ABSTRACT
BACKGROUND
In the United States, 1 in 6 women report a lifetime prevalence of sexual assault. Few population-based studies have examined the association between sexual assault victimization on health care utilization and unhealthy behaviors.
OBJECTIVE
To assess the relationship between experiencing sexual assault and health care utilization and unhealthy behaviors among a state-wide representative sample of Connecticut adults.
DESIGN AND PARTICIPANTS
Cross-sectional study of 4183 Connecticut residents who responded to sexual assault questions in the 2005 telephone-based Connecticut State Behavioral Risk Factor Surveillance System (CT-BRFSS).
MAIN MEASURES
Health care utilization and unhealthy behaviors among residents reporting sexual assault.
RESULTS
Approximately one out of eleven Connecticut adults (9.4%) experienced sexual assault at some point in their life. Among adults aged 65 years and older, 4.3% reported sexual assault compared to 11.2% of adults aged 18-34 years, (p < 0.001). Among men, 3.7% reported sexual assault victimization versus 14.6% of women, (p < 0.001). After controlling for sociodemographic factors, victims of forced sexual assault were less likely to have seen a physician in the previous 12 months for a routine checkup (Odds ratio [OR]: 1.49, 95%: 1.07–2.07) and more likely to report being unable to see a doctor because of cost (OR: 2.72, 95% CI: 1.70–4.34). Victims were more likely to currently smoke (OR: 2.01, 95% CI: 1.34–3.00) and drink heavily (OR: 3.30, 95% CI: 2.01–5.42) than those reporting no sexual assault.
CONCLUSIONS
For Connecticut adults, sexual assault victimization was associated with infrequent usage of some primary care health services and higher risks of unhealthy behaviors. Increased community-level interventions and public health outreach programs are needed to provide health-care services to this high-risk group.
KEY WORDS: sexual assault, health care utilization, health behavior
INTRODUCTION
Sexual assault or rape is a non-consensual act involving the use or threat of force in vaginal, anal, or oral intercourse.1 Some estimates place lifetime prevalence of sexual assault as high as 18% among women and 3% of men in the United States. Although similar to intimate partner violence (IPV), sexual assault may involve an assailant who is unknown to the victim and pertains specifically to forced sexual acts.1 Recognized as a significant global2 and domestic public health concern, victims of IPV generally, and sexual assault specifically, expend more health care costs than non-victims.3 Intimate partner violence in the United States alone is associated with an estimated annual cost of $8.3 billion dollars.4
Recent studies on sexual assault have documented not only the immediate health consequences of the assault, but how injuries and psychosocial stressors experienced during the assault can lead to chronic medical conditions, including smoking, alcohol abuse, chronic pain syndromes, asthma, heart disease, and arthritis among victims.5–10 Few studies, however, have documented the associations between sexual assault and unhealthy behaviors in population-based studies. Additionally, it is unclear how the experience of sexual assault may be associated with health-care utilization trends outside the immediate post-assault time period. Early studies on victimization documented high rates of all types of health services utilization, including emergency room, primary care, and community health center visits.11 More recent studies described a mixed picture of increased utilization of emergency and urgent care resources and decreased utilization of primary care or routine health services.8 Furthermore, most studies on the associations between health care utilization and sexual assault use convenience samples derived from emergency rooms,12,13 HMO populations3 or clinics and community-based health centers.14–18 Since sexual assault victims infrequently access health services, population-based studies are needed to examine this phenomenon in more detail. Connecticut, one of the wealthiest states in the country, has a paucity of evidence on the prevalence and sociodemographic correlates of sexual assault in the general adult population. Given this, the goals of our study were to: 1) describe the prevalence of sexual assault among the general adult population in Connecticut using the Behavior Risk Factor Surveillance System (BRFSS)19,20; 2) determine the unique sociodemographic correlates associated with this assault; 3) examine the patterns of health care utilization among victims of sexual assault in Connecticut; and 4) describe which negative health behaviors were associated with sexual assault victimization.
METHODS
Data Source
Our study involved participants surveyed by the Connecticut Behavioral Risk Factor Surveillance System (CT-BRFSS) in 2005.21 Created in 1984, the BRFSS is an ongoing, state-based, random-digit dialed telephone survey of non-institutionalized adults aged 18 years or older in the United States that annually tracks health behaviors and medical conditions. Trained interviewers administer identical core questionnaires to an independent probability sample of adults. Data from all states and the District of Columbia are pooled to produce nationwide estimates. The BRFSS methods, including the reliability, validity, and methodology of the survey are described elsewhere.19,20,22,23 The CT-BRFSS surveyed a total 5,254 adults in 2005. This included a subset of individuals (n = 4,183) who responded to a set of sexual assault questions in addition to core questions regarding health care utilization and unhealthy behaviors. This subset of individuals represented those that were willing to answer questions regarding sexual assault and sexual violence. The remainder of the sample refused to answer these questions (n = 1071).
To provide a meaningful comparison group, we also evaluated the prevalence of sexual assault in 19 other states that utilized the BRFSS Module on Sexual Assault in 2005. These states include Arizona, Colorado, Delaware, Florida, Hawaii, Idaho, Mississippi, Missouri, Nevada, Ohio, Oklahoma, Puerto Rico, Rhode Island, South Carolina, Tennessee, Vermont, Virgin Islands, Virginia, and Wisconsin. In aggregate, over 91,281 individuals were asked questions regarding sexual assault in these 19 states.24
Study Variables
A victim of attempted sexual assault in the survey was defined as someone who responded “Yes” to the following question: “Has anyone attempted to have sex with you after you said or showed that you didn’t want to or without your consent, but sex did not occur.” A victim of realized sexual assault was defined as someone who responded “Yes” to : “Has anyone ever had sex with you after you said or showed that you didn’t want them to or without your consent?” If a participant reported sexual assault, they were provided additional information regarding community resources and counseling services. We defined the lifetime prevalence of sexual assault broadly to include either attempted or realized sexual assault.
We assessed study participants’ access to health care with a series of four questions. First, respondents reported if they had any health care plan, which was defined broadly to include private health insurance, prepaid plans such as HMOs, and government plans such as Medicare or Medicaid. Second, participants described if they had at least one person that they identified as their “personal doctor or health care provider” and if in the past 12 months they needed to see a doctor but could not because of cost. Finally, participants reported whether they went for greater than 12 months without a routine health checkup.
We assessed negative health behaviors through a series of six questions regarding alcohol consumption, smoking history, fruit and vegetable intake, and adequate physical activity. We defined binge drinking as the consumption of five or more alcoholic drinks on at least one occasion over the last month. One drink was either 12 ounces of beer, a four ounce glass of wine, or a shot of liquor. At-risk or heavier drinking was defined as an average of greater than one drink daily for women or greater than two drinks daily for men over the last 30 days. These definitions correspond to definitions of at-risk drinking and binge drinking defined by the CDC and other large epidemiological studies on the negative health effects of alcohol.25,26 High risk HIV behavior was a composite variable that included behavior which would place the participant at increased risk for contracting HIV, including IVDU, prostitution, anal intercourse without a condom, and treatment for a sexually transmitted infection in the past year. Individuals with unhealthy dietary habits were defined as those who consumed fewer than 5 servings of fruits and/or vegetables a day. This corresponds to the WHO recommended intake of a minimum of 400 g of fruit and vegetables needed daily to prevent chronic disease and address micronutrient deficiencies.27 Finally, those with decreased physical activity included participants who did not report moderate physical activity for at least 30 minutes per day for 5 or more days or vigorous physical activity for 20 minutes per day for 3 or more days over the last week. This corresponds to the U.S. Department of Health and Human Services guidelines for minimal amounts of physical activity to maintain optimal cardiovascular health.28
Statistical Analyses
Statewide estimates were computed using complex samples analyses features in STATA 9.2 (College Station, TX). Chi-squared statistics and corresponding p-values described differences observed in sexual assault prevalence within socio-demographic groups. Similarly, chi-squared statistics were used to compute differences between the 19-state estimate and Connecticut. We used multiple multivariable logistic regression models to determine the association between sexual assault (main independent variable) and various health care utilization variables (main dependent variables) while adjusting for sociodemographic covariates. We also used multiple regression models to determine the association between sexual assault (main independent variable) and negative health behaviors (main dependent variables) while adjusting for sociodemographic covariates. Sociodemographic covariates included age, education, sex, employment, income, and racial-ethnic group. We included potential confounders in adjusted analyses if they either were significant predictors at alpha ≤ 0.20 or altered crude point estimates more than 10%.29 We used a cut-off of p < 0.05 to determine statistical significance.
RESULTS
Study Population Characteristics
Table 1 depicts selected sociodemographic characteristics of our study population with comparisons to the 2000 U.S. Census Bureau estimates. Most of the study population (84.2%) were White, non-Hispanic; 51.2% were female; and 15.9% were older than the age of 65. Four percent of the sample had an annual household income less than $15,000, 5.8% had an education level less than high-school, 6.3% reported being unemployed or unable to work, and 61.4% were married. When compared to 2000 U.S. Census Bureau estimates30 our study population was slightly more likely to be married, had a higher annual household income, and reported a higher rate of unemployment or inability to work. Of note, direct statistical comparisons cannot be done given different methods of data collection of BRFSS versus the U.S. Census Bureau.
Table 1.
Characteristics of Study Population 2005 CT-BRFSS (n = 4183) Compared with the 2000 U.S. Census Bureau Estimates
| Characteristics | Sample N | Connecticut Prevalence, % (95% CI) | 2000 U.S. Census Bureau Estimates (%)* |
|---|---|---|---|
| White, non-Hispanic | 3426 | 84.2 (82.3 – 85.9) | 81.6 |
| Female | 2520 | 51.2 (49.1 – 53.3) | 51.2 |
| Age >65 | 915 | 15.9 (14.7 – 17.1) | 13.8 |
| Annual household income <$15,000 | 351 | 5.4 (4.7 – 6.3) | 6.5 |
| Education < HS | 430 | 6.8 (6.0 – 7.8) | 5.8 |
| Unemployed or Unable to Work | 341 | 6.3 (5.4 – 7.3) | 3.5 |
| Married | 2254 | 61.4 (59.2 – 63.6) | 55.0 |
* Statewide demographics were obtained from the 2000 Census Report (Census 2000 demographic profiles. Available at: http://www.ctnow.com/search/dispatcher.front?Query=census+2000&target=article.)
Table 2 depicts the complete sociodemographic characteristics of our study sample.
Table 2.
Complete Sociodemographic Characteristics of Study Population, 2005 CT-BRFSS (n = 4183)
| Characteristics | Sample Size* | Prevalence, % (95% CI)† |
|---|---|---|
| Race | ||
| White, non-Hispanic | 3426 | 84.2 (82.3 – 85.9) |
| Black, non-Hispanic | 290 | 5.1 (4.1 – 6.3) |
| Hispanic | 285 | 7.1 (6.0 – 8.3) |
| Other | 125 | 3.6 (2.4 – 5.7) |
| Sex | ||
| Male | 1663 | 48.2 (46.7 – 50.9) |
| Female | 2520 | 51.2 (49.1 – 53.3) |
| Age (in years) | ||
| 18-34 | 693 | 27.7 (25.4 – 30.2) |
| 35-44 | 828 | 21.4 (19.8 – 23.1) |
| 45-54 | 976 | 20.7 (19.3 – 22.2) |
| 55-65 | 771 | 14.3 (13.1 – 15.6) |
| >65 | 915 | 15.9 (14.7 – 17.1) |
| Annual household income ($) | ||
| < 15 K | 246 | 5.4 (4.7 – 6.3) |
| 15-25 K | 451 | 10.6 (9.5 – 11.9) |
| 25-50 K | 901 | 22.6 (21.2 – 24.1) |
| 50-75 K | 645 | 17.9 (16.4 – 19.4) |
| > 75 K | 1416 | 43.4 (41.4 – 45.5) |
| Education | ||
| Less than high-school | 283 | 6.8 (6.0 – 7.8) |
| Completed high-school | 1061 | 26.3 (24.6 – 28.1) |
| Some College | 942 | 23.5 (21.9 – 25.1) |
| Completed College | 1873 | 43.4 (41.5 – 45.2) |
| Employment | ||
| Employed | 2590 | 65.9 (63.8 – 67.9) |
| Unemployed/Unable to work | 341 | 6.3 (5.4 – 7.3) |
| Homemaker/Student | 378 | 12.3 (10.6 – 14.1) |
| Retired | 863 | 15.6 (14.4 – 16.8) |
| Marital Status | ||
| Married | 2254 | 61.4 (59.2 – 63.6) |
| Not Married | 1910 | 38.6 (33.9 – 43.9) |
* Some numbers do not total 4183 due to lack of responder completion
†Prevalence is derived from utilizing BRFSS complex samples features which adjust for unique weights and the cluster design of the survey
Prevalence of Sexual Assault
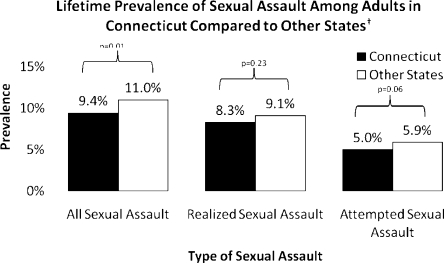
The lifetime prevalence of all forms of sexual assault in Connecticut was 9.4% (95% confidence interval [CI]: 8.3%–10.8%) (Fig. 1). Among all Connecticut adults surveyed, 8.3% (95% CI: 7.2%–9.6%) reported attempted sexual assault at sometime in their lives and 5.0% (95% CI: 4.1%-6.0%) reported realized sexual assault at sometime in their lives. Among the aggregated responses from 19 other states in the U.S., 11% of all adults reported sexual assault compared to 9.4% of Connecticut adults (p = 0.01).
Figure 1.
Lifetime prevalence of sexual assault among adults in Connecticut and other states. P-value for comparison generated from Wald-chi square statistics † Prevalence from other states describes the prevalence of sexual assault in 19 other states that utilized the BRFSS Module on Sexual Assault in 2005. These states include Arizona, Colorado, Delaware, Florida, Hawaii, Idaho, Mississippi, Missouri, Nevada, Ohio, Oklahoma, Puerto Rico, Rhode Island, South Carolina, Tennessee, Vermont, the U.S. Virgin Islands, Virginia, and Wisconsin.
Differences in Sexual Assault Rates by Sociodemographic Factors
Rates of sexual assault varied by sociodemographic factors (Table 3). Among adults aged 65 years and older, only 4.3% (95% CI: 3.0%–6.1%) reported sexual assault compared to 11.2% (95% CI: 8.3%–15.0%) of adults aged 18–34 years, (p < 0.0001). Among men, 3.7% (95% CI: 2.7%%–5.2%) reported sexual assault compared to 14.6% (95% CI: 12.6%–16.7%) of women, (p < 0.0001). Unemployed and home–maker student groups reported higher rates of sexual assault than employed and retired individuals. Although rates of sexual assault varied by education levels, no association existed between a higher education level and lower rates of sexual assault. Income was not significantly associated with sexual assault, with less affluent groups reporting rates of sexual assault that were comparable to more affluent groups. Similarly, no differences were seen in rates of sexual assault between racial-ethnic groups.
Table 3.
Differences in the Lifetime Prevalence of Realized or Attempted Sexual Assault by Sociodemographic Characteristics
| Demographic Characteristics | Number Sampled (N)* | Lifetime Prevalence of Realized or Attempted Sexual Assault, % (95% CI) | p-value† |
|---|---|---|---|
| Age, years | |||
| 18-34 | 693 | 11.2 (8.3 – 15.1) | <0.0001 |
| 35-44 | 828 | 10.2 (8.0 – 12.9) | |
| 45-54 | 976 | 10.0 (8.2 – 12.1) | |
| 55-65 | 771 | 8.6 (6.5 – 11.2) | |
| 65-over | 915 | 4.3 (3.0 – 6.1) | |
| Sex | |||
| Male | 1663 | 3.7 (2.7 – 5.2) | <0.0001 |
| Female | 2520 | 14.6 (12.6 – 16.7) | |
| Income, $ | |||
| <15,000 K | 246 | 10.5 (7.1 – 15.4) | 0.71 |
| 15-25 K | 451 | 8.3 (5.7 – 12.0) | |
| 25-50 K | 901 | 10.5 (8.2 – 13.2) | |
| 50 – 75 K | 645 | 11.5 (8.6 – 15.2) | |
| >75 K | 1416 | 9.8 (7.7 – 12.4) | |
| Race/Ethnicity | |||
| White, non-Hispanic | 3426 | 9.9 (8.6 – 11.5) | 0.15 |
| Black, non-Hispanic | 290 | 9.9 (6.2 – 15.4) | |
| Other | 285 | 6.4 (3.4 – 11.9) | |
| Hispanic | 125 | 6.0 (3.1 – 11.2) | |
| Employment | |||
| Employed | 2590 | 8.8 (7.6 – 10.2) | <0.0001 |
| Unemployed/Unable to work | 341 | 13.7 (9.8 – 18.9) | |
| Homemaker/Student | 378 | 15.4 (9.9 – 23.0) | |
| Retired | 863 | 4.5 (3.1 – 6.5) | |
| Education | |||
| Less than high-school | 283 | 7.8 (4.6 – 12.7) | 0.002 |
| Completed high-school | 1061 | 6.1 (4.6 – 8.0) | |
| Some College | 942 | 13.0 (9.8 – 17.1) | |
| Completed College | 1873 | 9.7 (8.2 – 11.5) | |
* Some numbers do not total 4183 due to lack of responder completion
†Wald chi-squared statistics
Sexual Assault and Health Care Utilization
Victims of sexual assault were more likely to report not having seen a physician in the previous 12 months for a routine check-up and more likely to report being unable to see a doctor because of cost (Table 4). This effect persisted even after multivariable adjustment with victims being more likely to report not having seen a doctor in the last 12 months for a routine check-up (adjusted odds ratio [AOR]: 1.5, 95% CI: 1.1–2.1) and reporting that they were unable to see a doctor because of cost in the prior year (AOR: 2.7, 95% CI: 1.7–4.3). No association existed in bivariate or multivariate analyses between sexual assault victimization and the absence of a health care plan or the presence of a personal physician.
Table 4.
Differences in Health Care Utilization Among Victims and Non-Victims of Sexual Assault
| Health Care Access Indices | Sexual Assault Victims, N = 422 N (%) | Non-victims of Sexual Assault N = 3739 N (%) (Referent Group) | Unadjusted Odds Ratio,* (95% CI) | Adjusted Odds Ratio,† (95% CI) | p-value ‡ |
|---|---|---|---|---|---|
| No health care plan§ | 31 (6.8) | 320 (9.0) | 0.7 (0.4 – 1.2) | 0.6 (0.4 – 1.0) | 0.06 |
| No personal physician║ | 45 (14.5) | 395 (12.1) | 1.2 (0.7 – 2.0) | 1.5 (0.9 – 2.7) | 0.16 |
| Could not see doctor because of cost in past 12 months¶ | 74 (19.9) | 283 (8.2) | 2.8 (1.8 – 4.3) | 2.7 (1.7 – 4.3) | <0.001 |
| Greater than 12 months without routine check-up# | 143 (39.4) | 1033 (30.3) | 1.5 (1.1 – 2.0) | 1.5 (1.1 – 2.1) | 0.001 |
*Odds ratio generated from Wald-chi square statistics
†After adjustment for age, sex, education, income, racial-ethnic group, and employment status in multivariable logistic regression modeling
‡Generated from multiple logistic regression modeling, after adjustment for age, sex, education, income, racial-ethnic group, and employment status
§ Health care plan included private insurance, prepaid plans such as HMOs, and government plans such as Medicare or Medicaid
║ Participants described if they had at least one person that they identified as their “personal doctor or health care provider”
¶ Participants were asked if in the past 12 months they needed to see a doctor but could not because of cost
# Participants reported whether they had gone for greater than 12 months without a routine health checkup
Sexual Assault and Unhealthy Behaviors
Higher rates of smoking, binge drinking, high-risk HIV behavior, at-risk alcohol consumption, and decreased physical activity levels were observed among victims of sexual assault when compared to non-victims (Table 5). After controlling sociodemographic factors, victims of sexual assault were more likely to be currently smokers (OR: 2.0, 95% CI: 1.3–3.0) and more likely to endorse at-risk drinking (OR: 3.3, 95% CI: 2.0–5.4) than those who reported no sexual assault. Associations between binge drinking and sexual assault victimization and decreased physical activity and sexual assault victimization were not statistically significant after multivariate modeling.
Table 5.
Differences in Unhealthy Behaviors Among Victims and Non-Victims of Sexual Assault
| Unhealthy Behaviors | Sexual Assault Victims, N (%) Total N = 419 | Non-victims of Sexual Assault, N (%) Total N = 3722 Referent Group | Unadjusted Odds Ratio,* (95% CI) | Adjusted Odds Ratio,† (95% CI) | p-value‡ |
|---|---|---|---|---|---|
| Current Smokers | 102 (26.6) | 586 (15.7) | 2.0 (1.4 – 2.8) | 2.0 (1.3 – 3.0) | 0.001 |
| Binge Drinking | 44 (16.7) | 420 (15.0) | 1.1 (0.6 – 2.0) | 1.6 (0.96 –1.8) | 0.07 |
| High Risk HIV Behavior | 20 (4.2) | 75 (3.3) | 1.3 (0.7 – 2.4) | 1.4 (0.7 – 2.8) | 0.30 |
| At-risk alcohol consumption | 45 (15.8) | 184 (4.9) | 3.7 (2.1 – 6.5) | 3.3 (2.0 – 5.4) | <0.001 |
| Unhealthy dietary habits | 278 (69.6) | 2687 (72.7) | 0.9 (0.6 – 1.1) | 1.0 (0.7 – 1.3) | 0.73 |
| Decreased physical activity | 215 (50.7) | 1841 (47.5) | 1.1 (0.9 – 1.5) | 1.3 (0.96 – 1.7) | 0.09 |
* Odds ratio generated from Wald-chi square statistics
†After adjustment for age, sex, education, income, racial-ethnic group, and employment status in multivariable logistic regression modeling
‡Generated from multiple logistic regression modeling, after adjustment for age, sex, education, income, racial-ethnic group, and employment status
DISCUSSION
Prevalence and Sociodemographic Correlates
In this first reported study of Connecticut residents, we found that 14.6% of women and 3.6% of men reported experiencing some form of sexual assault in their lifetime. These rates were significantly lower than national estimates. Our findings, however, confirm similarly lower rates of IPV in Connecticut compared to other states.31 Other sexual assault population-based studies have documented higher rates—as high as 19% among women9—in other less affluent, more racially-diverse states.
No significant association existed between income level and sexual assault in our study. This contradicts much of the literature on interpersonal violence and poverty,32 showing clear linkages between lower socioeconomic status and higher rates of interpersonal violence. In the 2007 U.S. Census Bureau publication,30 Connecticut ranked first among all states in personal income per capita. Indeed, few population-based studies have examined the sociodemographic correlates of sexual assault in relatively affluent environments. While in the developing world poverty may have clear linkages between financial mobility of victims, emasculation of male perpetrators of violence, may unmask gender inequality32 and therefore lead to higher rates of interpersonal violence. In our relatively affluent sample, other sociodemographic factors—specifically education and employment drove differences in assault rates. These findings are limited, however, in that they only describe bivariate, unadjusted associations and other indicators of poverty, aside from income, may drive the linkages between interpersonal violence and socioeconomic status.
Interestingly, although education level was significantly associated with sexual assault, no relationship existed between higher education level and lower rates of sexual assault. Specifically, individuals who received some college education but did not graduate reported higher rates of sexual assault than those who only attended high-school only or completed college. These findings have been replicated in two other population-based studies on the sociodemographic correlates of IPV.31,33 More studies are needed to document why those who attend some college but never graduate report higher rates of sexual assault then those who never attend or graduate college.
Our study also found higher rates of reported lifetime sexual violence among younger survey respondents. This finding has been confirmed in another study that examined male sexual assault rates in the United Kingdom and found higher rates of lifetime sexual violence among younger men.34 These findings suggest changes in sexual assault rates over time, which can be subject to both period and cohort effects. A period effect is less likely in this case given that our data were collected cross-sectionally, without any change in standard definition. A cohort effect is more likely and may have occurred for several reasons. First, recall bias may have blunted the sexual assault response rates of older Connecticut adults who may not have remembered sexual assault victimization which occurred in their youth. Second, disclosure of sexual assault may be more acceptable to younger as opposed to older adults. Third, rates of sexual assault may have increased over time. This assertion, however, seems less likely, given that recent studies have shown stable rates of sexual assault among cohorts of woman in the last thirty years.7
Health Care Utilization
A rich literature has described the association between forms of physical and sexual abuse by an intimate partner with unwanted health consequences, including higher rates of somatic complaints, sexually transmitted diseases, depression, and post-traumatic stress disorder.5,6,10 The association between abuse, whether physical or sexual, and health care utilization factors, especially outside of the immediate post-assault time period, is less well-understood. Earlier studies on this topic documented higher utilization of primary health care services among victims of interpersonal violence.11 Other population-based studies have shown no differences between utilization of primary health services between victims and non-victims.35,36 Our study is unique in that it is the first, to our knowledge, to examine the health care utilization trends of sexual assault victims, specifically. Furthermore, it shows that sexual assault victims were more likely to report not having a primary care provider, more likely to go without a routine check-up in the last 12 months, and more likely to report being unable to see a doctor because of cost than non-victims. These findings, in conjunction with findings from Chartier et. al.,8 Paranjape et. al.,18 and Henning et. al.,14 add to a growing body of literature that suggests that health-care utilization trends among victims of interpersonal violence are dynamic. While sexually assaulted victims may utilize more emergency health care services,37 both in the immediate post-assault period and later, they are less likely to access general preventive health services in primary care clinics and offices. Low utilization of routine health services may reflect the larger psychopathology of abusive partners who prevent the creation of a therapeutic alliance with the primary care physician, partner interference with health care,38 and control over household finances, including health care spending.
Riskier Behaviors
In addition to lower utilization rates of primary care services, sexual assault victims in our sample were more likely to smoke and to endorse heavy-drinking habits or “at-risk drinking” than non-victims. Population and clinic-based studies internationally and domestically have documented higher rates of tobacco abuse among victims of partner violence39 and sexual assault.9 Additionally, IPV victimization specifically has been associated with higher rates of other drug use including marijuana, crack-cocaine, and heroin use.40
Interestingly, our study did not find an association between lifetime prevalence of sexual assault and unhealthy dietary habits, inadequate physical activity, high risk HIV behavior, and binge drinking. This finding may suggest a statistical underpowering of our study to detect these differences; a larger BRFSS interstate study documenting the association between IPV and unhealthy behaviors found strong associations between lifetime exposure to IPV and smoking, binge drinking, high-risk HIV behavior, and obesity.41 More studies are needed, however, to examine the manner in which a history of sexual assault, a unique social determinant of disease, interplays with interpersonal violence to affect risky health behaviors and the subsequent development of chronic disease.
Our study is subject to limitations. First, the BRFSS, like any random-digit dialed telephone survey, does not survey homeless adults, institutionalized adults, and households without landline telephones. The increased use of cell-phone only households, particularly among the young, and declining response rates have provided other challenges to random-digit dialed telephone surveys, like the BRFSS.19,20 The populations excluded by the BRFSS including those who live in shelters, transient individuals, and the homeless, likely have higher rates of sexual assault perpetration. As such, the prevalence estimates in this study likely under-estimate the true prevalence of sexual assault in Connecticut. Second, because BRFSS is cross-sectional, we cannot establish causality between negative health behaviors, health care utilization and lifetime sexual assault. Finally, BRFSS relies on self-report data, which also may result in under-estimation of true prevalence given the sensitive nature asking about sexual assault history, the main outcome variable in this study. Despite these limitations, given the paucity of current population level data for state-wide sexual assault prevalence rates in the United States, the BRFSS and our study fulfills a critical role.31,42
Several clinical implications can be gleaned from our results. High rates of sexual assault in Connecticut and the absence of differences in prevalence among class and racial-ethnic groups necessitate public health workers, clinicians, and nurses to have a high index of suspicion for sexual assault victimization, regardless of sociodemographic profile. Given the concordance of tobacco and alcohol abuse among sexual assault victims, screening for these high risk behaviors should include an assessment of psychosocial stressors, especially a history of sexual assault. Finally, the burden of disease among sexual assault victims and their sporadic use of traditional primary care services necessitate more public health outreach programs and community level interventions to specifically target this high-risk group.
Acknowledgements
An earlier version of this manuscript was presented in oral format at the 31st Annual Society for General Internal Medicine (SGIM) Meeting in Pittsburgh, PA on April 10, 2008.
Conflicts of Interest None disclosed.
Financial Support Information None.
References
- 1.Tjaden P, Thoennes N. Prevalence, Incidence, and Consequences of Violence Against Women: Findings from the National Violence Against Women Survey Washington DC: National Institute of Justice; Centers for Disease Control and Prevention 1998.
- 2.Watts C, Zimmerman C. Violence against women: global scope and magnitude. Lancet. 2002;359:1232–7. doi: 10.1016/S0140-6736(02)08221-1. [DOI] [PubMed] [Google Scholar]
- 3.Jones AS, Dienemann J, Schollenberger J, et al. Long-term costs of intimate partner violence in a sample of female HMO enrollees. Womens Health Issues. 2006;16:252–61. doi: 10.1016/j.whi.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Max W, Rice DP, Finkelstein E, Bardwell RA, Leadbetter S. The economic toll of intimate partner violence against women in the United States. Violence Vict. 2004;19:259–72. doi: 10.1891/vivi.19.3.259.65767. [DOI] [PubMed] [Google Scholar]
- 5.Campbell J, Jones AS, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162:1157–63. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- 6.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359:1331–6. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 7.Casey EA, Nurius PS. Trends in the prevalence and characteristics of sexual violence: a cohort analysis. Violence Vict. 2006;21:629–44. doi: 10.1891/vivi.21.5.629. [DOI] [PubMed] [Google Scholar]
- 8.Chartier MJ, Walker JR, Naimark B. Childhood abuse, adult health, and health care utilization: results from a representative community sample. Am J Epidemiol. 2007;165:1031–8. doi: 10.1093/aje/kwk113. [DOI] [PubMed] [Google Scholar]
- 9.Cloutier S, Martin SL, Poole C. Sexual assault among North Carolina women: prevalence and health risk factors. J Epidemiol Community Health. 2002;56:265–71. doi: 10.1136/jech.56.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet. 2008;371:1165–72. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- 11.Plichta S. The effects of woman abuse on health care utilization and health status: a literature review. Womens Health Issues. 1992;2:154–63. doi: 10.1016/S1049-3867(05)80264-6. [DOI] [PubMed] [Google Scholar]
- 12.Dearwater SR, Coben JH, Campbell JC, et al. Prevalence of intimate partner abuse in women treated at community hospital emergency departments. JAMA. 1998;280:433–8. doi: 10.1001/jama.280.5.433. [DOI] [PubMed] [Google Scholar]
- 13.Kramer A, Lorenzon D, Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Womens Health Issues. 2004;14:19–29. doi: 10.1016/S1049-3867(03)00115-4. [DOI] [PubMed] [Google Scholar]
- 14.Henning KR, Klesges LM. Utilization of counseling and supportive services by female victims of domestic abuse. Violence Vict. 2002;17:623–36. doi: 10.1891/vivi.17.5.623.33714. [DOI] [PubMed] [Google Scholar]
- 15.McFarlane J, Wiist W, Soeken K. Use of counseling by abused pregnant Hispanic women. J Womens Health Gend Based Med. 1999;8:541–6. doi: 10.1089/jwh.1.1999.8.541. [DOI] [PubMed] [Google Scholar]
- 16.McNutt LA, Carlson BE, Gagen D, Winterbauer N. Reproductive violence screening in primary care: perspectives and experiences of patients and battered women. J Am Med Womens Assoc. 1999;54:85–90. [PubMed] [Google Scholar]
- 17.Miller E, Decker MR, Silverman JG, Raj A. Migration, sexual exploitation, and women’s health: a case report from a community health center. Violence Against Women. 2007;13:486–97. doi: 10.1177/1077801207301614. [DOI] [PubMed] [Google Scholar]
- 18.Paranjape A, Heron S, Kaslow NJ. Utilization of services by abused, low-income African-American women. J Gen Intern Med. 2006;21:189–92. doi: 10.1111/j.1525-1497.2005.00314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mokdad A, Stroup D, Giles W. Public Health surveillance for behavioral risk factors in a changing environment: recommendations from the Behavioral Risk Factor Surveillance team. MMWR Morb Mortal Wkly Rep 2003;52:1-12. [PubMed]
- 20.Mokdad AH. The Behavioral Risk Factors Surveillance System: past, present, and future. Annu Rev Public Health. 2009;30:43–54. doi: 10.1146/annurev.publhealth.031308.100226. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data: Centers for Disease Control and Prevention, US Department of Health and Human Services, 2005.
- 22.Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS) Social and Preventive Medicine. 2001;46(Suppl 1):S3–42. [PubMed] [Google Scholar]
- 23.Nelson DE, Powell-Griner E, Town M, Kovar MG. A comparison of national estimates from the National Health Interview Survey and the Behavioral Risk Factor Surveillance System. Am J Public Health. 2003;93:1335–41. doi: 10.2105/AJPH.93.8.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.(Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention 2005).
- 25.CDC FAQ on Alcohol Consumption. Available at: http://www.cdc.gov/alcohol/faqs.htm Accessed December 2, 2010.
- 26.Naimi TS, Brewer RD, Mokdad A, et al. Binge Drinking Among US Adults. JAMA. 2003;289(1):70–5. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- 27.Diet, nutrition and the prevention of chronic disease. Report of a joint FAO/WHO expert consultation, Geneva, WHO, 2003. WHO Technical Report Series, No. 916. [PubMed]
- 28.U.S. Department of Health and Human Services. Physical activity guidelines advisory committee report. Washington, DC: U.S. Department of Health and Human Services, 2008.
- 29.Rothman K, Greenland S. Modern epidemiology. Philadelphia, PA: Lippincott-Raven, 1998. 30.
- 30.Census 2000 Demographic Profiles. Available at: http://www.ctnow.com/search/dispatcher.front?Query=census+2000&target=article Accessed on December 2, 2010.
- 31.Breiding MJ, Black MC, Ryan GW. Prevalence and risk factors of intimate partner violence in eighteen U.S. states/territories, 2005. Am J Prev Med. 2008;34:112–8. doi: 10.1016/j.amepre.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Jewkes R. Intimate partner violence: causes and prevention. Lancet. 2002;359:1423–9. doi: 10.1016/S0140-6736(02)08357-5. [DOI] [PubMed] [Google Scholar]
- 33.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23:260–8. doi: 10.1016/S0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 34.Coxell A, King M, Mezey G, Gordon D. Lifetime prevalence, characteristics, and associated problems of non-consensual sex in men: cross sectional survey. BMJ. 1999;318:846–50. doi: 10.1136/bmj.318.7187.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hathaway JE, Mucci LA, Silverman JG, Brooks DR, Mathews R, Pavlos CA. Health status and health care use of Massachusetts women reporting partner abuse. Am J Prev Med. 2000;19:302–7. doi: 10.1016/S0749-3797(00)00236-1. [DOI] [PubMed] [Google Scholar]
- 36.Lemon SC, Verhoek-Oftedahl W, Donnelly EF. Preventive healthcare use, smoking, and alcohol use among Rhode Island women experiencing intimate partner violence. J Womens Health Gend Based Med. 2002;11:555–62. doi: 10.1089/152460902760277912. [DOI] [PubMed] [Google Scholar]
- 37.McCauley J, Kern DE, Kolodner K, et al. The "battering syndrome": prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann Intern Med. 1995;123:737–46. doi: 10.7326/0003-4819-123-10-199511150-00001. [DOI] [PubMed] [Google Scholar]
- 38.McCloskey LA, Williams CM, Lichter E, Gerber M, Ganz ML, Sege R. Abused women disclose partner interference with health care: an unrecognized form of battering. J Gen Intern Med. 2007;22:1067–72. doi: 10.1007/s11606-007-0199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ackerson LK, Kawachi I, Barbeau EM, Subramanian SV. Exposure to domestic violence associated with adult smoking in India: a population based study. Tob Control. 2007;16:378–83. doi: 10.1136/tc.2007.020651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.El-Bassel N, Gilbert L, Wu E, Go H, Hill J. Relationship between drug abuse and intimate partner violence: a longitudinal study among women receiving methadone. Am J Public Health. 2005;95:465–70. doi: 10.2105/AJPH.2003.023200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adverse health conditions and health risk behaviors associated with intimate partner violence--United States, 2005. MMWR Morb Mortal Wkly Rep 2008;57:113-7. [PubMed]
- 42.Verhoek-Oftedahl W, Pearlman DN, Coutu Babcock J. Improving surveillance of intimate partner violence by use of multiple data sources. Am J Prev Med. 2000;19:308–15. doi: 10.1016/S0749-3797(00)00237-3. [DOI] [PubMed] [Google Scholar]