors that recognize and initiate apoptotic cell clearance (Fig 5A). Second, our data raise an important point regarding an sRAGE/mRAGE balance in overall apoptosis recognition, because sRAGE might counteract the phosphatidylserine engagement of cell-surface RAGE and other receptors, such as BAI1, Tim4 or stabilin-2, during phagocytosis (Fig 5B). sRAGE is produced by alternative splicing of RAGE mRNA or by proteolytic cleavage of RAGE from the cell surface in humans, and sRAGE has the same ligand-binding specificity, resulting in competition with RAGE for ligand binding. As sRAGE functions as a competitor for mRAGE binding to phosphatidylserine, the balance of sRAGE and mRAGE could modify macrophage phagocytotic activity, which might be an important component of pathophysiological situations in which apoptosis recognition has a key role.
Figure 5.
Summary of a possible RAGE- and sRAGE-signalling pathway in phagocytosis that involves phosphatidylserine recognition. (A) We propose that RAGE is a PS receptor that functions similarly to stabilin-2, BAI1 and Tim-4. (B) By binding to PS, sRAGE might counteract RAGE and other PS receptors, such as BAI1 and stabilin-2. BAI1, brain-specific angiogenesis inhibitor-1; mDia-1, mammalian Diaphanous-1; PS, phosphatidylserine; RAGE, receptor for advanced glycation end products; Tim-4, T-cell immunoglobulin and mucin domains-containing protein 4; sRAGE, soluble receptor for advanced glycation end products.
The present finding that RAGE is a phosphatidylserine receptor reveals a new role for RAGE in apoptosis-induced pathophysiological conditions and identifies a potential new target for the treatment of the relevant human diseases.
Methods
Recombinant sRAGE protein and Rage−/− mice were used for this study.
Identification of sRAGE by flow cytometry. Alexa Fluor 660 dye-labeled sRAGE or bovine serum albumin was added to dexamethasone-treated thymocytes. Apoptotic cells were identified using a MitoProbe JC-1 assay kit (Molecular Probes). Flow cytometry was performed on a BD FACSCanto II (BD Biosciences).
PIP strip assay. PIP strips on which the indicated phospholipids had been spotted, were purchased from Echelon Bioscience, and dot-blot experiments were carried out according to the manufacturer's protocol.
Surface-plasmon resonance analysis (Biacore). The binding affinity of sRAGE to phosphatidylserine was analysed using a Biacore X100 (Biacore AB) in a single-cycle affinity model. KD was calculated using ka and kd values by a trivalent analyte model.
FRET analysis. FRET analysis was performed as described previously (Liu et al, 2008).
Confocal laser scanning microscopy. Alveolar macrophages were grown on coverslips and then preincubated with 5 μM NBD-phosphatidylserine liposome for 2 h, after which mRAGE was detected by indirect immunofluorescence using a rabbit polyclonal RAGE antibody (Abcam) with Alexa Fluor 647-conjugated goat rabbit IgG (Molecular Probes).
Phagocytosis of apoptotic thymocytes. Phagocytosis was assayed by adding apoptotic thymocytes (2.5 × 106 cells/ml) with or without sRAGE (3 μg/ml). Phagocytosis was determined as a phagocytic index under microscopy, as described previously (Morimoto et al, 2006). Each condition was tested in duplicate, and the samples were analysed blindly and independently by two researchers (M.H. and K.M.).
Rac1 activity assays. Rac1 activity was measured using an ELISA-based Rac1 Activation Assay Biochem Kit (G-LISA, Cytoskeleton).
LPS-induced lung injury. LPS from Escherichia coli serotype 055:B5 was obtained from Sigma-Aldrich, and the induction of lung injury was performed as described previously (Yamada et al, 2004).
Detailed methods are described in the supplementary information online.
Supplementary information is available at EMBO reports online (http://www.emboreports.org).
Supplementary Material
Acknowledgments
We thank J. Aoki and A. Inoue for technical advice on preparing phosphatidylserine and phosphatidylcholine liposomes, and M. Kanzaki and H. Hatakeyama for expert technical assistance on FRET analysis. This work was supported by a grant-in-aid from the Japan Society for the Promotion of Science (20.08466) and grants from National Institute of Biomedical Innovation to H.K.
Footnotes
The authors declare that they have no conflict of interest.
References
- Albert ML, Kim JI, Birge RB (2000) αvβ5 integrin recruits the CrkII–Dock180–rac1 complex for phagocytosis of apoptotic cells. Nat Cell Biol 2: 899–905 [DOI] [PubMed] [Google Scholar]
- Asano K, Miwa M, Miwa K, Hanayama R, Nagase H, Nagata S, Tanaka M (2004) Masking of phosphatidylserine inhibits apoptotic cell engulfment and induces autoantibody production in mice. J Exp Med 200: 459–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett J et al. (1993) Survey of the distribution of a newly characterized receptor for advanced glycation end products in tissues. Am J Pathol 143: 1699–1712 [PMC free article] [PubMed] [Google Scholar]
- Cohen PL, Caricchio R, Abraham V, Camenisch TD, Jennette JC, Roubey RA, Earp HS, Matsushima G, Reap EA (2002) Delayed apoptotic cell clearance and lupus-like autoimmunity in mice lacking the c-mer membrane tyrosine kinase. J Exp Med 196: 135–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox G, Crossley J, Xing Z (1995) Macrophage engulfment of apoptotic neutrophils contributes to the resolution of acute pulmonary inflammation in vivo. Am J Respir Cell Mol Biol 12: 232–237 [DOI] [PubMed] [Google Scholar]
- Fadok VA, Voelker DR, Campbell PA, Cohen JJ, Bratton DL, Henson PM (1992) Exposure of phosphatidylserine on the surface of apoptotic lymphocytes triggers specific recognition and removal by macrophages. J Immunol 148: 2207–2216 [PubMed] [Google Scholar]
- Hanayama R, Tanaka M, Miyasaka K, Aozasa K, Koike M, Uchiyama Y, Nagata S (2004) Autoimmune disease and impaired uptake of apoptotic cells in MFG-E8-deficient mice. Science 304: 1147–1150 [DOI] [PubMed] [Google Scholar]
- Hudson BI, Carter AM, Harja E, Kalea AZ, Arriero M, Yang H, Grant PJ, Schmidt AM (2008a) Identification, classification, and expression of RAGE gene splice variants. FASEB J 22: 1572–1580 [DOI] [PubMed] [Google Scholar]
- Hudson BI, Kalea AZ, Del Mar Arriero M, Harja E, Boulanger E, D'Agati V, Schmidt AM (2008b) Interaction of the RAGE cytoplasmic domain with diaphanous-1 is required for ligand-stimulated cellular migration through activation of Rac1 and Cdc42. J Biol Chem 283: 34457–34468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi N et al. (2007) TIM-1 and TIM-4 glycoproteins bind phosphatidylserine and mediate uptake of apoptotic cells. Immunity 27: 927–940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu G, Wang J, Park YJ, Tsuruta Y, Lorne EF, Zhao X, Abraham E (2008) High mobility group protein-1 inhibits phagocytosis of apoptotic neutrophils through binding to phosphatidylserine. J Immunol 181: 4240–4246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin TR (2002) Neutrophils and lung injury: getting it right. J Clin Invest 110: 1603–1605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyanishi M, Tada K, Koike M, Uchiyama Y, Kitamura T, Nagata S (2007) Identification of Tim4 as a phosphatidylserine receptor. Nature 450: 435–439 [DOI] [PubMed] [Google Scholar]
- Morimoto K, Janssen WJ, Fessler MB, McPhillips KA, Borges VM, Bowler RP, Xiao YQ, Kench JA, Henson PM, Vandivier RW (2006) Lovastatin enhances clearance of apoptotic cells (efferocytosis) with implications for chronic obstructive pulmonary disease. J Immunol 176: 7657–7665 [DOI] [PubMed] [Google Scholar]
- Neeper M, Schmidt AM, Brett J, Yan SD, Wang F, Pan YC, Elliston K, Stern D, Shaw A (1992) Cloning and expression of a cell surface receptor for advanced glycosylation end products of proteins. J Biol Chem 267: 14998–15004 [PubMed] [Google Scholar]
- Park D, Tosello-Trampont AC, Elliott MR, Lu M, Haney LB, Ma Z, Klibanov AL, Mandell JW, Ravichandran KS (2007) BAI1 is an engulfment receptor for apoptotic cells upstream of the ELMO/Dock180/Rac module. Nature 450: 430–434 [DOI] [PubMed] [Google Scholar]
- Park SY, Jung MY, Kim HJ, Lee SJ, Kim SY, Lee BH, Kwon TH, Park RW, Kim IS (2008) Rapid cell corpse clearance by stabilin-2, a membrane phosphatidylserine receptor. Cell Death Differ 15: 192–201 [DOI] [PubMed] [Google Scholar]
- Petit PX, Lecoeur H, Zorn E, Dauguet C, Mignotte B, Gougeon ML (1995) Alterations in mitochondrial structure and function are early events of dexamethasone-induced thymocyte apoptosis. J Cell Biol 130: 157–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramasamy R, Yan SF, Schmidt AM (2009) RAGE: therapeutic target and biomarker of the inflammatory response--the evidence mounts. J Leukoc Biol 86: 505–512 [DOI] [PubMed] [Google Scholar]
- Raucci A, Cugusi S, Antonelli A, Barabino SM, Monti L, Bierhaus A, Reiss K, Saftig P, Bianchi ME (2008) A soluble form of the receptor for advanced glycation endproducts (RAGE) is produced by proteolytic cleavage of the membrane-bound form by the sheddase a disintegrin and metalloprotease 10 (ADAM10). FASEB J 22: 3716–3727 [DOI] [PubMed] [Google Scholar]
- Santilli F, Vazzana N, Bucciarelli LG, Davi G (2009) Soluble forms of RAGE in human diseases: clinical and therapeutical implications. Curr Med Chem 16: 940–952 [DOI] [PubMed] [Google Scholar]
- Savill J, Fadok V (2000) Corpse clearance defines the meaning of cell death. Nature 407: 784–788 [DOI] [PubMed] [Google Scholar]
- Scott RS, McMahon EJ, Pop SM, Reap EA, Caricchio R, Cohen PL, Earp HS, Matsushima GK (2001) Phagocytosis and clearance of apoptotic cells is mediated by MER. Nature 411: 207–211 [DOI] [PubMed] [Google Scholar]
- Serhan CN, Savill J (2005) Resolution of inflammation: the beginning programs the end. Nat Immunol 6: 1191–1197 [DOI] [PubMed] [Google Scholar]
- Verhoven B, Schlegel RA, Williamson P (1995) Mechanisms of phosphatidylserine exposure, a phagocyte recognition signal, on apoptotic T lymphocytes. J Exp Med 182: 1597–1601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H et al. (1999) HMG-1 as a late mediator of endotoxin lethality in mice. Science 285: 248–251 [DOI] [PubMed] [Google Scholar]
- Watson RW, Redmond HP, Wang JH, Condron C, Bouchier-Hayes D (1996) Neutrophils undergo apoptosis following ingestion of Escherichia coli. J Immunol 156: 3986–3992 [PubMed] [Google Scholar]
- Xie J, Reverdatto S, Frolov A, Hoffmann R, Burz DS, Shekhtman A (2008) Structural basis for pattern recognition by the receptor for advanced glycation end products (RAGE). J Biol Chem 283: 27255–27269 [DOI] [PubMed] [Google Scholar]
- Yamada M, Kubo H, Kobayashi S, Ishizawa K, Numasaki M, Ueda S, Suzuki T, Sasaki H (2004) Bone marrow-derived progenitor cells are important for lung repair after lipopolysaccharide-induced lung injury. J Immunol 172: 1266–1272 [DOI] [PubMed] [Google Scholar]
- Zitvogel L, Kepp O, Kroemer G (2010) Decoding cell death signals in inflammation and immunity. Cell 140: 798–804 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.