ABSTRACT
BACKGROUND
Although Native Americans experience substantial disparities in health outcomes, little information is available regarding healthcare delivery for this population.
OBJECTIVE
To analyze trends in ambulatory quality of care and physician reports of barriers to quality improvement within the Indian Health Service (IHS).
DESIGN
Longitudinal analysis of clinical performance from 2002 to 2006 within the IHS, and a physician survey in 2007.
PARTICIPANTS
Adult patients cared for within the IHS and 740 federally employed physicians within the IHS.
MAIN MEASURES
Clinical performance for 12 measures of ambulatory care within the IHS; as well as physician reports of ability to access needed health services and use of quality improvement strategies. We examined the correlation between physician reports of access to mammography and clinical performance of breast cancer screening. A similar correlation was analyzed for diabetic retinopathy screening.
KEY RESULTS
Clinical performance significantly improved for 10 of the 12 measures from 2002 to 2006, including adult immunizations, cholesterol testing, and measures of blood pressure and cholesterol control for diabetes and cardiovascular disease. Breast cancer screening rates decreased (44% to 40%, p = 0.002), while screening rates for diabetic retinopathy remained constant (51%). Fewer than half of responding primary care physicians reported adequate access to high-quality specialists (29%), non-emergency hospital admission (37%), high-quality imaging services (32%), and high-quality outpatient mental health services (16%). Breast cancer screening rates were higher at sites with higher rates of physicians reporting routine access to mammography compared to sites with lower rates of physicians reporting such access (46% vs. 35%, ρ = 0.27, p = 0.04). Most physicians reported using patient registries and decision support tools to improve patient care.
CONCLUSIONS
Quality of care has improved within the IHS for many services, however performance in specific areas may be limited by access to essential resources.
KEY WORDS: Indian health service, Native American, American Indian, racial disparities, quality of care, quality improvement
Native Americans experience higher overall mortality rates and decreased life expectancy compared to the general US population1. The epidemic of chronic disease and mental health disorders in Native communities plays a large role in the persistence of these disparities2–5. This excess disease burden places increased importance on the delivery of high-quality care to prevent complications and improve the overall health of this population6.
Unfortunately, data are limited regarding the quality of health care for Native Americans7. The Indian Health Service (IHS) is a federal agency that provides health care services for a substantial proportion of the Native American population. Recent Congressional requirements for the IHS to measure and report clinical performance have prompted an increase in quality improvement efforts across the organization8, but data on the impact of these efforts are limited.
Quality improvement within the IHS may be hampered by a shortage of funding to provide needed health services and by limited availability of clinicians9–11. Little is known regarding the potential impact of limited resources on the quality of care for Native Americans. We conducted this study to analyze recent trends in the quality of care within the IHS and to assess the perceptions of primary care physicians regarding barriers to the delivery of high-quality care within this system.
METHODS
Study Setting
The IHS is a federal agency that provides health care to 1.9 million Native Americans, representing approximately 50% of the Native population10. The overall budget ($4.05 billion) supports expenditures per person that are substantially less than all other federal health care programs11.
The current Indian Health System consists of three branches: 1) the federally operated direct care system (the “IHS”), 2) independent tribally operated health care facilities, and 3) a small urban health care program. Tribally operated sites function through Public Law 93-638 as financially independent entities supported by funds allocated from the federal government, and represent 55% of the overall budget. Federally operated sites receive 45% of the overall budget and function as part of an integrated health system with funds pooled at the national level12,13.
The health care services provided by the federally operated IHS sites include comprehensive primary care, some specialty services, and prescription drug coverage. Contract health service funds are used to provide services not routinely available within IHS facilities, including subspecialty care. These funds are limited, with medical prioritization occurring based on clinical urgency14.
We focused our analysis on the federally operated IHS sites as they constitute one of the largest integrated health care delivery systems in the country, focused on care for Native Americans. We did not include any tribally operated clinics participating in the Public Law 93-638 program.
Clinical Performance Measures
We assessed clinical performance for the years 2002 through 2006 using data obtained from the IHS national clinical reporting system, which captures data on all patients receiving care in federally operated IHS sites12. Clinical data were abstracted electronically from datasets that include all laboratory and radiology results, and diagnosis and procedure codes. We used these data to assess clinical performance in the areas of preventive services, diabetes care, and cardiovascular disease care (Table 1). Identification of diagnoses, laboratory results, and procedures were based on Current Procedure Terminology (CPT) and International Classification of Disease (ICD)-9 codes consistent with Health Plan Employer Data and Information Set (HEDIS) standards15. We used county of residence to categorize patients as residing in rural or urban settings according to metropolitan statistical areas16.
Table 1.
Definitions of Clinical Performance Measures
| Measure | Denominator | Numerator |
|---|---|---|
| Breast cancer screening | • Females 52–64 years old | • Receipt of mammogram within the prior 2 years |
| • ≥2 outpatient visits within the past 3 years | • Refusal of exam within the prior 12 months | |
| • No history of bilateral mastectomy or two separate unilateral mastectomies. | ||
| Influenza vaccination | • ≥65 years old | • Receipt of vaccine within the prior 12 months |
| • ≥2 outpatient visits within the past 3 years | • Refusal of vaccination within the prior 12 months | |
| Pneumococcal vaccination | • ≥65 years old | • Receipt of vaccine at any time prior to current reporting year |
| • ≥2 outpatient visits within the past 3 years | • Refusal of vaccination within the prior 12 months | |
| Cholesterol screening | • 35–75 years old | • Receipt of total cholesterol exam within the prior 5 years |
| • ≥2 outpatient visits within the past 3 years | ||
| Diabetes | • 18–75 years old | • Receipt of retinal exam within the prior 12 months (including office visits in ophthalmology, optometry or tele-ophthalmology retinal evaluation clinics) |
| • ≥2 outpatient visits within the past year | • Receipt of LDL cholesterol exam within the prior 12 months | |
| • ≥2 outpatient diagnoses of diabetes ever, with the first diagnosis occurring at least 12 months prior | • Receipt of HbA1c exam within the prior 12 months | |
| • LDL < 100 mg/dL based on most recent value (missing values for current reporting year considered ≥100 mg/dL) | ||
| • HbA1c < 7% based on most recent value (missing values for current reporting year considered >7%) | ||
| • Blood pressure < 130/80 mmHg based on average of three (or two) most recent non-emergency room blood pressures during the reporting period (if zero or one blood pressures available, blood pressure assumed to be ≥130/80 mmHg) | ||
| • Receipt of LDL cholesterol exam within the prior 12 months | ||
| Cardiovascular disease | • 18–75 years old | • LDL < 100 mg/dL (missing values for current reporting year considered >100 mg/dL) |
| • ≥2 outpatient visits within the past 3 years | ||
| • Diagnosis of acute myocardial infarction, coronary angioplasty, coronary artery bypass graft, coronary artery disease, stable angina, peripheral arterial disease, stroke, abdominal aortic aneurysm at least 12 months prior |
We used data on quality of ambulatory care among health plans participating in the National Committee for Quality Assurance (NCQA) HEDIS reporting program for Medicaid and Medicare as benchmarks for trends in care17. These data differ from the IHS data in two important ways. First, NCQA-reported data rely primarily on patient surveys (adult flu shots) or claims data rather than the electronic medical record data used by the IHS. Second, the eligible denominator for the breast cancer screening measure in the IHS included women ages 52 to 65 years for all study years; however for the NCQA data it changed from 52 to 69 years in 2002-2006 to 40 to 69 years in 2007.
Physician Survey
We surveyed all 740 federally employed physicians who were clinically active at federally operated IHS sites during October 2007. The survey instrument was delivered using an initial paper mailing and an electronic mail invitation to complete the survey online; followed by a repeat paper mailing and electronic mailing to non-responders 3 weeks later, thereby achieving a 70% response rate. The survey instrument focused on ability to access needed health services and use of quality improvement strategies, and was closely modeled on the Community Tracking Study18–21. We focused on survey items that analyze access to care, as prior analyses have indicated that access to resources is a significant barrier to health care delivery in the IHS22,23.
The supply of essential services was assessed by six questions regarding availability of “subspecialists of high quality”, “nonemergency hospital admissions”, “high quality diagnostic imaging services”, “high quality outpatient mental health services”, “screening mammography”, and “screening diabetic eye examinations”. All responses were collected on a 5-point Likert scale from “almost always” to “never” available; and we defined adequate access to all services as a response of “almost always”. Physicians also reported what types of quality improvement activities were occurring within their clinic for diabetes management.
Physicians responded to the statement “In general, would you say that the complexity or severity of patients’ conditions for which you are currently expected to provide care without specialty referral is” on a 5-point scale ranging from “much greater than it should be” to “much less than it should be”. Barriers to the receipt of specialty care were assessed through two questions of the form “Thinking of access to subspecialists, how important are the following barriers to care?”, with the barriers including “lack of qualified service providers within geographic proximity” and “lack of Indian Health Service funding to support provision of recommended specialty care”. These responses were collected using a 4-point Likert scale ranging from “very important” to “not at all important”. Finally, physicians responded to the statement “It is possible to provide high quality care to all of my patients” using a 5-point Likert scale ranging from “strongly agree” to “strongly disagree”.
Data Analysis
We analyzed trends in clinical performance measures within the IHS by fitting logistic regression models with performance of the target measure as the dependent variable and year as the primary independent variable, after adjusting the standard errors for clustering of patients by health center using generalized estimating equations. We fit multivariable logistic regression models to analyze rural residence as a predictor of clinical performance in 2006 for each of the 12 measures. We focused on rural residence as the IHS has historically focused on delivering care in remote rural areas. The primary independent variable was rural residence, with additional covariates including geographic residence according to US Census divisions (Pacific, Mountain, West North Central, and South), and patient age and sex.
We calculated the Spearman correlation coefficient between the proportion of eligible patients receiving screening mammography or diabetic eye exams within an individual health center in 2006 and the proportion of primary care physicians reporting that each service was “almost always” available at that health center. For illustrative purposes, we defined three sets of clinics based on the proportion of physicians at each clinic reporting that either mammography or dilated eye exams were “almost always” available. This proportion was divided into three groups: <25th percentile (low access clinics), 25th to 75th percentile (moderate access clinics), and >75th percentile (high access clinics); and we calculated the breast cancer or diabetic retinopathy screening rates within each set of clinics.
All analyses were performed using SAS version 9.1. The study protocol was approved by the human studies committees of Brigham and Women’s Hospital and the Indian Health Service.
RESULTS
Clinical Performance
Clinical performance improved significantly from 2002 to 2006 for 10 of the 12 performance measures, including preventive services and chronic disease management (Table 2). These significant gains in chronic disease care were achieved despite the substantial relative increase in prevalence of both diabetes (23%) and cardiovascular disease (46%) over the 5-year study period. Notable exceptions to this trend of improvement included breast cancer screening rates, which decreased significantly from 44% to 40%; and rates of diabetic retinopathy screening, which remained unchanged at 51%.
Table 2.
Trends in Clinical Performance Within the Indian Health Service
| 2002 | 2003 | 2004 | 2005 | 2006 | p† | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N* | % | N* | % | N* | % | N* | % | N* | % | ||
| Preventive services | |||||||||||
| Breast cancer screening | 21,652 | 44% | 22,812 | 42% | 23,965 | 40% | 25,057 | 39% | 26,073 | 40% | 0.002 |
| Influenza vaccination | 26,020 | 53% | 26,821 | 54% | 27,809 | 58% | 29,084 | 65% | 30,222 | 62% | <0.001 |
| Pneumococcal vaccination | 26,020 | 68% | 26,821 | 71% | 27,809 | 74% | 29,084 | 77% | 30,222 | 80% | <0.001 |
| Cholesterol screening | 153,975 | 49% | 158,641 | 53% | 163,843 | 55% | 169,065 | 58% | 172,196 | 61% | <0.001 |
| Diabetes care | |||||||||||
| Retinopathy screening | 40,232 | 51% | 42,718 | 51% | 45,503 | 50% | 47,704 | 51% | 49,513 | 51% | 0.93 |
| HbA1c testing | 74% | 77% | 80% | 80% | 81% | <0.001 | |||||
| LDL cholesterol testing | 46% | 51% | 55% | 58% | 63% | <0.001 | |||||
| HbA1c <7% | 20% | 23% | 25% | 28% | 29% | <0.001 | |||||
| LDL cholesterol <100 mg/dl | 20% | 24% | 26% | 30% | 34% | <0.001 | |||||
| BP <130/80 mmHg | 35% | 36% | 37% | 38% | 39% | <0.001 | |||||
| Cardiovascular disease | |||||||||||
| LDL cholesterol testing | 6,513 | 50% | 7,209 | 54% | 7,941 | 59% | 8,437 | 61% | 9,524 | 64% | <0.001 |
| LDL cholesterol <100 mg/dl | 25% | 28% | 30% | 34% | 37% | <0.001 | |||||
*Number of patients eligible for each measure during each measurement year
†p value for 5 year trend adjusted for clustering of patients within sites
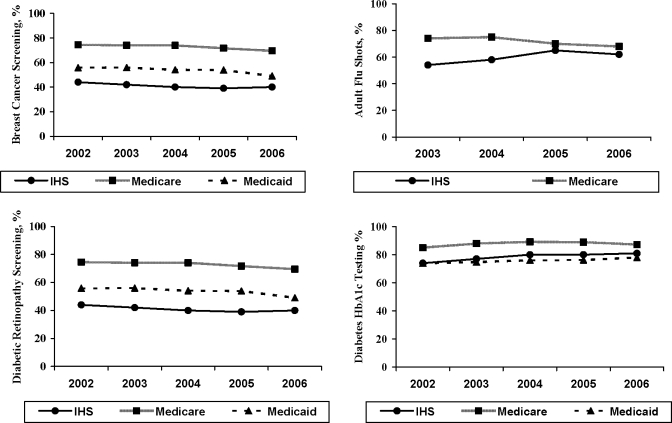
Five-year trends in breast cancer and diabetic retinopathy screening rates remained relatively flat within Medicare, Medicaid, and the IHS; though rates within the IHS were consistently lower than those reported by health plans participating in Medicaid, and were nearly half the rates reported by health plans participating in Medicare (Fig. 1). In contrast, rates of flu shots for elderly adults and HbA1c testing for adults with diabetes were more similar between Medicare and the IHS.
Figure 1.
National trends in clinical performance among Indian Health Service, Medicare, and Medicaid from 2002 through 2006. Five year trends in clinical performance for four selected ambulatory services, including cancer screening, flu shots for adults, and diabetes care. Medicare and medicaid data derived from the national committee for quality assurance State of Health Care Quality Report.
Rural residence was not a significant predictor of clinical performance for 10 of the 12 measures in 2006, with breast cancer screening rates slightly higher (odds ratio (OR) 1.07, 95% confidence interval (CI) 1.00 – 1.14) and annual hemoglobin A1c testing rates slightly lower (OR 0.96, 95% CI 0.94 – 0.99) in rural areas compared to urban areas.
Access to Essential Health Services
In our physician survey we received responses from 517 physicians in 18 states. We limited our analyses to 366 primary care physicians as we were focused on understanding the barriers perceived by generalist physicians within the IHS (Table 3). The median number of respondents across 60 clinical sites was 3.0 (interquartile range 2 – 8). Most of these primary care physicians were white, and 14% were American Indian/Alaska Native.
Table 3.
Characteristics of 366 Responding Primary Care Physicians
| Frequency (%) | |
|---|---|
| Personal Demographics | |
| Mean age, years (± standard deviation) | 47.1 (± 9.4) |
| Male | 209 (59) |
| Race/ethnicity* | |
| White | 261 (78) |
| American Indian/ Alaska Native | 48 (14) |
| Hispanic | 32 (9) |
| Asian | 26 (8) |
| Black | 13 (4) |
| Native Hawaiian/ Pacific Islander | 1 (1) |
| Other | 1 (1) |
| Clinical Background | |
| Primary clinical specialty | |
| Family practice | 215 (59) |
| General pediatrics | 76 (21) |
| Internal medicine | 64 (17) |
| Combined medicine-pediatrics | 11 (3) |
| Board certified | 302 (83) |
| Clinical practice | |
| Geographic region | |
| West | 284 (78) |
| Midwest | 42 (11) |
| South | 40 (11) |
| Median years working in IHS (interquartile range) | 8.0 (3 to 15) |
| Clinical sessions per week | |
| 1 to 3 | 60 (17) |
| 4 to 7 | 138 (39) |
| 8 to 10 | 152 (43) |
*Data missing in 31 (8%) respondents
Physicians reported relatively low rates of adequate access to high-quality specialists (29%), non-emergent hospital admission (37%), high-quality diagnostic imaging (32%), and high-quality outpatient mental health services (16%). The majority (59%) of primary care physicians felt that the complexity of conditions managed without specialty referral was either much greater (16%) or somewhat greater (43%) than it should be. While a lack of specialty providers within geographic proximity was cited by 32% of physicians as a “very important” barrier, a much larger majority (63%) felt that a lack of IHS funding to support provision of care through subspecialists was a “very important” barrier.
Correlation Between Physician Reports of Access and Quality
The proportion of primary care physicians reporting that preventive services were “almost always” available was relatively low for screening mammography (54%) and diabetic eye exams (60%). Clinical performance varied substantially across the sites for breast cancer screening (interquartile range 31% to 55%) and diabetic retinopathy screening (interquartile range 44% to 58%). Clinics with a higher proportion of physicians reporting that screening mammography was “almost always” available had a higher breast cancer screening rate (46%) than those clinics with the lowest proportion of physicians reporting such access (35%), with a significant correlation at the health center level (ρ = 0.27, p = 0.04). The magnitude of this effect was less pronounced for performance of diabetic eye exams (Table 4).
Table 4.
Correlation Between Primary Care Physician Reported Access and Clinical Performance
| Clinical Measure | Low Access Clinics* | Moderate Access Clinics* | High Access Clinics* | Spearman Correlation† | ||||
|---|---|---|---|---|---|---|---|---|
| Nclinic | Screening Rate, % | Nclinic | Screening Rate, % | Nclinic | Screening Rate, % | ρ | P value | |
| Breast cancer screening | 15 | 35% | 25 | 43% | 20 | 46% | 0.27 | 0.04 |
| Diabetic eye exams | 15 | 50% | 27 | 48% | 18 | 55% | 0.24 | 0.07 |
*Clinics separated into three groups based on the proportion of physicians at each clinic reporting the targeted health service is “almost always” available. This proportion was divided into 3 groups: <25th percentile (low access clinics), 25th to 75th percentile (moderate access clinics), and >75th percentile (high access clinics)
†Spearman correlation coefficient between proportion of physicians reporting service “almost always” available and performance rate for each clinic
Quality Improvement Strategies
Approximately three-quarters (72%) of primary care physicians agreed strongly or somewhat that they were able to provide high-quality care to their patients. Most physicians reported using patient registries (73%), decision support tools (61%), patient outreach (56%), and physician feedback (53%) for diabetes management. Nearly one-third of physicians reported the use of group visits (28%), and a majority (59%) enlisted the services of community health workers for diabetes care. Many primary care physicians agreed strongly or somewhat that health information technology (87%) can improve the quality of care in the IHS.
DISCUSSION
We found that clinical performance for preventive services and chronic disease management improved within the IHS for most performance measures. Primary care physicians reported substantial barriers in access to essential health services, and these reports were modestly correlated with lower performance on some measures of clinical quality. We did not find substantial differences in quality between rural and urban settings, confirming prior analyses within the IHS24, and suggesting that an integrated delivery system can ensure equivalent care across varied health care settings.
Substantial disparities in clinical performance persisted between the IHS and health plans participating in Medicare and Medicaid, particularly for screening mammography and diabetic retinopathy screening, two measures for which the IHS ranks below the 25th percentile of these health plans nationally. However, the IHS performed better than many health plans for other measures of diabetes care including annual HbA1c and LDL cholesterol testing, and the IHS performance exceeded the 90th percentile for adult pneumococcal vaccination25.
The Medicare program represents a national benchmark for quality of care across a variety of delivery systems26, and ultimately should represent a minimum achievement target for the IHS. Comparisons to the Medicaid program provide additional insight as Medicaid is focused on ensuring care for underserved low-income populations, and its funding levels more closely reflect those of the IHS. Our data suggest that quality of care within the IHS parallels that within the Medicaid program more closely. This observation may reflect similarity in patient characteristics or funding levels, though it is important to note that Medicaid expenditures per person are higher than those within the IHS11.
We found that primary care physicians caring for Native American patients reported suboptimal access to essential health services to a much greater extent than physicians caring for either white or black patients19,20. The IHS remains significantly underfunded, receiving only about half of the funding needed to adequately care for the patients it serves11,27. This budget shortfall could lead directly to the type of stark resource limitations reported by the physicians in this study. For example, 76% of primary care physicians caring for black patients report adequate access to subspecialists19, compared to 29% of physicians in the IHS. As a result, a majority (58%) of primary care physicians within the IHS report that complexity of clinical conditions managed without specialty input was greater than it should be, compared to only 26% of physicians caring for black and Hispanic patients20. These physician reports are further substantiated by the increasing number of out-of-network patient services denied due to lack of funding within the IHS, which rose by 68% from 2003 to 2006 (T. Cullen, written communication, August 6, 2009). Despite reporting substantial challenges to delivering care, a majority of physicians felt they were able to deliver high quality care. This divergence is likely related to physicians defining high quality care outside of the domains of care assessed in our study28,29.
As the IHS received a 13% increase in funding in FY201030, it is important to understand how such a substantial increase in funding might be best utilized. Our findings indicate several areas on which to focus, including increasing access to subspecialty and imaging services, physician recruitment, expanded use of health information technology, and improved chronic disease management strategies.
The importance of the first two areas is highlighted by our survey findings and clinical performance data. Physicians’ reports of inadequate access were significantly correlated with low clinical performance for mammography and a similar trend for diabetic eye exams. These findings likely reflect a scarcity of equipment or trained personnel to perform screening mammography and dilated eye exams. Access to these and other types of specialty services23 could most directly be addressed through contract health services, which received an 18% increase in the IHS FY2010 budget, but will likely require additional increases to meet the substantial need. Additional work is also needed to understand how to improve screening rates among clinics already reporting good access to essential services, highlighted by the suboptimal rates of mammography and diabetic eye exams among clinics with physicians reporting good access to these services. This effort will likely involve an examination of the role of social, community, and other patient factors that relate to delivering high quality care.
Recruiting qualified personnel to work in the IHS is also important, and the IHS currently has vacancy rates of 21% for physicians10. Promoting the training of Native American health professionals who may be more inclined to work in these settings is one strategy to address this unmet need31. Our survey identified that 14% of physicians working within the IHS were Native American, compared with less than 1% of medical students who are Native American32.
Our data also suggest that expanding the use of health information technology represents a promising strategy. The low rates of screening diabetic eye exams are particularly troubling given the burden of disease among this population. The use of a tele-ophthalmology program has increased performance of screening diabetic eye exams within the IHS, ultimately resulting in increased rates of laser therapy to prevent blindness without the need to recruit additional ophthalmologists33. This and other health information technology-based strategies such as dissemination of an advanced electronic health record13 represent attractive solutions to overcome both the financial and geographic barriers faced by the IHS.
Our study has some limitations. We presented national comparison data for the IHS, but were not able to adjust clinical performance rates for differences in age distributions between the IHS patient population and the Medicare and Medicaid populations. We also did not analyze care among tribally operated facilities. While the option to convert to tribally operated management has existed since 1975, many clinics have transitioned only in recent years9, and many of the issues identified by physicians in our survey are likely independent of this administrative change.
In addition, while the IHS provides health care for a substantial proportion of Native Americans in the United States, many Native Americans receive care outside of this system, particularly in urban areas. Future work is needed to better understand the state of health care delivery for these other segments of the Native American population. Finally, while we analyzed care according to rural residence, we were not able to identify whether patients resided on tribal reservations, which may present unique challenges to health care delivery such as limited access to electricity, indoor plumbing or telephone services.
In this large-scale assessment of care delivered within the Indian Health Service, we identified both significant quality improvement along with persistent barriers to delivering high-quality care to Native American patients. While the Indian Health Service is actively engaged in a variety of quality improvement programs, true advances in health care delivery and health outcomes may ultimately be limited by resource constraints. Further research is needed to understand and address the long-term impact of these constraints on the health of Native Americans.
Acknowledgements
Dr. Sequist was funded by the Robert Wood Johnson Foundation through the Harold Amos Minority Faculty Development Program and the Network for Multicultural Research on Health and Healthcare, Department of Family Medicine, David Geffen School of Medicine, U.C.L.A. Dr. Ayanian was supported by the Health Disparities Research Program of Harvard Catalyst | The Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, the National Center for Research Resources, or the National Institutes of Health. This research was presented at the Annual Research Meetings of the Society of General Internal Medicine (Miami, FL) and Academy Health (Chicago, IL) in 2009. We would like to thank the Indian Health Service physicians and their patients for participating in this study.
Conflict of Interest None.
References
- 1.Indian Health Disparities. Indian health service. Available at: http://info.ihs.gov/Disparities.asp. Accessed November 8, 2010.
- 2.Narva AS, Sequist TD. Reducing health disparities in American Indians with chronic kidney disease. Semin Nephrol. 2010;30:19–25. doi: 10.1016/j.semnephrol.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control Prevalence of heart disease–United States, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:113–118. [PubMed] [Google Scholar]
- 4.Centers for Disease Control Diabetes prevalence among American Indians and Alaska Natives and the overall population–United States, 1994–2002. MMWR Morb Mortal Wkly Rep. 2003;52:702–704. [PubMed] [Google Scholar]
- 5.Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, Manson SM. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. Am J Psychiatry. 2005;162:1723–1732. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]
- 6.Lillie-Blanton M, Roubideaux Y. Understanding and addressing the health care needs of American Indians and Alaska Natives. Am J Public Health. 2005;95:759–761. doi: 10.2105/AJPH.2005.063230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Healthcare Quality and Disparities Reports. Agency for healthcare research and quality. Available at: http://www.ahrq.gov/qual/qrdr08.htm. Accessed November 8, 2010. 2008
- 8.Wilson C, Gilliland S, Cullen T, Moore K, Roubideaux Y, Valdez L, Vanderwagen W, Acton K. Diabetes outcomes in the Indian health system during the era of the special diabetes program for Indians and the government performance and results act. Am J Public Health. 2005;95:1518–1522. doi: 10.2105/AJPH.2004.053710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katz RJ. Addressing the health care needs of American Indians and Alaska Natives. Am J Public Health. 2004;94:13–14. doi: 10.2105/AJPH.94.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Year 2009 Profile. Indian health service. Available at: http://info.ihs.gov/Profile09.asp. Accessed November 8, 2010.
- 11.Roubideaux Y. Beyond Red Lake–the persistent crisis in American Indian health care. N Engl J Med. 2005;353:1881–1883. doi: 10.1056/NEJMp058095. [DOI] [PubMed] [Google Scholar]
- 12.Sequist TD, Cullen T, Ayanian JZ. Information technology as a tool to improve the quality of American Indian health care. Am J Public Health. 2005;95:2173–2179. doi: 10.2105/AJPH.2004.052985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sequist TD, Cullen T, Hays H, Taualii MM, Simon SR, Bates DW. Implementation and use of an electronic health record within the Indian health service. J Am Med Inform Assoc. 2007;14:191–197. doi: 10.1197/jamia.M2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Contract Health Services. Indian health service. Available at: http://info.ihs.gov/CHS.asp. Accessed November 8, 2010.
- 15.National Center for Quality Assurance. HEDIS 2006: Technical specifications; 2006.
- 16.U.S. Census Bureau. Metropolitan and micropolitan statistical areas. Available at: http://www.census.gov/population/www/metroareas/metrodef.html. Accessed November 8, 2010.
- 17.National Committee for Quality Assurance. The state of health care quality. Washington, DC 2007. Available at: http://www.ncqa.org/tabid/136/Default.aspx. Accessed November 8, 2010.
- 18.Kemper P, Blumenthal D, Corrigan JM, Cunningham PJ, Felt SM, Grossman JM, Kohn LT, Metcalf CE, St Peter RF, Strouse RC, Ginsburg PB. The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry. 1996;33:195–206. [PubMed] [Google Scholar]
- 19.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 20.Reschovsky JD, O’Malley AS. Do primary care physicians treating minority patients report problems delivering high-quality care? Health Aff. 2008;27:w222–w231. doi: 10.1377/hlthaff.27.3.w222. [DOI] [PubMed] [Google Scholar]
- 21.St Peter RF, Reed MC, Kemper P, Blumenthal D. Changes in the scope of care provided by primary care physicians. N Engl J Med. 1999;341:1980–1985. doi: 10.1056/NEJM199912233412606. [DOI] [PubMed] [Google Scholar]
- 22.Sequist TD, Narva AS, Stiles SK, Karp SK, Cass A, Ayanian JZ. Access to renal transplantation among American Indians and Hispanics. Am J Kidney Dis. 2004;44:344–352. doi: 10.1053/j.ajkd.2004.04.039. [DOI] [PubMed] [Google Scholar]
- 23.Sequist TD, Zaslavsky AM, Galloway JM, Ayanian JZ. Cardiac procedure use following acute myocardial infarction among American Indians. Am Heart J. 2006;151:909–914. doi: 10.1016/j.ahj.2005.05.029. [DOI] [PubMed] [Google Scholar]
- 24.Moore K, Roubideaux Y, Noonan C, Goldberg J, Shields R, Acton K. Measuring the quality of diabetes care in urban and rural Indian health programs. Ethn Dis. 2006;16:772–777. [PubMed] [Google Scholar]
- 25.National Committee for Quality Assurance. Benchmarks and thresholds: 2006 MCO accreditation. National committee for quality assurance. Available at: http://www.ncqa.org/tabid/422/Default.aspx. Accessed November 8, 2010.
- 26.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353:692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 27.Westmoreland TM, Watson KR. Redeeming hollow promises: the case for mandatory spending on health care for American Indians and Alaska Natives. Am J Public Health. 2006;96:600–605. doi: 10.2105/AJPH.2004.053793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colosia AD, Peltz G, Pohl G, Liu E, Copley-Merriman K, Khan S, Kaye JA. A review and characterization of the various perceptions of quality cancer care. Cancer. 2010. [DOI] [PMC free article] [PubMed]
- 29.Cooperberg MR, Birkmeyer JD, Litwin MS. Defining high quality health care. Urol Oncol. 2009;27:411–416. doi: 10.1016/j.urolonc.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 30.IHS Profile. Indian health service. Available at: http://info.ihs.gov/Profile09.asp. Accessed November 8, 2010. 2009
- 31.Sequist TD. Paving the way–providing opportunities for Native American students. N Engl J Med. 2005;353:1884–1886. doi: 10.1056/NEJMp058218. [DOI] [PubMed] [Google Scholar]
- 32.Sequist TD. Health careers for Native American students: challenges and opportunities for enrichment program design. J Interprof Care. 2007;21(Suppl 2):20–30. doi: 10.1080/13561820601086841. [DOI] [PubMed] [Google Scholar]
- 33.Wilson C, Horton M, Cavallerano J, Aiello LM. Addition of primary care-based retinal imaging technology to an existing eye care professional referral program increased the rate of surveillance and treatment of diabetic retinopathy. Diab Care. 2005;28:318–322. doi: 10.2337/diacare.28.2.318. [DOI] [PubMed] [Google Scholar]