Abstract
Background:
Prior studies have supported an association between insufficient sleep and childhood obesity, but most have not examined nationally representative samples or considered potential sociodemographic confounders.
Objective:
The main objective of this study was to use a large, nationally representative dataset to examine the possibility that insufficient sleep is associated with obesity in children, independent of sociodemographic factors.
Methods:
The National Survey of Children's Health is a national survey of U.S. households contacted by random digit dialing. In 2003, caregivers of 102,353 US children were surveyed. Age- and sex-specific body mass index (BMI) based on parental report of child height and weight, was available for 81,390 children aged 6-17 years. Caregivers were asked, “How many nights of sufficient sleep did your child have in the past week?” The odds of obesity (BMI ≥ 95th percentile) versus healthy weight (BMI 5th-84th percentile) was regressed on reported nights of sufficient sleep per week (categorized as 0-2, 3-5, or 6-7). Sociodemographic variables included gender, race, household education, and family income. Analyses incorporated sampling weights to derive nationally representative estimates for a 2003 population of 34 million youth.
Results:
Unadjusted bivariate analyses indicated that children aged 6-11 years with 0-2 nights of sufficient sleep, in comparison to those with 6-7 nights, were more likely to be obese (OR = 1.7, 95% CI [1.2-2.3]). Among children aged 12-17 years, odds of obesity were lower among children with 3-5 nights of sufficient sleep in comparison to those with 6-7 nights (0.8, 95% CI: 0.7-0.9). However, in both age groups, adjustment for race/ethnicity, gender, family income, and household education left no remaining statistical significance for the association between sufficient nights of sleep and BMI.
Conclusion:
In this national sample, insufficient sleep, as judged by parents, is inconsistently associated with obesity in bivariate analyses, and not associated with obesity after adjustment for sociodemographic variables. These findings from a nationally representative sample are necessarily subject to parental perceptions, but nonetheless serve as an important reminder that the role of insufficient sleep in the childhood obesity epidemic remains unproven.
Citation:
Hassan F; Davis MM; Chervin RD. No independent association between insufficient sleep and childhood obesity in the national survey of children's health. J Clin Sleep Med 2011;7(2):153-157.
Keywords: Obesity, sleep, sleep deprivation, children, survey
Childhood obesity, both worldwide and within the United States, has risen dramatically during the last 30 years to reach epidemic proportions.1–3 Studies conducted among adults have suggested that insufficient sleep could be an important contributor.4 Shorter duration of sleep among adults reduces levels of leptin, resulting in decreased satiation and increased levels of ghrelin, resulting in increased appetite.5,6
Comparatively little is known about the effect of insufficient sleep on childhood obesity. Cross-sectional studies have reported that children with few hours of sleep have higher odds of obesity.7–10 However, several of these studies have not included sociodemographic variables as possible confounders.7,11 In addition, studies have been conducted among smaller samples without heterogeneity in race and ethnicity.7,9 Two large, cross-sectional studies of children aged 5-6 and 3-10 years showed higher odds of overweight, obesity, and excessive body fat when sleep duration was short (< 10 h), after controlling for potential confounders such as parental BMI and education.10,12
BRIEF SUMMARY
Current Knowledge/Study Rationale: A majority of the studies have shown a correlation between insufficient sleep and childhood obesity. We sought to investigate in a nationally representative population the association between insufficient sleep and childhood obesity after controlling for a range of potential sociodemographic confounders.
Study Impact: The results of our study indicate that the role of insufficient sleep on the childhood obesity epidemic remains unproven.
Some longitudinal studies have suggested that insufficient sleep is a risk factor for obesity later in childhood. Among children followed from birth to 9.5 years, less sleep assessed annually between 2 and 5 years, was a risk factor for obesity, but the effect stemmed mainly from daytime naps rather than the duration of nocturnal sleep.13 In the Toyama Birth Cohort Study of children aged 5-6 years, those with < 8 h, 8-9 h, and 9-10 h of sleep, in comparison to children with > 10 h of sleep per night, had higher odds of obesity—2.87, 1.89, and 1.49, respectively.9 However, household income and education were not considered. The Avon Longitudinal study found that the likelihood of obesity at 7 years of age was higher among 30-month-old children with 10.5 and 10.5-10.9 h of sleep as compared to those with > 12 h of sleep.8 However, maternal education and social class were the only sociodemographic variables taken into account. Another recent study took maternal education, race, television viewing, active play, and household income into account, but was conducted in a sample for which most household incomes exceeded $70,000 per year.14 A longitudinal study of 785 children, representing about one-half of the original cohort derived from 10 U.S. urban and rural areas, took into account gender, race, and maternal education, but not income15; the authors found an association between shorter sleep duration in 3rd grade and overweight status in 6th grade.
In short, although cross-sectional and longitudinal studies have generally supported an association between insufficient sleep and childhood obesity, findings may have been affected by community samples that were small or less than representative, or by lack of examination of a wider range of sociodemographic variables. In particular, age, gender, race/ethnicity, household education, and household income all may play important roles in obesity.16–19 The objective of this study, therefore, was to investigate the association between insufficient sleep and childhood obesity in a nationally representative sample for which a broad range of potential sociodemographic confounders were also assessed.
METHODS
Design and Study Sample
The National Survey of Children's Health (NSCH)20 was a telephone survey conducted by the National Center for Health Statistics (NCHS) from January 2003 to July 2004. The survey was sponsored by the Maternal and Child Health Bureau of the Health Resources and Services Administration. The NSCH data set is available for public use and contains no personal identifying information.
The purpose of the NSCH was to gather national and state-specific prevalence estimates of health indicators and children's experiences, from the caregiver perspective, with the health care system. The survey conducted by random digit dialing, gathered data from primary caregivers on 102,353 children aged 0-17 years. One child in each household was randomly selected to be a subject for the interview. The interviews were conducted in either English or Spanish. The survey was translated from English to Spanish by an experienced translator and was reviewed by several Spanish-speaking telephone interviewers. Bilingual (English/Spanish) interviewers conducted the interviews in Spanish. The weighted overall response rate was 55.3%.
The data file released contains demographic information on the child and substantive data on the health and well-being of the child as well as his or her family. Similar to a previous study estimates are based on the sampling weights generalize to the non-institutionalized population of children in each state and nationwide.21 The NSCH child weights are adjusted so that the sum of the weights equals the July 2003 Census bureau estimates for the number of children of each age by sex and by race/ethnicity group in each state, and further adjusted for weighted proportion of children in each household and educational level.
Study Cohort and Classification
The NSCH asked one specific question about sleep to the caregiver of children aged 6-17 years: “How many nights of sufficient sleep did your child get in the past week?” The response was on a scale from 0-7 nights. For the purpose of our analysis, responses were grouped into 0-2 nights, 3-5 nights, and 6-7 nights of sleep. Age- and sex-specific BMI was available for children aged 2-17 years. Children were classified based on their BMI: underweight (< 5th percentile), healthy weight (5th-84th percentile), overweight (85th-94th percentile), and obese (≥ 95th percentile). The study sample was divided by age into 2 groups: children aged 6-11 and 12-17 years. As in a previous study, to calculate the odds of obesity, healthy-weight children were used as a comparison group.22
Bivariate analyses using chi square tests were conducted to compare nights of sufficient sleep to BMI, age, sex, race/ethnicity, income level, and household education. Using bivariate logistic regression, we determined the odds that a given child had a BMI in the obese range versus the healthy weight range, given his/her nights of sufficient sleep.
In pre-planned multivariable models, we added 4 sociodemographic explanatory variables: child's sex and race/ethnicity, household income level, and household education.
All analyses were conducted using Stata 9.0 (Stata Corp., College Station, TX) statistical software with weights to account for the complex stratified sampling used to compile the NSCH database. All results are presented using weighted values. The study was approved by the University of Michigan Institutional Review Board.
RESULTS
Subject Characteristics
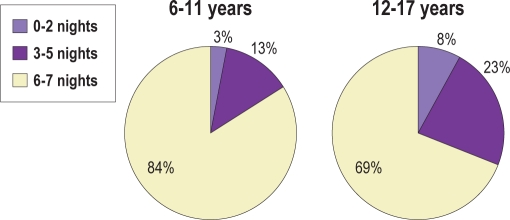
Age- and sex-specific BMI and data on nights of sufficient sleep were available for 81,390 children aged 6-17 years. The majority of the children (53%) were in the healthy weight category, 7% were underweight, 15% were overweight, and 25% were obese. Between the ages of 6 and 11 years, 3% of children were reported to obtain sufficient sleep on only 0-2 nights per week, whereas between the ages of 12 and 17 years, 8% were reported to do so (Figure 1).
Figure 1.
Proportions of children reported to have 0-2, 3-5, or 6-7 nights of sufficient sleep
Insufficient Sleep
In bivariate analyses, Hispanics were more likely to have only 0-2 nights of sufficient sleep (8%) vs. blacks (6%) and non-Hispanic whites (5%, p < 0.05), and more likely to have 6-7 nights of sufficient sleep (79% vs. 75% vs. 76%, p < 0.05).
In analyses within each of the 2 separate age groups, Hispanic children aged 6-11 years were more likely than blacks and non-Hispanic white children to have 0-2 nights of sufficient sleep; black children were less likely to have 6-7 nights of sufficient sleep in comparison to white and Hispanic children (Table 1). Similarly among the older subjects, Hispanic children aged 12-17 years were more likely to have a higher proportion of 0-2 nights of sufficient sleep than non-Hispanic whites and blacks (Table 1).
Table 1.
Percentage of children reported to obtain specified nights of sufficient sleep, for each age group and demographic variable category*
| 6-11 years |
12-17 years |
|||||
|---|---|---|---|---|---|---|
| Variable | 0-2 nights | 3-5 nights | 6-7 nights | 0-2 nights | 3-5 nights | 6-7 nights |
| Age- and sex-specific body mass index class | ||||||
| Underweight | 2 | 13 | 85 | 10 | 21 | 69 |
| Healthy weight | 2 | 13 | 85 | 8 | 24 | 68 |
| Overweight | 2 | 14 | 84 | 7 | 21 | 72 |
| Obese | 4 | 13 | 83 | 8 | 21 | 71 |
| Race | ||||||
| White | 3 | 13 | 84 | 8 | 24 | 68 |
| Hispanics | 7 | 11 | 82 | 10 | 16 | 74 |
| Black | 5 | 15 | 80 | 7 | 22 | 71 |
| Multiracial | 4 | 16 | 80 | 7 | 21 | 72 |
| Others | 1 | 6 | 93 | 9 | 21 | 70 |
| Gender | ||||||
| Male | 3 | 13 | 84 | 8 | 22 | 70 |
| Female | 4 | 13 | 83 | 8 | 23 | 69 |
| Household education | ||||||
| < High School | 9 | 11 | 80 | 9 | 15 | 76 |
| High School | 4 | 13 | 83 | 7 | 20 | 73 |
| College | 3 | 13 | 84 | 8 | 24 | 68 |
| Income Level (FPL¶) | ||||||
| < 100% | 6 | 13 | 81 | 8 | 17 | 75 |
| 100%-199% | 4 | 13 | 83 | 8 | 20 | 72 |
| 200%-399% | 2 | 14 | 84 | 8 | 24 | 68 |
| >400% | 2 | 13 | 85 | 8 | 26 | 66 |
FPL, Federal Poverty Level
chi square test for each panel of nights × variable categories, within each age group, was statistically significant (p value < 0.05) except for gender (both age groups).
Boys and girls were similarly likely to have insufficient sleep (6.0 % vs. 5.6%, p = 0.28). Children in households earning < 100% of the federal poverty level (FPL) were more likely to have only 0-2 nights of sufficient sleep (Table 1). The results were similar when the analysis was repeated separately for children aged 6-11 and 12-17 years, with the exception that children aged 6-11 years in households with parents with college education were more likely to get 6-7 nights of sufficient sleep (Table 1).
Insufficient Sleep and Childhood Obesity
In bivariate analyses among children aged 6-11 years, those who had 0-2 nights of sufficient sleep had almost 2-fold higher odds of obesity compared with children who obtained 6-7 nights of sufficient sleep (Table 2). In contrast, among children aged 12-17 years, no similar association was found (Table 3). In fact, older children who obtained 3-5 rather than 6-7 nights of sufficient sleep had slightly lower odds of obesity.
Table 2.
Logistic regression analysis between nights of sufficient sleep and odds of obesity among 6- to 11-year-old children
| Odds of obesity* (N = 15.2 million)† |
||
|---|---|---|
| Nights of sufficient sleep | Unadjusted odds ratio (95% CI) | Adjusted odds ratio¶ (95% CI) |
| 0-2 nights | 1.7 (1.2-2.3) | 1.1 (0.8-1.6) |
| 3-5 nights | 1.0 (0.9-1.2) | 1.0 (0.9-1.2) |
| 6-7 nights | 1.0 | 1.0 |
compared with normal weight
weighted to yield national estimates
adjusted for race/ethnicity, gender, household education, and household income level.
Table 3.
Logistic regression analysis between nights of sufficient sleep and odds of obesity among 12- to 17-year-old children
| Odds of obesity* (N = 18.8 million)† |
||
|---|---|---|
| Nights of sufficient sleep | Unadjusted odds ratio (95% CI) | Adjusted odds ratio¶ (95% CI) |
| 0-2 nights | 1.0 (0.8-1.2) | 0.9 (0.8-1.2) |
| 3-5 nights | 0.8 (0.7-0.9) | 0.9 (0.8-1.0) |
| 6-7 nights | 1.0 | 1.0 |
compared with normal weight
weighted to yield national estimates
adjusted for race/ethnicity, gender, household education, and household income level.
After adjusting for children's sex, race/ethnicity, household income and household education, the association between fewer nights of sufficient sleep and obesity among 6- to 11-year-old children was no longer statistically significant. Similarly, after adjustment for sociodemographic factors, the weak tendency for older children with 3-5 nights rather than 6-7 nights of sufficient sleep to be obese was no longer statistically significant (Tables 2 and 3). Similar results were obtained when we compared children who are obese or overweight, rather than just obese, with healthy weight children.
DISCUSSION
In this large, nationally representative sample of over 81,000 children, we did not find a statistically significant association between obesity and reported nights of sufficient sleep, after adjustment for confounding sociodemographic factors. Although our findings contradict those of previous studies that have reported associations between insufficient sleep and childhood obesity,7,9,10 our study is distinguished from several of the previous studies by its large sample size, national representation, and ability to adjust simultaneously for several potential confounders—age, gender, race/ethnicity, household education, and income—each reported previously to have relationships to obesity,17,23 if not sleep as well.16,24 One French study of about 1000 five-year-olds, for example, did find an association between insufficient sleep and childhood obesity but did not adjust for several sociodemographic variables.25 Although cross-sectional data cannot establish causal relationships, the converse absence of an independent association between insufficient sleep and obesity has important implications for the hypothesis that insufficient or inadequate sleep promotes obesity in children.
We planned our study in advance to include adjustment for age, gender, race/ethnicity, education, and income, based on results of prior studies that implicated each as an important variable with respect to obesity17,26 or sleep.14,18,19,24,25,27 Bivariate analyses in our dataset largely confirmed these expectations suggesting that our proxy measures of child sleep and obesity were reasonably consistent with more objective measures and other analyses. In our study, Hispanics were more likely than others to have many nights of insufficient sleep, as minorities did in a previous study.24 Small gender differences did not reach significance in our study, as they did in a previous study within a national data set, which also indicated that adolescent boys in comparison to girls obtained fewer hours of sleep.16 As we found in our data, low socioeconomic status has been reported previously to have a significant association with deficient sleep among preschool children: those living in homes with incomes < 100 % FPL were more likely to have insufficient sleep than those children in homes with incomes > 400 % FPL.17
Relationships also clearly exist between sociodemographic factors and childhood obesity. A national survey of adolescents found lower levels of parental education to be associated with obesity.26 Obesity is more prevalent among preschool children of lower rather than higher socioeconomic status.17 Black and Hispanic children show higher rates of childhood obesity than do non-Hispanic white children.28,29
Limitations
Prior studies have assessed parental accounts of children's hours of sleep.9,10,13–15,25,30 The National Survey of Children's Health asked caregivers about their children's “nights of sufficient sleep” and not how many hours children slept. The three-part grouping of responses (0-2, 3-5, and 6-7 nights of sufficient sleep) was constructed by the authors for simplification of analysis and comparison of reasonable number of subjects, but exploratory analysis of different groupings did not generate different conclusions. To assess the external validity of the “sufficient sleep” question-item in the National Survey of Children's Health, we used data available from a concurrent 2004 National Sleep Foundation poll31 of parents of nearly 1500 children ≤ 10 years old. For children aged 6-11 years in the National Survey of Children's Health, 84% of caregivers thought that they received sufficient sleep, a result very similar to that found in the National Sleep Foundation poll, in which 80% of parents thought that their child received the right amount of sleep. Although our study did not include an objective measure of sleep duration, neither did previous studies that have suggested causal relationships between childhood obesity and insufficient sleep; all used subjective parental reports about the duration of sleep. Sleep duration estimates may be somewhat more or less informative than parental perception of sufficient sleep for the individual child, as measured in the present analyses.32
The lack of association in our adjusted models between insufficient sleep and obesity could potentially represent statistical over-adjustment that obscured a true relationship between these variables. This could occur, in particular, if age, gender, race/ethnicity, education, or income were an intermediate variable within a mechanistic pathway between sleep sufficiency and childhood obesity. This seems unlikely.
Finally, another limitation of our study was that height and weight and therefore BMI, were derived from caregiver reports. Although imperfect, such proxy measures are used by necessity in a population sample of this size. Moreover, the childhood obesity patterns observed by the authors in this sample as it relates to child age and race/ethnicity are consistent with other evaluations of childhood BMI at the national level in which anthropometric measures are recorded by objective third parties.29 This external validation offers support for the use of proxy measures of child BMI in the current study.
CONCLUSION
This study of a large nationally representative sample, after adjustment for several important potential socioeconomic confounders, failed to reveal any independent association between insufficient sleep and childhood obesity. Although parental perception of sufficient sleep was assessed, as opposed to sleep duration or objective measures, the current results run counter to those derived from smaller less representative, and less broadly controlled studies. These findings raise doubt about an as-yet-unproven causal role for insufficient sleep in the childhood obesity epidemic.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Chervin has served on the advisory board of Pavad Medical. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was supported by T32 training grant (HD007534) from the National Institute of Child Health and Human Development (NICHD).
REFERENCES
- 1.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288:1728–732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 4.Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC. Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch Intern Med. 2005;165:25–30. doi: 10.1001/archinte.165.1.25. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel K, Tasali E, Penev P, Cauter EV. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 6.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLos Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaput JP, Brunet M, Tremblay A. Relationship between short sleeping hours and childhood overweight//obesity: results from the/`Quebec en Forme/' Project. Int J Obes. 2006;30:1080. doi: 10.1038/sj.ijo.0803291. [DOI] [PubMed] [Google Scholar]
- 8.Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sekine M, Yamagami T, Handa K, et al. A dose-response relationship between short sleeping hours and childhood obesity: results of the Toyama Birth Cohort Study. Child Care Health Dev. 2002;28:163–70. doi: 10.1046/j.1365-2214.2002.00260.x. [DOI] [PubMed] [Google Scholar]
- 10.von Kries R, Toschke AM, Wurmser H, Sauerwald T, Koletzko B. Reduced risk of overweight and obesity in 5- and 6-y-old children by duration of sleep. Int J Obes Relat Metab Disord. 2002;26:710–6. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 11.Padez C, Mourao I, Moreira P, Rosado V. Prevalence and risk factors for overweight and obesity in Portuguese children. Acta Paediatr. 2005;94:1550–7. doi: 10.1080/08035250510042924. [DOI] [PubMed] [Google Scholar]
- 12.Bayer O, Rosario A, Wabitsch M, von Kries R. Sleep duration and obesity in children: is the association dependent on age and choice of the outcome parameter? Sleep. 2009;32:1183–9. doi: 10.1093/sleep/32.9.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: A prospective study from birth to 9.5 years. J Pediatr. 2004;145:20. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162:305–11. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020–9. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 16.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147:830. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 17.Mei Z, Scanlon KS, Grummer-Strawn LM, Freedman DS, Yip R, Trowbridge FL. Increasing prevalence of overweight among US low-income preschool children: the centers for disease control and prevention pediatric nutrition surveillance, 1983 to 1995. Pediatrics. 1998;101:e12. doi: 10.1542/peds.101.1.e12. [DOI] [PubMed] [Google Scholar]
- 18.Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: the role of sleep. Psychosom Med. 2002;64:337–44. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Pagel JF, Forister N, Kwiatkowki C. Adolescent sleep disturbance and school performance: the confounding variable of socioeconomics. J Clin Sleep Med. 2007;03:19–23. [PubMed] [Google Scholar]
- 20.Blumberg SJ OL, Frankel MR, Osborn L, Srinath KP, Giambo P. Design and operation of the National Survey of Children's Health, 2003. Statistics NCfH, ed1. Vital Health Stat. 2005 [PubMed] [Google Scholar]
- 21.Gurney JG, McPheeters ML, Davis MM. Parental report of health conditions and health care use among children with and without autism: National Survey of Children's Health. Arch Pediatr Adolesc Med. 2006;160:825–30. doi: 10.1001/archpedi.160.8.825. [DOI] [PubMed] [Google Scholar]
- 22.de Beer M, Hofsteenge GH, Koot HM, Hirasing RA, Delemarre-van de Waal HA, Gemke R. Health-related-quality-of-life in obese adolescents is decreased and inversely related to BMI. Acta Paediatr. 2007;96:710–14. doi: 10.1111/j.1651-2227.2007.00243.x. [DOI] [PubMed] [Google Scholar]
- 23.Wake M, Hardy P, Sawyer MG, Carlin JB. Comorbities of overweight/obesity in Australian preschoolers: a cross-sectional population study. Arch Dis Child. 2008;93:502–7. doi: 10.1136/adc.2007.128116. [DOI] [PubMed] [Google Scholar]
- 24.Spilsbury JC, Storfer-Isser A, Drotar D, et al. Sleep behavior in an urban US sample of school-aged children. Arch Pediatr Adolesc Med. 2004;158:988–94. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- 25.Locard E, Mamelle N, Billette A, Miginiac M, Munoz F, Rey S. Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes Relat Metab Disord. 1992;16:721–9. [PubMed] [Google Scholar]
- 26.Goodman E. The role of socioeconomic status gradients in explaining differences in US adolescents' health. Am J Public Health. 1999;89:1522–8. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu Z, Cheuk DKL, Lee SL. Clinical evaluation in predicting childhood obstructive sleep apnea. Chest. 2006;130:1765–71. doi: 10.1378/chest.130.6.1765. [DOI] [PubMed] [Google Scholar]
- 28.Whitaker RC, Orzol SM. Obesity among US urban preschool children: relationships to race, ethnicity, and socioeconomic status. Arch Pediatr Adolesc Med. 2006;160:578–84. doi: 10.1001/archpedi.160.6.578. [DOI] [PubMed] [Google Scholar]
- 29.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 30.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mindell J, Carskadon M, Chervin R, Meltzer L. Sleep in America Poll. Washington DC: National Sleep Foundation; 2004. [DOI] [PubMed] [Google Scholar]
- 32.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:e60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]